Professional Documents
Culture Documents
Diabetes
Uploaded by
kep1313Copyright
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Diabetes
Uploaded by
kep1313Copyright:
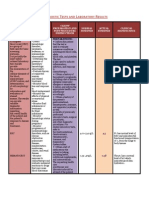
Table 103.
Mediators Implicated in Regulation of Energy Balance Regulation and target effect Released in the duodenum during a meal. Stimulates the vagus nerve projecting to the NTS and signals within the hypothalamus to induce satiety. Produced primarily by the stomach. Levels increase before meals and decrease following a meal. Stimulates growth hormone release, increases food intake. Overall has anti-leptin action. Plasma levels are low in obese patients. Member of the NPY family, released in the distal small intestine and colon in response to food. Blood levels remain elevated between meals. Reduces food intake. Peptide produced in the intestinal cells in response to high intestinal luminal glucose concentrations. Amplifies glucose-induced insulin release from the -cell.
Mediator Cholecystokinin Ghrelin
Gastrointestinal tract
PYY336 GLP-1
Adipose tissue Adiponectin (AdipoQ) Acylationstimulating protein Leptin Resistin Hypothalamus NPY Produced by hypothalamic neurons that express AgRP. Release is under leptin, insulin, and cortisol regulation. Stimulates food intake via the NPY5 receptor. -MSH CART AgRP Orexins (A and B) Diabetes Diabetic ketoacidosis Diabetic ketoacidosis arises from a number of metabolic derangements caused by insulin lack. Treatment is by intravenous fluids, insulin and potassium. Only in the most severe cases of DKA should sodium bicarbonate be used. Close clinical and biochemical monitoring are required to tailor the management protocol to the individual patient. Less common, severe metabolic disturbances of carb meta: hyperosmolar non-ketotic coma and lactic acidosis. Product of POMC in hypothalamic neuronal subset under leptin regulation. Decreases food intake through melanocortin-4 receptors in the hypothalamus. Peptide produced by hypothalamic POMC-expressing neurons stimulated by leptin and amphetamines. Reduces food intake. Released from hypothalamic NPY-expressing neurons. Inhibits neuronal melanocortin-4 receptors and increases food intake. Produced by neurons in the lateral hypothalamus perifornical area. Regulated by glucose, leptin, NPY, and POMC neurons. They stimulate food intake. Increases insulin sensitivity and tissue fat oxidation, resulting in reduced circulating fatty acid levels and reduced intramyocellular and liver triglyceride content. Levels decreased in obese patients; plasma levels correlate negatively with triglycerides. Stimulates triglyceride synthesis in adipocytes, resulting in more rapid postprandial lipid clearance. Stimulates translocation of glucose transporters to the cell surface. Secreted by fat cells in proportion to fat stores. Acts on hypothalamic neurons to decrease food intake. Leptin is necessary for maturation of the reproductive axis. Peptide hormone induced during adipogenesis. It antagonizes insulin action.
Hypoglycemia Hypoglycemia is not diagnosis but is a biochemical sign associated w/ diverse group of diseases. Management is by glucose therapy irrespective of the underlying cause. Excess insulin, excess alcohol or low calorie intake in a diabetic patient are most common causes of hypoglycemia. Insulinoma is characterized by hypoglycemia in the face of inappropriately high plasma insulin. Hypoglycemia in the neonate may result in brain damage. Fasting hypoglycemia: o Insulinoma. Insulin-producing -cell tumors of pancreas may be isolated or part of wider multiple endocrine neoplasia (MEN) syndrome. Insulin-induced weight gain characteristic feature. Tumor localization difficult. o Malignancy. Hypoglycemia can be found w/ any advanced malignancy. Some tumors (retroperitoneal sarcomas) cause hypoglycemia by producing insulin-like growth factors. o Hepatic and renal disease. Both the liver and kidneys are capable of gluconeogenesis. Hypoglycemia is occasionally a feature of advanced hepatic or renal impairment, but this is not diagnostic dilemma. o Addison's disease. Glucocorticoids antagonize insulin actions, adrenal insufficiency hypoglycemia Sepsis. Overwhelming sepsis may be associated with hypoglycemia; the mechanism is unclear. Reactive o Insulin-induced. Inappropriate or excessive insulin predictably produces hypoglycemia. Occasionally it is important to distinguish between exogenous insulin (administered by the patient or someone else) and endogenous insulin. Standard assays for insulin cannot distinguish between the two kinds. However, insulin and its associated connecting peptide (or C-peptide) are secreted by the islet cells in equimolar amounts, and thus measurement of C-peptide along with insulin can differentiate between hypoglycemia due, for example, to an insulinoma (high C-peptide) and that due to exogenous insulin (low C-peptide) o Drug-induced. Oral hypoglycemic, (sulphonylureas) hypoglycemia. Urinary screens for sulphonylureas exist. Other drugs include salicylate, paracetamol and -blockers. B blockers may mask pt awareness of hypoglycemia, by blunting -effect of adrenaline and reduce/eliminating warning symp (palpitation/tremor) o Alcohol. Hypoglycemia is not uncommon in alcoholic patients. Mechanisms include inhibition of gluconeogenesis, malnutrition and liver disease. o Dumping syndrome. Accelerated gastric emptying following gastric resection may result in the rapid absorption of large amounts of glucose with a resultant surge of insulin release. Smaller, more frequent meals may help to minimize this phenomenon. Diabetic patients: insufficient carbohydrate intake, excess of insulin or sulphonylurea, strenuous exercise, excessive alcohol intake. Neonatal: o Small-for-gestational-age infant. Dec glycogen stores/impaired gluconeogenesis contributes. o Babies of diabetic mothers. Fetus exposed to maternal hyperglycemia develops hyperplasia of islet cells and associated hyperinsulinemia. After delivery, neonate unable to suppress high insulin levels that are now inappropriate, and hypoglycemia results. o Nesidioblastosis. Hyperplasia of islet cells develop even if mom not diabetic; unk reason o Inborn errors of metabolism. Ex: FA oxidation defects, glycogen storage diseases and galactosaemia
Left: The differential diagnosis of hypoglycemia in presence high insulin levels. Right: The differential diagnosis of hypoglycemia in the absence of high insulin levels.
You might also like
- Case Studies 10Document5 pagesCase Studies 10kep1313No ratings yet
- Case Studies 8Document7 pagesCase Studies 8kep1313No ratings yet
- Case Studies 9Document7 pagesCase Studies 9kep1313No ratings yet
- Case Studies 1Document11 pagesCase Studies 1kep1313No ratings yet
- Virology 1 3Document5 pagesVirology 1 3kep1313No ratings yet
- Case Studies 7Document6 pagesCase Studies 7kep1313No ratings yet
- Case Studies 5Document4 pagesCase Studies 5kep1313No ratings yet
- Case Studies 3Document4 pagesCase Studies 3kep1313No ratings yet
- Case Studies 6Document8 pagesCase Studies 6kep1313No ratings yet
- Case Studies 4Document4 pagesCase Studies 4kep1313No ratings yet
- Case Studies 2Document4 pagesCase Studies 2kep1313No ratings yet
- SeizuresDocument3 pagesSeizureskep1313No ratings yet
- Week 4 Learning ObjectivesDocument24 pagesWeek 4 Learning Objectiveskep1313No ratings yet
- Biochem MedicineDocument27 pagesBiochem Medicinekep1313No ratings yet
- Neurology Notes For Clerkship ReviewDocument22 pagesNeurology Notes For Clerkship Reviewkep1313No ratings yet
- Physiology - BSDocument14 pagesPhysiology - BSkep1313No ratings yet
- Case 1: Cystic FibrosisDocument5 pagesCase 1: Cystic Fibrosiskep1313No ratings yet
- Week 2 Learning ObjectivesDocument21 pagesWeek 2 Learning Objectiveskep1313No ratings yet
- MicroanatomyDocument59 pagesMicroanatomykep1313No ratings yet
- Week 3 Learning ObjectivesDocument12 pagesWeek 3 Learning Objectiveskep1313100% (1)
- Genetics - MMDocument25 pagesGenetics - MMkep1313No ratings yet
- Week 5 Learning ObjectivesDocument34 pagesWeek 5 Learning Objectiveskep1313No ratings yet
- Psychiatry - BSDocument15 pagesPsychiatry - BSkep1313No ratings yet
- Case 1: Cystic FibrosisDocument5 pagesCase 1: Cystic Fibrosiskep1313No ratings yet
- Preventative Medicine PM - BSDocument22 pagesPreventative Medicine PM - BSkep1313No ratings yet
- Biogenic AminesDocument5 pagesBiogenic Amineskep1313No ratings yet
- Physiology - BSDocument14 pagesPhysiology - BSkep1313No ratings yet
- 2-5-10 HCT For Immunodeficiency and Autoimmune DisordersDocument2 pages2-5-10 HCT For Immunodeficiency and Autoimmune Disorderskep1313No ratings yet
- Biochem MedicineDocument27 pagesBiochem Medicinekep1313No ratings yet
- Anemia DifferentialDocument1 pageAnemia Differentialkep1313No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Practical nursing jeopardy game questions and answersDocument29 pagesPractical nursing jeopardy game questions and answersfairwoods80% (5)
- DR Pankaj NaramDocument20 pagesDR Pankaj NaramNitesh Kumar50% (6)
- FEVER Approach (Paeds)Document3 pagesFEVER Approach (Paeds)NorFarah Fatin AnuarNo ratings yet
- Incidence of Lumbosacral Radiculoplexus Neuropathy and Association with DiabetesDocument8 pagesIncidence of Lumbosacral Radiculoplexus Neuropathy and Association with DiabetesMohammad AjiNo ratings yet
- Benign Prostatic Hyperplasia (BPH) : Russel Cepriano V151622 MOA Feb 2021Document2 pagesBenign Prostatic Hyperplasia (BPH) : Russel Cepriano V151622 MOA Feb 2021Yeasa DolleteNo ratings yet
- Glands and HormonesDocument1 pageGlands and HormonesRussel Dave ValenzuelaNo ratings yet
- GUIDELINES ON MEDICAL SURVEILLANCEDocument139 pagesGUIDELINES ON MEDICAL SURVEILLANCEdean0160260% (1)
- Kendler 2005Document10 pagesKendler 2005MaximilianNo ratings yet
- Mcvary 2011 Update On AUA Guideline BPHDocument11 pagesMcvary 2011 Update On AUA Guideline BPHFoxglove83No ratings yet
- Research Essay - Aiden PsczulkoskiDocument14 pagesResearch Essay - Aiden Psczulkoskiapi-608831675No ratings yet
- Circumcision Devices: A Review of Techniques and TechnologiesDocument43 pagesCircumcision Devices: A Review of Techniques and TechnologiesMakbruri Abdul AzizNo ratings yet
- PracticeExam 2 QsDocument24 pagesPracticeExam 2 QsBehrouz YariNo ratings yet
- Premalignant Lesions & ConditionsDocument76 pagesPremalignant Lesions & ConditionsAman KankariaNo ratings yet
- Science Magazine 5688 2004-08-27Document150 pagesScience Magazine 5688 2004-08-27mrtomissNo ratings yet
- Moderate Consumption of AlcoholDocument5 pagesModerate Consumption of AlcoholpuchioNo ratings yet
- Final DX ResultsDocument9 pagesFinal DX ResultszysheaiNo ratings yet
- Patient FinalDocument51 pagesPatient FinalCharmmaine Yu-AcmanNo ratings yet
- FNCP - TB As A Health DeficitDocument6 pagesFNCP - TB As A Health DeficitIngrid Paula Nicolas100% (4)
- Xii English CoreDocument122 pagesXii English CoreShashwat Vyas0% (2)
- HEMPIRE MagazineDocument105 pagesHEMPIRE MagazineTodd McCormickNo ratings yet
- Lung Poorly Differentiated Adenocarcinoma With Cerebral MetastasesDocument2 pagesLung Poorly Differentiated Adenocarcinoma With Cerebral MetastasesasclepiuspdfsNo ratings yet
- Acid-Base and Electrolyte DisordersDocument13 pagesAcid-Base and Electrolyte DisordersJefferson Rojas GuimarayNo ratings yet
- Expression of Interest Build For Cancer Care Centre - 2Document5 pagesExpression of Interest Build For Cancer Care Centre - 2arakbaeNo ratings yet
- Definition, Types, Signs & Treatment of PneumothoraxDocument62 pagesDefinition, Types, Signs & Treatment of PneumothoraxmithramuruganNo ratings yet
- Syllabus Oncology 2024Document6 pagesSyllabus Oncology 2024Kunal BhamareNo ratings yet
- Philippine Music and Arts QuizDocument4 pagesPhilippine Music and Arts Quizrizabesmonte100% (1)
- Prelim OncologyDocument10 pagesPrelim OncologyErl D. MelitanteNo ratings yet
- UM 1 Mock 2 16.8.18Document18 pagesUM 1 Mock 2 16.8.18Anonymous d1CGjMTiNo ratings yet
- Varicocele and Semen QualityDocument8 pagesVaricocele and Semen QualityGrymjoe Angin EmasNo ratings yet