Professional Documents
Culture Documents
595 - 610 Chimponda T
Uploaded by
Syahrul Hamidi NasutionOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
595 - 610 Chimponda T
Uploaded by
Syahrul Hamidi NasutionCopyright:
Available Formats
Tropical Biomedicine 27(3): 595610 (2010)
Antimycobacterial activities of selected medicinal plants from Zimbabwe against Mycobacterium aurum and Corynebacterium glutamicum
Chimponda, T. and Mukanganyama, S.1*
1Biomolecular
Interactions Analyses Group, Department of Biochemistry, University of Zimbabwe, P.O. Box MP 167, Mount Pleasant, Harare, Zimbabwe *Corresponding author email: smukanganyama@medic.uz.ac.zw, Received 17 February 2010; received in revised form 21 June 2010; accepted 20 August 2010
Abstract. The spread of multi-drug resistant tuberculosis necessitates the discovery of new classes of antibacterials and compounds that inhibit macromolecules involved in these resistant mechanisms. Thirty ethanol extracts from nineteen selected plants from Zimbabwe were screened against Mycobacterium aurum and Corynebacterium glutamicum using the agar disk diffusion method. These two organisms were used as models for Mycobacterium tuberculosis . The amount of ciprofloxacin accumulated and effluxed by the test organism was used to determine whether the plant extracts could also act as drug efflux pump inhibitors. Vernonia adoensis and Mangifera indica extracts at 500 mg/disk had the highest growth inhibitory activity against M. aurum and C. glutamicum respectively. The extract from Parinari curatellifolia had an MIC of 8 g/ disk and an MBC of 63 g/disk; an MIC of 125 g/disk and an MBC of >500 g/disk against M. aurum and C . glutamicum respectively. All the plant extracts were bacteriostatic and showed antagonistic effects when combined with rifampicin. The extract from P. curatellifolia made M. aurum and C. glutamicum accumulate the highest amount of ciprofloxacin. The accumulation of ciprofloxacin caused by P. curatellifolia extract was greater than that caused by the drug efflux inhibitor reserpine. This plant may serve as a source of lead compounds in the search of new antimycobacterials with new mechanisms of action.
INTRODUCTION Tuberculosis (TB) was thought to have been eradicated in the early second half of the past century. However, this old disease has resurged at an alarming speed both in developing and industrialised countries (Bamuamba et al ., 2008). TB remains an important public health problem, accounting for 8 million new cases per year. Despite improvements in chemotherapy, the treatment of TB is severely affected by the development of multi-drug resistance in Mycobacterium tuberculosis strains (Higuchi et al ., 2008). The situation has been worsened by the association of TB and HIV especially in Sub-Saharan Africa
and many developing countries (WHO Global report, 2009). Zimbabwe is ranked 17 th on the list of 22 high burden TB countries in the world. According to the World Health Organizations (WHOs) Global tuberculosis report (2009), Zimbabwe had an estimated 71 961 tuberculosis cases in 2007 with an estimated incidence rate of 539 cases per 100 000 populations. She has the second highest mortality TB rate in the world and TB-HIV/AIDS co-infection rate is high with nearly 69% of new adult TB patients testing positive (WHO, 2009). National data suggests the actual figure to be about 80% after an increasing HIV surveillance in HIV patients. The rapid spread of TB calls for
595
decisive action and the need for newer antimycobacterial agents (Suresh et al ., 2008). Although drug regimens exist for treating tuberculosis, they are far from ideal. The current treatment requires that a person take at least three or four antituberculosis drugs. The leading drug combinations are isoniazid and rifampicin and may be supplemented with pyrizanamide and ethambutol. However, due to poor patient compliance, there has been an emergence of multi-drug resistant (MDR) strains of bacteria. The spread of multi-drug resistant strains of bacteria necessitates the discovery of new classes of antibacterials and compounds that inhibit macromolecules involved in these resistant mechanisms (Mann et al., 2008). Plant-derived drugs have been used worldwide in clinical medicines for the treatment of various diseases. Plant species still serve as a rich source of many novel biologically active compounds, as very few plant species have been thoroughly investigated for their medicinal properties (Jachak et al ., 2007). Plants have, thus, been screened for antimycobacterial activity as some of them have been shown to have this property (McGaw et al., 2008a). Buddleja saligna, for example, is used traditionally for the treatment of diarrhoea and gastric disorders (Bamuamba et al. , 2008). Furthermore, some of the plants screened are used in the traditional treatment of tuberculosis and other respiratory related ailments (Chigora et al., 2007) for example Vernonia adoensis. Phytochemicals can improve the activity of existing drugs by acting as efflux pump inhibitors and can also reduce the occurrence of drug resistant forms of bacteria (Stavri et al., 2007). Traditions of collecting, processing and applying plants and plant-based medications have been handed down from generation to generation. Because of this strong dependence on plants as medicines, it is important to study their safety and efficacy (Fennell et al ., 2004). Many medicinal plants produce a variety of
compounds of known therapeutic properties. Substances that can either inhibit the growth of pathogens or kill them and have little or no toxicity to host cells are considered good candidates for developing new antimicrobial drugs (Woods-Panzaru et al., 2009). The populations of developing countries worldwide continue to rely heavily on traditional medicine as their primary source of health care. Ethnobotanical studies carried out throughout Africa confirm that indigenous plants are the main constituents of traditional African medicines (Mann et al., 2008). With more than 80% of the population of developing countries relying on traditional medicines, the importance of the role of medicinal plants in the health care delivery is very enormous particularly for the respiratory diseases (Chigora et al., 2007). The spread of multi-drug resistant (MDR) strains of bacteria necessitates the discovery of new classes of antibacterials and compounds that inhibit these macromolecules involved in these resistant mechanisms (Mann et al., 2008). The aim of this study was to investigate the in vitro antimycobacterial activities of nineteen Zimbabwean medicinal plant extracts against two model non-pathogenic actinomycetales species; Mycobacterium aurum and Corynebacterium glutamicum. Corynebacterium glutamicum like, M. tuberculosis also contains mycolic acids as part of its outer membrane components (Arun et al., 2008). These plants were selected based on literature survey of their ethnomedicinal usages in the treatment of microbial infections and are listed in Table 1.
MATERIALS AND METHODS Mycobacteria and Reagents Corynebacterium glutamicum (ATCC 13022) and M. aurum (A+) were used as model organisms for M. tuberculosis . Mycobacterium aurum was kind gift
596
from Prof. Smith of the Department of Pharmacology, University of Cape Town and Prof. Steenkamp, of the Department of Clinical Laboratory studies, University of Cape Town provided the C. glutamicum. Luria Bertani media, glucose, Middlebrook 7H9, casein acid hydrosylate, Middlebrook 7H11, nutrient agar, sodium dihydrogen phosphate, disodium hydrogen phosphate, glycine, hydrochloric acid, reserpine, ciprofloxacin, dimethyl sulphoxide (DMSO) and sodium azide were obtained from Sigma Aldrich Company (Taufkirchen, Germany). All other chemicals used were of the highest grade and were obtained from various sources. Plant collection The plants used in this work were collected from three provincial localities of Zimbabwe, Norton (Mashonaland West), Centenary (Mashonaland Central) and University of Zimbabwe (Harare), Zimbabwe. The plants identity were authenticated and classified by Mr. Christopher Chapano, a taxonomist at the National Herbarium and Botanic Gardens, (Harare, Zimbabwe). Herbarium samples were kept at the Department of Biochemistry, University of Zimbabwe. Preparation of extracts Plant material were dried in an oven at 50C and ground in an electric blender (Cole Parmer Instrument Company, Connecticut, USA) to a fine powder. A volume of 8 ml of ethanol was added to 2 g of powder and shaken for 5 minutes on a vortex and left to sit for 10 minutes. A syringe was prepared by inserting a piece of fine sieve. The plant suspension was then transferred into syringe and filtered into a small glass vial. The sterile suspension was filtered again using 0.45 M Millipore sterile filter (Sigma-Aldrich, Taufkirchen, Germany) into a labeled small glass vial. Ethanol was left to evaporate overnight in fume hood with air stream. A constant dry weight of each extract was obtained and the residues were stored at 4C until when required.
Culture of bacteria Middlebrook 7H9 medium was prepared by combining 4 g of Middlebrook 7H9 base and supplementing it with 1 g casein acid hydrosylate, and making up to 1 litre with distilled water. LB broth was prepared by combining 10 g sodium chloride, 5 g yeast extract, 10 g tryptone and 5 g glucose and distilled water was added to make a 1 litre solution. The media was sterilized by autoclaving. Mycobacterium aurum was inoculated into 20 ml Middlebrook 7H9 solution supplemented with casein acid hydrosylate while C. glutamicum was inoculated into 20 ml LB broth supplemented with glucose (LBG) from solid slants of the bacteria. The tubes were incubated at 37C overnight and growth was checked for on the growth medium. Bacteria were enumerated and diluted to make up a concentration of 1 x 106 cfu/ml. Antimycobacterial susceptibility test Middlebrook 7H11 supplemented with casein acid hydrosylate and Luria bertani broth media supplemented with glucose were prepared and allowed to cool. A sample of 1 x 106 cfu/ml of M. aurum and C. glutamicum was inoculated into the media and mixed. The media now containing bacteria was allowed to solidify. The test material equivalent to 500 g, dissolved in ethanol was applied on sterile paper disks (6 mm diameter, cartridge susceptibility disks, Mast Diagnostics, Mast Group Ltd, Merseyside, UK). The solvent was allowed to evaporate under a stream of air from filters deposited on 96-well plates at room temperature. The disks were then deposited on the surface of the inoculated agar plates. Plates were incubated at 4C for 2 hours and then at 37C in a Labcon incubator (Gallenkamp, England) for overnight. The inhibition zone which is the diameter of inhibition around each of the disc was measured and recorded in millimeters. Rifampicin, a standard antimycobacterial agent was used as the positive control whilst ethanol was used as the negative control.
597
Determination of Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC) The in-disk agar disk diffusion assay was carried out to determine the MIC and MBC according to Zaidan et al. (2005) with slight modifications. The disk diffusion test was carried out with twelve disks of 2-fold serially diluted concentrations of the plant extracts (500 g/disk 0 g/disk). Extracts concentrations were prepared by serial dilution. Rifampicin was used a positive control for both M. aurum and C. glutamicum. An aliquot of 1 x 106 cfu/ml of the bacteria was inoculated into the media, Middle Brook 7H11 and LB supplemented with glucose for M. aurum and C. glutamicum respectively. The agar was poured into 90 mm petri dishes (Concorde Plastics, Johannesburg, SA) and was allowed to cool. The filter disks impregnated with the plant extract were then placed onto the agar plates in duplicates and were incubated for 2 hours at 4C. The agar plates were then incubated overnight at 37C and 30C for M. aurum and C. glutamicum respectively. The lowest concentration that inhibited growth was taken as the minimum inhibitory concentration (MIC) value for each of the bacterial species. The MIC was then determined as the lowest concentration where there was a zone of inhibition for each plant extract. Minimum bactericidal concentration (MBC) assay were determined as the lowest concentration that completely kills bacteria. The MBC was determined from the MIC plates and the preceding plates by streaking MIC plates on the zone of inhibition and sub-culturing the organisms onto fresh Middle Brook 7H9 and LBG agar for M. aurum and C. glutamicum respectively that had no extracts. The plates were incubated at 37C and 30C overnight for each particular for M. aurum and C. glutamicum respectively. The MBC was recorded, as the lowest concentration at which there was no growth of bacteria after the sub-culturing into an plant extract (or drug)-free medium. The assays were repeated four times.
Effect of combining plant extract and rifampicin Extracts at concentration of MIC, double the MIC and ten times the MIC value of the plant extract with or without rifampicin was placed on filter disks (6 mm diameter, cartridge susceptibility discs, Mast Diagnostics, Mast Group Ltd, Merseyside, UK) and allowed to dry. The extract and the rifampicin maintained constant at 15 g/ml were combined and placed on the disks. Rifampicin alone at concentrations of 15 g/ml, 10 g/ml and 5 g/ml was also placed on the filter paper. Rifampicin at varying concentrations was combined with the test compound constant (up to ten times the MIC) and placed onto filter papers and allowed to dry. A quantity of 1 x 106 cfu/ml of the bacteria was inoculated into the media, Middle brook 7H11 and LB. The agar was poured onto petri dishes and was allowed to cool. The filter disks were then placed onto the agar plates, incubated for 2 hours at 4C and then overnight at 30C and 37C for C. glutamicum and M. aurum respectively. The zone of inhibition was then measured. All the experiments were performed in quadruplicate. Flouroquinolone accumulation and active efflux Accumulation and efflux of the flouroquinolone, ciprofloxacin was measured by the method of Mortimer & Piddock (1991) with some modifications. Bacteria were grown in Middlebrook 7H11 and LB media at 37C and 30C for M. aurum and C. glutamicum to an A660 of 0.6-0.8 and harvested by centrifugation at 3000 rpm for 10 minutes. Bacteria were then washed twice with 50 mM sodium phosphate buffer (pH 7.0) at 4C. The cells were weighed and a volume needed to make up a volume of 40 mg/ml was made in 10 mM PBS containing sodium azide. The mixture was incubated at 37C for 15 minutes. The flouroquinolone ciprofloxacin was added to the mixture to a final concentration of 20 mg/ml. The reaction mixture was incubated at 37C with shaking at 120 rpm for 60 minutes. The sample was
598
divided into two aliquots, a 2/3 and 1/3 volume sample, which were then centrifuged for 5 minutes at 2800 x g. The supernatant was discarded and the pellet was weighed. PBS was added to the 1/3 sample to make up to a concentration of 40 mg/ml, this tube representing a sample without glucose. The 2/3 sample was further subdivided into 3 equal aliquots of 40 mg/ml containing reserpine, ethanol and plant extracts. Appropriate controls were set up to rule out the effects of the solvent. The samples were mixed and incubated at 37C at 120 rpm for 30 minutes. The samples were centrifuged in a Rotofix centrifuge (Zentrifugen, Germany) for 5 minutes at 2800 x g. The cells were washed in the chilled buffer and re-centrifuged for 5 minutes. Glycine hydrochoride 3.0 ml (0.1M, pH 3.0) was added to the pellet at 37C and 30C for M. aurum and C. glutamicum respectively with agitation to ensure exposure of the cells to the lysis buffer and the solutions were left overnight. The pellet was then centrifuged at 2800 x g for 10 minutes in a Rotofix centrifuge. The supernatant was centrifuged for another 5 minutes. The fluorescence of ciprofloxacin was determined at the excitation and emission wavelengths of 270 nm and 452 nm respectively using an RF-1501 Shimadzu spectroflourimeter (Shimadzu Cooperation, Tokyo, Japan). Both supernatant samples from the intact cells (representing efflux samples) and the lysed cells (representing influx samples) were quantified for ciprofloxacin using a standard curve. To rule out interference from the reserpine and the plant extracts, their fluorescence was determined at the same excitation and emission wavelength as ciprofloxacin. The active efflux/influx of ciprofloxacin from the mycobacteria species was also examined in the presence of ethanolic extracts from the plants V. adoensis, Parinari curatellifolia, Mangifera indica for C. glutamicum and V. adoensis, P. curatellifolia and Faurea species for M. aurum. Statistical analysis All values have been expressed as mean 599
standard deviation and the comparison of the antibacterial activity of the samples with standard antibiotics was evaluated by applying One-way ANOVA with Dunnetts Multiple Comparison Test using Graphpad Instat software (Graphpad Prism Inc. San Diego, CA, USA, www. Graphpad.com). P values less than 0.05 were considered to be statistically significant difference.
RESULTS Screening by Disk diffusion assay The study was carried out to offer a better understanding of the ethnomedicinal and biological use of some of the plants widely distributed in Zimbabwe. A total of 30 ethanol extracts from nineteen different plants belonging to seventeen families were analysed. Plants were selected on the basis of their ethnomedicinal uses in the treatment of symptoms associated with TB in Zimbabwe (Table 1). Table 2 shows the growth inhibitory parameters of the ethanol plant extracts against M. aurum and C. glutamicum. V. adoensis was the most potent plant extract when using M. aurum and M. indica was the most potent plant extract when using C. glutamicum. Generally the antibacterial activity was low when using C. glutamicum as the test organism. The other plants showed mild to moderate antibacterial activities against the bacterial species. Determination of MIC and MBC Table 2 shows the antibacterial activities (MIC values in g/disc) of five plant extracts which were found to have the most potent antibacterial activity by disc diffusion assay. The lowest MIC for C. glutamicum was that for the extract from Lippia javanica (32 g/disk). The extract from Ziziphus mucronata had antibactericidal activity at a high concentration of 500 g/disk. These results suggest that the plant extracts had bacteriostatic activity when C. glutamicum was used as the test organism. For M. aurum, the extract from the stems of P. curatellifolia was the most potent with an
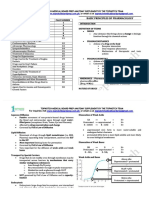
Table 1. Ethnobotanical information of investigated plants from Zimbabwe
Family Botanical name Local name Voucher Plant part tested fruit Major traditional use (Reference) Okra is a traditional food plant. It is used for the treatment of bronchitis, heart diseases and tuberculosis of the lungs (www.greenpatio, 2010) Widely used for external treatment of minor wounds and inflammatory skin disorders. It is used for the treatment of pneumonia, tuberculosis and cough (Gelfand et al., 1985) Leaves are used for pulmonary infections, bark is an astringent (Serada et al ,2002). Various respiratory ailments (Gelfand et al. , 1985). Treatment of diarrhea (Chinemana et al ., 1985). Roots and bark infusions treat respiratory disorders (Roodt 1998). Treatment of bilharzias, helminthiasis (Baerts & Lehmann, 1989). Treatment of cough, pneumonia and tuberculosis (Gelfand et al. , 1985). Treatment of coughs, pneumonia and TB (Gelfand et al., 1985). Leave infusion used to treat coughs, colds and fever, influenza, measles, malaria and stomach ache (Van Wyk, 2009). Treatment of tuberculosis (Kisangau et al ., 2007). Treatment of abdominal pain (Chinemana et al .,1985). Skin rashes, tuberculosis, Chronic diarrhea, herpes zoster, herpes simplex (Chigora et al. , 2007). Trearment of headache (Maliwichi, 2000). Treatment of menorrhagia (Lewu & Afolayan, 2009). Chest pain (De Boer et al., 2004). Roots treat diarrhea and stomach disorders (Van Wyk 2009), a hot infusion of the root bark treats pneumonia (Roodt,1998). The leaves are used for treatment of TB (Kisangau et al ., 2007). Mastitis and backache (Ruffo,1991). Paste of leaves treats boils, carbuncles and swollen glands, leaf infusion is taken against chest complaints (Roodt, 1998).
Malvaceae
Abelmoschus esculentus Moench
Derere
N15E10
Aloaceae
Aloe vera barbadensis Miller
Gavakava
N16E4
Leaves
Rubiaceae
Catunaregam spinosa Thunb
Mutsvairachuru Murovaduri
C5E7 C5E4 C5E1
Leaves Bark Roots
Leguminosae Euphobiaceae
Rhynchosia insignis (O.Hoffm.) R.E.Fr. Croton gratissimus Burch.
Mukoyo Gunukira, Mufandemenge, Mugugu, Mubvukuta Mutsatstsi
C15E7 UZ13E7
Leaves Leaves
Proteaceae
Faurea saligna Harv Garcinia huillensis Welw Gymnosporia senegalensis Loes Lippia javanica (Burm.f.) Spreng
C13E7
Leaves
Clusiaceae
Mutunduru
C10E7
Leaves
Celastraceae Verbenaceae
Chishuzhu Musosawafa Zimbani
N3E7 C3E7 C3E4 C3E7 N17E4 UZ8E7 UZ8E4 C6E7 C6E4
Leaves Leaves Bark Roots Stems Twigs Leaves Stems Leaves Bark
Anarcardiaceae Olacaceae Chrysobalanaceae
Mangifera indica (L) Olax obtusifolia De Wild Parinari curatellifolia Planch, ex Benth
Mumango Gungwe Kahungwarara Muhacha
Anarcadiaceae Solanaceae Myrtaceae Combretaceae
Rhus longipes Engl Solanum mauritianum Scop Syzygium guineense Guill & Perr Terminalia sericea Burch. ex DC.
Muchokochiana Mudzambuya Muboo Mukonono
C11E10 C11E7 UZ10E7 C8E7 C14E7
Flowers Leaves Leaves Leaves Leaves
Asteraceae
Vernonia adoensis Sch.Bip.ex Walp Xerroderris stuhlmannii (Taub) Mendonca and E.P Sousa. Ziziphus mucronata Willd.
Musikavakadzi
C1E10 C1E7 C1E1 C4E7 C4E4 C7E7 C7E4
Flowers Leaves Roots Leaves Bark Leaves Stems
Leguminosae
Murumanyama
Rhamnaceae
Muchecheni
600
Table 2. Minimum inhibitory concentrations and minimum bactericidal concentrations of extracts towards the mycobacterial species
Plant extract
aZone
of inhibition (mm) at 500 (g/disc) bMIC (g/disc) cMBC (g/disc) M. aurum
Plant extract
Zone of inhibition (mm) at 500 (g/disc) MIC (g/disc) MBC (g/disc) C. glutamicum
Vernonia adoensis leaves
a 28 b 31
Mangifera Indica (leaves)
c 250
17 1 250 >500 15 1 250 >500 13 1 125 >500 13 1 125 500 12 1 32 >500
Faurea saligna leaves
18 1 250 >500
Vernonia adoensis leaves roots
Syzygium guineense leaves
19 2 18 1 31 125 18 1 8 63 18 1 63 125 29 2 2 16
Parinari curatellifolia stems
Xerroderris stuhlmannii leaves
Ziziphus Mucronata stems
Parinari curatellifolia stems
Lippia javanica roots
Parinari curatellifolia Leaves
Rifampicin
Rifampicin
40 1 <1 63
aResults are the average ( SD) of two separate antibacterial susceptibility test (Each antibacterial susceptibility test was followed by a disk diffusion assay done in quadruplicate). The zone of inhibition being determined at a concentration of 500 g/disk MIC Minimum inhibition concentration MBC Minimum bactericidal concentration
MIC of 8 g/disk and an MBC of 63 g/disk. Generally the plant extracts showed both bacteriostatic and bactericidal activities as compared to their effects on C. glutamicum. The values of the MBCs of the plant extracts in both species were less than that of the drug rifampicin. The effect of combining rifampicin and plant extracts on growth inhibition Plant extract and rifampicin were combined and the effects assessed on the growth of the bacteria. The concentration 601
of the rifampicin was varied while that of the plant extract was maintained constant and vice-versa. Typical results are shown in Figure 1 for the combination of the extract from X. stuhlmannii and rifampicin. There was a gradual increase in rifampicin in the zone of inhibition with increase in concentration of rifampicin. When rifampicin, and the ethanol plant extract (maintained constant) were combined there was a decrease in the zone of inhibition as compared to rifampicin alone. The zone of inhibition obtained when
Figure 1. The effects of combining rifampicin and the extract from X. stuhlmannii on the growth of M. aurum. Rifampicin and the extract were kept constant (A/C) or varied (B/D). The combined effects of the drug and extract were assessed on the growth inhibition. Data are the mean + SD for n=4. ** Values differ significantly (P<0.01)
Table 3. The effects of combining the plant extract and rifampicin on growth inhibition Plant extract Parinari curatellifolia Xerroderris stuhlmannii Lippia javanica Ziziphus mucronata Test organism M. aurum M. aurum C. glutamicum C. glutamicum Effects of combining extract + rifampicin Antagonism Antagonism No effect Antagonism
Antagonistic A plant extract acting against rifampicin by decreasing its potency No effect A plant extract not showing a significant change in the activity of rifampicin
the ethanol extract of X. stuhlmannii and rifampicin (maintained constant) combined showed an increase in zone of inhibition but lower than when rifampicin was used on its own. Xerroderris stuhlmannii was, 602
thus, decreasing the potency of rifampicin and, hence, the lower zone of inhibition. Generally these results showed an antagonistic activity between the plant extracts and rifampicin (Table 3).
Ciprofloxacin accumulation assay Overexpression of ATP binding cassette (ABC) transporters has been proposed as a major mechanism contributing to the innate drug resistance in M. tuberculosis and related Mycobabcteria (Jiang et al., 2008). The aim of this part of the study was, therefore, to determine the effects of three most potent antimycobacterial extracts screened by disk diffusion assay, on the ATP mediated-drug efflux of the bacteria species. Bacterial cells were exposed to the plant extract, reserpine, glucose and buffer as shown in Figures 2 and 3. The fluorescence of the ciprofloxacin accumulated was then quantified. The extract from Parinari curatellifolia had the highest drug efflux pump inhibitory effect against both C. glutamicum and M. aurum . Vernonia adoensis and Faurea saligna leaf extracts also inhibited the action of the efflux pumps. The cells exposed to glucose showed a high amount of ciprofloxacin efflux compared to those without as glucose provides the ATP needed to drive the efflux pumps.
To rule out interference due to the plant extracts, their fluorescence was determined separately at the same wavelengths and the results are shown in Figure 4. All the plant extracts at the same concentration as reserpine did not fluoresce at the excitation and emission wavelengths. The fluorescence by reserpine was not significant as compared to the fluorescence of ciprofloxacin as this compound was added at a concentration of 61 ng/ml whilst ciprofloxacin was at 20 mg/L.
DISCUSSION Natural products continue to play a role in the drug discovery and development process, and plants are recognized as a very useful source of highly active antimycobacterial metabolites (McGaw et al ., 2008b). Approximately 75% of the Worlds population relies on medicinal plants as their primary source of medicine (Chigora et al., 2007; Gonzalez-Santiago et
Figure 2. The effects of the plant extracts on the accumulation and efflux of ciprofloxacin in M. aurum . Cells were loaded with ciprofloxacin and then incubated with the plant extract. The accumulation (A) was measured by determining the fluorescence of ciprofloxacin in the lysed cells. The efflux (B) was determined from the amount of ciprofloxacin in the supernatant of cells before lysis. Experiments were performed in duplicate and each measurement was done twice. Values differ significantly (**P<0.01;*P<0.05). All values are compared to the value of the sample with glucose
603
Figure 3. The effects of the plant extracts on the accumulation and efflux of ciprofloxacin from C. glutamicum. Cells were loaded with ciprofloxacin and then incubated with the plant extract. The accumulation (A) was measured by determining the fluorescence of ciprofloxacin in the lysed cells. The efflux (B) was determined from the amount of ciprofloxacin in the supernatant of cells before lysis. Experiments were performed in duplicate and each measurement was done twice. Values differ significantly (**P<0.01;*P<0.05). All values are compared to the value of the sample with glucose
Figure 4. Baseline fluorescence of the plant extracts. Fluorescence of each extract, at 61 ng/ml, the same concentration as that of the standard inhibitor reserpine, was determined at 254 nm emission wavelength 270 nm excitation wavelength
604
al., 2008). Plants with antimycobacterial activity are being studied resulting in the isolation and characterization of several bioactive compounds. Plant species still serve as sources of many novel biologically active compounds, as very few plants have been thoroughly investigated for their medicinal properties (Jachak et al., 2007). There has been a renewed interest in plants as source of novel therapeutics the past decade and, hence, many plants are being investigated for their pharmacological effect. The present study shows that 11 ethanol plant extracts had antimycobacterial effects as determined from the effects of the positive control, rifampicin and, therefore, may have potential use as antimycobacterial agents (Table 2). Corynebacterium glutamicum was less sensitive to plant extracts than M. aurum. This may be due to the differences in their structure mainly the length of the mycolic acids. Corynebacterium glutamicum has a highly ordered outer mycolic acid layer which has low fluidity and permeability which plays a crucial role in the flux of solutes (Eggeling et al., 2001). Alteration in this layer may lead to an increase in efflux rendering the plant extracts inactive. Mycobacterium aurum is a species of saprophytic, rapidly growing, non-pathogenic mycobacteria. Mycobacterium aurum is used as a test organism in the initial primary screening process of plant extracts and has a similar drug sensitivity profile to M. tuberculosis (Newton et al., 2001). The extract from V. adoensis was a potent inhibitor of growth in M. aurum with inhibitory effects rifampicin equivalent to 80 g of rifampicin (MIC-31 g/disk). Similar effects were also observed in C. glutamicum. V. adoensis leaves are used in the treatment of symptoms associated with TB in Tanzania. The family Asteracea to which V. adoensis belongs stands out in medicinal plant inventories with large numbers of medicinal species (Tabuti et al. , 2010). The popularity of Asteracea is thought to be due to the large diversity of bioactive components 605
members of this family possess. Vernonia adoensis has been found to have high levels of sequiterpene lactones which correlate with a high anti-proliferative activity (Fouche et al., 2009). In a study by Kisangau et al. (2007) the crude extract of V. adoensis had the highest activity against Escherichia coli with an activity index (AI) of 1.76. The extract from the leaves and stems of P. curatellifolia showed a considerable amount of activity against C. glutamicum. Both the leaves and the stems of P. curatellifolia are used traditionally in the treatment of symptoms associated with TB (Chigora et al., 2007). This could be the basis for its ethnobotanical use in the treatment of symptoms associated with TB in Zimbabwe. Parinari curatellifolia is also used to treat malaria, wounds, typhoid, fever and has been reported to have antiplasmodic effects (Audu & Amupitan, 2006). Extracts from Parinari curatellifolia have been found to have moderate anti-proliferative activity against breast cancer cell lines. The high levels of ent-kaurene terpenoids that have been isolated from the leaves of P. curatellifolia may be responsible for this property (Rundle et al ., 2001). Parinari curatellifolia was found to have antimicrobial effect against Staphylococcus aureus, Corynebacterium ulceran, E. coli, Salmonella typhi and Candida albicans (Audu & Amupitan, 2006). Mangifera indica stems and twigs extracts were the most potent inhibitor of growth using C. glutamicum . Based on ethnopharmacological knowledge, a standard aqueous extract of M. indica stem was shown to have anti-oxidant, antiinflammatory, and immunomodulatory properties (Wauthoz et al., 2007) and was proposed to improve the quality of life in AIDS, cancer and asthma patients. Gallotannins isolated from M. indica have been shown to have antimicrobial activity (Schieber et al ., 2009). Leaf extracts of M. indica have been shown to have antibacterial activity against Staphylococcus aureus, Escerichia coli and Pseudomonas aeruginosa (Bbosa et al ., 2007). The activity of M. indica against Clostridium
tetani has been investigated and it has been shown that ethanolic extracts contained alkaloids, tannins, triterpenoids and these compounds could have antimycobacterial activity in the case of our study. Lippia javanica extract had the lowest MIC of 31.25 g/disk when using C. glutamicum. Several plants that belong to the same genus have been found to possess antimycobacterial activity. These include Lippia origanoides and Lippia alba (Bueno-Sanchez et al., 2009). However, V. adoensis which was expected to show the lowest MIC, based on growth inhibition zones, ranked third with an MIC of 250 g/ disk and its MBC was greater than 500 g/ disk. This may be because its antimycobacterial activity exerts itself at high concentrations of the plant extract as the zone of inhibition was determined at a concentration of 500 g/disk. Syzygium guineense showed considerable activity in the agar disk diffusion assay. Djoukeng et al . (2005) found ten triterpenes in Syzygium guineense that had antibacterial activity against gram positive and gram negative bacteria and human pathogen bacteria. Triterpenes may also be responsible for the antimycobacterial activity observed in these studies. The possibility of multiple plant secondary metabolites working together has to be taken into account when evaluating for biological activity of botanical and ethnobotanical preparations (Wang et al ., 2003). The mode of action of combination differs significantly than that of the same drugs acting individually; hence isolating a single component may make the plant extract lose its potency (Hemaiswarya et al ., 2008). It has been shown that Emblica officinalis fractions prevent rifampicin, isoniazid and pyrizanamide induced toxicity (Tasduq et al., 2005). All the plant extracts examined in this study did not show any synergistic activity with the standard drug rifampicin. This may be because the plant extracts consists of different compounds which interact differently with rifampicin at the target site. Rifampicin inhibits bacterial 606
RNA synthesis by binding to the - subunit of bacterial DNA-dependent RNA polymerase. The compounds in the plant extract may have altered the drug target for rifampicin rendering it inactive or altered the transport of rifampicin to the target site. Efflux pumps can cause multi-drug resistance and have recently received a lot of interest as promising new targets in antimicrobial therapy (Lechner et al ., 2008). In Mycobacterium smegmatis , the isoflavone biochanin A, a phenolic compound, exhibited efflux pump inhibiting activity for ethidiun bromide comparable to the effects of the standard efflux inhibitor verapamil. Ciprofloxacin is a fluoroquinolone that targets DNA gyrase (topoisomerase II) and, therefore, stabilizes the complex between DNA and DNA gyrase (Walker, 1999). It was used in this study to assess the effects of the plant extracts on the drug efflux pumping activity of ATPbinding cassette transporter proteins in the two mycobacterial species. The extract from P. curatellifolia made the bacteria accumulate a higher concentration of ciprofloxacin in comparison with the other plant extracts and that of reserpine, a known efflux pump inhibitor (Figure 3). These results suggest that inhibition of efflux pumps could be a mechanism for P. curatellifolia in its role as an antimycobacterial agent. The effects observed in vitro may differ from those effects observed in vivo (Houghton et al ., 2007). The lack of activity in vivo may be impracticable to extrapolate the dose from that activity in vitro, which will be required in equivalence for the size of a human adult. Metabolism and adsorption may lead to discrepencies as in vivo, there are enzymes which may bioconvert the active compound to an inactive compound that may have no effect on the target. Further tests need to be carried out of the effect of the plant extracts on M. tuberculosis to test the efficacy of the plant species with the pathogenic form of mycobacteria. The results in this study provide leads for plant extracts that may be developed into antimycobacterial agents. Water is the
common solvent used to extract active compounds from plant sources. Dried plants can be ingested as teas or, rarely, tinctures, or inhaled via steam from boiling suspensions of the parts. Since nearly all of the identified components from plants active against microorganisms are aromatic or saturated organic compounds, they are most often obtained through ethanol and water extraction. The study tried to mimick traditional medicine by using absolute ethanol which has similar polarities to the traditional solvent water and, therefore, expected to extract similar compounds. Although, water could have been used in the study, ethanol was used instead as it is quicker to extract and this solvent reduces microbial contamination. The plant extracts in this study are not only able to inhibit mycobacterial growth but are also able to enhance the accumulation of drugs inside the bacteria. This activity may contribute to the suppression of drug resistance to the existing antimycobacterials. Therefore, the antimycobacterial activity of these plants may be due to direct effects on growth as well as indirect effects due to inhibition of efflux of compounds from these cells. These results also indicate the potential of plants used by traditional healers in Zimbabwe as a source of possible bioactive compounds. Further investigations on isolation and characterization of antimycobacterial bioactive agents from these plants are in progress. In conclusion, the extracts from P. curatellifolia showed the greatest antibacterial activity through both inhibition of growth and inhibition of drug efflux in M. aurum and C. glutamicum. The active plant extracts were found to be bacteriostatic rather than bactericidal and showed antagonism with rifampicin. This plant may serve as a source of lead compounds in the search of new antimycobacterials. Acknowledgements. The authors wish to acknowledge the support of this study by the Academy of Sciences for the Developing World (TWAS-RGA-05-075RGBIO/AF/AC, Trieste, Italy), International 607
Program in the Chemical Sciences (IPICS, ZIM01, Uppsala University, Sweden), and the International Foundation for Science (IFS F/3413-02, Stockholm, Sweden). We would also like to thank Mr. Christopher Chapano of the National Botanical Gardens, Harare, Zimbabwe, for the assistance of the taxonomical identification of some plant species.
REFERENCES Arun, K.M., Luke, J.A., Doris R., Cindy, W., Apoorva, B., William, R.J. Jr, Kuni, T., Lothar, E. & Gurdyal, S.B. (2008). Identification of a novel (1,6) mannopyranosyltransferase MptB from Corynebacterium glutamicum by deletion of a conserved gene, NCgl1505, affords a lipomannan- and lipoarabinomannan-deficient mutant. Molecular Microbiology 6: 15951593. Audu, T.I. & Amupitan, O.J. (2006). The bioactivity of Parinari curatellifolia. Research Journal of Biological Science 1: 6062. Baerts, M. & Lehmann, J. (1989). Guerisseurs et plantes mdicine de la region des crtes Zaire-Nil au Burundi Muse royal de LAfrique central Tervuren, Belgique. ANN.Sc. Eco 18: 214. Bamuamba, K., Gammon, D.W., Meyers, P., Dijoux-Franca M. & Scott, G. (2008). Anti-mycobacterial activity of five plant species used as traditional medicines in the Western Cape Province (South Africa). Journal of Ethnopharmacolgy 117: 385390. Bbosa, G.S., Lubega, A., Musisi, N., Kyegombe, B., Waako, P., Ogwal-Okeng, J. & Odyek, O. (2007). The activity of M. indica L. leaf extracts against the tetanus causing bacterium Clostridium tetani. African Journal of Ecology 45: 5458. Bbosa, G.S., A., Musisi, N., Kyegombe, D., Ogwal-Okeng, J., Odyek, O. & Waako, P. (2007). Antibacterial activity of Mangifera indica (L). African Journal of Ecology 45: 1316.
Bueno-Snchez, J.G., Martinez-Morales, J.R., Stancheko, E.E. & Ribn, W. (2009). Anti-tubercular activity of eleven aromatic and medicinal plants occurring in Colombia. Biomdica 29: 5160. Chigora, P., Masocha, R. & Mutenheri, F. (2007). The role of indigenous medicinal knowledge (IMK) in the treatment of ailments in rural Zimbabwe: The case of Mutirikwi Communal Lands. Journal of Sustainable Development for Africa 9: 2643. Chinemana, F., Drummond, R.B., Mavi, S. & De Zoysa, I. (1985). Indeginous plant remedies in Zimbabwe. Journal of Ethnopharmacology 14: 159172. Country TB profile for Zimbabwe. In WHO Report. (2009). De Boer, H.J., Kool, A., Broberg, A., Mziray, W.R., Herdberg, I. & Levenfors, J.J. (2004). Antifungal and antibacterial activity of some herbal remedies from Tanzania. Journal of Ethnopharmacology 96: 461469. Djoukeng, J.D., Abou-Mansour, E., Tabacchi, R., Tapondjou, H., Bouda, H. & Lonts, D. (2005). Antibacterial triterpenes from Syzygium guineense (Myrtaceae). Journal of Ethnopharmacology 101: 283286. Eggeling, L., Krumbach, K. & Sahm, H. (2001). L-Glutamate efflux with Corynebacterium glutamicum : Why is penicillin treatment or TWEEN addition doing the same? Journal of Molecular, Microbiological and Biotechnology 3: 6788. Fennell, C.W., Lindsey, K.L., McGaw, L.J., Sparg, S.G., Stafford, G.I., Elgorash, E.E., Grace, O.M. & van Staden, J. (2004). Assessing African medicinal plants for efficacy and safety: pharmacological screening and toxicology. Journal of Ethnopharmacology 94: 205217.
Fouche, G., Senabe, J., Khorombi, E., Kolesrukova, N., Moharaj, V.J. & Nthambeleni, R. (2009). High throughput screening of South African plants for anticancer properties. CISR Biosciences Journal 119: 455461. Gonzalez-Santiago, O., Garza-Gonzalez, E., Palacios, I.P., Luna-Herrera, J., Camacho-Corona, M.R. & RamirezCabrera, M.A. (2008). Activity against drug resistant-tuberculosis strains of plants used in Mexican traditional medicine to treat tuberculosis and other respiratory diseases. Phytotherapy Research 22: 8285. Hemaiswarya, S., Kruthiventi, A. & Doble, M. (2008). Synergism between natural products and antibiotics against infectious diseases. Phytomedicine 15: 639652. Higuchi, C.T., Sannomiya, M., Pavan, F.R., Vilegas, W., Leite, C.Q.F. & Sato, D.N. (2008). Antimycobacterial activity of Byrsonima crassa nied leaf extracts. Botucatu 10: 6366. Houghton, P.J., Howes, M.J., Lee, C.C. & Steventon, G. (2007). Uses and abuses of in vitro tests in ethnopharmacology: Visualizing an elephant. Journal of Ethnopharmacology 110: 391400. Jachak, S.M., Saklani, A. & Gautam, R. (2007). Indian Medicinal plants as a source of antimycobacterial agents. Journal of Ethnopharmacology 110: 200223. Jiang, X., Zhang, W., Zhang, Y., Gao, F., Lu, C., Zhang, X. & Wang, H. (2008). Assessment of efflux pump gene expression in a clinical isolate Mycobacterium tuberculosis by realtime reverse transcription PCR. Microbial Drug Resistance 14: 711. Kisangau, D.P., Hosea, K.M., Joseph, C.C. & Lyaruu, H.V.M. (2007). In vitro antimicrobial assay of plants used in traditional medicine in Bukoba rural district Tanzania. African Journal of Traditional and Complementary Alternative Medicines 4: 520523.
608
Lechner, D., Gibbons, S. & Bucar, F. (2008). Plant phenolic compounds as ethidium bromide efflux inhibitors in Mycobacterium smegmatis . Journal of Antimicrobial Chemotherapy 62: 345 348. Lewu, B.F. & Afolayan, A.J. (2009). Ethnomedicine in South Africa, The role of weedy species. African Journal of Biotechnology 8: 929934. Maliwichi, C.P. (2000). A study of medicinal plants used for maternal and child diseases in Malawi: An ethnobotanical perspective. Status report submitted to UNESCO. Mann, A., Amupitan, J.O., Oyewale, A.O., Okogun, J.I., Ibrahim, K., Oladosu, P., Lawson, I., Olajide, L. & Nnamdi, A. (2008). Evaluation of in-vitro antimycobacterial activity of Nigerian plants used for treatment of respiratory diseases. African Journal of Biotechnology 7: 16301636. McGaw, L.J., Lall, N., Meyer, J.J.M. & Eloff, J.N. (2008a). The Potential of South African plants against Mycobacterium infections. Journal of Ethnopharmacology 119: 482500. McGaw, L.J., Lall, N., Hlokwe, T.M., Michel, A.A., Meyer, J.J.M. & Eloff, J.N. (2008b). Purified compounds and extracts from Euclea species with antimycobacterial activity against Mycobacterium bovis and fast growing Mycobacteria. Biological Pharmacology Bulletin 31: 14291433. Mortimer, P.G. & Piddock, L.G. (1991). A comparison of methods used for measuring the accumulation of quinolones by Enterobacteriaceae, Psuedomonas aeruginosas and Staphylococcus aureus . Journal of Antimicrobial Chemotherapy 28: 639 653. Newton, M.S., Lau, C., Gurcha, S.S., Gurdyal, S.B. & Wright, W.C. (2001). The evaluation of forty-three plant species for in-vitro antimycobacterial activities; isolation of active constituents from Psoralea corylifolia and Sanguinaria canadensis. Journal of Ethnopharmacology 79: 5767. 609
Ruffo, C.K. (1991). A survey of medicinal plants in Tabora region, Tanzania. Journal of Traditional and Medicinal Plant 391. Rundle, N.T., Xu, L., Anderson, R.J. & Roberge, M. (2001). G 2DNA damage checkpoint inhibition and antimitotic activity of 13 hydroxy-15-oxozoapatlin. Journal of Biological Chemistry 45: 160164. Sarada, S., Sreekandan, G. & Reghunath, B.R. (2002). Qantification of medicinally valuable weeds in oil palm plantation of Kerala. Journal of Tropical Agriculture 40: 1926. Schieber, A., Engels, C., Gnzle, M.G., Carle, R., Engels, C., Kndler, M. & Zhao, Y.Y. (2009). Antimicrobial activity of gallotannins isolated from mango ( Mangiferin indica L.) kernels. Journal of Agricultural Food Chemistry 57: 77087712. Starvri, M., Piddock, J.V.L. & Gibbons, S. (2007). Bacterial efflux pumps from natural sources. Journal of Antimicrobial Chemotherapy 59 : 1247 1260. Suresh, K., Babu, S.S. & Harisaranraj, R. (2008). Studies on in vitro antimicrobial activity of ethanol extract of Rauvolfia tetraphylla. Ethnobotanical Leaflets 12: 58690. Tabuti, J.R.S., Kukunda, C.B. & Waako, P.J. (2010). Medicinal practitioners in the treatment of tuberculosis and related ailments in Uganda. Journal of Ethnopharmacology 127: 130136. Tasduq, S.A., Kaisar, P., Gupta, D.K., Kapahi, B.K., Jyotsna, S., Mahashwari, H.S. & Johri, R.K. (2005). Protective effects of a 50% hydroalcoholic fruit extract of Emblica officinalis against antituberculosis drugs induced liver toxicity. Phytotherapy Research 19 : 193197. Walker, R.C. (1999). The flouroquinolones. Symposium on antimicrobial agents Part XIII. Mayo Foundation for Medical Education and Research 74 : 1030 1037.
Wang, N., Yao, X., Ishii, R. & Kitanaka, S. (2003). Bioactive sucrose esters from Bidens parviflora. Phytochemistry 62: 741746. Wauthoz, N., Balde, A., Balde, E.S., Van Damme, M. & Duez, P. (2007). Ethnopharmacology of Mangifera indica L. bark and pharmacological studies of its main C-glucosylxanthone, magiferin. International Journal of Biomedical and Pharmaceutical Sciences 1 (2) 112119.
Woods-Panzaru, S., Nelson, D., McCollum, G., Ballard, L.M., Millar, B.C., Maeda, Y., Goldsmith, C.E., Rooney, P. J., Loughrey, A., Rao, J.R. & Moore, J.E. (2009). An examination of antibacterial and antifungal properties of constituents described in traditional Ulster cures and remedies. Ulster Medicinal Journal 78: 1315. Zaidan, M.R.S., Noor Rain, A., Badrul, A.R., Adlin, A., Norazah, A. & Zakia, I. (2005). In vitro screening of five local medicinal plants for antibacterial activity using disc diffusion method. Tropical Biomedicine 22: 165170.
610
You might also like
- Dermatosa Vesiko BulosaDocument14 pagesDermatosa Vesiko BulosaSyahrul Hamidi NasutionNo ratings yet
- DM Hiperestesia 4 PDFDocument6 pagesDM Hiperestesia 4 PDFSyahrul Hamidi NasutionNo ratings yet
- Nutrition, Diabetes and Tuberculosis in The Epidemiological TransitionDocument7 pagesNutrition, Diabetes and Tuberculosis in The Epidemiological TransitionSyahrul Hamidi NasutionNo ratings yet
- EvaluationDocument7 pagesEvaluationSyahrul Hamidi NasutionNo ratings yet
- Relationship Between Computed Tomography Findings and Nutritional Status in Elderly Patients With Pulmonary TuberculosisDocument6 pagesRelationship Between Computed Tomography Findings and Nutritional Status in Elderly Patients With Pulmonary TuberculosisSyahrul Hamidi NasutionNo ratings yet
- NIH Public Access: Author ManuscriptDocument10 pagesNIH Public Access: Author ManuscriptSyahrul Hamidi NasutionNo ratings yet
- Research Paper: ISSN 0189-6016©2009Document6 pagesResearch Paper: ISSN 0189-6016©2009Syahrul Hamidi NasutionNo ratings yet
- AJTCAM0701 0079jkjlkDocument6 pagesAJTCAM0701 0079jkjlkSyahrul Hamidi NasutionNo ratings yet
- AFHS0901 0040lkDocument6 pagesAFHS0901 0040lkSyahrul Hamidi NasutionNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- TRS - 2003.full - Crocodyliform Biogeography During The CretaceousDocument7 pagesTRS - 2003.full - Crocodyliform Biogeography During The CretaceousKanekoNo ratings yet
- Antibody Responses To Minor Histocompatibility Antigens After Solid Organ TransplantationDocument5 pagesAntibody Responses To Minor Histocompatibility Antigens After Solid Organ TransplantationBruna VoroniukNo ratings yet
- Hsslive XI Zoology 05 Digestion and AsorptionDocument15 pagesHsslive XI Zoology 05 Digestion and AsorptionbnairNo ratings yet
- Eoc Biology Rview Packet 2012-2013Document48 pagesEoc Biology Rview Packet 2012-2013api-282682755No ratings yet
- Certificate of Analysis No.: 1927745: CustomerDocument2 pagesCertificate of Analysis No.: 1927745: CustomerDimitris KNo ratings yet
- Revista - BJSM - Price Vs Police. PRICE Needs Updating, Should We Call The POLICE?Document3 pagesRevista - BJSM - Price Vs Police. PRICE Needs Updating, Should We Call The POLICE?Giancarlo Gardella MartínezNo ratings yet
- Irjet V9i1124Document5 pagesIrjet V9i1124BALAJINo ratings yet
- An Introduction To: The Respiratory SystemDocument22 pagesAn Introduction To: The Respiratory SystemSHANJIDA ALI RIANo ratings yet
- Personality DevelopmentDocument25 pagesPersonality DevelopmentmonishaNo ratings yet
- (Gardner) - (Snustad) Kontrol Genetik Respon ImunDocument21 pages(Gardner) - (Snustad) Kontrol Genetik Respon ImunFAUZI IBNUNo ratings yet
- Management of Diabetic KetoacidosisDocument4 pagesManagement of Diabetic Ketoacidosiscarla jazmin cortes rodriguezNo ratings yet
- Executive Summary: Intended Goals of SequencingDocument1 pageExecutive Summary: Intended Goals of SequencingBrahim JabbaneNo ratings yet
- IFAP Matrice D Import TAXO I Fap V12 31082020Document1,426 pagesIFAP Matrice D Import TAXO I Fap V12 31082020jamiNo ratings yet
- Food Enzymology: FD-206 Spring Semester 2021 Second Year Food EngineeringDocument25 pagesFood Enzymology: FD-206 Spring Semester 2021 Second Year Food EngineeringSahar Batool QaziNo ratings yet
- H O P E - 2-Module-2Document12 pagesH O P E - 2-Module-2kmpguarin.tshsNo ratings yet
- Allergic ConjunctivitisDocument16 pagesAllergic ConjunctivitisJose Antonio Fuentes VegaNo ratings yet
- B001 Arihant PDFDocument12 pagesB001 Arihant PDFmathclubNo ratings yet
- Qdoc - Tips Topnotch Supplement Pharmacology HandoutDocument57 pagesQdoc - Tips Topnotch Supplement Pharmacology HandoutShehana MusahariNo ratings yet
- Minerals Engineering: E.T. Pecina, L.F. Camacho, C.A. Herrera, D. MartínezDocument3 pagesMinerals Engineering: E.T. Pecina, L.F. Camacho, C.A. Herrera, D. MartínezMohsin ALiNo ratings yet
- Practice Prelim 3 Answer KeyDocument10 pagesPractice Prelim 3 Answer KeyEricaNo ratings yet
- QUS 104 Building ScienceDocument70 pagesQUS 104 Building ScienceOlagoke Habeeb Ademola100% (3)
- Old Earth History Book 1 - 5 Million To 750 B.C. - The AnnunakiDocument218 pagesOld Earth History Book 1 - 5 Million To 750 B.C. - The Annunaki123jump100% (11)
- Dissolved Oxygen and Aquatic Productivity LabDocument6 pagesDissolved Oxygen and Aquatic Productivity Labapi-235548856No ratings yet
- HemosIL APTT Brochure Rev2 May 07 PDFDocument4 pagesHemosIL APTT Brochure Rev2 May 07 PDFKath ONo ratings yet
- Pinus Roxburghii - WikipediaDocument16 pagesPinus Roxburghii - WikipediaGener Habala NavarroNo ratings yet
- Fusion Diagnostics Lingad, Joselito Bohots: Sars-Cov-2 PCRDocument2 pagesFusion Diagnostics Lingad, Joselito Bohots: Sars-Cov-2 PCRjb lingadNo ratings yet
- Double CirculationDocument2 pagesDouble CirculationMonika KanojiaNo ratings yet
- 5 Paragraph Essay: Genetically Modified FoodDocument5 pages5 Paragraph Essay: Genetically Modified FoodAwais AliNo ratings yet
- Soal TOEIC Listening Ricky Dwi Agustyas (17020230056)Document9 pagesSoal TOEIC Listening Ricky Dwi Agustyas (17020230056)dwyas rickNo ratings yet