Professional Documents
Culture Documents
MG Sulphate
Uploaded by
phobicmd0 ratings0% found this document useful (0 votes)
39 views6 pagesjk
Original Title
Mg Sulphate
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentjk
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
39 views6 pagesMG Sulphate
Uploaded by
phobicmdjk
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
Arch Argent Pediatr 2012;110(4):291-296 / 291
Effectiveness of magnesium sulfate as initial
treatment of acute severe asthma in children,
conducted in a tertiary-level university
hospital. A randomized, controlled trial
SUMMARY
Introduction. Magnesium sulfate is a calcium an-
tagonist that inhibits bronchial smooth muscle
contraction promoting bronchodilation. It is used
for the management of acute severe asthma in
children; however most of the studies have been
performed in adults.
Objective. To evaluate the effectiveness of in-
travenous magnesium sulfate for the treatment
of pediatric patients with acute severe asthma
exacerbations.
Population and Methods. A clinical, random-
ized, controlled trial was conducted between
March 2006 and March 2011 at Hospital Uni-
versitario Austral. Children with acute severe
asthma admitted to the emergency department
were randomized into two groups. Group A
(control group): standard protocol for the initial
treatment of acute asthma exacerbation. Group
B: treatment protocol with magnesium sulphate
for acute severe asthma exacerbation. The pri-
mary outcome was the requirement of invasive
or non invasive mechanical ventilation support.
Results. One hundred and forty three patients
randomized into 2 groups were analyzed. The
treatment group included 76 patients receiving
magnesium sulfate within the rst hour of the
initiation of rescue treatment at the hospital, and
the control group included 67 patients not treated
with magnesium sulphate. Among the patients
in the control group, 33% (n= 22) required me-
chanical ventilation support, compared to only
5% (n= 4) of the patients in the treatment group
(p = 0.001).
Conclusions. Intravenous infusion of magnesium
sulfate during the rst hour of hospitalization in
patients with acute severe asthma signicantly
reduced the percentage of children who required
mechanical ventilation support.
Key words: magnesium sulphate, acute severe asth-
ma in children, Woods score, mechanical ventilation
support, emergency department.
http://dx.doi.org/10.5546/aap.2012.eng.291
INTRODUCTION
Magnesium sulphate is a physi-
ological calcium antagonist that acts
by inhibiting the contraction medi-
ated by the bronchial smooth muscle.
In addition, it interferes with the para-
a. Department of
Mother and Child
Health.
Hospital Austral.
Buenos Aires,
Argentina.
E-mail address:
Silvio Torres:
storres@cas.austral.
edu.ar
Conflict of interest:
None.
Received: 12-1-2011
Accepted: 4-26-2012
sympathetic stimulation and prevents
acetylcholine release to the axon ter-
minal; therefore promoting a broncho-
dilating effect.
1
Magnesium sulphate also has a
role in the reduction of inflammation
by inhibiting mast cell degranulation
and reducing thromboxane, histamine
and leukotrienes circulation.
The first publication on the use
of magnesium sulphate for the treat-
ment of asthma was the report of
a case
2
sixty years ago, but only in
1989, Skobeloff et al. published the
first randomized, double-blind, pla-
cebo-controlled trial on the benefits of
magnesium sulphate for acute asthma
exacerbations.
3
Several subsequent publications
showed that magnesium sulphate
was effective for its use both in emer-
gency departments and intensive care
units.
4,5
In the last years, several studies
analyzed the effectiveness of magne-
sium sulphate in acute severe asthma
episodes as an intravenous therapy or
inhaled together with bronchodilators.
However, most studies were devel-
oped for adult populations, as shown
in the 2000 Cochrane Collaboration
systematic review.
6
In pediatric populations, the study
conducted by Ciarallo et al. should be
pointed out, with a randomized, dou-
ble-blind and controlled design based
on pulmonary function tests. Among
its weakness it is worth mentioning
that it only included patients older
than 6 years and that pulmonary func-
tion tests measurements had been er-
ratic, as shown in the studys editorial
discussion.
7
Silvio Torres
a
M.D., Nicols Sticco
a
M.D., Juan Jos Bosch
a
M.D., Toms Iolster
a
M.D.,
Alejandro Siaba
a
M.D., Manuel Rocca Rivarola
a
M.D. and Eduardo Schnitzler
a
M.D.
Original article
292 / Arch Argent Pediatr 2012;110(4):291-296 / Original article
The lack of pediatric studies has been associ-
ated with the difficulty of measuring pulmonary
function in younger children and the unwilling-
ness of older children to be subjected to a test.
For this reason, studies developed in this age
range sought to measure the following: an im-
provement in respiratory scores, hospitalization
length-of-stay, and the use or not of mechanical
ventilation (MV).
6,8.
OBJECTIVE
To evaluate the effectiveness of intravenous
magnesium sulphate for severe asthma exacerba-
tions in pediatric patients.
Acronyms:
SO
4
Mg: Magnesium sulphate.
HUA: Hospital Universitario Austral.
MV: Mechanical ventilation.
PICU: Pediatric Intensive Care Unit.
CPG: Clinical Practice Guidelines.
POPULATION AND METHODS
Between March 2006 and March 2011, a clini-
cal, open-label, randomized, controlled trial was
conducted at Hospital Universitario Austral. The
clinical treatment protocol was approved by the
Ethics Committee and the Clinical Research Unit
of Hospital Universitario Austral. The Clinical
Practice Guidelines on acute severe asthma used
in this study were prepared by HUAs Clinical
Practice Guidelines Sub-Committee and approved
by the Ethics Committee.
The study included patients aged 2 to 15 who
attended the hospital emergency department due
to acute severe asthma, classified according to a
Woods score (Table 1) of 5 or more. This assess-
ment was performed by the Pediatric Intensive
Care Unit (PICU) staff doctors, who indicated the
patients admission following such classification
(if Woods score was 5). Patients with hyper-
thermia (temperature 38.3C [100.94F]), systol-
ic blood pressure <25th percentile for their age,
treatment with theophylline or aminophylline in
the previous 48 hours, and children with a history
of kidney, heart or restrictive chronic pulmonary
disease were excluded.
Parents or legal guardians were asked to give
their written informed consent to participate in
the study after understanding the study objec-
tives, scope and likely risks.
Randomization was performed using a ran-
dom number sequence, a computer and STATA
8.0 software. Two physicians responsible for the
study prepared the randomization series, the as-
signment was then performed using opaque en-
velopes. A sequence number was assigned to each
of these sealed envelopes, thus blinding was en-
sured. Professionals taking part in the randomiza-
tion process were different from those in charge
of recruitment and data analysis.
A database was built using the following end-
points: age, sex, length-of-stay in PICU, need of
MV, days of stay in MV, length-of-stay in MV,
length-of-stay in intensive care unit, hospitaliza-
tion length-of-stay, family history of asthma (yes/
no), history of at least one admission to the inten-
sive care unit or intermediate care unit (yes/no),
background outpatient treatment with broncho-
dilators, background outpatient treatment with
inhaled corticosteroids.
Treatment protocol
Patients with acute severe asthma seen at the
emergency department, whose parents had given
their consent for the study, were included and as-
signed to one of two groups:
- Group A: magnosium suIplalo lroalmonl pro-
tocol for acute severe asthma exacerbation.
(Table 2a)
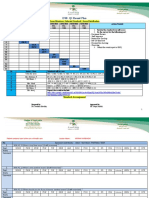
TABLE 1. Woods score
Endpoints 0 1 2
PaO
2
(mmHg) 70-100 en ambient air <70 in ambient air <70 in 40% O
2
Cyanosis No In ambient air In 40% O
2
Inspiratory murmur Normal Uneven Reduced or absente
Use of accessories No Moderate Maximum
Expiratory wheezes No Moderate Marked
Brain function Normal Depressed or agitated Coma
A score of 5 means a severe attack.
Effectiveness of magnesium sulfate as initial treatment of acute severe asthma in children, conducted in a tertiary-level university hospital. / 293
- Group B: slandard iniliaI prolocoI for aculo so-
vere asthma exacerbation. (Table 2b)
All patients were initially treated with 3 doses
of inhaled -2-adrenergic nebulization (salbuta-
mol) at 0.15 mg/kg/dose (minimum 2.5 mg and
maximum 10 mg every 20 minutes during the first
hour), and methylprednisolone at 1 mg/kg/dose
IV.
4
All patients in the treatment group received
IV magnesium sulphate, at 25 mg/kg (maximum
2 g) in a 20-minute infusion, within the first hour
after being admitted to the hospital.
9
A nurse stayed next to the child during the
entire infusion time, supervised by the physician
who had prescribed the treatment.
The following parameters were monitored on
an ongoing basis: heart rate, respiratory rate, blood
oxygen saturation, and blood pressure. The phar-
macy of Hospital Universitario Austral provided
the medication for the study in its usual commer-
cially available presentation for children and adults.
Treatment discontinuation criteria
The treatment protocol was discontinued and
the next stage in the CPGs was initiated if any of
the following occurred during the drug infusion:
- Oxygon saluralion <88 vill a mask (IiO
2
0.35).
- Markod cIinicaI dolorioralion ovidoncod by an
increase of >2 points in Woods score from ba-
seline at study enrollment.
- ArloriaI lypolonsion (<25ll porconliIo for llo
patients age).
- Hoarl ralo >3O from basoIino al sludy inilia-
tion.
Statistical analysis
For the sample size required we observed
that, in accordance with the reviewed literature,
the incidence for positive pressure support is 10-
15%.
10,11
Taking into consideration a reduction of
20% of the endpoint Use of MV (primary pre-
determined endpoint) in the treatment group, and
assuming a power of 80% and a 95% confidence
interval (CI), the sample size estimated for the dif-
ference in proportion between the 2 groups was
65 patients per arm.
A database was established, where quantita-
tive outcomes were analyzed using median and
quartiles, when distribution was not parametric,
SBT 0.15 mg/kg x 3
MPD 2 mg/kg IV
O
2
SBT 0.2 mg/kg x 3
CRIA
Inadequate
response
SBT 0.15-0.4 mg/kg/h
Mechanical ventilation
Inadequate
response
TABLE 2A. Treatment group TABLE 2B. Control group
SBT: Salbutamol. MPD: Methyprednisolone. SO
4
Mg: Magnesium sulphate. IARF: Impending Acute Respiratory Failure.
TABLE 2. Treatment protocol with IV magnesium sulphate, included in the Clinical Practice Guidelines of Hospital
Universitario Austral
SBT 0.15 mg/kg x 3
MPD 2 mg/kg IV
O
2
SO
4
Mg 25 mg/kg
SBT 0.2 mg/kg x 3
CRIA
Inadequate
response
SBT 0.15-0.4 mg/kg/h
Mechanical ventilation
Inadequate
response
294 / Arch Argent Pediatr 2012;110(4):291-296 / Original article
and using means and standard deviations, when
outcomes met alleged normal values. Categori-
cal endpoints were stated in percentages and ab-
solute values.
Continuous endpoints were compared using a
t-test (according to their parametric distribution)
or a Wilcoxon test, while categorical endpoints
were analyzed using a chi-square test (
2
) or a
Fishers exact test. A p-value of <0.05 was consid-
ered statistically significant. The statistical analy-
sis was performed on an intention-to-treat basis
in both groups.
A multivariate logistic regression analysis was
also done. A baseline univariate analysis was do-
ne comparing all endpoints with that of the need
of mechanical ventilation support; since this was
considered influential, the previous treatment with
inhaled -2-adrenergics and corticosteroids interac-
tion endpoint was established. Those resulting in
p 0.1 were included in the multivariate analysis.
One by one, they were included in the model, an-
alyzing the confounding and modification effect,
to eventually reach a predictive model with the
following: treatment with magnesium sulphate,
family history of asthma, previous treatment with
inhaled corticosteroids/-2-adrenergics, and age
younger than 60 months.
The statistical software, STATA 8.0 (California,
USA) was used.
RESULTS
During the study period, 148 eligible patients
were assisted but parents consent was not ob-
tained for 5 of them. Therefore, 143 patients di-
agnosed with acute severe asthma according to
Woods score were randomized. Of these, 76 were
included in the treatment group and 67 in the con-
trol group. None of the patients met any of the
treatment discontinuation criteria.
The baseline characteristics of the individuals
included in the groups are shown in Table 3.
Of the patients in the control group, 33%
(n = 22) required MV (6 required invasive MV and
16 non-invasive MV), compared to only 5% (n = 4)
of the patients in the magnesium sulphate group
(3 required non-invasive MV and 1 invasive MV),
with a statistically significant difference (p = 0.001).
The mean length-of-stay with MV was 5 days
(range (r): 2-12) in the control group, and 3 days
(r: 1-6) in the treatment group (p = 0.087). The
median admission to the PICU was 2 days (r: 1-4)
in the treatment group, compared to 10 days (r:
6-18) in the control group (p = 0.0367). The median
length-of-stay was 7 days in the treatment group
(r: 3-12) compared to 19 days in the control group
(r: 14-29); this difference was statistically signifi-
cant (p = 0.046). (Table 4)
Following the baseline univariate analysis, the
endpoints to be included in the multivariate logis-
tic regression analysis were selected according to
their statistical significance. The endpoint history
of admission to the PICU, previously considered
influential, was eventually not significant in our
univariate analysis. It should be mentioned that
the confounder of the endpoints family history
of asthma, outpatient treatment (inhaled -
2-adrenergics and inhaled corticosteroids as inter-
action term), and age younger than 60 months
were finally included in the model together with
the endpoint treatment with magnesium sul-
phate. This last endpoint had a statistically sig-
nificant protective effect on the non-use of MV
(OR: 0.680, 95% CI: 0.238-0.836). Among the re-
maining outcomes analyzed, age younger than
60 months was associated with a statistically sig-
nificant higher risk of use of MV. (Table 5)
DISCUSSION
This clinical randomized and controlled tri-
al on the use of magnesium sulphate during the
first hour is the first one conducted in this field in
Argentina and may serve as the basis for future
research on acute severe asthma and its manage-
ment in the emergency department.
TABLE 3. Demographics
Treatment group n= 76 Control group n= 67 Total p-value
Sex (M) 33 25 58 NS
Age in months (median, interquartile range) 75 (30-174) 62 (26-168) NS
History of admission to the PICU 27 22 49/143 NS
Family history 47 59 106/143 NS
Outpatient treatment with inhaled -2-adrenergics 28 22 50/143 NS
Outpatient treatment with inhaled corticosteroids 61 53 114/143 NS
Woods score (; SD) 7.4; 2 6.9; 1 NS
: mean; SD: standard deviation; NS: not signicant.
Effectiveness of magnesium sulfate as initial treatment of acute severe asthma in children, conducted in a tertiary-level university hospital. / 295
Our results showed that intravenous mag-
nesium sulphate delivery during the first hour
of hospitalization in children with acute severe
asthma significantly reduced the requirement of
mechanical ventilation support.
In addition, a shorter stay in the PICU and in
the hospital was observed in the treatment group
(both differences were statistically significant). In
the treatment group, the duration of respiratory
support was also shorter, but this difference was
not statistically significant.
In children younger than 5 years old, a higher
risk of MV requirement was observed compared
to children older than 5 years old. This difference
was statistically significant and independent of
the confounders that the other concomitant end-
points of the model may have had. The severity
of an acute exacerbation of asthma in young chil-
dren may make this population susceptible not to
improve with the accepted drug treatment and to
require a different therapy, such as positive pres-
sure support. In spite of the severity posed by the
use of MV, no children died.
In 2005, a metaanalysis of 5 randomized and
controlled studies that included 182 children
compared magnesium sulphate together with -
2-agonists and intravenous corticosteroids ver-
sus placebo. It was concluded that magnesium
sulphate provides an additional benefit in acute,
moderate and severe asthma by reducing hos-
pitalization in these patients with a decrease of
absolute risk by 0.26 (95% CI 0.12-0.39). In four
studies a dose of 25 mg/kg was used, while in the
fifth study a dose of 40 mg/kg was used; no ad-
verse events were observed in any of the studies.
8
The evidence supporting the use of magne-
sium sulphate for acute severe asthma has in-
creased over the last years. In 2009, Knut and
Halvorsen
9
endorsed the use of intravenous mag-
nesium sulphate for severe asthma exacerbations
in children, after using inhaled -2-adrenergics
and corticosteroids.
In relation to our study, when patient recruit-
ment started in 2006, there was no sound evidence
regarding its use. As of 2009, magnesium sul-
phate has been recommended in pediatric care. In
its 2010 version, the Global Initiative for Asthma
(GINA) considers magnesium sulphate level A of
evidence in children who do not respond to stan-
dard treatment after the first hour of therapy or
in those who do not exceed 60% of the theoretical
FEV after an hour of therapy. However, in the dif-
ferent pediatric intensive care units it is not used in
a protocolized manner and has not been included
in the different clinical practice guidelines.
4,5
We
believe that our study offers additional evidence
by specifically analyzing the use of positive pres-
sure support.
It is widely accepted that both invasive and
non-invasive ventilation have deleterious effects
on asthma patients, because morbidity and mor-
tality are increased.
12
However, not all patients
with asthma exacerbations will progress to acute
respiratory failure, and only 8-24% of patients are
hospitalized in a PICU.
13,14
In this group of pa-
tients, approximately 10-15% will require MV.
10,11
The need for excessive sedation, the contro-
versies regarding ventilation approaches, and the
use of positive end expiratory pressure (PEEP) in
these patients cast a shadow over the prognosis
TABLE 5. Logistic regression analysis on the objective clinical improvement in the endpoint called use of MV
Regression variables OR (95% CI) p-value
Treatment with magnesium sulphate 0.680 (0.238-0.836) 0.0147
Family history of asthma 1.239 (0.565-3.4103) (NS)
Previous treatment with inhaled -2-adrenergics and corticosteroids 1.3669 (0.821-5.168) (NS)
Age 60 months (5 years old) 2.639 (1.205-4.108) 0.041
TABLE 4. Univariate analysis
Treatment group n= 76 Control group n= 67 p-value
Need of MV 5% (n= 4) 33% (n= 22) 0.001
Length-of-stay in MV (days) 3 (1-6) 5 (2-12) 0.087
Total hospital length-of-stay 7 (3-12) 19 (14-29) 0.046
Length-of-stay in PICU (days) 2 (1-4) 10 (6-18) 0.0376
: median, interquartile range.
MV: Mechanical ventilation.
296 / Arch Argent Pediatr 2012;110(4):291-296 / Original article
CONCLUSIONS
The intravenous administration of magnesium
sulphate during the first hour of the patients
admission to the hospital was associated with a
significant decrease in the number of children re-
quiring mechanical ventilation support.
17
Acknowledgments
To Mara Elina Serra M.D., for her collabora-
tion in this study.
BIBLIOGRAPHY
1. Corbridge TC, Hall JB. The assessment and management
of adults with status asthmaticus. Am J RespirCrit Care Med
1995;151(5):1296-316.
2. Hurry V Getal. Blood serum magnesium in bronchial asth-
ma and its treatment by administration of magnesium sul-
phate. J Lab ClinMed1940;26:340-6.
3. Skobeloff EM, Spivey WH, McNamara RM, Greenspon
L. Intravenous magnesium sulphate for the treatment of
acute asthma in the emergency department. JAMA 1989;
262:1210-13.
4. NHLBI Guidelines for the Diagnosis and Treatment of
asthma. Available at: http.//www.nhlbi.nih.gov/guide-
lines/asthma.
5. Global strategy for asthma management and prevention
2010 (update). Available at: http.//www.ginasthma.org.
6. Rowe BH, Bretzlaff JA, Bourdon C, Bota GW, Camargo CA
Jr. Magnesium sulphate for treating exacerbations of acute
asthma in the emergency department. Cochrane Database
Syst Rev 2000;(2):CDO01490.Review.
7. Ciarallo L, Sauer AH, Shannon MW. Intravenous magne-
sium therapy for moderate to severe pediatric asthma: re-
sults of randomized, placebo-controlled trial. J Pediatrics
1996;129:809-14.
8. Cheuk DK, Chau TC, Lee SL. A meta-analysis on intrave-
nous magnesium sulphate for treating acute asthma. Arch
Dis Child 2005;90:74-77.
9. Oymar K, Halvorsen T. Emergency presentation and man-
agement of acute severe asthma in children. Scandinavian
journal of trauma. Res Emerg Med 2009;17:40.
10. Paret G, Kornecki A, Szeinberg A, Vardi A, et al. Severe
acute asthma in a community hospital pediatric intensive
care unit: a ten-year experience. Ann Allergy Asthma Im-
munol1998;80:339-44.
11. Beers SI, Abramo TJ, Wiebe RA: Bilevel positive airway
pressure in the treatment of status asthmaticus in pediat-
rics. Am J Emerg Med 2007;25:6-9.
12. Maffei FA, van der Jagt EW, Powers KS, et al. Duration of
mechanical ventilation in life-threatening pediatric asth-
ma: description of an acute asphyxial subgroup. Pediatrics
2004;114(3):762-7.
13. Cox RG, Barker GA, Bohn DJ. Efcacy, results, and com-
plications of mechanical ventilation in children with sta-
tus asthmaticus. PediatrPulmonol1991;11:120-6.
14. Malmstrom K, Kaila M, Korhonen K, et al. Mechanical
ventilation in children with severe asthma. PediatrPulm-
onol2001;31:405-11.
15. Bohn D, Kissoon N. Acute Asthma. Ped Crit Care Med 2001;
2:151-63.
16. Alter HJ, Koepsell TD, Hilty WM. Intravenous magnesium
as an adyuvant in acute bronchoespasm: a meta-analysis.
Ann Emerg Med 2000;36:191-7.
17. Rodrigo G, Rodrigo C, Burschtin O. Efcacy of magnesium
sulphate in acute adult asthma: a meta-analysis of random-
ized controlled trials. Am J Emerg Med 2000;18:2-18.
of these children due to the high risk of compli-
cations, such as barotrauma and alveolar air leak
syndrome, thus increasing their risk of death.
15
Currently, the accepted ventilation strategies
are based on short inhaling times and prolonged
exhaling times, with low tidal volumes, low re-
spiratory rates, pressure-controlled ventilation
modes and permissive hypercapnia to avoid baro-
trauma.
9
It should be noted that our population com-
prises a wide age range, from 2 to 15 years old.
This is considered a weakness of our study due
to the small number of subjects included, which
prevents us from conducting a subset analysis,
although the age distribution in both groups was
balanced.
Another limitation is not having done pulmo-
nary function tests, because it is difficult to imple-
ment them in children younger than 6 years old,
as pointed out by Ciarallo et al.
7
The endpoint use of systemic corticosteroids
on an outpatient basis was not recorded either,
which could be important to classify bronchi-
al inflammation status. In relation to the use of
Woods score 5 to be included in the study, al-
though it was always done by the same healthcare
professionals, it should be noted that subjectivity
at assigning a score cannot be avoided.
In spite of an open-label design, those who
treated patients were different from those who
collected the data, and also different from those
who processed and analyzed the data in order to
mitigate such bias.
Among the study strengths, homogeneity be-
tween both groups regarding their baseline char-
acteristics and severity status to be eligible for the
study are worth pointing out, together with the
management of confounders by stratification and
multivariate regression analysis.
It should be noted that magnesium sulphate is
a drug approved by the National Administration
of Medicines, Food and Technology of Argentina
(ANMAT) for its use in children, as stated in res-
olution N 0798. It is safe and available for use, so
we believe it is feasible to disseminate its use in
the emergency department or PICU as shown by
our study and the international literature.
16
Our findings match the evidence obtained
from different reviews in this field, focused on
objectives similar to ours, regarding the shorter
hospital length-of-stay and the smaller number
of children requiring mechanical ventilation sup-
port.
17
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Protocol 1 Hypoglycemia 2006Document7 pagesProtocol 1 Hypoglycemia 2006Aprilian Ayu SitaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Paediatric Empyema: A Case Report and Literature ReviewDocument5 pagesPaediatric Empyema: A Case Report and Literature ReviewphobicmdNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Pneumococcal Conjugate Vaccine (PCV) Catch-Up Guidance For Children 4 Months Through 18 Years of Age 2015Document3 pagesPneumococcal Conjugate Vaccine (PCV) Catch-Up Guidance For Children 4 Months Through 18 Years of Age 2015phobicmdNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- 1B Draft Annce-Wshop 020113.amendedDocument1 page1B Draft Annce-Wshop 020113.amendedphobicmdNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Diagnosis of Tuberculosis in Children: Increased Need For Better MethodsDocument9 pagesDiagnosis of Tuberculosis in Children: Increased Need For Better MethodsphobicmdNo ratings yet
- AsthmaDocument17 pagesAsthmaphobicmdNo ratings yet
- 1A Draft Annce-CME Course 020113.amendedDocument1 page1A Draft Annce-CME Course 020113.amendedphobicmdNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Left Bronchus SyndromeDocument3 pagesLeft Bronchus SyndromephobicmdNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Difficult Coughing Child: Prolonged Acute Cough in ChildrenDocument5 pagesThe Difficult Coughing Child: Prolonged Acute Cough in ChildrenphobicmdNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Wet CoughDocument2 pagesWet CoughphobicmdNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Diagnostic Assessment of Patients With Interstitial Lung DiseaseDocument8 pagesDiagnostic Assessment of Patients With Interstitial Lung DiseasephobicmdNo ratings yet
- Empyema 2Document9 pagesEmpyema 2phobicmdNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Pi Is 0954611105000491Document5 pagesPi Is 0954611105000491phobicmdNo ratings yet
- Pediatrics 2013 E1089 104Document18 pagesPediatrics 2013 E1089 104phobicmdNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Pediatrics 2013 Iwamoto E817 24Document10 pagesPediatrics 2013 Iwamoto E817 24phobicmdNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Pediatrics 2013 Andrews S36Document3 pagesPediatrics 2013 Andrews S36phobicmdNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Pediatrics 2013 Bivins S47Document3 pagesPediatrics 2013 Bivins S47phobicmdNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Pediatrics 2013 Davis S5Document3 pagesPediatrics 2013 Davis S5phobicmdNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- CP Guideline Ats ILDDocument19 pagesCP Guideline Ats ILDphobicmdNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Al MarbinDocument6 pagesAl MarbinAu Cassie100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- New Nurse Survival GuideDocument207 pagesNew Nurse Survival GuideAlo Al- hassan100% (1)
- REVISED FInalDocument41 pagesREVISED FInalJohn Lewis SuguitanNo ratings yet
- Clinical Outcome of Tetanus Based On Dakar Tetanus Severity Score in Paediatric Intensive Care Unit of ADocument5 pagesClinical Outcome of Tetanus Based On Dakar Tetanus Severity Score in Paediatric Intensive Care Unit of Ahusna fitriaNo ratings yet
- Clinical Rotation PlanDocument2 pagesClinical Rotation PlanManisha ThakurNo ratings yet
- Lexi Rockenbaugh Resume RNDocument2 pagesLexi Rockenbaugh Resume RNapi-437831661No ratings yet
- Horn International University College: Colleege of Health ScienceDocument27 pagesHorn International University College: Colleege of Health Sciencekaise AbdiNo ratings yet
- Cover Letter For Critical Care Nurse PositionDocument6 pagesCover Letter For Critical Care Nurse Positionafmrrxijgwnnxa100% (1)
- Istat CME TalkDocument22 pagesIstat CME TalkmuhammadNo ratings yet
- Neonatal Intensive Care UnitDocument16 pagesNeonatal Intensive Care Unitbhawna100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- PICU BookletDocument98 pagesPICU BookletTufail MemonNo ratings yet
- PICU Protocol FINALDocument120 pagesPICU Protocol FINALwalaa mousaNo ratings yet
- PICU HandbookDocument113 pagesPICU HandbookCarkos Moreno100% (2)
- Paediatrica IndonesianaDocument6 pagesPaediatrica IndonesianayusrinastitiNo ratings yet
- Pediatric Critical Care 5Th Edition Jerry J Zimmerman Download PDF ChapterDocument51 pagesPediatric Critical Care 5Th Edition Jerry J Zimmerman Download PDF Chaptergloria.ramos636100% (5)
- Esr Check ListDocument8 pagesEsr Check ListMona Ismail AlsomaliNo ratings yet
- Intravenous Maintenance Fluid Therapy in The Pedia PDFDocument18 pagesIntravenous Maintenance Fluid Therapy in The Pedia PDFAdrianRuizNo ratings yet
- Vent Weaning Ped22Document9 pagesVent Weaning Ped22Obed AhumadaNo ratings yet
- Patterns of Creactive Protein Ratio Response To Antibiotics in Pediatric Sepsis A Prospective Cohort StudyDocument6 pagesPatterns of Creactive Protein Ratio Response To Antibiotics in Pediatric Sepsis A Prospective Cohort StudynicloverNo ratings yet
- Covid 19 Faqs Hospitals Hospital Laboratory Acute Care Facility Data ReportingDocument52 pagesCovid 19 Faqs Hospitals Hospital Laboratory Acute Care Facility Data ReportingRajesh SharmaNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Gpas 2015 10 PaediatricsDocument14 pagesGpas 2015 10 PaediatricsZack TaylorNo ratings yet
- Code Team Training and Assessment Best Practices From The Floor UCM - 486059Document34 pagesCode Team Training and Assessment Best Practices From The Floor UCM - 486059JoaoNo ratings yet
- Amanda Hawkins Resume 2024Document1 pageAmanda Hawkins Resume 2024api-484275177No ratings yet
- Iatrogenic Withdrawal Syndrome in Specialty Pediatric Critical CareDocument5 pagesIatrogenic Withdrawal Syndrome in Specialty Pediatric Critical Carefuka priesleyNo ratings yet
- Pediatric Surgery Zimbabwe.Document7 pagesPediatric Surgery Zimbabwe.Thomas MutanikwaNo ratings yet
- Resume KRDocument1 pageResume KRapi-662026473No ratings yet
- Bmjopen 2020 038648Document5 pagesBmjopen 2020 038648MarceloCorralesNo ratings yet
- The Pediatric Early Warning System Score: A Severity of Illness Score To Predict Urgent Medical Need in Hospitalized ChildrenDocument8 pagesThe Pediatric Early Warning System Score: A Severity of Illness Score To Predict Urgent Medical Need in Hospitalized ChildrenRavikiran SuryanarayanamurthyNo ratings yet
- Specialty Rotation Nicu PedsDocument7 pagesSpecialty Rotation Nicu Pedsapi-733590799No ratings yet
- Early Mobilization in The Pediatric Intensive Care Unit A Systematic ReviewDocument6 pagesEarly Mobilization in The Pediatric Intensive Care Unit A Systematic ReviewJuly ZaballaNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet