Professional Documents
Culture Documents
Exd 12303
Uploaded by
Gustavo WollOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Exd 12303
Uploaded by
Gustavo WollCopyright:
Available Formats
Letter to the Editor
ever, because we have used cultured endothelial cells from a single source as the immobile phase, endothelial cell-based between-subject differences cannot be addressed. Although the individual responsiveness of patient-derived endothelial or other resident or circulating cells to TNFa and the respective adalimumab effects could be associated with clinical responses (2327), such an approach would not be feasible in any routine clinical setting.
healthy and psoriatic donors alike, and (iii) such differences are not associated with clinical responses of patients with psoriasis to adalimumab treatment.
Acknowledgements
We thank Dr. K. Wallbrecht for help with setting up experimental techniques and K. Zachmann for excellent technical assistance. AL performed the experiments, analysed and interpreted data and drafted the paper, MPS designed the research study, analysed and interpreted data and wrote the paper.
Conclusions
We have demonstrated that (i) dynamic interactions of human PBMC with TNFa-stimulated endothelial cells show considerable interindividual differences, (ii) these differences are found among
Conict of interests
This work was supported by a research grant from AbbVie, the manufacturer of adalimumab.
References
1 Fantuzzi F, Del Giglio M, Gisondi P et al. Expert Opin Ther Targets 2008: 12: 10851096. 2 Nestle F O, Kaplan D H, Barker J. N Engl J Med 2009: 361: 496509. n M P, Boehncke W H. N Engl J Med 2005: 3 Scho 352: 18991912. 4 Klein C L, Bittinger F, Kohler H et al. Pathobiology 1995: 63: 8392. 5 Nickoloff B J, Xin H, Nestle F O et al. Clin Dermatol 2007: 25: 568573. 6 Mako V, Czucz J, Weiszhar Z et al. Cytometry A 2010: 77: 962970. 7 Saurat J H, Stingl G, Dubertret L et al. Br J Dermatol 2008: 158: 558566. 8 Menter A, Tyring S K, Gordon K et al. J Am Acad Dermatol 2008: 58: 106115. 9 Tak P P, Taylor P C, Breedveld F C et al. Arthritis Rheum 1996: 39: 10771081. 10 Paleolog E M, Hunt M, Elliott M J et al. Arthritis Rheum 1996: 39: 10821091. 11 Burmester G R, Panaccione R, Gordon K B et al. Ann Rheum Dis 2013: 72: 517524. n M P. Exp Dermatol 2013: 12 Lockmann A, Scho 22: 358359.
13 Goodman R S, Kirton C M, Oostingh G J et al. Transplantation 2008: 85: 471477. 14 Wallbrecht K, Drick N, Hund A C et al. Exp Dermatol 2011: 20: 980985. 15 Oostingh G J, Schlickum S, Friedl P et al. J Invest Dermatol 2007: 127: 22532258. 16 Gordon K B, Langley R G, Leonardi C et al. J Am Acad Dermatol 2006: 55: 598606. 17 Scheinfeld N. J Dermatolog Treat 2004: 15: 348352. 18 Aggarwal B B. Nat Rev Immunol 2003: 3: 745 756. 19 Traczewski P, Rudnicka L. Br J Clin Pharmacol 2008: 66: 618625. 20 den Broeder A A, Joosten L A, Saxne T et al. Ann Rheum Dis 2002: 61: 311318. 21 Zaba L C, Suarez-Farinas M, Fuentes-Duculan J et al. J Allergy Clin Immunol 2009: 124: 1022 1010. 22 Campanati A, Orciani M, Gorbi S et al. Br J Dermatol 2012: 167: 6876. 23 Capsoni F, Sarzi-Puttini P, Atzeni F et al. Arthritis Res Ther 2005: 7: R250R255.
24 Bedini C, Nasorri F, Girolomoni G et al. Br J Dermatol 2007: 157: 249258. 25 Jokai H, Szakonyi J, Kontar O et al. Exp Dermatol 2013: 22: 221223. 26 Donetti E, Gualerzi A, Ricceri F et al. Exp Dermatol 2012: 21: 549551. 27 Fujiwara S, Nagai H, Oniki S et al. Exp Dermatol 2012: 21: 7072.
Supporting Information
Additional Supporting Information may be found in the online version of this article: Figure S1. The timing of adalimumab exposure determines the inuence on TNFa-induced leucocyte endothelial cell interactions. Figure S2. TNFa-induced endothelial cell adhesion molecule expression is abrogated by adalimumab in a time-critical fashion. Figure S3. Dynamic interactions of PBMC with TNFa-activated endothelial cells are not associated with the clinical response to adalimumab. Table S1. Primer sequences applied in RT-PCR. Data S1. Material and methods.
DOI: 10.1111/exd.12303 www.wileyonlinelibrary.com/journal/EXD
Letter to the Editor
First-in-human trial of nanoelectroablation therapy for basal cell carcinoma: proof of method
Richard Nuccitelli1, Ryan Wood1, Mark Kreis1, Brian Athos1, Joanne Huynh1, Kaying Lui1, Pamela Nuccitelli1 and Ervin H. Epstein Jr2
BioElectroMed Corp., Burlingame, CA, USA; 2Childrens Hospital Oakland Research Institute, Oakland, CA, USA Correspondence: Richard Nuccitelli, BioElectroMed Corp., 849 Mitten Rd., Ste 104, Burlingame, CA 94010, USA, Tel.: 650-697-3939, Fax: 650-697-3737, e-mail: rich@bioelectromed.com
Abstract: This nanoelectroablation therapy effectively treats subdermal murine allograft tumors, autochthonous basal cell carcinoma (BCC) tumors in Ptch1+/-K14-Cre-ER p53 / mice, and UV-induced melanomas in C57/BL6 HGF/SF mice. Here, we described the rst human trial of this modality. We treated 10 BCCs on three subjects with 1001000 electric pulses 100 ns in duration, 30 kV/cm in amplitude, applied at 2 pulses per second. Seven of the 10 treated lesions were completely free of basaloid cells when biopsied and two partially regressed. Two of the 7 exhibited seborrheic keratosis in the absence of basaloid
1
cells. One of the 10 treated lesions recurred by week 10 and histologically had the appearance of a squamous cell carcinoma. No scars were visible at the healed sites of any of the successfully ablated lesions. One hundred pulses were sufcient for complete ablation of BCCs with a single, 1-min nanoelectroablation treatment.
Key words: ablation apoptosis basal cell carcinoma nanoelectroablation nanosecond pulsed electric eld
Accepted for publication 8 December 2013
2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd Experimental Dermatology, 2014, 23, 130142
135
Letter to the Editor
Background
Very short electric pulses in the nanosecond domain have been found to penetrate into cells and tissues and permeabilize both organelle membranes and the plasma membrane if the electric eld strength is at least 10 kV/cm (1). One cellular response to the non-thermal application of hundreds of 100 ns pulses at 30 kV/cm is the initiation of apoptosis (2) and this nanoelectroablation therapy is very effective in eliminating murine skin tumors
without scarring (37). Direct measurement of mouse skin temperature during the application of 100 pulses indicated a temperature increase of only a few degrees (3,5) Therefore this is a non-hyperthermic therapy.
Questions addressed
The goals of this study were to test a new modality for the treatment of BCCs for the rst-in-human trial and to demonstrate safety and efcacy in treating human tumors leading to the application of this therapy to internal organ malignancies.
Experimental design
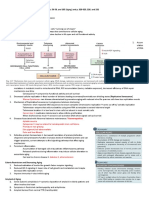
(a) (b) (c) (d) (e)
This rst Safety Clinical Trial of the NanoBlate System as a nonsignicant risk device was approved by the Childrens Hospital Oakland Research Institutes IRB and was registered on Clinicaltrials.gov (NCT01463709). Three subjects were recruited to participate and provided written informed consent. About 14 weeks
(a)
(b)
(c)
(d)
(e)
Figure 1. Five BCCs treated on a 55-year-old woman with basal cell nevus syndrome. (a) 5 9 10 mm lesion treated with 100 p, 30 kV/cm over two regions to cover the entire lesion. Images indicate lesion appearance before and after nsPEF treatment as well as 2, 10 and 14 weeks later. A histological section of each lesion collected at 14 weeks is shown on the bottom. Lesion a was undetectable by 10 weeks and histological analysis at 14 weeks indicated a dermal scar characterized by horizontally oriented collagen bundles and an increased number of vertically oriented vessels. Carcinoma was not identied within the biopsied portion of this lesion. (b) 5-mm-wide lesion treated with 100 p, 30 kV/cm. Lesion was nearly gone by 10 weeks and undetectable at 14 weeks. Carcinoma was not identied within the biopsied portion of this lesion. (c) 6-mm-wide lesion treated with 500 pulses, 30 kV/cm. Histological analysis of biopsy indicated invasive squamous cell carcinoma, keratoacanthoma type, narrowly excised on plane of section examined. The cup-shared lesion invaginates into the dermis and is lled with keratin. Squamous cells show minimal atypia and cells at base of lesion have a glassy-appearing cytoplasm. (d) 8-mm-long lesion treated with 380 pulses, 30 kV/cm. The electrode did not cover the entire lesion. Histology conducted at 14 weeks shows skin with multiple buds and irregular proliferations of basaloid cells attached to the undersurface of the epidermis. The peripheral layer of basaloid cells shows nuclear palisading and there is focal retraction artifact between the tumor islands and surrounding stroma. Necrotic keratinocytes and mitotic gures are present among the tumor cells. (e) 5-mm-wide lesion treated with 1000 pulses, 30 kV/cm. This lesion took longer to fade away. Histology conducted at 14 weeks indicated a dermal scar, characterized by horizontally oriented collagen bundles and an increased number of vertically oriented vessels. Carcinoma is not identied within the biopsied portion of this lesion.
Figure 2. Five BCCs treated on two subjects. (ab) 46-year-old woman. Lesion (a) was treated with 100 pulses, 30 kV/cm over two regions to cover the entire lesion with the 5 9 7 mm electrode coverage. Lesion was gone by 7 weeks and histological analysis of the treated region at 11 weeks indicated dermal scar, characterized by horizontally oriented collagen bundles and an increased number of vertically oriented vessels. Dermal melanophages are present within the supercial dermis. There is minimal lymphohistiocytic inltrate present. Carcinoma is not identied within the biopsied portion of this lesion. Lesion (b) was treated with 500 pulses, 30 kV/cm. The treated region was removed for biopsy at 11 weeks. Sections show a dermal scar, characterized by horizontally oriented collagen bundles and an increased number of vertically oriented vessels. There is focal calcication and keloidal collagen present within the dermis. A lymphohistiocytic inltrate is present surrounding the dermal brosis. Carcinoma is not identied within the biopsied portion of this lesion. (ce) Three BCCs treated on the scalp of a 60-year-old male. Lesion (c) was treated in four regions with 100 pulses, 30 kV/cm. At 15 weeks, the entire treated region was removed for histology. Sections show skin with buds and irregular proliferations of basaloid cells attached to the undersurface of the epidermis. The peripheral layer of basaloid cells shows nuclear palisading and there is focal retraction artifact between the tumor islands and surrounding stroma. Necrotic keratinocytes and mitotic gures are present among the tumor cells. Lesion (d) was treated with 1000 pulses, 30 kV/cm. Entire treated region was removed at 15 weeks and histological analysis indicated skin with seborrheic keratosis, including orthokeratotic hyperkeratosis, acanthosis, horn pseudocysts and an epidermal proliferation composed of small, bland, cuboidal keratinocytes. This proliferation lacks signicant cytologic atypia or mitotic activity. Dermal brosis is present. Lesion (e) was treated in two regions with 100 pulses, 30 kV/cm. The entire treated region was removed at 15 weeks and histological analysis indicated seborrheic keratosis, including orthokeratotic hyperkeratosis, acanthosis, horn pseudocysts and an epidermal proliferation composed of small, bland, cuboidal keratinocytes. This proliferation lacks signicant cytologic atypia or mitotic activity. Dermal brosis is present.
136
2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd Experimental Dermatology, 2014, 23, 130142
Letter to the Editor
after treatment of 10 BCCs, the treated skin regions were removed and processed for histological examination by a dermatopathologist to provide an objective evaluation of the treated region. Pre-treatment biopsies were not conducted, but post-treatment biopsies conrmed that the partially ablated lesions were BCCs by the presence of basaloid cells. Additional details regarding the methodology can be found in the Data S1.
Lesion (c) in Fig. 1 appeared to be completely covered by our electrode and was not visible on week 2. However, by week 10, a recurrent tumor was visible which histologically had the appearance of a squamous cell carcinoma (SCC).
Conclusions
This rst-in-human safety trial of nanoelectroablation indicated that this new therapy is safe and may offer a fast and scarless alternative to the current standard of care for small BCCs. The main advantages of this therapy over surgical excision or electrodesiccation and curettage are the reduced pain, the short treatment time and the absence of scarring. The efcacy of this treatment modality was good. Assuming that lesion (c) (Fig. 1) was actually a SCC that recurred, seven of the nine BCCs treated (78%) exhibited no basaloid cells when biopsied at 14 weeks after treatment. Three of these lesions disappeared completely, two exhibited hyperpigmentation and two exhibited seborrheic keratosis. We still need to conduct a real validation of this method with sufcient clinical data. Thereafter, we can compare it with other methods with relevant information for clinicians. This therapy could also be used to ablate other lesion types. BioElectroMed has had success ablating angiomas, moles and lentigines. Another group has used 20 ns pulses to successfully ablate several other tumor types in mice and one BCC on a human subject (8,9).
Results
We treated ten basal cell carcinomas (BCC) on three Caucasian patients with 1001000 electric pulses, each 30 kV/cm in amplitude and 100 ns long, at a rate of 2 pulses per second (pps) (See Data S1 for electrode and pulse shape images). We found that a single treatment of 100 pulses per treatment zone was sufcient to cause most of these lesions to disappear during the ensuing several weeks. Edema was present following treatment and the penetration points of the electrode needles were also evident (Fig. 1). A crust appeared over the treatment region within 2 days and began to fall off in 2 weeks. The skin was initially slightly pink in colour and after a few weeks appeared normal such that some treated lesions could not be located several weeks after treatment without reference to a pre-treatment map. However, in one patient with skin that was slightly darker than that of the other two patients, there was a hyperpigmentation at the two treatment sites (Fig. 2a,b). Histological analysis conrmed that this discoloration was not indicative of persisting tumor. Rather it is most likely due to inammation-induced stimulation of melanin production by melanocytes that is subsequently taken up by macrophages that remain long after inammation has ended. About 14 weeks after treatment, we removed skin from the treated region and collected serial thin sections every 100 lm through the entire region. These H&E-stained sections were subjected to independent histological analysis by a dermatopathologist. Seven of the 10 lesions were completely free of basaloid cells and two were partially ablated. Both of these two had not been treated over their entire surface. One of these was lesion (d) in Fig. 1. That lesion was slightly larger than our electrode; hence, the single treatment of 380 pulses did not cover the entire lesion. The second partial ablation is shown in Fig. 2c. This lesion was 2 cm long by 1 cm wide, and while we treated it with 100 pulses in four different regions, this treatment did not cover the entire lesion.
Acknowledgements
We want to thank Joselyn Lindgren and Maria Acosta Raphael for recruiting the patients for this study and the dermatopathologist, Dr. Jinah Kim, for providing histological analysis of the biopsies. This work was supported by NIH grants R44CA123924, R44CA150484 and R01CA125722 to RN.
Author contribution
RW, MK and BA built the pulse generator and electrodes. JH and KL developed the optimal pulse parameters for lesion treatment. RN, PN, MK and EE conducted the treatments. RN analysed the data and wrote the paper. All authors contributed to the nal draft of the paper.
Conict of interest
BioElectroMed built the prototype NanoBlate models used in these experiments but is not marketing these pulse generators. Two of the authors own stock in BioElectroMed.
References
1 Schoenbach K H, Beebe S J, Buescher E S. Bioelectromagnetics 2001: 22: 440448. 2 Schoenbach K H. Bioelectric effect of intense nanosecond pulses. In: Pakhomov A G, Miklavcic D, Markov M S, eds. Advanced Electroporation Techniques in Biology and Medicine. Boca Raton: Taylor and Francis Group, 2010: 1950. 3 Nuccitelli R, Pliquett U, Chen X et al. Biochem Biophys Res Commun 2006: 343: 351360.
4 Nuccitelli R, Chen X, Pakhomov A G et al. Int J Cancer 2009: 125: 438445. 5 Nuccitelli R, Tran K, Sheikh S et al. Int J Cancer 2010: 127: 17271736. 6 Nuccitelli R, Tran K, Lui K et al. Pigment Cell Melanoma Res 2012: 25: 618629. 7 Nuccitelli R, Tran K, Athos B et al. Biochem Biophys Res Commun 2012: 424: 446450. 8 Garon E B, Sawcer D, Vernier P T et al. Int J Cancer 2007: 121: 675682.
9 Yin D, Yang W G, Weissberg J et al. PLoS ONE 2012: 7: e43891.
Supporting Information
Additional Supporting Information may be found in the online version of this article: Data S1. Methods.
2013 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd Experimental Dermatology, 2014, 23, 130142
137
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Class-10 Revision Test - NutritionDocument4 pagesClass-10 Revision Test - NutritionVarshini PeraNo ratings yet
- MED12 mutations common in breast phyllodes tumours and fibroadenomasDocument6 pagesMED12 mutations common in breast phyllodes tumours and fibroadenomasLuis GuzmánNo ratings yet
- Science 10 - 2ND Summative TestDocument2 pagesScience 10 - 2ND Summative Testalmira villarealNo ratings yet
- Food Chain SimulationDocument5 pagesFood Chain SimulationJose CabezasNo ratings yet
- Antibiotic: Prepared By: Osama Edris Hama SamanDocument18 pagesAntibiotic: Prepared By: Osama Edris Hama SamanSaviana TiekuNo ratings yet
- Robbins Notes: Aging, Radiation, and Inflammation Self StudyDocument44 pagesRobbins Notes: Aging, Radiation, and Inflammation Self StudyJustine HungNo ratings yet
- AP Biology - Chapter 29 Discussion AnswersDocument3 pagesAP Biology - Chapter 29 Discussion Answersangel91me6371100% (1)
- Module 3 - Biodiversity and EvolutionDocument39 pagesModule 3 - Biodiversity and EvolutionMichael Ramirez100% (9)
- Sexual Reproduction in PlantsDocument23 pagesSexual Reproduction in PlantsStephen AreriNo ratings yet
- Liv.52 TabletsDocument2 pagesLiv.52 TabletsSYED MUSTAFANo ratings yet
- (Studies in Behavioural Adaptation) Robin I. M. Dunbar (Auth.) - Primate Social SystemDocument382 pages(Studies in Behavioural Adaptation) Robin I. M. Dunbar (Auth.) - Primate Social SystemSourav Kapri100% (1)
- Science Technology and Society Chapter 3Document76 pagesScience Technology and Society Chapter 3JOHN RONALD SAJOL67% (3)
- Ginther, 1998 Equine PregnancyDocument32 pagesGinther, 1998 Equine PregnancyAdrian Ayala GutierrezNo ratings yet
- Aflp 1Document55 pagesAflp 1Purushotham PaspuletiNo ratings yet
- How To Keep Your Brain HealthyDocument3 pagesHow To Keep Your Brain HealthySyahidah IzzatiNo ratings yet
- General Pathology (Lecture-1) - 3Document14 pagesGeneral Pathology (Lecture-1) - 3Usman AkramNo ratings yet
- Patentability of Biotech Subject MatterDocument136 pagesPatentability of Biotech Subject MatterGareth WealeNo ratings yet
- Paper 6 November 2000Document2 pagesPaper 6 November 2000MSHNo ratings yet
- Molecular Biology: Louise Kamona Kabwe 1616713: 1001839253:::: / 784199656856434: 100821ASTJ0035Document1 pageMolecular Biology: Louise Kamona Kabwe 1616713: 1001839253:::: / 784199656856434: 100821ASTJ0035Louise KamonaNo ratings yet
- HUMAN PHYSIOLOGY KEY FUNCTIONSDocument17 pagesHUMAN PHYSIOLOGY KEY FUNCTIONSplsssssNo ratings yet
- General Biology 2 TG PDFDocument269 pagesGeneral Biology 2 TG PDFCamille Sison-Almirol100% (2)
- Friedreich 'S Ataxia: Clinical Features, Pathogenesis and ManagementDocument12 pagesFriedreich 'S Ataxia: Clinical Features, Pathogenesis and ManagementVaibhav BhatiaNo ratings yet
- Test I. Blood Puzzle: Find The Words Listed Below in The Word SearchDocument2 pagesTest I. Blood Puzzle: Find The Words Listed Below in The Word SearchPilarieBernalNo ratings yet
- Gender Is It A Social Construct or A Biological InevitabilityDocument5 pagesGender Is It A Social Construct or A Biological InevitabilitySaurabhChoudharyNo ratings yet
- Lecture-Cell Membranes and SignalingDocument64 pagesLecture-Cell Membranes and SignalingDiabyNo ratings yet
- Function of RBCDocument9 pagesFunction of RBCAthea MelosantosNo ratings yet
- 04 Macromolecules-1Document53 pages04 Macromolecules-1keikisboyNo ratings yet
- Cell Transport Practice TestDocument4 pagesCell Transport Practice TestLavander Blush100% (2)
- Malaria in MitteleuropaDocument12 pagesMalaria in MitteleuropaZ ZNo ratings yet
- Yong-Kyu (2009) Handbook Behavior GeneticsDocument579 pagesYong-Kyu (2009) Handbook Behavior GeneticsMaria Angelica MuñozNo ratings yet