Professional Documents
Culture Documents
Bruximo PDF
Uploaded by
cemoaraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bruximo PDF
Uploaded by
cemoaraCopyright:
Available Formats
Fall 2013 Volume 84, Number 4
Inside:
New Jerseys Own Maxine Feinberg
to Head American Dental Association
Facial Pain of Non-Odontogenic Origin
New Jersey Dental Establishments
in 2011: After the Last Recession
The Crowd Pleaser.
Nearly one-third of patients with dental benefits are covered by Delta Dental.
Over 54 million Americans rely on the dentists in the national Delta Dental system. If youre already
participating in Delta Dental Premier
, why not join another network to have more exposure to new
patients? If you do not participate with Delta Dental, why not join the crowd? We think youll be pleased.
Delta Dental. Theres safety in our numbers. To participate with Delta Dental of New Jersey, call
1-888-396-6641 or visit www.deltadentalnj.com.
DDI-1045 NJDA Crowd 7x10_DDI-1045 NJDA Crowd 7x10 9/14/11 12:35 PM Page 1
American Practice Consultants, a full service Dental Practice Broker
& Appraiser, was founded in 1985 by Philip A. Cooper, D.M.D.,
M.B.A. to provide a range of transition services to dentists who are
selling or buying a practice.
Let Us Expertly
Guide You Through:
VALUATION MARKETING
NEGOTIATION CONTRACT REVIEW
FINANCING MINIMIZING TAXES
TRANSITION PLANNING WITH PATIENTS & STAFF
AND SO MUCH MORE!
Philip A. Cooper, D.M.D., M.B.A.
Ask
About Our
FREE GUIDES
For Sellers
& Buyers!
DENTAL
PRACTICE
SALES
Want to Know More? We Can Guide You.
www.ameriprac.com
704 East Main Street, Suite D Moorestown, New Jersey 08057
856-234-3536 800-400-8550 cooper@ameriprac.com
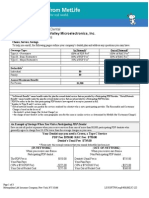
New Jersey Dental Association and Mid-Atlantic Insurance Resources proudly
endorse Meadowbrook Insurance Group for your Workers Compensation
Insurance needs.
Choosing the right Workers Compensation insurance provider makes all the difference.
We can assist you with the steps needed to protect you and your employees.
Insurance. Protection. Save. Smile.
For more information about this
program, please contact us at:
P: 877.476.4588
F: 717.234.4163
www.midatlanticir.com
7%
workers compensation
dividend paid in 2011 to
NJDA members that met
eligibility requirements.
Endorsed Provider of
Editor
Harvey S. Nisselson, DDS, FACD, FICD
17 Alpine Drive
Denville, NJ 07834
hn3@columbia.edu
Managing Editor
Lorraine Sedor
lsedor@njda.org
Business Manager
Arthur Meisel, Esq.
ameisel@njda.org
Publication Manager
Mastergraphx
NJDA 20132014 Officers
President, Robert A. Giantomas, DMD
President-Elect, Bryon E. Roshong, DMD
Vice President, Gregory LaMorte, DDS
Treasurer, Giorgio DiVincenzo, DMD
Secretary, Mark A. Vitale, DMD
Speaker, House of Delegates, Walter I. Chinoy, DMD
Editor, Harvey S. Nisselson, DDS
Immediate Past President, Michael M. Messana, DMD
Executive Director, Arthur Meisel, Esq.
NJDA 20132014 Board Of Trustees
Atlantic-Cape May, OPEN
Bergen, Priya Gupta, DDS
Central, Joseph R. Krulewicz, DMD
Essex, Thomas A. Rossi, DMD
Hudson, Luciano A. Ghisalberti, DMD
Mercer, Fred P. Babinowich, DMD
Middlesex, Mitchell L. Weiner, DMD
Monmouth-Ocean, Dipika T. Shah, DDS
NJ Student Dental, Meha Sheth
Passaic, Teresa Michaud, DDS
Southern, Paul J. Lawyer, DMD
Tri-County, Alan Rothstein, DMD
Union, Barry R. Wolinksy, DDS
Professional Staff
Patricia DeCotiis, Esq.
Assistant Executive Director/Director of Membership
Mary B. Moskal
Director of Dental Care Programs
James J. Schulz, Jr.
Director of Governmental Affairs
Maureen Barlow
Director of Meetings & Events
Stanley Orenstein
Business Manager
Nicole Fredrickson
Marketing Communications Manager
The New Jersey Dental Association
is proud to partner with
Mastergraphx
to provide the community with a journal printed
on environmentally-friendly paper. By using
products with the FSC label you are supporting the
growth of responsible forest management worldwide.
Volume 84, Number 4
Member Publication
American Association of Dental Editors
Journal of the New Jersey Dental Association (ISSN
0093-7347, USPS No. 104-650) is published quarterly
by the New Jersey Dental Association. Periodical
postage paid at North Brunswick, NJ and additional
mailing offices. All views expressed herein are published
on the authority of the writer under whose name
they appear and are not regarded as the views of the
Association. We reserve the right to reduce, revise,
or reject any manuscript submitted for publication.
Copy for publication should be addressed to: Dr.
Nisselson. Business communications and address
changes should be addressed to: One Dental Plaza,
P.O. Box 6020, North Brunswick, NJ 08902-6020,
(732-821-9400). Materials may be reproduced without
written permission. Subscription rate for members
is $20 which is included in the dues; $60 per year
for non-members and $100 for foreign subscribers.
Single copies are $5 per issue. Periodicals postage paid
at New Brunswick, NJ. The Association, in its sole
discretion, has the absolute right to accept, reject, and /
or cancel any advertisement for any reason whatsoever.
POSTMASTERsend address changes to: Journal of
the New Jersey Dental Association, One Dental Plaza,
PO Box 6020, North Brunswick, NJ 08902-6020.
Advertisers
AFTCO 7
American Academy of Facial Esthetics 24
American Practice Consultants 1
Anesthesia for Dentistry 8
B.C. Szerlip Insurance Agency Inc. 38
Botwinick & Co. 4
Te Bronx County Dental Society 18
Te Clemens Group 31
Delta Dental Plan of New Jersey, Inc. IFC
Dental Dreams 17
Te Dentists Insurance Company OBC
Eastern Dental Society IBC
Eastern Dentists Insurance Company 5
Great Expressions Dental Centers 20
Te Insurance Agency for Dentists, LLC 32
Meadowbrook Insurance Group 2
Mid-Atlantic Insurance Resources 35
NJ School of Dental Assisting 23
Paragon Dental Practice Transitions 39
PNC Bank 19
RMN Consultants 13
Rutgers School of Dental Medicine 40
Te Snyder Group 15
Temple University Kornberg School of Dentistry 37
Mastergraphx 11
Valley Forge Dental Conference 33
Cover
Delaware Water Gap National Recreation Area
The New Jersey Dental Association serves and
supports its members and fosters the advancement of
quality, ethical oral healthcare for the public.
Mission Statement:
Departments
4 From Your President
6 Reflections
6 In Memoriam
8 Executive Directors Desk
10 Members in the News
20 Oral Pathology Quiz #81
24 Oral Pathology Quiz Answers #81
37 Classifieds
Articles
9 New Jerseys Own Maxine Feinberg to Head American Dental Association
12 3 Major Obstacles to Going Chartless; and How to Get Around Them!
14 Effects of Smoking on Implant FailureA Review
16 Facial Pain of Non-Odontogenic Origin
22 NJDA Annual Golf Outing Recap
23 Opinion: The Economics of Healthcare and its Implication for Dentistry
26 Five Things to Know About Bruxism
27 Preprocedural Rinsing in the Dental Office: A Consideration for Improved
Infection Control Among the Dental Team and Patients
32 New Jersey Dental Establishments in 2011: After the Last Recession
36 Opinion: New Kid on the Block
3 Volume 84, Number 4
From Your President
Robert A. Giantomas, DMD
W
e all know about our tripartite membership, but there is
a fourth part that is often overlookedthe New Jersey
Dental Political Action Committee (NJDPAC).
NJDPAC is a committee run by dentists that raises money to support
candidates that support our positionnot a party, but our profession. This
is a call to action; I am writing this because we need you to join. Less than
one in three NJDA members belong to NJDPAC. It has been the number
one health PAC in the state for five years but our numbers are dropping.
NJDPAC lets us forge relationships with legislators that drive our agenda
forward, be it stopping mid-level providers, or advancing the assignment
of benefits law. All legislators are important, regardless of whether you
like them personally. NJDPAC affords you the opportunity to avoid
partisan politics, and make it all about the politics of your profession.
Campaigns are expensive, and legislators need to communicate a
message to get reelected. NJDPAC allows us to demonstrate value to
politicians in their time of need. The strength of our PAC distinguishes
NJDA as a leader and a friend against the insurers, attorneys,
environmentalists, and others who seek to change how dentistry is
practiced in New Jersey. It allows us to change our own destiny.
For more information or to join, contact me at rgiantomas@njda.org.
Botwinick & Company, LLC
Certied Public Accountants
Serving NJ Dentists Since 1968
Sherbrooke Offce Center II 201 West Passaic St., Rochelle Park, NJ 07662
T (201) 909.0090 F (201) 909.8533 www.botwinick.com
Isnt it about time YOU had something to smile about?
When i t comes to sel ecting an accounting firm for your
practi ce, why not fol l ow the l ead from your peers.
Botwinick & Company, LLC has been serving the accounting
needs of New Jersey dentists since 1968. With a frm wide
concentrati on i n dental practi ce accounti ng, practi ce
management, and acquisition consulting, we are the most
trusted dental accounting firm in the Metropolitian Area.
What sets us apart from other frms is the partners hands
on approach to your accounting, tax and management
consul ti ng needs. One on one attenti on from your
accountant i s guaranteed.
We encourage you to set up a complimentary meeting with
one of our partners. Let us show you how you should be
treated by your most trusted advisor.
Volume 84, Number 4 4
ENDORSED BY ENDORSED BY
RHODE ISLAND
DENTAL
ASSOCIATION
ENDORSED BY
NORTH CAROLINA
DENTAL SOCIETY
1-800-898-3342 www.edic.com
EASTERN DENTISTS INSURANCE COMPANY
Malpractice Insurance | By Dentists, For Dentists
YOUR COLLEAGUES! EDICs Board of Directors is
comprised of dentists and dental educators. We have a network of national experts
and the best defense counsel at your disposal at any given time. We will go to the wall
to defend you, your reputation, and stand by your side when you need us the most.
At EDIC, we only insure our colleagues which means you and your claim is our
top priority.
For over 20 years, EDIC has been committed to dentistry and its colleagues. As a
mutual-owned company we give back to our colleagues, our dental societies, and
our dental schools. Our 99% customer retention rate proves we are committed to our
dental community indefinitely.
Join the By Dentists, For Dentists
company for all your dental malpractice insurance
needs, and you can be sure EDIC will always stand by your side.
WHEN YOU GET A CLAIM,
WHO WILL DEFEND YOU THE BEST?
EDIC BOARD OF DIRECTORS 2013 - 2014
P
ower tends to corrupt, said Lord Acton, the
19
th
century historian. Absolute power corrupts
absolutely. This maxim has been vividly illustrated
in psychological studies, notably the 1971 Stanford Prison
Experiment, which was halted when one group of students
arbitrarily assigned as prison guards over another group began
to abuse their wards.
But new scholarship is bringing fresh subtlety to psychologists
understanding of when power leads people to take ethical shortcuts
and when it doesnt. Indeed, for some people, power seems
to bring out their best. After all, good people do win elective
office, says Katherine DeCelles, a professor of management at the
University of Toronto, and no few business executives want to
do good while doing well. When you give good people power,
DeCelles says she wondered, are they more able than others to
enact that moral identity, to do whats right?
In a study recently published in the Journal of Applied Psychology,
DeCelles and her co-authors found that the answer is yes. Peoples
sense of moral identitythe degree to which they thought it was
important to their sense of self to be caring, compassionate, fair,
generous and so onshaped their responses to feelings of power.
DeCelles and her colleagues developed moral identity scores for two
groups, 173 working adults and 102 undergraduates, by asking the
participants to rate how important those ethically-related attributes
were to them. The researchers had some participants write an essay
recalling an incident in which they felt powerful, while others
wrote about an ordinary day. Then the participants took part in lab
experiments to probe how they balanced self-interest against the
common good.
The undergraduates were told they shared a pool of 500
points with other people, and they could take between zero
and ten points for themselves. The more points they took,
the better their odds of winning a $100 lottery. But if they
took too manythere was no way of knowing what that
tipping point wasthe pot would empty and the lottery
would be called off.
The participants who had just written about an ordinary day each
took roughly 6.5 points, regardless of their moral identity score.
But among those who had been primed to think of themselves
as powerful, the people with low moral identity scores grabbed
7.5 pointsand those with high moral identity scores took only
about 5.5.
In surveys, the last group showed a greater understanding of
how their actions would affect other people, which is the crucial
mechanism, DeCelles says. Power led them to take a broader, more
communally centered perspective.
The experiment involving the adults found a similar relationship
between moral identity, ethical behavior and innate aggressiveness.
Assertive people who scored low on the moral identity score were
more likely to say theyd cheated their employer in the past week
than more passive types with similar moral identity scores. But
among those with high moral identity scores, the assertive people
were less likely to have cheated.
In sum, the study found power doesnt corrupt; it heightens
pre-existing ethical tendencies. Which brings to mind another
maxim, from Abraham Lincoln: Nearly all men can stand
adversity, but if you want to test a mans character, give
him power.
Reflections
Power
Harvey S. Nisselson, DDS, FACD, FICD
In
Memoriam
Monmouth-Ocean
Gerald S. Gildenberg September 15, 2013
Lloyd L. Vaccarelli August 14, 2013
Southern
Norman F. Sengin August 24, 2013
We note with sadness the passing of the
following members:
Volume 84, Number 4 6
Call 1-800-232-3826 today for a
free practice appraisal,
a $2,500 value!
AFTCO is the oldest and largest dental practice transition
consulting firm in the United States. AFTCO assists dentists
with associateships, purchasing and selling of practices, and
retirement plans. We are there to serve you through all
stages of your career.
Helping dentists buy & sell practices for over 40 years.
WWW.AFTCO.NET
Paul M. Goodman, D.M.D., Jeffrey M. Goodman, D.M.D., &
David H. Goodman, D.D.S. have acquired the practice of
Richard M. Friedman, D.D.S. - Lawrenceville, New Jersey
Richard Goldberg, D.M.D. has acquired the practice from the estate of
Michael I. Verona, D.D.S. - Monroe Township, New Jersey
Madalina-Elena Iorgulescu, D.M.D. has acquired the practice of
Jane Giordano, D.M.D. - Morristown, New Jersey
AFTCO is pleased to have represented
all parties in these transactions.
I
f you receive a complaint from the New Jersey State Board of
Dentistry, dont panic. Typically, between five hundred and
eight hundred complaints are received by the State Board
each year.
Under the review procedure established by the State Board,
most complaints from patients are forwarded to the affected
dentists together with a request to produce records and
to submit a responsive narrative statement. While the
correspondence has the appearance of being personally written,
actually it is a form letter. In some instances, the State Board
will initiate an investigative inquiry, which is analogous to
a deposition.
Upon receiving either a complaint or a notice of an investigative
inquiry, NJDA members are encouraged to contact the
Association. As a service to members only, at no charge,
lawyers with State Board experience will assist members in
assessing the seriousness of the complaint and in fashioning a
written response.
The tone, content and length of a responsive narrative
statement are always important. Depending upon how a
narrative statement is written, it can create unnecessary
problems or it can hasten a favorable outcome. In more serious
matters, where it appears that individual representation is
necessary, like when a dentist is summoned for an investigative
inquiry or when a formal suspension or revocation proceeding is
initiated, lawyers who have experience in appearing before the
State Board and who are viewed as being knowledgeable and
effective will be recommended.
Among other responsibilities, the State Board has the obligation
to protect the public. While at one time the State Board had
the reputation of being particularly antagonistic to dentists,
that generally is no longer the case. In fulfilling its important
public responsibility, the members of the State Board do
try to do the right thing in a fair-minded manner without
being punitive.
The overwhelming majority of complaints made by patients
to the State Board are predicated on disputes over money.
When such disputes arise, members are encouraged to
promptly contact the NJDA. In many instances, resolutions
can be achieved and complaints can be avoided. Patients
who feel that they have been treated fairly usually do not
file complaints.
The NJDA stands ready and anxious to assist its members by
making available legal consultation at a critical time in their
professional lives. This is a truly valuable benefit that should not
be overlooked or forgotten.
Executive Directors Desk
Arthur Meisel, Esq.
Anesthesia for Dentistry
Administered in your office
There is no fee to become a participating dentist
Glen Atlas, M.D.
Board Certified Anesthesiologist
Phone: 973-758-0758
Call for availability
www.glenatlasmd.com
Project5_Layout 1 11/13/09 12:44 PM Page 1
Volume 84, Number 4 8
A
t the American Dental Associations House of Delegates
meeting on November 4 in New Orleans, Maxine Feinberg,
DDS, was elected president-elect of the American Dental
Association. She will begin her one-year term as president in
October, 2014, succeeding Dr. Charles Norman, when the ADA
house reconvenes in San Antonio, TX.
Dr. Feinberg, a periodontist, practices in Cranford. A strong
proponent of organized dentistry, she has been an ADA member for
32 years. During that time, Dr. Feinberg served locally, at the state
level and nationally. She is a member of the Union County Dental
Society and is a past president and current member of the New
Jersey State Board of Dentistry.
Dr. Feinberg is the first woman to hold the office of president of
the NJDA (20022003), where she also was treasurer and chair of
the Finance Committee. During her term in office at NJDA, Dr.
Feinberg is credited with bringing the Give Kids a Smile campaign
to the state.
Keeping the Dentist in Dentistry
In her message to the delegates of the ADA, Maxine Feinberg noted
that her goal would be to keep the dentist in dentistry. In her
comments, she emphasized three critical issues facing the profession:
an uncertain economic future, a volatile regulatory environment,
and evolving dental education. As ADA president, Dr. Feinberg
plans to expand the ADAs role in public education and advocacy,
noting We must help states understand the Affordable Care Act
while increasing efforts to educate employers and patients on the
benefits of good oral health.
In an interview she gave to the Journal of NJDA in 2002 when
she became NJDA president, Dr. Feinberg said, because
there were few women practitioners, especially specialists, when
I started in private practice, it allowed me the freedom to define
my own success. She did say she had great role models, both
men and women, whose own commitment to the profession and
dedication to organized dentistry fueled her early involvement.
She went on to say, I hope that I can bring about the same
feelings in the young practitioners I will meet in the years to
come, an expectation she echoes today at the national level. In
her statement to the ADA delegates she said, My involvement
today is to ensure the next generation will be able to afford to go
to dental school and continue our proud tradition of improving
lives. From 20112013, Dr. Feinberg was the ADA Trustee
Liaison to the Task Force on Student Debt and chaired the task
force in 20122013.
Dr. Feinberg was ADA 4
th
District trustee at the time of the
election. The 4
th
district is comprised of New Jersey, and Delaware,
the District of Columbia, Federal Dental Services, Maryland, Puerto
Rico and the Virgin Islands. As an ADA trustee since 2009, Dr.
Feinberg served on numerous committees and chaired the Audit
Committee in 201213. She also has been a delegate to the FDI
World Dental Federation since 2009.
Dr. Feinberg is especially committed to strengthening the dentist
as the head of the dental team in all practice models. After the
election results were announced Dr. Feinberg pledged to move this
Association forward as we want to move it, not as others want to.
A 1980 graduate of New York University College of Dentistry, Dr.
Feinberg is a fellow in the American College of Dentists (2000), the
International College of Dentists (2002) and the Pierre Fauchard
Society (1998). She also maintains memberships in the American
Academy of Periodontology and the Academy of General Dentistry.
In addition to serving on the NJ State Board of Dentistry, Dr.
Feinberg has been a member of the NJ State Dental Medicaid
Advisory Committee since 2004, and a member of the North East
Regional Board of Dental Examiners. She has been a volunteer with
Donated Dental Services since 1998 and was presented with the
NJDA Give Kids a Smile Pioneer award in 2012.
Dr. Feinberg is married to John Wynne. They have two daughters,
Haley and Rebecca. The family resides in Westfield, NJ.
New Jerseys Own Feinberg
to Head American Dental Association
Former NJDA President and
ADA 4
th
District Trustee
9 Volume 84, Number 4
Welcome to the 20132014 NJDA Component
Society Presidents:
Boris Kalika, DMD, Atlantic-Cape May
Ilya Lipkin, DDS, Bergen County
Michelle Weddle, DDS, Central
Carol E. Mann, DMD, Essex County
P. David Gleaner, DMD, Hudson County
Janhavi S. Rane, DDS, Mercer County
David M. Stein, DMD, Middlesex County
Miriam T. Furlong, DMD, Monmouth-Ocean
Leslie Elfenbein, DMD, Passaic
Frank R. Batastini, DMD, Southern
Edward M. Tirpack, DMD, Tri-County
Jay L. Greenfield, DMD, Union
Meha Sheth, New Jersey Student Dental
Montclair Orthodontist Edward Gold,
DDS, has merged his passion for running
with his passion for reading. In 2012,
Dr. Gold was ready to run in the New
York City marathon for the first time.
Unfortunately, Hurricane Sandy put a
damper on that effort, but not before
he received pledges of nearly $10,000 in
support of the Montclair Public Library. Dr. Gold did make good
on his promise, running instead in the Philadelphia marathon on
November 18, 2012. This year, proceeds will go to the librarys
childrens programs. Dr. Gold explained, I knew that if I were ever
to run a marathon, that I would want to and needed to support a
cause...The Montclair Public Library, along with all public libraries
can assist in laying the foundation for learning for children that will
help our generation and future generations make contributions in
all areas of science and humanities He noted that the large sum
of money raised was realized in increments of 26.2 pennies, dimes
and dollars, contributed by Montclairs children and their parents.
When not working, running or reading, Dr. Gold represents the
specialty of orthodontics on the NJDA Peer Review Committee.
Give Kids a Smile! Save the Date.
Friday, February 7, 2014 is Give Kids a Smile
Day! Have you or your office signed up? Its
not too late! February is National Childrens
Dental Health Month. On February 7 you and
your staff can make a big difference in a childs life by accepting
patients ages 12 and younger for free screenings, sealants and/or
restorative treatment. Register at http://www.ada.org/givekidsasmile.
aspx or call the NJDA at 732-821-9400 for information. If youd
like, you can opt to volunteer at another location, such as one of
the states hygiene schools or another facility. If you are unable
to participate but would like to help, please consider making a
monetary donation to GKAS-NJ. Donations to GKAS-NJ will
be used to offset the cost of student transportation or to provide
restorative materials and disposables to locations as needed. Call the
number above or email: gkas@njda.org.
Irving Horowitz, DMD, an NJDA
member practicing in Rocky Hill
since 1979, was recently honored
with the NYU Faculty of the
Year award. A Rutgers College
undergrad and Tufts Dental
alum, Dr. Horowitz received a
certificate in Periodontics from the
University of California. He has
been an assistant professor at both the University of Illinois and the
University of Pennsylvania dental programs. Currently, Dr. Horowitz
is an assistant professor of periodontology and implantology in the
NYU residency program, where he has taught for 13 years.
The Southern Dental Society of NJ gathered on April 17
th
to
celebrate the career of long-time business manager, Elaine OBrien.
Elaine began working for the Southern in 1977 and has worked
hand in hand with 37 presidents, facilitating the work of the
dental society. Over 75 people gathered to honor her many years of
dedicated service; among them twenty former Southern presidents.
Elaine received many good wishes along with a diamond initial
pendant and a framed photograph of her with the former presidents.
She will be missed. Elaine is seen in the first row on the right.
Future Members in the News
The 91 members of the Rutgers School of Dental Medicines
(RSDM) inaugural classthe Class of 2017were welcomed into
dentistry and pledged to uphold the integrity of the profession at
the 2013 White Coat ceremony. Joining them were 25 students
from RSDMs Internationally Trained Dentist (ITD) program and
members of the Class of 2015. The ITD program is for qualified
dentists educated outside of the US or Canada, who become part
of the third-year class after completing a rigorous three-month
program. The ceremony was held on August 28 on the Newark
campus of the Rutgers Biomedical Health Sciences unit, part of
Rutgers, The State University of New Jersey.
After being cloaked by the presidents of each of the RSDM
current classes, the students signed the Rutgers School of Dental
Medicine Code of Professional Conduct and Ethics. The ceremony
ended with the recitation of the dental oath, led by Dr. Robert
Giantomas, president of the New Jersey Dental Association.
Members In The News
Volume 84, Number 4 10
Members In The News
Photo of Chanan Lerer. (Photo credit: Nick Romanenko)
The first White Coat ceremony took place at Columbia University
College of Physicians and Surgeons in 1993. Since then it has become a
tradition at medical and dental schools around the world. The School of
Dental Medicine held its first ceremony in 2005. It was one of the first
dental schools in the country to do so.
To Contact the NJDA JOURNAL
Tell us about honors and awards that you have received, special
things that you wish to share with your colleagues in a Journal
article and traditional letters to the editor. Your Journal wants to
hear from and about you. Journal of NJDA welcomes submissions of
photographs or artwork for consideration as cover art. Submissions
should have a vertical orientation and be sent in JPEG, EPS or TIFF
format with a minimum resolution of 300 DPI at full size (8.5 x
11). Please include the title, your name and location/date of photo.
The Journal reserves the right to reject any submission and to crop
images as necessary. The JNJDA also invites members to submit
lifestyle and feature stories, in addition to clinical articles. Send
inquiries to: Lorraine Sedor, managing editor, at lsedor@njda.org or
phone 732-821-9400. Harvey S. Nisselson, DDS, Editor.
45 Stouts Lane | P.O. Box 567 | Monmouth Junction, NJ 08852
732.329.0088
800.675.9819
732.329.0024
mgxprint.com
sales@mgxprint.com
Mastergraphx Printing
Your one stop source for:
offset printing
digital printing
posters
banners
color copies
pad printing
graphic design
CD/DVD duplication
11 Volume 84, Number 4
W
ell, its no secret. Chartless dentistry is coming, fast and
furious! Its not a requirement in dentistry yet (unless 30%
of your practice is treating Medicaid or Medicare patients),
but at some time in the future, its going to be. Lets look at your
practice. Have you started the process of eliminating paper from your
chart yet? If not, it is highly recommended to begin. For eliminating
a chart in an existing practice with hundreds and even thousands of
charts, the process is best done over a longer period of time. Most of
the chartless practices today are new ones, that have been built from
the ground-up to practice electronically. As for the 25-year old practice
that has been pulling, stuffing, and filing charts since its inception, its
going to take some time, and certainly lots of planning.
This is not going to be a how-to article on how to go chartless.
There are just too many variables. A strategy should be developed
with someone that has the proper expertise, like a dental technology
integrator, software trainer, or a practice management consultant. As
for any financial investment that would need to be made, there are
only three main ingredients: an adequate practice management
system, a digital X-ray system, and a computer in the operatories.
Most practices today have all three of these already, making the
transition fairly painless in terms of a monetary investment.
This article, however, is about the obstacles that the typical doctor has
created for himself, in his efforts to move forward, or at least begin the
process. But here is a secret...most dentists dont even realize that they
have already started the process. There are quite a few technologies
that have already been adopted into the practice that have set the ball
rolling, eliminating pieces of the paper chart and turning them into
bits and bytes and ones and zeros. Take for instance, electronic claims.
There was a time when we used to manually fill out a dental claim
form, and then make a copy for the chart. Then there is the innovation
of digital x-ray technology. Almost 75% of practices have already
eliminated x-ray film mounts from their charts. So lets keep it going.
As a dental IT consultant, my daily conversations with clients and
prospects will always lead to a discussion about going chartless. At this
point in the evolution of dental technology it certainly should be a goal
of your practice. If its not, you will do one of two things after reading
this article. You will either call your IT support professional and start
turning the wheels (even at a slow pace), moving your practice more and
more towards chartlessness. Or, you will create one of the three most
popular obstacles for yourself in order to not move forward; stopping the
movement towards eliminating a chart in your practice entirely.
These three obstacles are real, and I hear at least one of them in any
given day. Chances are that you are using one, two, or all three of
these reasons to keep your practice from moving forward. These are
obstacles that you probably have not received good answers to, or
you never asked yourself the question. So, lets address them now,
very simply and adequately.
Obstacle 1: Nervous about losing data or patient records to a crash!
This is a very real concern. Every healthcare provider with a
computer should take this one very seriously. In the industry, we call
this a data breach. And data breaches in the healthcare community
are now subject to huge fines and serious consequences for losing
someones patient record; but thats a different article, for a later
date. Getting past this obstacle though, is very easy. BACK IT UP!
Please take the time out of your busy practice to meet with a skilled
computer professional to design an adequate, full-proof backup strategy.
Your strategy should include at least two backup systems, with at least
one of them having an offsite option. Also, as a chartless office, it is not
only recommended to have a regular backup system, but you should
really make the investment in a Backup/Disaster Recovery (BDR)
system. A BDR will not only backup your data, but it will include
technology that allows you to deploy a backup server if ever needed.
As long as you take this strategy very seriously, and do the research to
learn what your technology support company actually recommends and
supports, you may never have to worry about this obstacle again.
Here are two very important hints for success to make note of: First, test
your backup system, including manually restoring data on a monthly
basis. Second, have the backup system monitored. Most IT firms offer
backup and server monitoring these days.
Obstacle 2: Doctors or staff s computer skills are not adequate.
This is tough one, even tougher than data security. There is a real
human element to this obstacle, which may lead to some tough
3 Major Obstacles to Going Chartless;
and How to Get Around Them!
Jeffrey Weiss
Volume 84, Number 4 12
RMN Cohsultahts . 167 Madisoh Ave . Suite 506, New York, NY 10016
RMNdehtalbrokers.com . RMNLLC47@gmail.com
Transitions can be bard, but tbey
don't bave to be.
Call now for free consultation
212-223-2844
Helping Dentists Uver 20 Years
Buy
Sell
Expand
Prosper
Check our website for more ihformatioh
RMNdehtalbrokers.com
Consul t ant s
The Leader i n Dent al Pr act i ce Tr ansi t i ons
decisions about the practices personnel. Computer skills are skills
that are pretty much a standard necessity these days, not only in
dentistry and healthcare, but in any profession. Computers are
here and are not going away. If anything, they are becoming more
involved in our lives. I hear of this obstacle pretty often, and its not
just from the older generation of doctors. We have seen some young
doctors who admit that they have very weak computer skills.
Make no mistake about it, if youre going to have a chartless office, you
are going to either need very good computer skills yourself, or have
staff with very strong computer skills. I have seen many offices get by
with a doctor that did not have the skills to work the computer in the
operatory himself. The routine with his assistant had to be redefined
and adjusted to compensate for the doctors lacking these skills.
Here are two very important hints for success to make note of:
First, get trainingand second, get MORE training. Training has
been such an important factor in successfully transitioning to chartless
dentistry. If you think you know everything that your charting program
can do, wait until you realize what it can do that you arent even aware
of! Furthermore, there are many customizable features in your software
that HAVE to be set up and personalized for you before you even begin.
Obstacle 3: The computers or computer network are slow,
unreliable or not stable.
This one is certainly a deal breaker. If your computers or computer
network are not running smoothly and efficiently, then going chartless
is going to be the most frustrating event of your career. Think about
how frustrating it will be for you, your staff, and your patients if the
digital x-ray system does not fire during an x-ray, or worse yet, the
internet has not been working all week so the office manager has not
been able to send out electronic claims. These events can not only be
annoying, but costly as well, resulting in lost patients or business.
The computers in your office need the same attention, importance, and
relevance to your practice that your other dental equipment has. Your
dental chairs, your compressor, your handpieces, and the x-ray generators,
must all be in tip-top shape to have your operations running smoothly.
So, why not maintain your computers? Computers are machines;
and machines need service on a regular basis in order to not break
down and to keep running smoothly.
To overcome this obstacle it might be time to get some professional
advice from a qualified IT service firm. Many practices do not have
a trusted service firm for their computer networks, but instead have
a part-time, go-to person who is a patient or a friend. We even come
across the Do-It-Yourself computer technician/dentist at times.
For a chartless dental office, here are a few reasons to engage a full-
time, IT professional to maintain your office from here on out:
Reliable response time when a question or issue arises. A typical
response time should be under one hour.
Regular maintenance and updates, as recommended by
the software and hardware manufacturers. It is proven that
computers run better and smoother when manufacturer updates,
patches, and firmware are installed.
Monitoring services, in order to be proactive in catching issues
with hardware as early as possible. Most issues that develop in a
computer or server, if caught early enough, will not result in a
crash or freeze-up.
Help Desk support available during regular hours and the
proper off-hours protocols.
A professional who is aware of and familiar with HIPAA laws,
Hi Tech Act, and now the final Omnibus Rule for healthcare.
So, those are the three most common obstacles that dentists create
in keeping their practices from moving forward with chartless
dentistry. Im sure there are others, however, this would be a good
time to schedule a consultation with your IT support firm or
software vendor to see where your practice is at with your charts.
Then, take that knowledge one step further by putting a plan in
place to slowly start eliminating the paper inside of it. So when
being chartless is required, you will be there already.
About the Author
Jeffrey Weiss is President and partner of High Tech Innovations,
LLC, the largest dental integrator in the tri-state area; currently
supporting 500+ dental practices. High Tech Innovations
prides itself on not only knowing IT and technology, but also
understanding the field of dentistry. They are certified as installers
by most of the largest dental technology companies in the profession
and have recently become an Endorsed Partner of the New Jersey
Dental Association. Weiss can be contacted at (973)889-0030 or
at jeffw@hticonsultants.com.
13 Volume 84, Number 4
Introduction
Implant therapy is highly predictable and successful. However,
certain risk factors can predispose individuals to lower rates of
success. Cigarette smoking has long been known to be associated
with a variety of oral conditions including periodontal disease, bone
loss, tissue loss, tooth loss, edentulism, peri-implantitis and dental
implant failure. Nicotine in tobacco has been shown to reduce the
blood flow in the mouth. Pipe smoking can be worse than cigarettes
due to the higher temperatures generated in the upper jaw. Not only
is smoking detrimental to implants, it is also bad for conventional
bridgework. Smoking affects healing and tissue health in many
ways, including impaired neutrophils, altered blood flow to tissues
and diminshed oxygen perfusion.
Oral Conditions:
1. Periodontal DiseasePeriodontitis is an inflammatory
condition of the periodontium in response to bacterial
pathogens that promote the release of numerous cytokines
and leads to periodontal attachment and bone loss. Twenty
years of research show that cigarette smoking is probably a
true risk factor for periodontitis. A smoker is 2 to 3 times
as likely to develop clinically detectable periodontitis. In
addition to increased prevalence, smokers also experience more
severe periodontal disease. It appears that a history of treated
periodontitis does not adversely affect implant outcome.
3,5,10,11
2. Bone and Tissue lossA study examining the effect of oral burn
syndrome on dental implants indicated that there is a direct link
between oral tissue loss and smoking.
1
In addition, smoking had a
significant impact on bone loss.
7
The most significant differences
regarding implant survival between smokers and nonsmokers
were found in studies that identified and evaluated implants
placed in the maxilla and those placed in grafted sites. It appears
that smoking is a significant risk factor with an adverse effect on
implant survival and success in areas of loose trabecular bone.
11
3. Tooth loss and EdentulismTooth loss and edentulism are
more common in smokers than in nonsmokers.
4
Tooth loss in
older adults occurs because of increased exposure to pathogenic
bacteria. Smoking also predisposes patients to develop more
severe periodontal disease.
2,6
4. Peri-ImplantitisThe formation of deep mucosal pockets
with inflammation of the peri-implant mucosa around dental
implants is called peri-implantitis. Smokers treated with dental
implants have a greater risk of developing peri-implantitis.
This condition can lead to increased resorption of peri-implant
bone. If left untreated, peri-implantitis can lead to implant
failure. In a retrospective study conducted at the University of
Vienna, the peri-implant tissue of smokers and nonsmokers was
compared. The smokers showed a higher score in bleeding index
with greater peri-implant pocket depth and radiographically
discernible bone resorption around the implant, particularly
in the maxilla.
8
Implant surface characteristics can influence
bone-implant contact and may improve implant outcomes. HA-
coated implants can improve the survival or success of implants
in smokers compared with nonsmokers.
11
Smoke Cessation
Former smokers have a lower risk for periodontitis than current
smokers. Smoking cessation will result in improved periodontal
health and improve a patients chance for successful implant
osseointegration.
4,9
Conclusion
The review of this literature demonstrated that smoking has an
adverse affect on implant survival and success. Implant success rates
tend to be lower than survival rates and vary greatly depending on
the criteria used to measure success. Despite these high implant
survival and success rates, there is a general appreciation that risk
factors predispose individuals to more complications and implant
Effects of Smoking on Implant Failure
A Review
Haritha Mikkilineni, MDS
Deepika M. Reddy, DDS
Narendra Jayanth, BDS
Volume 84, Number 4 14
failures, and may result in lower implant survival and success
rates. The effect of smoking on implant survival appeared to be
more pronounced in areas of loose trabecular bone. A history of
treated periodontitis does not appear to adversely affect implant
survival rates but it may have a negative influence on implant
success rates, particularly over longer periods. Whichever course
of treatment patients decide to pursue, they can expect slower
healing and a greater possibility of failure if they continue to
smoke during or following the treatment healing period. If
patients stop smoking three to four weeks prior to implant
placement and remain smoke-free during the healing period,
results may improve. Many of our smoking patients have used
implant treatment as an opportunity to quit smoking altogether.
The dentists can prescribe smoke cessation medications and
products to assist in the quitting process.
References
1. The oral burn syndrome and its effects on dental implants . R.Cullen. J
Oral Implantol 1998;24(4):21921.
2. Periodontal diseases and dental implants in older adults.
Wilson,Higginbottom. J Esthet Dent 1998;10(5):265:71.
3. Surgical determinants of clinical success of osseointegrated oral
implants: a review of the literature. Sennerby, Roos. Int J. Prosthodont
1998 septoct; 11(5):40820.
4. Cigarette smoking and periodontal diseases: etiology and management
of disease. Tonetti. Ann periodontal 1998 Jul;3(1):88101.
5. Biological factors contributing to failures of osseointegrated oral
implants. (II) Etiopathogenesis. Esposito, Hirsch, Lekholm. Thomsen.
Eur J Oral sci 1998 Jun;106(3):72164.
6. Influences of smoking on the periodontium and dental implants. Dent
Update 1997 oct;24(8)32830.
7. A prospective 15 year follow up study of mandibular fixed prostheses
supported by osseointegrated implants. Clinical results and marginal
bone loss. Clin Oral Implants Res 1996 Dec;7(4):32936.
8. The relationship of smoking on peri implant tissue: a retrospective
syudy. Haas R; Haimbock W; Mailath G; Watzek G. J Prosthet Dent
1996 Dec;76(6):5926.
9. Smoking and implant failurebenefits of a smoking cessation protocol.
Int J Oral Mxillofac Implants 1996 NovDec; 11(6):7569.
10. The effect of smoking on early implant failure. DeBruyn, Collaert. Clin
Oral Implants Res 1994 Dec;5(4):2604.
11. INT J Oral Maxillofac Implants 2007;22(suppl):173202.
About the Authors
Haritha Mikkilineni, MDS, is a prosthodontist in Hyderabad, India.
Deepika M. Reddy, DDS, is a member of the NJDA and an associate
dentist at Signature Smiles in Atlantic City, New Jersey. Narendra
Jayanth, BDS, is a general dentist in Anantapur, India.
Personalized
for Your
Individual Needs
Buying or selling a dental practice is one of the most
important business decisions you will ever make.
Thats why Professional Practice Transitions (PPT)
is the best choice to make when you are trying to nd
opportunities that match your needs and goals.
With PPT, you are ensured that your life-long
dedication to building and sustaining a successful
business will be respected and leveraged to bring
the results you look forward to.
Call 1-800-988-5674 today to learn more about
improving your opportunities for success.
Professional Practice Transitions
well get you there
www.henryschein.com/ppt
www.snydergroup.net
12PT6814_PPT_3.5x10bw 10/31/12 3:55 PM Page 3
15 Volume 84, Number 4
D
entists encounter patients with facial pain every day in
their practices. The most common source of any facial pain
involves that of an odontogenic origin. This would include:
Teeth: caries, periapical pathology, root hypersensitivity,
fractured roots and tooth structure, failed restorations,
periodontal, non-carious lesions, occlusal traumatism
Oral Mucosal Lesions: aphthous, lichen planus, vitral, trauma,
mucous membrane disease
Burning Mouth Syndrome: hormonal influence,
medications, xerostomia
When the dentist or endodontist definitively rules out an
odontogenic source of facial pain, it is prudent to eliminate all other
possible considerations. Too often a TMJ/TMD origin is considered
without thoroughly investigating other possible non-odontogenic
sources of facial pain.
Facial Pain of Non-odontogenic Source:
Myogenous: Muscle spasm or edema; ligamentous or tendinous strain
Cervicogenic: Upper cervical spine misalignment involving Atlas bone
Neural and Vascular CompressionCervico-Trigeminal nerve
convergence pain into face
Neurogenous: Associated with Trigeminal, facial & sympathetic
nervous system dysregulationsNeurological (conditions of the
brain), Multiple sclerosis
Vascular/Glandular: Temporal arteritis, Vascular compression,
Glandular disease (Parotid and Submaxillary) Arthrogenous
(Structural Displacement TMJ): TMJ with disc displacement,
Condylar bone changes
Neoplastic (Obstructive): Neoplasm
Referred Source: Otologic, Paranasal Sinuses, Cardiac
We can consider a TMJ source if the patient presents with:
Temporal and frontal headaches
Preauricular and masseteric region pain
TMJ clicking and popping
Ear ringing and clogging
Sensitive teeth.
It is often thought that patients develop facial pain from bruxism.
However, grinding of the teeth can be a manifestation of an existing
structural problem. It may also develop from sources other than a
TMJ dysfunction.
The upper cervical spine is very typically misaligned in patients that
have a TMJ dysfunction. Often the same trauma that causes a TMJ
disc displacement can cause atlas misalignment. Atlas misalignment
contributes to subluxation and compression of the upper cervical
nerves. There is a convergence of the upper cervical nerves and
trigeminal nerve in the trigeminal nucleus caudalis. Therefore, facial
pain from an upper cervical spine source is very common due to this
convergence pattern.
There are several conditions where patients present with facial pains
and symptoms that mimic that of a TMJ source. Therefore, when
a primary TMJ source of pain is suspect, other conditions to
consider include Chiari malformation. This is a condition that
can be both congenital and acquired where the cerebellar tonsils
are located below the foramen magnum into the spinal cord.
Symptoms include headache, neck pains, dizziness, changes in
the gait, ear ringing and tingling into the face. (Fig.1)
A typical incidental finding would include styloid elongation. This
is a condition whereby the styloid bony process appears to be longer
than usual. The stylomandibular ligaments and/or the stylohyoid
ligaments undergo calcification and ossification and appear bone
like. Typical symptoms are preauricular pain, dizziness especially
with head turning, pain with swallowing and extending the tongue
and pain in the teeth. (Fig. 2)
Neurogenous pain sources would include trigeminal neuropathic
pain as in trigeminal neuralgia, herpetic or post-herpetic neuralgia,
(Fig. 3) multiple sclerosis and neoplasm. (Fig 4) Neurogenous pains
are typically described as sharp, shooting, stabbing, electric like,
tingling with numbness into the face and teeth unilaterally. These
can be of short duration and intermittent with pain-free episodes.
Facial Pain of Non-Odontogenic Origin
Louis R. Vita, DDS, FAGD
(Fig.1)
(Fig.2)
Volume 84, Number 4 16
An infectious source can be that of otalgic, mastoid (Fig. 5) or sinus
pathology. It is common for sinus disease, ear infections and cardiac
conditions to refer pain into the face.
Another common complaint of facial pain involves a dysregulation
of the sympathetic nervous system. Commonly thought of as Reflex
Sympathetic Dystrophy, this condition is now referred to as Facial
Complex Regional Pain Syndrome, i.e., Facial CRPS. When there is
a disturbance in the sympathetic nervous system, patients can present
with constant burning pain in multiple areas of the head, face and
neck. Dental implications of Facial CRPS include hypersensitivity
of the teeth especially to cold, pulpal edema and pain even without
obvious dental causes as caries or large fillings, painful dental injections
from an exaggerated reaction to the stimuli, swelling and pain in the
gingiva, cheeks and nasal cavities (congestion). There can be oral and
tropic skin changes with tooth discoloration. Facial CRPS would
typically contribute to a reduced mandibular range of motion, tremors,
dystonia and parafunction as with bruxism and nebulous occlusion in
which maximum intercuspation position is not reproducible.
Therefore, when a patient presents with facial pain, the potential
odontogenic source must be initially eliminated. Once the health of
the oral cavity is determined, all other systems and conditions can
be investigated.
References
1. Mayo Foundation for Medical Education and Research (MFMER);
19982013
2. Zohar et al. 1986, Krennmair et al. 1994 Symptoms of
Styloid Elongation.
3. Janetta, Peter: Trigeminal Neuralgia, Oxford University Press, Inc.
2011. Diagnostic Criteria for Trigeminal Neuralgia; Table 7.1
Page 75
4. Melis, M et al. Complex Regional Pain Syndrome in the head and neck:
a review of the literature. J Orofac Pain 2002 Spring; 16(2): 93104
About the Author
Louis Vita, DDS, FAGD, has a general, family practice in Clifton, NJ.
He established and directs the Vita Head, Neck & Facial Pain Relief
Center and is a recognized authority on the subject. Dr. Vita serves as
an attending dentist and lecturer at Hackensack University Medical
Centers Dental Department where he instructs the residents in dentistry
and TMJ disorders.
(Fig.3)
(Fig.4)
(Fig.5)
17 Volume 84, Number 4
B
i
g
A
p
p
l
e
2
0
1
4
D
e
n
t
a
l
M
e
e
t
i
n
g
Sponsored by
The Bronx County
Dental Society
WEDNESDAY, MARCH 19, 2014
THURSDAY, MARCH 20, 2014
THE SHERATON MAHWAH. MAHWAH, NEW JERSEY
Two full days of education
Morning, afternoon and evening seminars
Commercial Exhibits
$25/$10 Discount Coupons for Purchases at the
Meeting
Free Parking: Indoors and Outdoors
Free Breakfast and Free Buffet Lunch
For Full Day Seminars
EXHIBIT HOURS: 9:30 a.m. to 7:00 p.m.
CONTINUING EDUCATION CREDITS WILL BE GIV-
EN TO ALL ATTENDEES. THESE CREDITS WILL BE
APPLICABLE FOR DENTIST AND DENTAL HYGIENIST RE-
QUIREMENTS AS ALLOWED BY STATE LAW.
SPECIAL BONUS FOR
ATTENDING OUR SEMINARS
A $25 exhibitors coupon will be given to each dentist for attend-
ing a full-day seminar and a $10 coupon to each dentist attending
a half-day or evening seminar. When presenting your $25 or $10
coupon for full day, half day and evening paid seminars any
purchase made at the exhibitors booth will be discounted at the
$25 or $10 rate. You will receive a coupon for every paid course
that you attend and no minimum purchase is required!
28th Annual
BIG APPLE
DENTAL MEETING
Sponsored by
The Bronx County Dental Society
1. MATERIALS AND ESTHETICS
Dr. George Bambara
Dr. David Clark
Dr. Howard Glazer
Dr. Richard Trushkowsky
Dr. Arthur Volker
Dr. Carlos Alfonso
2. ENDODONTICS
Dr. Douglas Lambert
Dr. J effrey Linden
3. PROSTHETICS
Dr. Michael DiTolla
4. PRACTICE MANAGEMENT
Dr. Matthew Krieger
Linda Lakin, RDH, MS
Christine Taxin
5. TECHNOLOGY
Dr. Paul Feuerstein
Dr. Gary Severance
6. INFECTION CONTROL
Dr. Harold Edelman
2014 Partial List of Speakers
7. RISK MANAGEMENT
Dr. Robert Peskin
Amy Kulb, Esq.
8. PATHOLOGY
Dr. Alvin Heller
Olga Ibsen, RDH, MS, FAADH
9. MEDICAL EMERGENCIES
Dr. Stanley Malamed
10. OPERATIVE
Dr. J oel Berg
11. DENTAL ASSISTING
Shannon Pace Brinker, CDA, CDD
12. FINANCE
Mr. W. Michael Prendergast
For further information, contact:
The Bronx County Dental Society
718-733-2031 718-733-0186 (fax)
email: bronxdental@optonline.net
Website: www.bigappledentalmeeting.us
Secure
online registration
on our website.
B
i
g
A
p
p
l
e
2
0
1
4
D
e
n
t
a
l
M
e
e
t
i
n
g
Sponsored by
The Bronx County
Dental Society
WEDNESDAY, MARCH 19, 2014
THURSDAY, MARCH 20, 2014
THE SHERATON MAHWAH. MAHWAH, NEW JERSEY
Two full days of education
Morning, afternoon and evening seminars
Commercial Exhibits
$25/$10 Discount Coupons for Purchases at the
Meeting
Free Parking: Indoors and Outdoors
Free Breakfast and Free Buffet Lunch
For Full Day Seminars
EXHIBIT HOURS: 9:30 a.m. to 7:00 p.m.
CONTINUING EDUCATION CREDITS WILL BE GIV-
EN TO ALL ATTENDEES. THESE CREDITS WILL BE
APPLICABLE FOR DENTIST AND DENTAL HYGIENIST RE-
QUIREMENTS AS ALLOWED BY STATE LAW.
SPECIAL BONUS FOR
ATTENDING OUR SEMINARS
A $25 exhibitors coupon will be given to each dentist for attend-
ing a full-day seminar and a $10 coupon to each dentist attending
a half-day or evening seminar. When presenting your $25 or $10
coupon for full day, half day and evening paid seminars any
purchase made at the exhibitors booth will be discounted at the
$25 or $10 rate. You will receive a coupon for every paid course
that you attend and no minimum purchase is required!
28th Annual
BIG APPLE
DENTAL MEETING
Sponsored by
The Bronx County Dental Society
1. MATERIALS AND ESTHETICS
Dr. George Bambara
Dr. David Clark
Dr. Howard Glazer
Dr. Richard Trushkowsky
Dr. Arthur Volker
Dr. Carlos Alfonso
2. ENDODONTICS
Dr. Douglas Lambert
Dr. J effrey Linden
3. PROSTHETICS
Dr. Michael DiTolla
4. PRACTICE MANAGEMENT
Dr. Matthew Krieger
Linda Lakin, RDH, MS
Christine Taxin
5. TECHNOLOGY
Dr. Paul Feuerstein
Dr. Gary Severance
6. INFECTION CONTROL
Dr. Harold Edelman
2014 Partial List of Speakers
7. RISK MANAGEMENT
Dr. Robert Peskin
Amy Kulb, Esq.
8. PATHOLOGY
Dr. Alvin Heller
Olga Ibsen, RDH, MS, FAADH
9. MEDICAL EMERGENCIES
Dr. Stanley Malamed
10. OPERATIVE
Dr. J oel Berg
11. DENTAL ASSISTING
Shannon Pace Brinker, CDA, CDD
12. FINANCE
Mr. W. Michael Prendergast
For further information, contact:
The Bronx County Dental Society
718-733-2031 718-733-0186 (fax)
email: bronxdental@optonline.net
Website: www.bigappledentalmeeting.us
Secure
online registration
on our website.
Oral Pathology Quiz #81
Presented by Rutgers School of Dental Medicine Biopsy Service
The NJDS oral pathology faculty are showing the clinical presentation of some relatively common lesions for readers to self-evaluate
their skills in clinical differential diagnosis. You are expected to choose the most likely clinical diagnosis on the basis of history and
clinical or radiographic appearance with the appreciation that definitive diagnosis requires microscopic examination of the specimen.
Case Number 1 Figures 1 and 2: Courtesy Drs. Daynet Fraga and Maano Milles, Rutgers University
A 32-year-old man complained of a painless swelling in his mouth, which he
said had been present for about a month. The dome-shaped lesion appeared
to arise from the left maxillary ridge, in the area of the premolars that had
been extracted 3 months previously. The enlargement was relatively soft in
consistency, red, and measured approximately 2 cm by 1.5 cm. Clinical and
radiographic examination revealed numerous carious teeth and an edentulous
left posterior maxillary ridge. There was a small defect in the floor of the
left maxillary sinus at the site of the extracted first premolar. The shadow of
the soft tissue enlargement is also visible on the radiograph. Which of the
following is the most likely diagnosis?
A. Maxillary sinus pseudocyst
B. Postoperative maxillary cyst
C. Herniated maxillary sinus
D. Epulis granulomatosum
Volume 84, Number 4 20
Answers on page 24
Case Number 4 Figure 5: Courtesy Dr. Roberta Grill Deutsch, New York, NY
Clinical examination of a healthy 63-year-old African-American male detected a compressible
area in the mucobuccal fold adjacent to his left maxillary lateral incisor and canine. The canine
was an abutment for a bridge. A periapical radiograph revealed a moderately well-defined,
unilocular radiolucency above the apices of the two teeth. It measured approximately one cm
in diameter. Root canal therapy had been performed on the canine 2 years earlier, with no change
in the size of the radiolucency. The lateral incisor was vital. Which of the following is the most
likely diagnosis?
A. Radicular (periapical) cyst
B. Dental (periapical) granuloma
C. Ameloblastoma
D. Globulomaxillary cyst
Case Number 2 Figure 3: Courtesy Dr. Daniel Barabas, Ridgewood
A 27-year-old healthy male presented with a solitary, painless, firm, pink, sessile, smooth-
surfaced papule on his lower labial mucosa, immediately to the right of the midline. It was 3
mm in maximum dimension. He reported that he had been aware of the lesion for 10 years,
but now wanted it removed and diagnosed as soon as possible because he was leaving the
United States. The most likely diagnosis is:
A. Pyogenic granuloma
B. Peripheral giant cell lesion
C. Traumatic neuroma
D. Verruca vulgaris
Case Number 3 Figure 4: Courtesy Dr. Andrew Yampolsky, Rutgers University
A 27-year-old female complained of slight buccal expansion in the left body
of her mandible. There was no pain or tenderness. She reported that she had
cyst surgery and extractions in her left lower jaw some time ago but did
not know what the diagnosis had been. The only teeth remaining in her left
mandible were the incisors and second molar. A panoramic radiograph revealed
a multilocular, radiolucent lesion in the edentulous canine-premolar region
of her left mandible. It measured approximately 2.5 cm mesiodistally by 1.5
cm vertically. The honeycomb lesion expanded the superior alveolar border
and extended inferiorly two-thirds of the way into the jaw. The patient was
otherwise healthy and there were no other significant lesions. Which of the
following is the most likely diagnosis?
A. Ameloblastoma B. Residual cyst C. Dentigerous cyst D. Lateral periodontal cyst
21 Volume 84, Number 4
NJDA Annual Golf Outing Recap
Golf is a game in which you yell fore, shoot six and write down five.
Paul Harvey
lr: Giancarlo Ghisalberti, and Drs. Luciano Ghisalberti, Thomas
Rossi and Gregory LaMorte.
lr: Drew Nagle, Sharon and Dr. Richard Riva, Scott Elias.
O
ld York Country Club in Chesterfield was the site of the
Associations annual golf outing in August. Eighteen holes
of golf, interspersed with occasional rain drops and bright
sunshine, brought out some of the Associations best golfers,
friends and business associates.
Here are this years winners: 1
st
place net, Cristos Gikas, 72; 2
nd
place
net, Drew Nagle, 72; and, 3
rd
place net, Giancarlo Ghisalberti,
72. First place gross went to Jimmy Arbef, 71; 2
nd
place gross, Ross
Selby, 77; and 3
rd
place gross to Dr. Luciano Ghisaberti, 81.
Dr. Ghisalbertis son, Giancarlo, also won the longest drive,
on hole #14. Dr. Ralph Baines won closest to the pin, on
hole #2, missing a hole-in-one by only 4 6. Winners of
Dr. Charlie Perles Putting Challenge, sponsored by
Delta Dental of NJ, were Dr. Rocco DiAntonio and Dr.
Paul Kaplan.
The annual event is sponsored by the Associations partners
and other corporate supporters, including: New Providence
Financial, Delta Dental, NJCAR, Medical Design Build,
The Dental Laboratory Group, CareCredit, PNC Bank,
AFTCO, Bank of America, Colgate, The Glove Club,
Henry Schein Dental, TD Bank, TDIC, Meadowbrook
Insurance, High Tech Innovations, FSI, Kuwata Pan Dent,
and Demandforce.
Volume 84, Number 4 22
R
ecently a patient of mine, who is a physician, told me he
sold his practice to Atlantic Health System. Atlantic Health
System owns a number of hospitals and also private, or
formerly private, medical practices. There is a trend for the same
companies that own hospitals to acquire private practices. The
more hospitals and doctors owned by the company, the stronger the
power to negotiate with insurers for higher reimbursement rates.
The insurer, in turn, raises premiums to cover any increases and
additional profit.
As a believer in quality healthcare, I become concerned when
decisions are taken away from doctors and other health
professionals, and their patients. While consolidation to a point
can lower costs and increase efficiency, the number one goal of any
corporation is to increase profits. So I question whether the long-
term effect of this arrangement offers any benefit to patients.
In the early days of medical insurance, doctors were happy receiving
a guaranteed payment of 80% or more of the now obsolete
terminology UCR (usual, customary and reasonable) fees, so they
were less concerned about collecting the remaining copayment.
Insurance companies realized this and started to set their own prices
through PPOs and HMOs.
Initially, dental insurance was a totally different entity. We also had
UCR fees, but insurance companies, along with our State Board,
ensured that copayments were collected. The true difference was,
and still is, the overall economics of dentistry vs. medicine. Dental
insurance has a maximum per year, where medical insurance
did not. In fact, I would propose that dental insurance shares
more similarities to auto insurance, with both deductibles and
maximums, than medical insurance. Also, the overall cost of dental
care is 100 times less than medical care.
I have been a dentist long enough to have seen the HIV scare
resulting in necessary improvements in infection control, OSHA,
HIPAA, and the effects of a recession on dentistry. So, in the past
where patients questions may have been about sterilization of
instruments, they are now much more concerned about cost of
treatment than any other issue. Since the average dental student
graduates these days with about $200,000 of student loan debt,
coupled with the substantial cost of buying or opening a practice, I
am concerned about my professions future.
There has to be a reasonable return on investment for students to
want to invest a minimum of 8 years of college and postgraduate
education and the associated cost of acquiring a dental practice,
or we risk becoming an employee profession of corporate health
systems. I do believe the current and primary form of solo dental
practice is an endangered species due to cost issues.
About the Author
Jeffrey A. Mermelstein, DMD, is a general practitioner with
offices in Livingston. A member of the Essex County Dental
Society, Dr. Mermelstein also is a member of the NJDA Council
on Annual Session.
Opinion:
The Economics of Healthcare and
its Implication for Dentistry
Jeffrey A. Mermelstein, DMD
X-RAY TRAINING FOR NJ LICENSE
NJ School of Dental Assisting has a
Sunday only 10 week program which
fulflls state license training requirements.
We have small classes with experienced
instructors. Classes are available at our
New Brunswick and Forked River locations.
Dental Assistants Available
We have trained assistants looking for
employment, please e-mail your job
requirements and graduates will contact
you directly. This is a free service.
NJ School of Dental Assisting
www.njdentalassist.com
njdentalassist@att.net
800-726-2137
The dental radiology course for dental assistants is accredited by
the New Jersey Radiologic Technology Board of Examiners
23 Volume 84, Number 4
Oral Pathology Quiz #81
Answers
Case Number 1 C. Herniated maxillary sinus
There is considerable individual variation in the thickness and density of bone between the apices of posterior maxillary teeth and the soft
tissue lining of the maxillary sinus. Oro-antral communication is most likely to occur as a consequence of extraction of posterior maxillary
teeth when the maxillary sinus floor extends beyond one quarter of the length of the roots of the teeth, or between the roots of adjacent
teeth. It has been suggested that a sudden increase in pressure within the sinus, such as post-extraction sneezing, may contribute to this
complication. Some small oro-antral communications will heal without the formation of a fistula or chronic sinusitis. Numerous factors
may interfere with spontaneous resolution, including the presence or absence of pre-existing infection and quality of post-operative care. It
is not clear why herniated maxillary sinus mucosa (C) developed in this case.
A biopsy of the soft tissue mass revealed mucosa that lines the sinus, but is not normally found in the oral cavity. The biopsy specimen also
revealed typical oral epithelium overlying inflamed connective tissue. That is consistent with epulis granulomatosum (D), which is also known
as post-extraction inflammatory mucosal hyperplasia. Hyperplastic tissue growing in an extraction socket is a relatively common event.
In this case, the entire soft tissue mass was removed and the oro-antral defect was surgically repaired.
Maxillary sinus pseudocyst (A) is a relatively common, asymptomatic, non-expansile lesion that presents radiologically as a smooth, non-corticated,
dome-shaped, slightly opaque hemisphere above sinus floor. Postoperative maxillary cyst (B) is also known as surgical ciliated cyst. This rare
entity is caused by displacement of part of the sinus epithelial lining, usually during surgery. The implanted epithelium then generates a true,
expansile cyst that appears radiologically as a well-defined, spherical, radiolucent lesion, within bone but separate from the maxillary sinus.
Te Oral Pathology Quiz is presented by faculty of the Rutgers University Rutgers School of Dental Medicine, Division of Oral
Pathology, Drs. Deborah B. Cleveland, Joseph Rinaggio, and Lawrence C. Schneider. Clinicians who have clinical pictures and/or
radiographs of cases suitable for future quizzes should call Dr. Schneider at (973) 972-4375. E-mail: Lawcschneider@aol.com.
Biopsy kits may be obtained without charge by calling (973) 972-1646. Faculty are available to answer questions Monday through
Friday, from 8:00 AM to 4:00 PM.
Answers from page 20
Botox
& Dermal Filler Training
for Every Dental Practice
THE BEST LIVE PATIENT TRAINING AVAILABLE
December 13-14 ............................New York (Levels I, II)
January 30 - Febuary 1 ................................. New Jersey
CALL 800.952.0521 : : WWW.FACIALESTHETICS.ORG
[SCAN FOR DETAILS]
Register by December 15
th
and Save!
> SIGN UP NOW AND SAVE UP TO $1000
> AGD & AACD MEMBERS SAVE MORE
> CHECK THE AAFE WEBSITE FOR MORE UPCOMING COURSES
Frontline TMJ, Headache and Facial Pain
Therapy for Every Dental Practice
LIVE PATIENT 2-DAY COURSE
December 12-13 ................................................ New York
January 30-31 ................................................ New Jersey
Earn up to 24 CE Credits!
Botox
& Dermal Filler Training
for Every Dental Practice
THE BEST LIVE PATIENT TRAINING AVAILABLE
December 13-14 ............................New York (Levels I, II)
January 30 - Febuary 1 ................................. New Jersey
CALL 800.952.0521 : : WWW.FACIALESTHETICS.ORG
[SCAN FOR DETAILS]
Register by December 15
th
and Save!
> SIGN UP NOW AND SAVE UP TO $1000
> AGD & AACD MEMBERS SAVE MORE
> CHECK THE AAFE WEBSITE FOR MORE UPCOMING COURSES
Frontline TMJ, Headache and Facial Pain
Therapy for Every Dental Practice
LIVE PATIENT 2-DAY COURSE
December 12-13 ................................................ New York
January 30-31 ................................................ New Jersey
Earn up to 24 CE Credits!
AAFE-DJ-NewJersey-7.5x3.25-2clr.indd 1 9/23/13 1:50 PM
Volume 84, Number 4 24
Case Number 2 C. Traumatic neuroma
Traumatic (amputation) neuroma (C) is linked to injury. Damage to a peripheral nerve fiber bundle sometimes produces a disorganized
proliferation of neural tissue and scar tissue. Clinically, it presents as a normal-colored, firm, smooth-surfaced, well-defined nodule or
papule that is attached to surrounding mucosa. These lesions may be tender or even painful.
Pyogenic granuloma (A) is excluded because it is soft and red. Peripheral giant cell lesion (B) is excluded because it occurs only on the
gingivae or alveolar ridge. Verruca vulgaris (D) is excluded because it has a papillary surface contour.
The differential diagnosis for a solitary, dome-shaped, normal-colored, firm, well-defined nodule or papule on the oral mucosa includes
reactive lesions (irritation fibroma, traumatic neuroma, peripheral ossifying fibroma, peripheral giant cell lesion) and benign neoplasms
(pleomorphic adenoma, canalicular adenoma, neurilemoma, solitary neurofibroma, and leiomyoma). Peripheral ossifying fibroma and
peripheral giant cell lesion occur only on the gingivae or alveolar ridge.
Case Number 3 A. Ameloblastoma
Ameloblastoma (A) is the most common odontogenic neoplasm. The majority of these benign tumors are the classical, infiltrative,
aggressive subtype. Most of such lesions are asymptomatic and are recognized during routine clinical or radiographic examination or
because they have caused expansion of the jaw. If untreated, they may eventually cause serious deformity. Although they arise anywhere in
the jaws, the posterior mandible is the most common location and the mean age at diagnosis is about 35 years. Radiologically, they appear
as well-defined radiolucencies, which are more often multilocular than unilocular. Recurrence rates are lowest when tumors are excised at
least one cm beyond their radiographic margins.
Residual cyst (B) is excluded because it almost always presents as a unilocular radiolucency. Dentigerous cyst (C) is excluded because it
appears as a unilocular radiolucent lesion enveloping all or part of the crown of an impacted tooth. Lateral periodontal cyst (D) is excluded
because it is a unilocular radiolucent lesion. (The botryoid odontogenic cyst is the polycystic and multilocular variant of the lateral
periodontal cyst.)
The differential diagnosis of well-defined, multilocular radiolucencies of the jaw also includes other odontogenic tumors (odontogenic
myxoma and ameloblastic fibroma), odontogenic cysts (odontogenic keratocyst and calcifying odontogenic cyst), non-odontogenic tumors
(solitary central giant lesion, central hemangioma, and central mucoepidermoid carcinoma), brown tumor of hyperparathyroidism, and
aneurysmal bone cyst.
Case Number 4 B. Dental (periapical) granuloma
Dental (periapical) granulomas (B) are by far the most common inflammatory periapical lesions that are the consequence of pulp necrosis.
They are approximately three times more common than radicular (perapical) cysts (A), although that differential is much less significant in
cases that have failed to respond to conservative endodontic measures. Clinically and radiologically the two conditions are inseparable.
Ameloblastoma (C) occasionally presents as a periapical radiolucent lesion but all variants of ameloblastoma combined are much less
common than dental granulomas.
Historically, the term globulomaxillary cyst (D) was applied to cysts between the roots of maxillary lateral incisors and canines that were
believed to be fissural in origin. It was assumed that they arose from epithelium trapped in line of fusion between median nasal and
maxillary processes. Research revealed that they are odontogenic cysts (radicular, lateral periodontal, calcifying odontogenic or odontogenic
keratocysts). Currently, the term indicates the location of a cystic radiolucency.
The differential diagnosis of a well-defined periapical unilocular radiolucency includes inflammatory lesions (dental granuloma, radicular
cyst, apical abscess, and apical scar), other odontogenic cysts (odontogenic keratocyst and calcifying odontogenic cyst), odontogenic tumors
(ameloblastoma) , and Langerhans cell disease (histiocytosis X).
25 Volume 84, Number 4
1. Bruxism is a repetitive jaw-muscle activity characterized by
clenching or grinding of the teeth
Bruxism has been recently defined by an international consensus
as a repetitive jaw-muscle activity characterized by clenching
or grinding of the teeth and/or by bracing or thrusting of the
mandible. Bruxism has two distinct circadian manifestations:
it can occur during sleep (indicated as sleep bruxism) or during
wakefulness (indicated as awake bruxism).
1
2. Bruxism is a centrally-mediated phenomenon
Systematic literature reviews reported that the etiological role
of peripheral (i.e., anatomy of dental occlusion and other
morphological features) has been progressively dismantled in favor
of central origin theories (i.e., psychological, social, neurobiological
factors). Importantly, bruxism must not be considered a disorder per
se, so that the etiology and clinical meaning of the different forms
(i.e., clenching-type vs. grinding-type; sleep vs. awake bruxism)
should be better discriminated.
2,3
3. Epidemiology of bruxism is characterized by a decrease with
age and no gender differences
In recent systematic reviews, bruxism prevalence in adults was
between 8% and 31.4%.
4
Bruxism was found to be unrelated to
gender, and a decrease with age was common to all of the reviewed
studies. Very little information is available on the epidemiology of
different bruxism activities.
4. Bruxism might be a threat for dental implant treatments
Conclusions from a systematic review suggest that bruxism may be
a risk factor for mechanical complications on implant-supported
rehabilitations. However, bruxism is less likely to be a risk factor for
biological complications around dental implants.
6
5. Management of bruxism requires a multidisciplinary
approach as well as occlusal appliances, behavioral and
pharmacological therapy
Bruxism should be assessed by a multidisciplinary team that includes
dentists, neurologists, sleep-medicine specialists, and psychologists.
Bruxism can best be managed by adopting a multiple-P approach:
Plates (i.e., oral appliances), Pep talk (i.e., counseling), Pills (i.e.,
pharmacological treatments with centrally-acting drugs), and
Psychology (i.e., supporting psychological techniques).
7
References
1. Lobbezoo F, Ahlberg J, Glaros AG, et al. Bruxism defined
and graded: an international consensus. J Oral Rehabil
2013;40(1):24.
2. Lobbezoo F, Ahlberg J, Manfredini D, Winocur E. Are
bruxism and the bite causally related? J Oral Rehabil
2012;39(7):489501.
3. Manfredini D, Lobbezoo F. Role of psychosocial factors in the
etiology of bruxism. J Orofac Pain 2009;23(2):15366.
4. Manfredini D, Winocur E, Guarda-Nardini L, Lobbezoo F.
Epidemiology of bruxism in adults: a systematic review of the
literature. J Orofac Pain 2013;27(2):99110.
5. Manfredini D, Restrepo C, Diaz-Serrano K, Winocur E,
Lobbezoo F. Prevalence of sleep bruxism in children: a systematic
review of the literature. J Oral Rehabil 2013;40(8):63142.
6. Manfredini D, Poggio CE, Lobbezoo F. Is Bruxism a Risk Factor
for Dental Implants? A Systematic Review of the Literature.
Clin Implant Dent Relat Res 2012.
7. Lobbezoo F, van der Zaag J, van Selms MK, Hamburger HL,
Naeije M. Principles for the management of bruxism. J Oral
Rehabil 2008;35(7):50923.
About the Authors
Dr. Kelvin I. Afrashtehfar is a member of the faculty in the department
of Restorative Dentistry, at McGill University in Montreal, Canada.
Dr. Daniele Manfredini is a member of the department of Maxillofacial
Surgery at the University of Padova in Italy.
Five Things to Know
About Bruxism
Kelvin I. Afrashtehfar, DDS, FADI
Daniele Manfredini, DDS, PhD
Volume 84, Number 4 26
Introduction
In the practice of dentistry, the dentist and the dental team are
utilizing ultrasonic and sonic scalers, prophylactic polishing
angles, low- and high-speed handpieces, air polishers and air
abrasion devices to conduct both preventive and restorative
procedures on their patients. When conducting these procedures
in the dental operatory, small particles are generated which
combine with oral microbes, food debris, saliva and blood in the
patients mouth, causing an aerosol or splatter to occur outside
of the oral cavity in the operatory environment. In this article,
the transmission of bacteria, rationale for preprocedural rinsing,
research published on the use of antimicrobial agents such as
chlorhexidine gluconate, essential oils and cetylpyridinium
chloride will be discussed. The importance of preprocedural
rinsing in reducing salivary bacterial load and microorganisms in
saliva and aerosols generated during dental procedures should be
taken into consideration in the dental office.
Transmission of Microorganisms in the Dental Operatory
Current infection control procedures in the dental office include
the use of face masks, plastic eye shields/loupes, gloves and wearing
lab coats over scrubs or professional attire to assist in providing
barriers for transmission of microorganisms. When conducting
dental procedures, an aerosol can occur. This is a mist of particles
that are less than 50 micrometers in diameter and may stay in the
operatory air or evaporate into smaller invisible particles. Splatter
can also occur, which consists of larger droplets that may be more
than 50 micrometers in diameter and can spread to the dental
practitioners lab coat/uniform, eyewear, mask, skin or operatory
surfaces. Aerosol and splatter contain airborne or bloodborne
pathogens.
14
The greatest airborne infection threat in dentistry
is from aerosols, due to their ability to stay airborne and their
potential to enter respiratory passages.
57
Microorganisms included
in dental aerosols have been associated with respiratory infections,
hepatitis, tuberculosis, conjunctivitis, herpes lesions and other skin
infections.
2,3
The prevalence of Streptococcus and Staphylococcus
bacteria in the air after dental surgery has been cited.
8,9
The most intensive aerosol and splatter occurs during work
with an ultrasonic and power scaler tip, the bur on a high-
speed handpiece and with air polishers.
1014
Another study
reported that when ultrasonic scalers are used, even in the
absence of coolant water, there is aerosolization of material
from the operative site.
11,18
Research, utilizing a dye expulsion,
has confirmed the potential for retracting oral fluids in the
internal compartments of the high-speed handpiece.
1517
In
dental aerosols, there are elements of saliva, nasopharyngeal
secretions, plaque, blood, tooth components and material used
in dental procedures.
1820
Preprocedural Rinsing in Dentistry
Preprocedural rinsing is defined as using an antimicrobial
agent for a period of 30 to 60 seconds as a mouthrinse prior
to a dental preventive or restorative procedure. The rationale
for incorporating preprocedural rinsing prior to dental and
dental hygiene appointments is to decrease salivary bacterial
load in the mouth, thereby decreasing bacterial microorganisms
incorporated into the dental aerosol or splatter that occurs
during these procedures.
Antimicrobial Agents Used in Preprocedural Rinsing
Chlorhexidine GluconateChlorhexidine gluconate (CHX) is
a cationic bis-biguanide that has a broad antimicrobial activity
against a wide variety of Gram-positive and Gram-negative
supragingival and subgingival plaque microorganisms and
fungi.
21,22
It can reduce plaque, dental caries and gingivitis
and binds to sites in the oral cavity and is slowly released over
seven hours, restricting bacterial growth.
21
CHX will rupture
the bacterial cell walls and the loss of the cytoplasm results in
cell death.
23
In one study, CHX reduced salivary bacterial load by 97%
and continued for 60 minutes after scaling and root planning;
aerobic bacteria at 30 and 60 minutes were reduced 77%
compared to control.
24
Eapen cited statistically higher
reductions in both aerobic and anaerobic counts for CHX
versus cetylpyridinium chloride (CPC) and fluoride and normal
saline at 2 minutes, 30 minutes and one hour postrinse, but
not statistically significantly different at the 2 minute anaerobic
count.
25
After a single rinse, salivary bacterial counts remained
Preprocedural Rinsing in the Dental
Office: A Consideration for Improved
Infection Control Among the Dental
Team and Patients
Christine A. Hovliaras, RDH, BS, MBA, CDE
27 Volume 84, Number 4
reduced up to 90 minutes for CPC and 5 hours for CHX.
26
In another study, Balbuena et al. studied the efficacy of
essential oils (EO) and CHX on salivary counts in healthy
adults. Both mouthrinses significantly reduced aerobic and
anaerobic bacterial counts 1 hour following their use. At
4 hours, CHX continued to produce an 85% reduction in
bacteria and the EO was no more effective than rinsing with
a normal saline solution.
27
Briner et al. compared CHX to EO on salivary bacterial counts;
both rinses were equally effective at 30 minutes. However, CHX
was more effective at 3 hours and at 5 hours after rinsing than the
EO.
28
The use of CHX and EO-containing mouthrinse for one
minute before a dental procedure has been shown to significantly
reduce the bacterial load and contamination of the operative area
and staff.
29
Feres et al. reported that a 0.05% CPC mouthrinse, when used as a
preprocedural mouthrinse, was equally effective as CHX in reducing
the levels of splatter bacteria generated during ultrasonic scaling.
30
Suresh et al. showed that one minute of preprocedural rinsing
with 0.2% of CHX before dental procedures consistently reduced
colony-forming units (CFU) as compared to prerinsing with an EO-
containing mouthrinse.
31
Essential Oilsinclude four active compounds derived from
essential oils contained in a currently marketed EO mouthrinse:
0.063% thymol, 0.091% eucalyptol, 0.02% menthol with
0.0660% methyl salicylate.
21,32
EO have strong evidence to
support efficacy in reducing plaque and gingivitis.
21,33
These
essential oils kill microorganisms by disrupting their cell
membranes and inhibiting enzyme activity.
21,34
The EOs
prevent bacteria from aggregating with Gram-positive
pioneer species, slow bacterial multiplication and extract
endotoxins from Gram-negative pathogens which reduces
bacterial load.
21,35
Rinsing with the EO antiseptic mouthrinse produced a 94.1%
reduction in recoverable CFU compared with the non-rinse
control. The non-rinse control treatment produced a 33.9%
reduction in CFU.
36
Preprocedural rinsing with an EO
mouthrinse resulted in a 93.6% reduction in recoverable counts
in aerosols generated 40 minutes after rinsing.
37
DePaola et
al. reported that an EO mouthrinse produced a 60 to 65%
reduction in intraoral salivary bacteria (aerobic, anaerobic,
Streptococci, Veillonella sp) from baseline at 2 minutes; the
significant decreases were sustained up to 60 minutes. Total
EO group aerobic, anaerobic and Streptococcal counts were
significantly lower than the placebo group.
38
Another study by Fine et al. reported the results of two clinical
studies that were conducted to determine the efficacy of a mint
flavored EO mouthrinse on the level of viable bacteria recovered
from dental aerosols immediately after rinsing and then 40
minutes after rinsing. In the first study, the mint flavored
mouthrinse group resulted in a 92.1% reduction in viable bacteria
in aerosols immediately after rinsing, as compared to a control
rinse.
39
In the second study, the mint flavored EO mouthrinse
group produced a 91.3% reduction in viable bacteria in aerosols
40 minutes after rinsing, as compared to a control rinse. These
studies suggest that preprocedural rinsing with a mint flavored EO
mouthrinse may potentially reduce the risk of cross contamination
in the dental operatory.
39
Cetylpyridinium Chloride (CPC)is a quarternary ammonium
compound that is a cationic agent that will interact with the cell
membrane of bacteria, affecting its permeability and resulting in
the loss of cell contents, interference with cellular metabolism,
inhibition of cell growth and cell death.
21,40,41,42,43
CPC has been
shown to inhibit the co-aggregation of bacteria, absorb to pellicle-
covered enamel and inhibit co-adhesion of bacteria.
44, 45, 46
A mouthrinse containing 0.05% CPC and 0.05% sodium
fluoride was compared to a control mouthrinse containing 0.05%
sodium fluoride to control supragingival plaque bacterial counts
for 12 hours after a single treatment and 12 hours after 14 days
use. The CPC mouthrinse significantly reduced supragingival
plaque bacteria counts by 35.3% and 70.9% compared to the
control fluoride mouthrinse 12 hours after a single use and
after 14 days of use, respectively
.47
Other studies have exhibited
significant reductions in salivary aerobic and/or anaerobic
bacterial counts for up to seven hours following a single rinse
with a CPC-containing product.
26,46,48,49
Schaeffer et al. reported that a new mouthrinse formulation
containing 0.075% CPC and 0.05% sodium fluoride with and
without alcohol statistically significantly reduced bacteria levels
(Actinobacillus actinomycetemcomitans and Streptococcus mutans) by
greater than 99.9% after a 30 second exposure.
50
As mentioned previously, Feres et al. reported that a 0.05% CPC
mouthrinse when used as a preprocedural mouthrinse was equally
effective as CHX in reducing the levels of splatter bacteria generated
during ultrasonic scaling.
30
Discussion
The Centers for Disease Control and Prevention (CDC)
have indicated that dental aerosols should be controlled to
the greatest extent possible.
51,52
The CDC reports there is no
scientific evidence that indicates that preprocedural mouth
rinsing prevents clinical infections among patients or dental
healthcare professionals. However, a possible association
between the spread of oral microorganisms in the dental
office and the development of infectious diseases such as
ophthalmic or acute respiratory infections and tuberculosis
can occur.
1719,30
Studies have shown that a preprocedural rinse with a product
containing an antimicrobial product (chlorhexidine gluconate,
essential oils, povidine iodine) can reduce the level of oral
microorganisms generated in aerosols or splatter during routine
dental procedures with dental handpieces and ultrasonic
scalers.
36,37,39,5358
In 1997, the American Heart Association
(AHA) suggested that patients at risk for bacterial endocarditis
use an antimicrobial mouthrinse before dental treatment.
Now, however, the AHA does not list preprocedural rinsing
Volume 84, Number 4 28
in their bacterial endocarditis guidelines.
59
The CDC reports
that preprocedural mouthrinses can be most beneficial
before procedures (ultrasonic scaling, rubber cup prophylaxis
polishing) where a rubber dam cannot be used to minimize
aerosol and splatter.
22,60
The use of a high volume evacuator
should be used with ultrasonic or power scaling devices to
control aerosols and splatter.
18
The information discussed on the antimicrobial agents (CHX,
EO and CPC) in this article will assist the dentist in choosing
the proper mouthrinse to consider for a preprocedural rinsing
protocol in practice. The dentist should determine the
advantages and disadvantages of these agents to provide the
clinical and scientific efficacy to reduce salivary bacterial load
and aerosolized bacteria in the dental operatory. Selecting a
product that is easy to purchase (prescription vs. over-the-
counter), cost effective (using the mouthrinse with every
patient), tastes pleasant (flavor is appealing to patients), and does
not produce an aftertaste or burning sensation after rinsing will
provide the best solution.
Conclusion
The implementation of a preprocedural rinsing program in the
dental or specialty practice can assist in reducing bacterial salivary
load in patients mouths and limit aerosolized bacteria and splatter
in the dental operatory for a healthier office environment for the
entire dental team.
References
1. Micik RE, Miller RI, Mazzarella MA, Ryge G. Studies on dental
aerobiology, I: bacterial aerosols generated during dental procedures.
J Dent Res 1969; 48(1): 4956.
2. Miller RL, Micik RE, Abel C, Ryge G. Studies of dental aerobiology
II:microbial splatter discharged from the oral cavity of dental patients.
J Dent Res 1971;50:6215.
3. Micik RE, Miller RL, Leong AC. Studies on dental aerobiology,
III: efficacy of surgical masks in protecting dental personnel
from airborne bacterial particles. J Dent Res 1971;50:62630.
4. Abel LC, Miller RL, Micik RE, Ryge G. Studies on dental aerobiology,
IV: bacterial contamination of water delivered by dental units. J Dent
Res 1971;50:15679.
5. Hinds WC. Aerosol technology: Properties, behavior, and measurement
of airborne particles. New York: Wiley;1982:68.
6. Cottone IA, Terezhalmy GT, Molinari JA. Practical infection control in
dentistry. Baltimore: Williams & Wilkins;1996:13940.
7. Crawford JJ, Broderius C. Control of cross-infection risks in the dental
operatory: preventon of water retraction by bur cooling spray systems. J
Am Dent Assoc 1988;116:6857.
8. Osorio R, Toledano M, Liebana J, Rosales JI, Lozano JA.
Environmental microbial contamination. Pilot study in a dental
surgery. Int Dent J 1995, 45: 352357.
9. Szymanska J. Dental bioaerosol as an occupational hazard in a dentists
workplace. Am Agric Environ Med 2007;14:203207.
10. Bennett AM, Fulford MR, Walker JT, Bradshaw DJ, Martin MV,
Marsh PD. Microbial aerosols in general dental practice. Br Dent J
2000, 189: 664667.
11. Harrel SK, Barnes JB, Rivera-Hidalgo F. Aerosol and splatter
contamination from the operative site during ultrasonic scaling. J Am
Dent Assoc 1998;129:12411249.
12. Leggat PA, Kedjarune U. Bacterial aerosols in dental clinic: review. Int
Dent J 2001;51:3944.
13. Mills SE, Kuehne JC, Bradley DV Jr. Bacteriological analysis of high-
speed handpiece turbines. J Am Dent Assoc 1993;124:5962.
14. Perry DA, Bird WF, Armitage GC. Aerosol management policy for
powered scalers. CDHA J 2002;18:11720.
15. Lewis DL, Arens M, Appleton SS, et al. Crosscontamination potential
with dental equipment. Lancet 1992;340:12524.
16. Lewis DL, Boe RK. Crossinfection risks associated with current
procedures for using high-speed dental handpieces. J Clin Microbiol
1992;30:4016.
17. Checchi L, Montebugnoli L, Samaritani S. Contamination of the
turbine air chamber: a risk of cross infection. J Clin Periodontol
1998;25:60711.
18. Harrel SK, Molinari J. Aerosols and splatter in dentistry: A brief
review of the literature and infection control implications. JADA
2004;135(4): 429437.
19. King TB, Muzzin KB, Berry CW, Anders IM. The effectiveness
of an aerosol reduction device for ultrasonic scalers. J Periodontol
1997;68(1): 459.
20. Logothetis DD, Gross KB, Eberhart A, Drisko C. Bacterial airborne
contamination with an air-polishing device. Gen Dent 1988; 4969.
21. Hovliaras CA. SAVVY SUCCESS: Achieving professional excellence
and career satisfaction in the dental hygiene profession, Volume II:
Patient care. Charles C, Santos S, Morris A. Chapter 29: Role of daily
use mouthrinses in maintaining oral health. Indiana; Authorhouse;
2012:245262.
22. Stanley A, Wilson M, Newman H. The in-vitro effect of chlorhexidine
on subgingival plaque bacteria. J Clin Periodontol 1989;16(4):254264.
23. Kaplowitz G, Collins FM. Preprocedural rinsing: A preemptive
protocol. Available at: http://www.ineedce.com/courses/1478/PDF/
PreProceduralRinsing.pdf. Accessed on September 15, 2013.
24. Veksler AE, Kayrouz GA, Newman MG. Reduction of salivary bacteria
by pre-procedural rinses with chlorhexidine 0.12%. J Periodontol
1991;62(11):64951.
29 Volume 84, Number 4
25. Eapen T. Efficacy of two commonly available mouth rinses used
as preprocedural rinses in children. J Ind Soc Pedo Prevent Dent
2011;29(2): 113116.
26. Roberts WR, Addy M. Comparison of the in vivo and in vitro
antibacterial properties of antiseptic mouthrinses containing
chlorhexidine, alexidine, cetyl pyridinium chloride and
hexetidine. Revelance to mode of action. J Clin Periodontol
1981;8(4):295310.
27. Balbuena I, Stambaugh KI, Ramirez SG, Yeager C. Effects of
topical oral antiseptic rinses on bacterial counts of saliva in
healthy human adults. Otolaryngol Head Neck Surg
1998;118(5):625629.
28. Briner WW, Kayrouz GA, Chanak MX. Comparative antimicrobial
effectiveness of a substantive (0.12% chlorhexidine) and a
nonsubstantive (phenolic) mouthrinse in vivo and vitro. Compendium
1994;15(9):1158, 1160, 1162.
29. Worral SF, Knibbs PJ, Glenwright HD. Methods of reducing bacterial
contamination of the atmosphere arising from use of an airpolisher. Br
Dent J 1987;163:1189.
30. Feres, M, Figueiredo LC, Faveri M, Stewart B, DeVizio W. The
effectiveness of a preprocedural mouthrinse containing cetylpyridinium
chloride in reducing bacteria in the dental office. JADA 2010;141(4):
415422.
31. Suresh S, Manimegalai M, Sudhakar U, Sopia. Comparison
of efficacy of preprocedural rinsing with chlorhexidine and
essential oil mouthwash in reducing viable bacteria in dental
aerosolsA microbiological study. Int J Contemp Dent
2011;2(6):16.
32. Department of Health and Human Services. Oral health care drug
products for over-the-counter human use; antigingivits/antiplaque
drug products; establishment of a monograph; proposed rules.
Part III. Food and Drug Administration. Federal Register
2003;68(103):3224132243.
33. Van Leeuwen MPC, Slot DE, Van der Weijden GA. Essential oils
compared to chlorhexidine with respect to plaque and parameters
of gingival inflammation: A systemic review. J Periodontol
2011;82(2):174194.
34. Fine DH, Furgang D, Lieb R, Korik I, Vincent JW, Barnett ML. Effect
s of sublethal exposure to an antiseptic mouthrinse on representative
plaque bacteria. J Clin Periodontol 1996;23(5): 444451.
35. DePaola LG, Overholser CD, Meiller TF, Minah GE, Niehaus C.
Chemotherapeutic inhibition of supragingival dental plaque and
development. J Clin Periodontol 1985;12:697704.
36. Fine DH, Mendieta C, Barnett ML, Furgang D, Meyers R,
Olshan A, Vincent J. Efficacy of preprocedural rinsing with an
antiseptic in reducing viable bacteria in dental aerosols. J Periodontol
1992;63(10)8214.
37. Fine DH, Yip J, Furgang D, Barnett ML, Olshan AM, Vincent J.
Reducing bacteria in dental aerosols: pre-procedural use of an antiseptic
mouthrinse. JADA 1993;124(5)L568.
38. DePaola LG, Minah GE, Overholser CD, Meiller TF, Charles CH,
Harper DS, McAlary M. Effect of an antiseptic mouthrinse on salivary
microbiota. Am J Dent 1996;9(3):935.
39. Fine DH, Furgang D, Korik I, Olshan A, Barnett ML, Vincent JW.
Reduction of viable bacteria in dental aerosols by preprocedural rinsing
with an antiseptic mouthrinse. Am J Dent 1993;6(5):21921.
40. ten Cate JM, Marsh PD. Procedures for establishing efficacy of
antimicrobial agents for chemotherapeutic caries prevention. J Dent Res
1994; 73(3):695703.
41. Scheie A. Modes of action of currently known chemical anti-plaque
agents other than chlorhexidine. J Dent Res 1989;68(Spec Iss):160916.
42. McDonnell G, Russell AD. Antiseptics and disinfectants: activity,
action, and resistance. Clin Microbiol Rev 1999;12:14779.
43. Gilbert P, Moore LE. Cationic antiseptics: diversity of action under a
common epithet. J Applied Micro 2005;99:70315.
44. Smith RN, Andersen RN, Kolenbrander PE. Inhibition of intergeneric
coaggregation among oral bacteria by cetylpyridiunium chloride,
chlorhexidine digluconate and octenidine dihydrochloride. J Periodontol
Res 1991;26: 4228.
45. Busscher HJ, White DJ, Atema-Smith J, Geertsem a-Doornbusch
G, de Vries J, van der Mei HC. Surfacttive and antibacterial activity
of cetylpyridium chloride formulations in vitro and in vivo. J Clin
Periodontol 2008;35:54754.
46. Williams MI. The antibacterial and antiplaque effectiveness of
mouthwashes containing cetylpyridinium chloride with and without
alcohol in improving gingival health. J Clin Dent 2011;22[Spec
Iss]:179182.
47. Hu D, Li X, Sreenivasan PK, DeVizio W. A randomized, double-blind
clinical study to assess the antimicrobial effects of a cetylpyridium
chloride mouth rinse on dental plaque bacteria. Clin Ther
2009;31:25408.
48. Jenkins S, Addy M, Wade W, Newcombe RG. The magnitude and
duration of the effects of some mouthrinse products on salivary
bacterial counts. J Clin Periodontol 1994;21:397401.
49. Elworthy A, Greenman J, Doherty FM, Newcombe RG, Addy M.
The substantivity of a number of oral hygiene products determined
by the duration of effects on salivary bacteria. J Periodontol
1996;67:5726.
50. Schaeffer LM, Szewczyk G, Nesta J, Vandeven M, Du-Thumm
L, Williams MI, Arvanitidou E. In vitro antibacterial efficacy of
cetylpyridinium chloridecontaining mouthwashes. J Clin Dent
2011;22[Spec Iss]:1836.
Volume 84, Number 4 30
51. Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection
control in dental health-care settings2003. MMWR Recomm Rep
2003;52(RR17):161.
52. Centers for Disease Control and Prevention. Infection control in
dental settings. Frequently asked questionspreprocedural mouth
rinse. Available at: http://www.cdc.gov/oralhealth/infectioncontrol/faq/
preprocedural_mouthrinse.htm. Accessed on September 30, 2013.
53. Litsky BY, Mascis JD, Litsky W. Use of an antimicrobial mouthwash
to minimize the bacterial aerosol contamination generated by the high-
speed drill. Oral Surg Oral Med Oral Pathol 1970;29:2530.
54. Mohammed CI, Monserrate V. Preoperative oral rinsing as a means of
reducing air contamination during use of air turbine handpieces. Oral
Surg Oral Med Oral Pathol 1970;29:2914.
55. Wyler D, Miller RL, Micik RE. Efficacy of self administered preoperative
oral hygiene procedures in reducing the concentration of bacteria in
aerosols generated during dental procedures. J Dent Res 1971;50:509.
56. Muir KF, Ross PW, MacPhee IT, Holbrook WP, Kowolik MJ.
Reduction of microbial contamination from ultrasonic scalers. Br Dent
J 1978;145:768.
57. Logothetis DD, Martinez-Welles JM. Reducing bacterial aerosol
contamination with a chlorhexidine gluconate pre-rinse. JADA
1995;126:16349.
58. Klyn SL, Cummings DE, Richardson BW, Davis RD. Reduction of
bacteria-containing spray produced during ultrasonic scaling. Gen Dent
2001; 49:64852.
59. Wilson W, Taubert KA, Gewitz M, Lockhart BP, et al. Prevention of
infective endocarditis: guidelines from the American heart association.
Circulation 2007;116:17361754.
60. Costello MR. Dental dams: the secret tool for infection control.
Compend Contin Educ Dent 2006;27(3):1969.
About the Author
Christine A. Hovliaras, RDH, BS, MBA, CDE, is president of
Professional Savvy, LLC, an oral care consulting, professional
marketing and continuing education company in New Jersey.
Christine is a dental hygiene professional with over 29 years
experience in the dental profession and works for Dr. Marc
Appelbaum in Morristown, NJ. The authors honorarium for
production of this article was supported by an unrestricted
educational grant from Colgate-Palmolive.
With its unmatched record of successes in dental practice transitions, dont
you owe it to yourself to discover why more than 3,600 dental professionals
have turned to The Clemens Group to get them the highest possible valuations
for their practices?
Clemens professionals are there to guide and support you every step of the
way with the understanding, expertise, and integrity you deserve from the area
leader in dental practice sales.
Call today for a confidential, complimentary consultation and see the differ-
ence a second opinion can make.
THINKING OF SELLING YOUR PRACTICE?
GET A SECOND OPINION FIRST.
Visit us at
TheClemensGroup.com
or call us toll-free at
1-800-300-2939
Founding member, American Dental Sales
All ADS companies are independently owned and operated
Listed ADA Dental Practice Appraiser and Valuator
Founding member, National Practice Valuation Study Group
31 Volume 84, Number 4
(Just before the last recession) in 2007, the number
of dental establishments throughout the state had
increased to 4,618 facilities (from 4,380 in 2001)
with a continuing decrease in population to
1,880 residents per establishment (compared to
2,385 nationally). The number of employees per
average establishment increased to 6.2 individuals
(comparable to 6.3 nationally).
2
This was the summary statement in an earlier presentation in the
JNJDA just before the onset of the last recession. The Business
Cycle Dating Committee of the National Bureau of Economic
Researchdetermined thatthe recession that began in December
2007 (had ended) in June 2009. The recession lasted 18 months,
which makes it the longest of any recession since World War II.
3
Reports from the Census Bureaus annual study of business patterns
for each county and state (with specific information on numbers
of establishments, employees and salaries) permit a review of
these differences. (See the Legend section for the definition of an
establishment.)
Evolving Practice Configurations
In 2013, the ADAs Health Policy Resources Center suggested
very strongly that the dental economy is in a major transition
New Jersey Dental Establishments in
2011: After the Last Recession
H. Barry Waldman, DDS, MPH, PhD
30 years experience serving the
dental community!
Providing quality insurance products, at com-
pettve prices, with outstanding customer ser-
vice; this is our business philosophy. You, our
clients, are our primary concern.
The Insurance Agency for Dentsts, LLC
Bob Opperman
609-492-5608/215-990-6709
Fax: 609-492-5609
Email: dentstsinsagt@gmail.com
MY PROFESSION IS
YOUR PROTECTION!
Volume 84, Number 4 32
Dental spending has not rebounded since the end of the Great
Recession and has been stagnant, on a per capita basis, since 2008
the declines in both dental spending and visits predate the economic
crisis of 2008.
4
In light of these findings, the changes in business
patterns for the delivery of dental services were considered.
NationallyBetween 2007 and 2011 there was an increase of
almost five thousand dental establishments, including almost 2,300
small establishments (less than 5 employees) and almost 2,050
establishments with 59 employees. (See the Legend section for the
definition of employees.) Nevertheless, in this recent period just before
the last recession and a couple of years after the end of the recession, as
the nation struggled to overcome the impact of the recession:
The proportion of the dental establishments with less than five
employees remained essentially unchanged (at approximately
40%). In the past, between 1990 and 2001, these small
establishments decreased from 54.9% to 43.4% of all dental
establishments.
2
(Table 1).
The increase of almost five thousand dental establishments between
2007 and 2011 mirrored the general national population increases.
As a result, there was only a slight decrease in the population per
dental establishment from 2,401 to 2,376 individuals.
New JerseyBetween 2007 and 2011 there was an increase of 102
dental establishments, with the largest increase in the number of 59
employee dental establishments. During this period, there was limited
change in the proportional representation of small establishments
(46%). Similarly, during this period, there were very limited changes in
the: 1) number of employees per average dental establishment (from
6.1 to 6.2 employees), and 2) population per dental establishment at
the overall state level (from 1,880 residents per establishment in 2007
to 1,862 residents per establishment in 2011).
5
In 2011, the average
salary of a dental establishment employee was $43,800. (Table 2) (See
Legend section for definition of average.)
Legend
An establishment is a single physical location where services are
performed. It is not necessarily identical to a company or enterprise,
which may consist of one or more establishments. In addition,
one or more practitioners may be present in an establishment.
Throughout this presentation, (except where specified) the term
dental establishment refers to those facilities 1) with employees
and 2) subject to federal income tax. Government agency programs
(hospitals and health department clinics) are not included.
Employees may include dentists, dental hygienists, dental assistants,
office staff, etc.
Average dental establishment While there is no such thing
as an average dental establishment, comparisons between
averages (over time and between locales) do provide a picture
Dr. Gordon Christensen - Im
plant Prosthodontics - 2014
Dr. Uche Odiatu - The M
iracle of Health
AAFE - Botox Use In Dentistry - Lecture and Hands On, Part I
Hiossen - AIC Basic Im
plant Course - Part I
Dr. Rella Christensen - W
hat's New in Caries, Restoratives, Laser Perio
and Infection Control
Dr. Sam
uel B. Low - Successful M
anagem
ent of Periodontal Patient
AAFE - Derm
al Fillers In Dentistry - Hands On, Part II
Hiossen - AIC Basic Im
plant Course - Part II
Dr. Harold L. Crossley - The Real Deal About Street Drugs and Their Effects on You, Your Friends, and Your Dental Practice
Dr. John H. Tucker - Dental Sleep M
edicine
Dr. Leonard F. Tau - 21
st
Century M
arketing: Using the Power of the Internet and Social M
edia to Step Up Your Practice
Hiossen - AIC Basic Im
plant Course - Part III
P
ennsylvanias P
rem
iere D
ental C
o
nference
S
T
E
P
P
IN
G
U
P
Y
O
U
R
P
R
A
C
T
IC
E
w
ith
a
little
h
e
lp
fro
m
y
o
u
r frie
n
d
s
2
8
T
H
A
N
N
U
A
L
V
A
L
L
E
Y
F
O
R
G
E
D
E
N
T
A
L
C
O
N
F
E
R
E
N
C
E
M
a
rk
Y
o
u
r C
a
le
n
d
a
r fo
r th
e
...
M
A
R
C
H
5
-
6
-7
, 2
0
1
4
V
A
L
L
E
Y
F
O
R
G
E
R
A
D
IS
S
O
N
H
O
T
E
L
K
IN
G
O
F PR
U
SSIA, PA
R
E
G
IS
TR
ATIO
N
N
O
W
O
P
E
N
AT:
w
w
w
.v
fd
c
.o
r
g
800-854-V
FD
C
CERP & PDHA Accredited Seminars
PA CE Requirements
Cutting Edge Courses for Doctors & Staff
Exhibit Hall Featuring 52 Companies
W
E
D
N
E
S
D
A
Y
, M
A
R
C
H
5
, 2
0
1
4
T
H
U
R
S
D
A
Y
, M
A
R
C
H
6
, 2
0
1
4
F
R
ID
A
Y
, M
A
R
C
H
7
, 2
0
1
4
33 Volume 84, Number 4
of the evolving practice of dentistry. The average number of
employees in New Jersey was determined by dividing the total
number of dental employees (29,374) by the number of dental
establishments (4,720). The average salary was determined
by dividing the total annual state payroll figure for dental
establishment employees ($1,285,677,000) by the total number
of employees (29,374 individuals).
Number of Employees at the County Level
In 2011, there were 29,374 employees in dental establishments in
New Jersey (almost 855,000 nationally). The number of employees
in average dental establishments in New Jersey counties ranged
from a low of 5.0 employees in Bergen County to 10.9 employees in
Cumberland County. (Table 2)
Average Salary at the County Level
Statewide, the average employee salary was $43,800 (nationally,
$45,200). Average employee salaries ranged from $34,800 in
Hudson County to $55,700 in Mercer County. (Table 2) (Again, it
should be noted, that employees may include dentists.)
Dental Establishments With No Employees
In 2010, there were an additional 1,588 New Jersey dental
establishments that were subject to federal income tax but with no
employees. These non-employee dental facilities represented one-
quarter of the total number of dental establishments in the state in
2010 (i.e., 4,720 dental establishments with employees plus 1,588
establishments with no employees). The New Jersey dental facilities
with no employees in 2010 reported a total of $138 million in gross
receipts ($86,900 per establishment). Nationally, in 2010 there were
40,897 dental establishments with no employees that reported more
than $3.1 billion in gross receipts (an annual average of $75,800 in
gross receipts per establishment).
During 2010, in New Jersey, most nonemployee dental
establishments were individual proprietorships with average
annual gross receipts of $72,400. A smaller number of corporate
arrangement facilities had average annual gross receipts of $177,200;
a few partnerships had average annual gross receipts of $329,000.
8
Given the increasing numbers of employees per dental establishment
with employees, how does one account for the great number of
facilities with no employees? It was suggested in a previous review
that nonemployee establishment arrangements might include:
Recent graduates just starting practices.
Older practitioners who are decreasing their time commitment
to practice as they prepare for eventual retirement.
An establishment that serves as a secondary activity for an
individual who works full-time for someone else.
Contracts with independent outside firms for auxiliary personnel.
Use of family members as auxiliary personnel and where no
reports are made for Social Security and income tax purposes.
Establishments of independent corporate arrangements for in-
house auxiliaries.
Any number of other alternative practice arrangements
(including practice in private homes and other locations) that do
not file required quarterly payroll tax reports.
9
Overview: 20072011
Between 2007 and 2011:
The number of dental establishments has increased nationally
and in New Jersey (albeit at a slower rate than in previous periods).
The population per dental establishment in New Jersey
decreased to a very limited extent.
The number of employees per average establishment in New
Jersey has remained constant.
Nationally and in New Jersey, the proportional representation of
small dental establishments has remained stable.
Nevertheless, in light of the ADA economic report regarding
the stagnation of dental economics, continued monitoring of
generalized dental establishment business activities beyond the
confines of a single facility is essential, and does provide an
appreciation of developments that affect the profession in general
and in particular, your establishment.
Hows Your Practice Doing?
Now that youve compared your personal dental establishment
numbers to those of the average establishment in your county,
remember: there is no such thing as an average dental establishment.
The particular requisites of your community determine business
events in your establishment, including employment patterns,
employee salaries and the like. Unfortunately, information from
various government agency and professional association reports does
not provide data for the numerous particular locales.
Table 1. Distribution of dental employees by size of dental
establishments. New Jersey and the United States: 2007, 2011
5
Note: Differences in percentage totals are due to rounding
5
Table 1. Distribution oI dental employees by size oI dental establishments
New Jersey and the United States: 2007, 2011
5
New Jersey United States
Number oI establishments Number oI establishments
Number oI Number Number
employees 2007 2011 change 2007 2011 change
1-4 2,164 2,198 34 50,893 53,191 2,298
5-9` 1,606 1,685 79 50,662 52,711 2,049
10-19 709 689 - 20 21,421 21,646 225
20-49 130 143 13 3,204 3,392 188
50 9 5 - 4 212 239 27
Total 4,618 4,720 102 126,392 131,179 4,787
Employees
per establish. 6.1 6.2 6.5 6.5
Percent distribution oI establishments
1-4 46.9 46.5 40.2 40.6
5-9 34.8 35.7 40.0 40.1
10-19 15.4 14.6 16.9 16.5
20-49 2.8 3.0 2.5 2.5
50 0.1 0.1 0.1 0.1
Total 100 100 100 100
Note: DiIIerences in percentage totals are due to rounding
Volume 84, Number 4 34
Table 2. New Jersey dental establishments with payrolls. Number and
salary of employees and population per establishment and county (week
of March 12, 2011)
57
References
1. Waldman HB. Dental establishments in New Jersey. JNJDA
2004;75(Winter):3436.
2. Waldman HB. Update on dental establishments in New Jersey. JNJDA
2009;80(Winter):2728.
3. The Business Cycle Dating Committee of the National Bureau of
Research. The recent recession. Web page: http://www.nber.org/cycles/
sept2010.html Accessed May 8, 2013.
4. American Dental Association, National dental sending flat since 2008. April
18, 2013. Web site: http://www.noodls.com/view/3F1A30966AA6C833A799
B7C0BBD4A768C8534A05?9531xxx1366388107 Accessed April 23, 2013.
5. U.S. Census Bureau. County Business Patterns: 2011. Web site: http://
censtats.census.gov/cgi-bin/cbpnaic/cbpdetl.pl Accessed May 2, 2013.
6. Fenney TC. NJ Press. New Jersey population inched up in 07.
Web site: http://www.nj.com/news/index.ssf/2007/12/new_jersey_
population_inched_u.html Accessed May 10, 2013.
7. State of New Jersey. Department of Labor and Workforce Development
of Labor. Estimate of county population by age and sex, New Jersey,
2010-2011. Web site: http://lwd.dol.state.nj.us/labor/lpa/dmograph/
est/cnty06/cntysumm11.xls Accessed May 10, 2013.
8. Census Bureau. 2010 Nonemployee statistics. Web site: http://censtats.
census.gov/cgi-bin/nonemployer/nondetl.pl Accessed May 5, 2013.
9. Waldman HB, Cannella D. Mapping dental establishment in New York State
just before the recession. New York State Dental Journal 2010:76:2225.
About the Author
H. Barry Waldman, DDS, MPH, PhD, is a distinguished teaching
professor in the Department of General Dentistry, School of Dental
Medicine at Stony Brook University in New York.
6
Table 2. New Jersey dental establishments with payrolls. Number and salary oI employees and
population per establishment and county (week oI March 12, 2011)
5-7
Average Average Resident
State & Number oI Number oI employees number salary per population
County establishments 1-4 5-9 10-19 20 employees employee per establishment
(in 000s)
Statewide 4,720 2,198 1,685 689 148 6.2 $43.8 1,862
Atlantic 94 28 37 20 9 8.8 44.7 2,918
Bergen 781 443 255 73 10 5.0 43.7 1,166
Burlington 176 62 66 35 13 8.2 46.5 2,554
Camden 227 91 80 41 15 7.3 42.4 2,260
Cape May 38 15 14 8 1 7.3 45.4 2,542
Cumberland 44 10 14 13 7 10.9 48.2 3,570
Essex 413 216 139 52 6 5.3 42.8 1,901
Gloucester 98 39 15 8 8.1 48.0 2,950
Hudson 268 162 73 29 4 4.8 34.8 2,392
Hunterdon 74 25 36 12 1 6.3 44.0 1,730
Mercer 190 89 66 26 8 6.9 55.7 1,931
Middlesex 416 191 148 67 10 6.2 41.7 1,957
Monmouth 422 170 155 85 12 6.7 42.3 1,495
Morris 366 170 139 46 11 5.9 45.8 1,352
Ocean 237 90 101 35 11 6.9 44.8 2,444
Passaic 224 106 82 31 5 6.1 41.5 2,241
Salem 19 9 7 3 5.5 45.8 3,468
Somerset 226 98 88 34 6 6.0 44.0 1,437
Sussex 60 22 24 12 2 6.9 42.8 2,475
Union 306 149 109 41 7 5.8 43.2 1,763
Warren 303 41 13 16 12 7.4 42.5 2,642
A PARTNERSHIP
OF TRUST
We build on it
everyday.
Mid-Atlantic Insurance Resources is
the endorsed broker for
TDIC to the New Jersey Dental
Association members.
Your coverage will be placed with a leader.
TDIC is the Endorsed Carrier of the
New Jersey Dental Association for Professional
Liability & Ofce Property Insurance.
Copyright Mid-Atlantic Insurance Resources 2011. All Rights Reserved.
Mid-Atlantic Insurance Resources logo is a registered trademark of Mid-Atlantic Insurance Resources.
Call today for a FREE quote.
877 476 4588
www.midatlanticir.com
35 Volume 84, Number 4
I
t may come as no surprise to anyone, but I am the youngest
member of the Passaic County Dental Society. I am also the
youngest member on the Board of Trustees and third in line to
be our next society president. You can say that I got an early start to
getting involved.
Becoming a dentist never made my top ten list of what I wanted
to be when I grew up. Even though I had a father who was a
dentist, becoming a ballerina or a baker seemed much more
appealing to me. As the years passed, I did some maturing,
reached high school and realized medicine was where my future
was headed. I studied hard, got good grades, got accepted to
Georgetown University and started college as a biology major.
Throughout college, various family and friends would hint at
the possibility of applying to dental school. I would usually just
brush it off until one of my fathers dental school classmates sat
me down at a summer barbecue and told me to apply to medical
school but to also apply to just one dental school and then make
my decision. That conversation ended up changing my life and
future career path. I took his advice, took the DATs, applied to
dental school on a whim and got accepted to UMDNJ. Hello
dentistry! Those four years in dental school were the best and
worst years of my life. However, as they say, at the end of every
dark tunnel is a white light. Graduation day, May 16, 2010,
was the happiest day of my life. I felt lucky to have found a
profession that I truly loved and was passionate about. It was
also the happiest day of my fathers life, because he finally found
his exit strategy.
Even before the ink had dried on my diploma, my father talked
to me about joining organized dentistry and the importance of
getting involved and giving back to the profession. My first year
out of dental school I attended every Passaic County Dental Society
meeting and the next year joined the Board of Trustees, alongside
my father; the year after that I became an officer. As you can see, it
did not take much time or effort to suck me in.
So far, my experience with PCDS has been great. I was warmly
welcomed by my fellow colleagues. I have made valuable friendships
and been exposed to many different aspects of the dental world. I
have formed bonds and mentorships with clinicians thirty years my
senior. More importantly, I have found a forum where there is no
stupid question, there is no judgment, and members are there to
mutually support each other. Not only that, they are there to share
their stories and ideas: What worked for them, and what didnt
work so much.
We, PCDS, are known to have one of the most culturally diverse
societies and one of the nicest. We also have many more women
than any other society in New Jersey. Our meetings are not cliquish,
our members are all approachable and inviting and there is always
someone to greet you. There really is the sense of camaraderie and
family at every meeting. More often than not, the conversations are
centered around family, kids, health and sports.
We also cannot forget what organized dentistry has done and
continues to do for us as a profession. We have constant support and
resources from a group of people who advocate for our rights and
best interests as dentists. As an NJDA member, I can call the NJDA
headquarters at any time, pertaining to any issue I may be having in
the office. These include legal issues and/or questions, state board,
advertising, laws governing hygienists, HIPAA, OSHA, insurance
issues, and many, many more. These people have all, for the most
part, been involved in dentistry their entire careers and are here to
provide us with advice and know-how which, in the long run, saves
us time, money, and most importantly, aggravation. All you have to
do is call and they actually return the call!
The bottom line is, I honestly do not understand how anyone in
this present environment can afford to practice without the backing
of organized dentistry. Yes, the economy has changed; yes, practices
are slower; and yes, patients have become more demanding.
However, these are all the more reasons to stick together as peers,
as a profession, and ride out the storm together. There will always
be something that could be better, that could be changed, but I
am happy to be part of an organization that embraces change and
engages conversation for a better tomorrow for you and me.
About the Author
Dena Constandelis, DMD, is a general dentist in practice with her
father, Theodore Constandelis, DDS. Their practice, Constandelis
Dental Family and Aesthetic Dentistry, has been located in Clifton
for more than 30 years. In addition to being involved in organized
dentistry, when she finds the time, Dr. Dena enjoys reading, trying new
restaurants and running.
This guest editorial originally was published in the PCDS newsletter
and is reprinted with permission of the author and the Society.
Opinion:
New Kid on the Block
Dena Constandelis, DMD
Volume 84, Number 4 36
Opportunities Available
Dentist Needed for Space Share in Newly
Renovated Office.
State-of-the-art, recently remodeled facility
equipped with an in-office lab & cone
beam technology. Located on a professional
suburban street in Bloomfield, New Jersey
with easy access rear parking. Well-respected
office established for over 50 years. Contact
the Office Manager, at: (973) 769-4794 to
get details.
Established Multidisciplinary Specialty
Dental Practice Seeks a Pediatric Dentist.
Located in a suburb of Princeton, Hamilton
Dental Associates has been serving central New
Jersey for over 50 years. Full-time or part-time
associate position leading to equity position
for the right individual. Hamiltondental.com.
Email: drdeluca@hamiltondental.com or
telephone (609) 586- 6603.
Offices For Lease
Or Purchase
Dental Office.
Monmouth CountyOcean Township
NJIn modern established medical arts
building. All dental plumbing, electrical,
dental cabinetry and lab in place. Plus 2/3
operatories, furnished waiting room, private
bathroom, nurses station, private doctors
office. $1,675 per month, all inclusive.
Including all utilities, HVAC, CAM and
maintenance. Mr. Mirne (732) 539-6987.
Perfect Office for a Dental Specialist
& Support Staff (Medical Practice, or
Health Care Professional).
Operatory/treatment rooms are plumbed
and with electrical power. First floor,
parking. Desirable Princeton NJ, high traffic
location. Possibly sub-dividable. Contact
Michael Mayo, Weichert Realtors, (609)
921-1900 ext 241 cell (713) 449-6498,
michaelkmayo@yahoo.com for details.
Linwood Office Condo Lease/Sale.
1235 sf., beautiful space, excellent condition,
3 plumbed, networked rooms with cabinetry.
Track lights, 4
th
plumbed, central nitrous.
Some equipment for sale separately. Long
term lease available. Can sublease. Rent
$1999/month includes taxes and condo fees.
Purchase option or sale for 250K. (609)
335-4387; mannyfa.@comcast.net.
Dental Office Space for Rent:
Medical office complex in Hunterdon
County, presently with 3 chairs/lines,
2 offices, lab, waiting room and
bathroom-approximately 1,500 sq. ft.
Ideal location for professional, dental or
oral surgery office. Office is beautifully
decorated/updated in a well cared for
medical office building located just
off Route 31 with easy access to
Route 78 in Annandale, NJ. Available
February 2014. Call Judy or Manny
(908) 730-6774.
Forked River Ocean County.
Office space to share. Orthodontic practice
looking to share existing 2,500 sq. ft. office.
Ideal for an Endodontist or Periodontist.
There are no Perio or Endo practices
between Toms River and Barnegat. Space
has 2 pvt. treatment rooms and a bay
with 4 chairs. Call (732) 995-5297 or
email alignm@aol.com.
For Sale-Dental BuildingDunellen
Middlesex County$299,900
The first floor is a full dental office with
4 operatories. The second floor has a
2 bedroom rental apartment. Separate
utilities. Downtown location, walk to train
station. Have your dental office downstairs
and offset the expenses with the rental
income from the apartment. Contact
Andrea Lacerda, Prudential NJ Properties
(908) 578-1166.
Opportunities Sought
NJ DDS (Semi-Retired) Seeking
P/T Position
1.) for diagnosis and treatment planning
(732) 506-7777. 2.) Seeking satellite
office (P/T) Ocean/Monmouth
County (732) 644-3000 with/
without staff.
Classifieds
2014 6ont|nu|ng Educat|on 6ourses
Wednesday, February 26, 2014
Nitrous Oxide Sedation (HANDS-ON)
Dr. Stanton Braid and Dr. Allan Fielding
Wednesday, March 12, 2014
Dental Management of Emergencies and
Medically Compromised Patients
Dr. Gary Jones and Dr. Allan Fielding
Friday, March 21, 2014
2
nd
Annual Engine Driven Instrumentation in
Endodontics Panel Discussion
Moderator: Dr. Cemil Yesilsoy
Speakers: Dr. Chris Glass, Dr. Eric Herbranson
and Dr. Martin Trope
Wednesday, April 2, 2014
Updates in Pediatric Dentistry:
Treating Tiny Tots to Teens
Dr. Lance Kisby
Friday, April 18, 2014
Feel Good Dentistry
A Sane Approach to Esthetic Dentistry
Dr. Steven Weinberg
Friday, May 16, 2014
Limiting Exposure in the 21
st
Century Dental Practice
Dr. Michael Ragan
September 12-14, 2014
Bender Seltzer and Grossman
Academic Review of Endodontology
Course Director: Dr. Cemil Yesilsoy;
Speakers: Drs. Eleazer, Fouad, Hersh, Holland,
Hutter, Keiser, Khan, Pringle and Trope
6ourse Reg|strat|on||nfo:
rllp://derl|slry.lerp|e.edu/corl|ru|rg-ed
0uest|ons?
6a|| 215-707-7541 or
Ema|| ncarrenotemp|e.edu
To advertise please visit:
www.mgxprint.com
and click on the JNJDA link
to fill out a classified ad order form
37 Volume 84, Number 4
Consultants/Services
Practice Transitions.
We specialize in Practice Sales, Appraisals
and Partnership Arrangements. Financing
available. Free Guides for Sellers and Buyers.
Contact Philip Cooper, DMD, MBA,
American Practice Consultants, (800)
400-8550, cooper@ameriprac.com.
Let Me Pay for Your Hawaiian Vacation!
NJ and PA licensed GP will do quality
endo in your office. Also available as an
office fill-in for a general dentist. Call
(856) 772-2293.
Florida Health Seminar.
December 20, 2013. Boca Raton, Fla.
AGD, ADA-CERP, C.E. Credits.
Endodontics, oral surgery, pediatric
dentistry, risk management (HIV update).
Contact Linda Golnick, Coordinator:
(248) 388-1959 Fax (248) 681-0315.
Sell Your Practice, Realize Your Equity,
and Begin Enjoying Your Career!
Summit Dental Group is a Dentist-focused
organization that allows owner doctors to
realize the equity in their practice while
continuing to practice in a management free
role allowing them to focus on what they
enjoy most...patient care.
SDG was created by exceptional dentists,
and we want to acquire exceptional
practices. We offer win-win-win solutions
for you, your staff and your patients that
provide you with the greatest value for your
practice so you can move forward with your
future. You can continue to work without
the responsibilities of running a business
and we will customize a solution thats well-
suited for you. Our dentists have the clinical
control enjoyed in a traditional private
practice without the additional financial
or administrative burdens associated with
practice management. When considering a
practice transition with SDG, dentists can
expect unlimited production-based earnings,
a strong benefits package, a familiar patient
base, continuing education opportunities,
and long-term clinical or managerial
career growth. To learn more please call
(201) 875-7522 or visit us on the web
at www.SummitDentalGroupNJ.com.
Classifieds
THE
Your Business, Lifestyle, and Retirement
PRACTICE
INSURANCE INCLUDES
BEST
SINCE INSURANCE IS A NECESSITY
WHY NOT GET THE MOST OUT OF IT?
Because of our synergistic approach, we provide more dental
practice insurance than any other New Jersey agency. Why? We
cover every risk aspect from malpractice to property, casualty,
workers comp, cyber, health and disability coverage. Constant
updating of these plans keeps you safe. Some of our work-site
features also supply your employees with college scholarships
at no cost to them. Your house and properties, including all
vehicles are integrated into these plans to cut costs and provide
you with total peace of mind. Retirement? By using Pension
Protection Act 2006 we help you to get more retirement income.
HOW DO YOUR PRESENT PLANS STACK-UP?
Now, you can eliminate risk, lower your costs, and gain an
enhanced retirement all supported by an unexcelled three
decades of experienced professional service to your profession.
Call us now for an audit of your situation with helpful
suggestions at no cost. Because the best practice insurance
must include your business, lifestyle and retirement.
34 Sycamore Avenue Little Silver, NJ 07739
T: 732-842-2020 F: 732-842-2221 www.bcszerlip.com
Endorsed By
BCSzerlip_NJDA_BestAd_v8 7/18/13 4:36 PM Page 1
Volume 84, Number 4 38
Practices For Sale
Practices for Sale
ESSEX COUNTY: 2M long-established
PPO insurance practice located in a storefront
in a high traffic area. The practice is
completely digital with 6 equipped operatories
and room for expansion. The practice receives
30 new patients per month and has close to
3,000 active patients. The real estate can be
purchased or leased at the buyers discretion.
Asking price for practice is 1.3M.
TRENTON: 800K long-established PPO/
FFS practice located in a professional building.
Space has 4 equipped operatories in 1,250 square
feet. Practice has 4.5 days of hygiene. Office is
computerized and has digital x-rays as well as a
digital panorex. Real estate can be purchased for
200K or leased. Asking price for practice is 550K.
If interested in either of the above
opportunities please call Dr. Ronald Nemeroff
at (212) 223-2844 or visit our website at
rmndentalbrokers.com for more information.
Classifieds
C
M
Y
CM
MY
CY
CMY
K
NJ-SEP-2013.pdf 1 9/6/13 4:15 PM
MEMBERSHIP WITH NJDA
Considering membership with the NJDA? Here are some highlights of what you get as a member.
MEMBERSHIP SUPPORTS
YOUR PROFESSION
Exciting new changes!
NJ DA announces several new improvements coming soon
that will contribute to better serving member dentists as
technology and the economy change.
New Dentist conference
Member Day
Register, pay for, and keep track of NJDA CE
courses you take on our NEW website
Special Discounts and Services from
Endorsed Business Associates (EBA)
NEW job search & classifed advertisement
functionality available to all members
automatically
Easy-to-access information via our website,
the Advocate, the Journal, and your
component newsletter
Members-only courses at less than $10/credit
We are constantly learning and growing as an association.
If you feel we could better serve you, wed like to know
how! Feel free to reach out at any time. The more dentists
involved in our organization, the stronger your practice and
your profession.
Serving your practice. Advancing your profession.
Dont leave decisions that impact you and your
profession up to people who arent dentists
Organized dentistry is a political force in Trenton.
Through a combination of a vibrant New J ersey Dental
Political Action Committee (NJ DPAC), and an active
grassroots membership (including more than 4,600
NJ DA members), organized dentistry makes its voice
heard in the State House.
Membership and support of NJ DPAC guarantee you
and other New J ersey dentists that we keep our
infuential voice in Trenton.
Questions?
Call us today: 800-831-6532
Or Email: membership@njda.org
MEMBERSHIP WITH NJDA
Considering membership with the NJDA? Here are some highlights of what you get as a member.
MEMBERSHIP SUPPORTS
YOUR PROFESSION
Exciting new changes!
NJ DA announces several new improvements coming soon
that will contribute to better serving member dentists as
technology and the economy change.
New Dentist conference
Member Day
Register, pay for, and keep track of NJDA CE
courses you take on our NEW website
Special Discounts and Services from
Endorsed Business Associates (EBA)
NEW job search & classifed advertisement
functionality available to all members
automatically
Easy-to-access information via our website,
the Advocate, the Journal, and your
component newsletter
Members-only courses at less than $10/credit
We are constantly learning and growing as an association.
If you feel we could better serve you, wed like to know
how! Feel free to reach out at any time. The more dentists
involved in our organization, the stronger your practice and
your profession.
Serving your practice. Advancing your profession.
Dont leave decisions that impact you and your
profession up to people who arent dentists
Organized dentistry is a political force in Trenton.
Through a combination of a vibrant New J ersey Dental
Political Action Committee (NJ DPAC), and an active
grassroots membership (including more than 4,600
NJ DA members), organized dentistry makes its voice
heard in the State House.
Membership and support of NJ DPAC guarantee you
and other New J ersey dentists that we keep our
infuential voice in Trenton.
Questions?
Call us today: 800-831-6532
Or Email: membership@njda.org
MEMBERSHIP WITH NJDA
Considering membership with the NJDA? Here are some highlights of what you get as a member.
MEMBERSHIP SUPPORTS
YOUR PROFESSION
Exciting new changes!
NJ DA announces several new improvements coming soon
that will contribute to better serving member dentists as
technology and the economy change.
New Dentist conference
Member Day
Register, pay for, and keep track of NJDA CE
courses you take on our NEW website
Special Discounts and Services from
Endorsed Business Associates (EBA)
NEW job search & classifed advertisement
functionality available to all members
automatically
Easy-to-access information via our website,
the Advocate, the Journal, and your
component newsletter
Members-only courses at less than $10/credit
We are constantly learning and growing as an association.
If you feel we could better serve you, wed like to know
how! Feel free to reach out at any time. The more dentists
involved in our organization, the stronger your practice and
your profession.
Serving your practice. Advancing your profession.
Dont leave decisions that impact you and your
profession up to people who arent dentists
Organized dentistry is a political force in Trenton.
Through a combination of a vibrant New J ersey Dental
Political Action Committee (NJ DPAC), and an active
grassroots membership (including more than 4,600
NJ DA members), organized dentistry makes its voice
heard in the State House.
Membership and support of NJ DPAC guarantee you
and other New J ersey dentists that we keep our
infuential voice in Trenton.
Questions?
Call us today: 800-831-6532
Or Email: membership@njda.org
39 Volume 84, Number 4
Surgical and Restorative
Excellence in Dentistry
Symposium
Featured Speakers:
Emil Cappetta, DMD
David Garber, DMD
Shankar Iyer, DDS, MDS
John Kois, DMD, MSD
Ernesto Lee, DMD
Myron Nevins, DMD
Rade Paravina, DDS, PhD
Maurice Salama, DMD
Michael Sonick, DMD
Christian Stappert, DDS, PhD
Dennis Tarnow, DMD
Arnold Weisgold, DDS
Join us for this one-of-a-kind event where experts
from both specialties will share their wealth
of knowledge. The most compelling topics
will be discussed and debated by panels of
these dental masters.
Dates: Friday & Saturday, April 4 & 5, 2014
Location: The New York Athletic Club
Central Park South, New York City
Tuition: $645 register by February 15, 2014
$695 register after February 15, 2014
REGISTER ONLINE: cde.sdm.rutgers.edu OR CALL US: 973-972-6561
Continuing Dental Education 110 Bergen St, B701 Newark, NJ 07103 email: cde@sdm.rutgers.edu
2013 NJDA Partners
Platinum
Platinum Premier
Gold
Silver
Bronze
Volume 84, Number 4 40
We continue our 106th year of camaraderie and education as
one of the oldest dental societies in the region!
Spring Dine Around: Wednesday, March 12, 2014
"The Many Faces of Facial Pain"
Alan Stiles, D.M.D.
limited to the management of head, neck, and facial pain. Following his completion of his DMD at Temple University, he completed a residency
CPR: Friday, April 25, 2014
The Buck Hotel, Feasterville, PA
Spring All Day Program: Friday, May 9th, 2014
The Buck Hotel, Feasterville, PA
Productivity: It's not by chance
Bruce Baird, D.D.S.: The business of dentistry is changing as rapidly as new technology is changing how we treat patients. To succeed in todays
change your thinking on the business of dentistry, challenge many of the beliefs that prevent practices from realizing their full potential, and
Dental Center. Dr. Baird specializes in cosmetic makeovers, full mouth rehabilitation, and dental implants.
Annual Golf Outing: June, 2014
Philmont Country Club
You are also not a sales goal or a benchmark or a market segment.
You are a dentist. And we are The Dentists Insurance Company,
TDIC. More than 30 years ago, the small group of dentists who
started this company made three promises: to only protect dentists,
to protect them better than any other insurance company out there
and to be there when you need us. Because with TDIC, youre a
dentist rst, last and always.
Protecting dentists. Its all we do.
877.476.4588 | thedentists.com
You are not a statistic.
Endorsed by
the New Jersey
Dental Association
njda_ad_10-13 2.indd 1 10/17/13 9:50 AM
You might also like
- There Is No Perfect Dentist: The Never Before Revealed Secrets to Choosing the Right Dentist for You!From EverandThere Is No Perfect Dentist: The Never Before Revealed Secrets to Choosing the Right Dentist for You!No ratings yet
- Senior Dental Care Program in PennsylvaniaDocument2 pagesSenior Dental Care Program in PennsylvaniaJesse WhiteNo ratings yet
- House Hearing, 112TH Congress - The Health Care Reform Law: Its Present and Future Impact On Small Businesses and Job CreationDocument50 pagesHouse Hearing, 112TH Congress - The Health Care Reform Law: Its Present and Future Impact On Small Businesses and Job CreationScribd Government DocsNo ratings yet
- Metlife - Dental Ppo 12 15Document3 pagesMetlife - Dental Ppo 12 15api-252555369No ratings yet
- Our Dental Plan For Individuals and FamiliesDocument4 pagesOur Dental Plan For Individuals and Familiesapi-41207808No ratings yet
- The Profitable DentistDocument72 pagesThe Profitable DentistTheProfitableDentist0% (1)
- Member Info: Provider Info:: Custom Dental Provider ListingDocument2 pagesMember Info: Provider Info:: Custom Dental Provider ListingJammy LaiNo ratings yet
- Annual Report 2010Document56 pagesAnnual Report 2010amatamesNo ratings yet
- Journal of The IDADocument48 pagesJournal of The IDAWill SearsNo ratings yet
- Eportfolio Business AnalysisDocument5 pagesEportfolio Business Analysisapi-546628554No ratings yet
- Behind the Dental Chair: How Smart Dentists Crack the Code and Build a Dream PracticeFrom EverandBehind the Dental Chair: How Smart Dentists Crack the Code and Build a Dream PracticeRating: 5 out of 5 stars5/5 (2)
- Academy of General Dentistry DelawardDocument1 pageAcademy of General Dentistry Delawardiraqi iraqiNo ratings yet
- Practical Practice Solutions: Building Your Successful FutureFrom EverandPractical Practice Solutions: Building Your Successful FutureNo ratings yet
- The Houston Fill June 2014Document12 pagesThe Houston Fill June 2014UTSD HoustonASDANo ratings yet
- Summer Dateline 2016Document24 pagesSummer Dateline 2016indydentalsocietyNo ratings yet
- Dentaltown 2015augustDocument118 pagesDentaltown 2015augustLorin ColumbNo ratings yet
- Arduin Kool Smiles Publichealth House TXDocument24 pagesArduin Kool Smiles Publichealth House TXDentist The Menace100% (1)
- January 2014: California Dental AssociationDocument72 pagesJanuary 2014: California Dental AssociationrommeloliveiraNo ratings yet
- DR Jose Cazares Handout 10-15-2012Document2 pagesDR Jose Cazares Handout 10-15-2012Dentist The MenaceNo ratings yet
- Care1st Dental DirectoryDocument137 pagesCare1st Dental DirectorytxgenicNo ratings yet
- Current Web Presence Analysis Arizona State University TWC 301Document9 pagesCurrent Web Presence Analysis Arizona State University TWC 301Briseida AguirreNo ratings yet
- My Friend's Dentist To Perform TLC's "No Scrubs" To Raise Money For Wilmington CharityDocument2 pagesMy Friend's Dentist To Perform TLC's "No Scrubs" To Raise Money For Wilmington CharityPR.comNo ratings yet
- Great Expressions Aquisition Solicitation PackageDocument9 pagesGreat Expressions Aquisition Solicitation PackageDentist The MenaceNo ratings yet
- Aug 16 Million Dollar PPODocument2 pagesAug 16 Million Dollar PPOHenryScheinDentalNo ratings yet
- 2015 Winter DatelineDocument24 pages2015 Winter DatelineindydentalsocietyNo ratings yet
- Jerzie Sackett - Ssem Abstract - 2895050Document1 pageJerzie Sackett - Ssem Abstract - 2895050api-542735726No ratings yet
- Dental Hygiene EssayDocument7 pagesDental Hygiene Essayapi-287131007No ratings yet
- Dental Office Marketing Plan SampleDocument8 pagesDental Office Marketing Plan SampleAnna TranNo ratings yet
- Oral Maxillofacial Surg Clin N Am 20 (2008Document2 pagesOral Maxillofacial Surg Clin N Am 20 (2008Гулпе АлексейNo ratings yet
- ACP MessengerDocument24 pagesACP MessengerSuchada KongkiatkamonNo ratings yet
- Dental Evolving Medical Scene: Care in The CareDocument5 pagesDental Evolving Medical Scene: Care in The Carecarlina_the_bestNo ratings yet
- Building A Profitable PracticeDocument2 pagesBuilding A Profitable PracticeHenryScheinDentalNo ratings yet
- The Guide For Nonprofit Organizations: Montgomery, Mccracken, Walker & Rhoads, LLPDocument36 pagesThe Guide For Nonprofit Organizations: Montgomery, Mccracken, Walker & Rhoads, LLPWidiyarti DardjonoNo ratings yet
- 6 Secrets To More Patients and Higher ProfitsFrom Everand6 Secrets To More Patients and Higher ProfitsRating: 2 out of 5 stars2/5 (2)
- Garden City Community Clinic DentalDocument1 pageGarden City Community Clinic DentalgenesisworldmissionNo ratings yet
- Dental Ethics of AdvertisingDocument6 pagesDental Ethics of AdvertisingLorenzini GrantNo ratings yet
- DentalUM Fall 2012Document40 pagesDentalUM Fall 2012umdentNo ratings yet
- 2013 Lwe 081313 FinalDocument29 pages2013 Lwe 081313 Finalapi-124030554No ratings yet
- HLC Client Welcome Kit BookletDocument28 pagesHLC Client Welcome Kit BooklethousingworksNo ratings yet
- Newsletter April2012PART2Document13 pagesNewsletter April2012PART2msweder6831No ratings yet
- Allied Success: Making The Most of The Relationship Between The Doctor and The Lab TechnicianDocument8 pagesAllied Success: Making The Most of The Relationship Between The Doctor and The Lab TechnicianDiaa Eldin SaadNo ratings yet
- G Part 21Document1 pageG Part 21rerereNo ratings yet
- W. 34th St. Los Angeles, CA 90089: September 2012Document20 pagesW. 34th St. Los Angeles, CA 90089: September 2012USCSDNo ratings yet
- At Your Service: 5-Star Customer Care for a Successful Dental PracticeFrom EverandAt Your Service: 5-Star Customer Care for a Successful Dental PracticeNo ratings yet
- CACARE3 WYG - UnlockedDocument2 pagesCACARE3 WYG - UnlockedlollieNo ratings yet
- DRS - 2014 Annual ReportDocument9 pagesDRS - 2014 Annual ReportScott DeelNo ratings yet
- Spirit Dental PowerpointDocument21 pagesSpirit Dental PowerpointJohn BerkowitzNo ratings yet
- Insider's Guide to Saving Money at the Dentist: A Dentist's Advice on How to Effectively Create and Keep an Amazing SmileFrom EverandInsider's Guide to Saving Money at the Dentist: A Dentist's Advice on How to Effectively Create and Keep an Amazing SmileNo ratings yet
- Dentaltown 2015octoberDocument133 pagesDentaltown 2015octoberbellaNo ratings yet
- Kaiser Dental 2016pdfDocument8 pagesKaiser Dental 2016pdfErdeli StefaniaNo ratings yet
- Ids Final Bound PacketDocument20 pagesIds Final Bound Packetapi-302564973No ratings yet
- DentalUM Fall 2011Document36 pagesDentalUM Fall 2011umdentNo ratings yet
- OD Apr15 CorporateLaws V2Document3 pagesOD Apr15 CorporateLaws V2Chandra ClarkNo ratings yet
- Editorial Board AdajDocument4 pagesEditorial Board Adajdalal huNo ratings yet
- Locally Owned & Family Operated Since 1948!!: Milwaukee NorthDocument12 pagesLocally Owned & Family Operated Since 1948!!: Milwaukee NorthHometown Publications - Express NewsNo ratings yet
- Academy Examiner: Special Humanitarian Service Update EditionDocument8 pagesAcademy Examiner: Special Humanitarian Service Update Editionjoe4299No ratings yet
- What Happens During A Routine Dental Checkup?: Say Hello To Your ReceptionistDocument1 pageWhat Happens During A Routine Dental Checkup?: Say Hello To Your ReceptionistAishani MeggiNo ratings yet
- Dentist Email ListDocument3 pagesDentist Email ListNikitaNo ratings yet
- Microcephaly: Normality Parameters and Its Determinants in Northeastern Brazil: A Multicentre Prospective Cohort StudyDocument12 pagesMicrocephaly: Normality Parameters and Its Determinants in Northeastern Brazil: A Multicentre Prospective Cohort StudycemoaraNo ratings yet
- Axis Laboratoire ChartDocument2 pagesAxis Laboratoire ChartcemoaraNo ratings yet
- The Neuropsychology of Human Memory : Larry R. SquireDocument35 pagesThe Neuropsychology of Human Memory : Larry R. SquirecemoaraNo ratings yet
- Provisional RestorationsDocument10 pagesProvisional Restorationsapi-3775747100% (1)
- Inflammation and Neuroprotection in Traumatic Brain InjuryDocument8 pagesInflammation and Neuroprotection in Traumatic Brain InjurycemoaraNo ratings yet
- Book PetkoDocument47 pagesBook PetkocemoaraNo ratings yet
- Exposure Lesson 1 (FREE)Document19 pagesExposure Lesson 1 (FREE)Marco Paulo SantosNo ratings yet
- Child Fatalities From Religion-Motivated Medical Neglect PDFDocument5 pagesChild Fatalities From Religion-Motivated Medical Neglect PDFcemoaraNo ratings yet
- Aesthetic Crown Lengthening PDFDocument14 pagesAesthetic Crown Lengthening PDFcemoaraNo ratings yet
- Ana PnsDocument15 pagesAna PnsDr. T. BalasubramanianNo ratings yet
- Evolution at Two Levels PDFDocument8 pagesEvolution at Two Levels PDFcemoaraNo ratings yet
- Aesthetic Crown Lengthening PDFDocument14 pagesAesthetic Crown Lengthening PDFcemoaraNo ratings yet
- Diabéticos - Como Cuidar Dos Seus Rins PDFDocument28 pagesDiabéticos - Como Cuidar Dos Seus Rins PDFcemoaraNo ratings yet
- Dwivedi PDFDocument9 pagesDwivedi PDFsacks_tubbieuNo ratings yet
- Suturando para Sucesso Cirúrgico PDFDocument11 pagesSuturando para Sucesso Cirúrgico PDFcemoaraNo ratings yet
- The Physics of UFOs PDFDocument2 pagesThe Physics of UFOs PDFcemoaraNo ratings yet
- Contemporary Crown-Lengthening PDFDocument10 pagesContemporary Crown-Lengthening PDFcemoaraNo ratings yet
- 473 1400 1 PB PDFDocument2 pages473 1400 1 PB PDFcemoaraNo ratings yet
- 5-1tardigrades Survival PDFDocument20 pages5-1tardigrades Survival PDFcemoaraNo ratings yet
- Beyond Belief PDFDocument16 pagesBeyond Belief PDFcemoaraNo ratings yet
- Your Genes, Your Choices:: Exploring The Issues Raised by Genetic ResearchDocument89 pagesYour Genes, Your Choices:: Exploring The Issues Raised by Genetic ResearchcemoaraNo ratings yet
- U.S. Cancer Death Rates Continue To Drop PDFDocument3 pagesU.S. Cancer Death Rates Continue To Drop PDFcemoaraNo ratings yet
- Am I An Atheist or An Agnostic - Bertrand Russell PDFDocument4 pagesAm I An Atheist or An Agnostic - Bertrand Russell PDFcemoaraNo ratings yet
- Jaj707 PDFDocument7 pagesJaj707 PDFcemoaraNo ratings yet
- Philosophy of Science (Collection of Quotes)Document67 pagesPhilosophy of Science (Collection of Quotes)tototheclownNo ratings yet
- Jean Meslier and 'The Gentle Inclination of Nature' PDFDocument29 pagesJean Meslier and 'The Gentle Inclination of Nature' PDFcemoaraNo ratings yet
- Alfred Loisy (1857-1940) PDFDocument10 pagesAlfred Loisy (1857-1940) PDFcemoaraNo ratings yet
- Can We Know The Universe$Document4 pagesCan We Know The Universe$cemoaraNo ratings yet
- Intro PDFDocument13 pagesIntro PDFcemoaraNo ratings yet
- Milobar Alexus Resume MayoDocument2 pagesMilobar Alexus Resume Mayoapi-338646789No ratings yet
- Mini-implant molar intrusion caseDocument1 pageMini-implant molar intrusion caseVesna AndreevskaNo ratings yet
- CLUSTERS LIST - (CHNCS) GO-209Document45 pagesCLUSTERS LIST - (CHNCS) GO-209Gadde Srinivasarao67% (3)
- Medical certificate from Pantalan SHSDocument2 pagesMedical certificate from Pantalan SHSAngelo Villafranca67% (3)
- 2.3. Mental Health Nursing: Course DescriptionDocument5 pages2.3. Mental Health Nursing: Course Descriptioncharanjit kaurNo ratings yet
- The Natural Way To A Healthy HealingDocument111 pagesThe Natural Way To A Healthy HealingAnjanaNo ratings yet
- Abu Dhabi DRGDocument62 pagesAbu Dhabi DRGDolly creationsNo ratings yet
- Triage and Approach To The Acute Abdomen: Elisa M. Mazzaferro, MS, DVM, PHDDocument6 pagesTriage and Approach To The Acute Abdomen: Elisa M. Mazzaferro, MS, DVM, PHDRatna SariNo ratings yet
- Clinical Biochemistry ReviewDocument10 pagesClinical Biochemistry Reviewyaykatai100% (2)
- FormsDocument15 pagesFormsBiswajit DasNo ratings yet
- Delafloxacin 4Document23 pagesDelafloxacin 4Muhammad RamzanNo ratings yet
- Rheumatic Fever For All For DR Wilfredo Stokes B. Guatemala Nov 2,009Document9 pagesRheumatic Fever For All For DR Wilfredo Stokes B. Guatemala Nov 2,009drwstokes100% (1)
- CH 14 Part 1 Principles of Disease & Epidemiology (FA20)Document15 pagesCH 14 Part 1 Principles of Disease & Epidemiology (FA20)sammy alanNo ratings yet
- Assignment 1 Cs 0902Document4 pagesAssignment 1 Cs 0902prince12No ratings yet
- Nephrons (Functional Unit)Document44 pagesNephrons (Functional Unit)Nur SanaaniNo ratings yet
- Hypertension in PregnancyDocument18 pagesHypertension in Pregnancyshubham kumarNo ratings yet
- Interpretting ABG SuccessfullyDocument15 pagesInterpretting ABG Successfullyanimathz100% (1)
- Detailed Lesson Plan Respiratory SystemDocument7 pagesDetailed Lesson Plan Respiratory Systemjane89% (9)
- Understanding the Benefits of Physical ActivitiesDocument17 pagesUnderstanding the Benefits of Physical ActivitiesRealisan DulnuanNo ratings yet
- Lesson 3 ReviewDocument4 pagesLesson 3 ReviewHo Yong WaiNo ratings yet
- Medical Handwashing Procedure StepsDocument3 pagesMedical Handwashing Procedure StepsKERL RAMANo ratings yet
- Advanced Burn Life SupportDocument118 pagesAdvanced Burn Life SupportIntan Noa100% (1)
- ACLS NotesDocument3 pagesACLS Notessaxmanwrv0% (1)
- Case Study 5 Year Boy With CoughDocument3 pagesCase Study 5 Year Boy With CoughAryl Eduarte100% (1)
- Vancouver Coastal Health Enhanced Surveillance and Precautions ProtocolsDocument1 pageVancouver Coastal Health Enhanced Surveillance and Precautions ProtocolsIan YoungNo ratings yet
- Akupresur Point Hugo Mengurangi Nyeri Tusukan AVF pada Pasien HemodialisaDocument10 pagesAkupresur Point Hugo Mengurangi Nyeri Tusukan AVF pada Pasien HemodialisamargaretNo ratings yet
- Sanctification of The Heart 4th Edition by DR Michelle StrydomDocument771 pagesSanctification of The Heart 4th Edition by DR Michelle StrydomDios Estrella67% (3)
- PATIENT INFORMATION - New App System - WebsiteDocument2 pagesPATIENT INFORMATION - New App System - WebsiteA M P KumarNo ratings yet
- Fish & Shellfish PoisoningDocument29 pagesFish & Shellfish Poisoningkolita kamal100% (4)
- Minimum Inhibitory ConcentrationDocument7 pagesMinimum Inhibitory ConcentrationToshio HamazakiNo ratings yet