Professional Documents
Culture Documents
46 66 1 SM
Uploaded by
I Made Agus SetiawanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
46 66 1 SM
Uploaded by
I Made Agus SetiawanCopyright:
Available Formats
.
Bali Medical Journal (BMJ) 2013, Volume 2, Number 2: 55-58
P-ISSN.2089-1180, E-ISSN.2302-2914
EFFECT OF PROPHYLACTIC ANTIBIOTIC ON SURGICAL SITE INFECTION AFTER TENSION-FREE HERNIOPLASTY
1
Saskia-Javi, Y., 1Sudartana, I K., and 2Raka-Widiana, I G.
Surgery Depart. Faculty of Medicine Udayana University/Sanglah General Hospital Bali-Indonesia Internal Depart. Faculty of Medicine Udayana University/Sanglah General Hospital Bali-Indonesia
Objective: prophylactic antibiotics were remains applied for hernioplasty treatment at Sanglah General Hospital Bali-Indonesia. On the other hand, there were no comprehensive infection incidence data gathered. This research aims to determine incidence differences of post operative infection in patients underwent tension-free hernioplasty and received prophylactic antibiotics compared to those who received placebo. The general purpose of this research is to determine the necessity of prophylactic antibiotics in the hope of setting new procedural standards in elective hernia procedures thus reducing cost and bacteria resistance. Patients and Method: This was an open label randomized clinical trial conducted at Sanglah General Hospital Department of General Surgery from October 2011. The target population was all patients who underwent tension-free hernioplasty procedure, in Sanglah General Hospital. The acquired data was analyzed after an independent t test was performed. a Mann-Whitney U test, Fishers exact test, and Two-Sample Kolmogorov-Smirnov test were used to determine the correlations between variables, where p < 0.05 was regardless of significant. Results: From 54 subjects 3 (5.6%) of them were found to have a slight erythema around the operation wound, on the 7th,14th,21th, and 28th day no signs of erythema were found. From the three subjects two (7.4%) were from the placebo group and one (3.7%) from the antibiotic group. All clinical assessment of post operative wound was made using Southampton Wound Assessment Scale, where erythema is a grade 1C, all subjects healed primarily. Conclusion: An Open Label Randomized Clinical Trial comparing SSI in post tension-free hernioplasty patients who were given prophylactic antibiotics and placebo. No significant difference were found. Keywords: Tension-free hernioplasty, prophylactic antibiotic, SSI
INTRODUCTION The incidence of groin hernias, which include inguinal and femoral hernias average at 70 per 10.000 people in the age group of 45 years to 64 years old, increasing to 150 cases per 10.000 people above 75 years old. Inguinal hernia procedures are one of the most common procedures performed. NHS data showed that it is the 10th most often performed operation in England.1 Prophylactic agents are antibiotics which are given before a surgical procedure with the intent of preventing infection or commonly known as surgical site infections (SSI). Out of 23 million patients who underwent surgery in the united states every year, 920.000 suffer from SSI, which increases length of stay twice as long and increases cost to 5 times higher.2 The role of prophylactic antibiotics is still controversial as shown by Jain, et al. (2008) as no decrease in post operative Correspondence: Saskia-Javi, Y. Address: Surgery Depart. Faculty of Medicine Udayana University/Sanglah General Hospital Bali-Indonesia. Email: saskia@gmail.com infection were found,3 Hernioplasty procedure in Sanglah General Hospital still uses prophylactic antibiotics, while a comprehensive infection incidence data has not been gathered. The general purpose of this research is to determine the necessity of prophylactic antibiotics in the hope of setting new standard procedure in elective hernia procedures thus reducing cost and bacterial resistance. PATIENTS AND METHOD This was an open label randomized clinical trial conducted from October 2011. The target population was all patients who underwent tensionfree hernioplasty procedure, with inclusion criterias: patients with primary uni or bi-lateral inguinal hernia who underwent tension-free hernioplasty within the age group of 18-80 years old. Patients with obesity, who are immunocompromized, such as patients with HIV, Diabetes, receiving corticosteroid or chemotherapy, patients with recurrent, strangulated, and incarcerated hernias, allergic to cephalosporins, anemic, low nutritional status, who are taking antibiotics for other medical conditions, and patients with other systemic or chronic illness were
Open access: www.balimedicaljournal.com or www.ojs.unud.ac.id
55
Bali Medical Journal (BMJ) 2013, Volume 2, Number 2: 55-58
P-ISSN.2089-1180, E-ISSN.2302-2914
excluded from the research. the SSI scoring was based on The Southampton Wound Assessment Scale. The subjects were divided into two groups using a permuted block, the first group was given with an open label an intravenous injection 1 gr of cephazolin during induction, and the second group was given a placebo (saline solution). Then a lichtenstein tension-free hernioplasty was performed using the standard operating procedure. post operative control on the 3rd,7th, 14th,21 st and 28th day, for suture removal, and evaluation of infection signs. The acquired data was analyzed after an independent t test was performed. a MannWhitney U test, Fishers exact test, and Two Sample Kolmogorov-Smirnov test was used to
determine the correlations between variables, where p < 0.05. RESULTS Randomization was successful; there were no significant differences with respect to median age, sex, frequencies of different hernia types and location (Table 1). From 54 subjects 3 (5.6%) were found to have a slight erythema around the operation wound, on the 7th,14th,21th, and 28th day no signs of erythema were found. From the three subjects two (7.4%) were from the placebo group and one (3,7%) from the antibiotic group. All clinical assessment of post operative wound was made using Southampton Wound Assessment Scale, where erythema is a grade 1C, all subjects healed primarily (Table 2).
Table 1 Characteristics of Patients With Primary Inguinal Hernia Randomized Between Prophylactic and Placebo Characteristic Sex -Male 26 -Female 1 Age (Year) 45,04 16,803 Hernia Type -Direct 4 -Indirect 23 Hernia Location -Right 14 -Left 10 -Bilateral 3 *Fishers Exact. p < 0.05; **Mann Whitney. p <0.05; Kolmogorov-Smirnov test. p < 0.05 25 2 44,48 18,039 3 24 0.500* 0.883** 0.500*** Antibiotic Group (n = 27) Placebo Group (n = 27) p
13 0.996**** 14 0 ***Fishers Exact. p < 0,05; ****Two-Sample
Table 2 Post operative wound assessment Days Infection Antibiotic Placebo Amount D3 G0 27 27 54 G1 0 0 0 G0 26 25 5 D7 G1C 1 2 3 D14 G0 27 27 54 G1 0 0 0 G0 27 27 54 D21 G1 0 0 0 G0 27 27 54 D28 G1 0 0 0
Description : D3 = Day 3 post operation D7 = Day 7 post operation D14 = Day 14 post operation D28 = Day 28 post operation GO = Normal Healing G1 =Normal healing with erythema G1C =Normal healing with light erythema
Open access: www.balimedicaljournal.com or www.ojs.unud.ac.id
56
Bali Medical Journal (BMJ) 2013, Volume 2, Number 2: 55-58
P-ISSN.2089-1180, E-ISSN.2302-2914
DISCUSSION Hernial repair is a clean procedure, but some surgeons still use prophylactic antibiotics in a lichtenstein procedure as a gold standard, this is assumed due to the use of a mesh as a synthetic material that may increase SSI.4,5 This research has concluded that on elective hernioplasty, clinically using Southampton Wound Assessment Scale, no SSI was found on the post operative wound, as erythema is still considered normal wound healing. This is similar to the results achieved by another author, which states that prophylactic antibiotics are not mandatory for such cases.3,4,6,7,8,9 Infection signs that were found are erythema on the wound (grade 1C) on the 7th day on 1(3.7%) subject of the antibiotic group, and 2 (7.4%) on the placebo group, both cases were treated with wound care and no signs were found on the 7th,14th,21th, and 28th day, and all subjects healed primarily. Aufenacker, et al. (2004) reported SSI of 1.6% on the antibiotics group, and 1.8% on the placebo group6; while Perez et al, (2005) reported SSI of 2.2% on the antibiotics group, and 1,7% on the placebo group7; Tzovaras, et al, (2007) also showed that only 4.7% placebo group and 2,6% on the antibiotic group8. On the other hand, Yerdel, et al.(2001) reported that a decrease of 8.3% infection rates were found by the use of prophylactic antibiotics.10 A meta-analysis by Sanchez et al.(2003) concluded that prophylactic antibiotic use still requires further research.11 A meta-analysis by Gravante et al. (2008) states that a 2.9% on the antibiotic group and 4.2% on the placebo group were found, while 1.7% on the antibiotics group and 3.7% on the placebo group were found on patients using mesh.12 Some studies included only assessed low-risk patients, so conclusion could be applied solely to this kind of patients.13 It should be noted that studies in which the rate of SSI are higher have reported that prophylactic antibiotis are beneficial, whereas similar conclusion could not be derived in the studies with low rates of SSI8. Therefore, surgeons and hospitals must assess their own SSI rates to define if prophylactic antibiotics must be widely used in all patients.13 It is concluded the decision to use prophylactic antibiotic, therefore, must be based on balancing possible benefits against adverse effects.14 Clean operation is a procedure with no mistakes in sterilization, and no leaks on the digestive, respiratory and urinary tract. The four sources of infection are the medical staff, sterilization techniques, environment, and patient risk factors. A surgeon should be able to minimalize such factors. Antibiotics should not be used to replace proper aseptic and antiseptic methods, along with good surgical techniques and proper tissue handling infection can be prevented.15
CONCLUSION Based on this research and other previous research, it can be concluded that no difference were found in the occurence of SSI post tensionfree hernioplasty between patients who received prophylactic antibiotics and placebo. REFERENCES 1. McIntosh, A., Hutchinson, A., and Roberts, A. 2000. Evidence-based management of inguinal hernia in primary care a systematic review. Family Practice. 17: p 442-447. 2. Sunarto, R. 2007. Antibiotik Profilaksis pada Pembedahan. 3. Jain, S. K., Jayant, N., and Norbu, C. 2008. The role of antibiotic prophylaxis in mesh repair of primary inguinal hernias using prolene hernia system: A randomized prospective double-blind control trial. Trop. Doctor. 38:80-82. 4. Shankar, V. G., Srinivasan, K., Sistla, S. C., and Jagdish, S. 2010. Prophylactic antibiotics in open mesh repair of inguinal hernia a randomized controlled trial. Int J of Surgery. 8:444-447. 5. Ijaz, A. A., et al. 2010. Post Operative Wound Infection: Prevention The Role of Antibiotic Prophylaxis in Lichtenstein. Professional Med J. p 174-179. 6. Aufenacker, T. J., Geldere, D., Mesdag, T., Bossers, A. N., et al. 2004. The Role of Antibiotic Prophylaxis in Prevention of Wound Infection after Lichtenstein Open Mesh Repair of Primary Inguinal Hernia. Annals of Surgery, Vol 240. p 955-961. 7. Perez, R. A., Roxas, M. F., and Hilvano, S. S. 2005. A Randomized, Double-blind Placebocontrolled Trial to Determine Effectiveness of Antibiotic Prophylaxis for Tension-free Mesh Herniorrhaphy. J Am Coll Surgeon. Vol 200. No 3: p 393-397. 8. Tzovaras, G., Delikoukos, S., Christodoulides, G., et al. 2007. The Role of Antibiotic Prophylaxis in Elective Tension-Free Mesh Inguinal Hernia Repair: Results of a SingleCentre Prospective Randomised Trial. Int J Clin Pract. Vol 61: p 236-239. 9. Hosseini, M., and Heidari, A. 2011. Evaluation of Prophylactic Antibiotic Prescription in PostOperative Infection in Patients Undergone Inguinal Herniorraphy Surgery with Prolene Mesh: A Randomized Double Blind Study. Surgery Journal. Vol 6: p 21-25. 10. Yerdel, M. A., et al. Effect of Single Dose Prophylactic Ampicillin and Sulbactam on Wound Infection After Tension-free Inguinal Hernia Repair with Polypropylene Mesh. Annals of Surgery. Vol 233. No 1: p 26-33. 11. Manuel-Sanchez, F. J., et al. 2009. Antibiotic Prophylaxis for Hernia Repair; the Cochrane Collaboration. John Wiley and Sons, Ltd.
Open access: www.balimedicaljournal.com or www.ojs.unud.ac.id
57
Bali Medical Journal (BMJ) 2013, Volume 2, Number 2: 55-58
P-ISSN.2089-1180, E-ISSN.2302-2914
12. Gravante, G., Venditti, D., and Vincenzino, F. 2008. The role of single-shot antibiotic prophylaxis in inguinal hernia repair. Annals of Surgery. 248:496-497. 13. Sanabria, A., et al. Prophylactic Antibiotics for Mesh Inguinal Hernioplasty. Annals of Surgery, Vol 245. No 3: p 392-396. 14. Ansari, A. S., Saddique, M., and Azim, W. 2005. Antibiotic Prophylaxis in Clean Surgery. Biomedica. Vol 21: p 121-124.
15. Rose, P. A., and Matti, A. 2002. Prescribing Practices of Surgeons and Factors that Limit Adherence to the Philippine College of Surgeons Clinical Practice Guidelines on Antimicrobial Prophylaxis for Elective Surgical Procedures at the UP-PGH Surgical Wards. Phil J Micobiol Infect Dis. Vol 31: p 107-124.
This work is licensed under a Creative Commons Attribution
Open access: www.balimedicaljournal.com or www.ojs.unud.ac.id
58
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Large Databases in Anaesthesiology: ReviewDocument6 pagesLarge Databases in Anaesthesiology: ReviewSoumya DasNo ratings yet
- Complex Torch Si SarcinaDocument23 pagesComplex Torch Si SarcinamoldoveanuNo ratings yet
- Gastrointestinal Health Problems Test DrillDocument9 pagesGastrointestinal Health Problems Test DrillChristian Angel PoncianoNo ratings yet
- Gowning: Bagasbas, Krizzamer P. Balagso, Jezzica RDocument13 pagesGowning: Bagasbas, Krizzamer P. Balagso, Jezzica RNdor BariboloNo ratings yet
- St. Anthony's College Nursing Care Plan TemplateDocument2 pagesSt. Anthony's College Nursing Care Plan TemplateKristine YoungNo ratings yet
- Comparison Between Proprioceptive Neuromuscular Facilitation and Neuromuscular Reeducation For Reducing Facial Disability and Synkinesis in Patients W PDFDocument8 pagesComparison Between Proprioceptive Neuromuscular Facilitation and Neuromuscular Reeducation For Reducing Facial Disability and Synkinesis in Patients W PDFbenjiNo ratings yet
- HSYLCSyllabus Beijing 2016Document5 pagesHSYLCSyllabus Beijing 2016Akshay SwaminathanNo ratings yet
- OperativenotesinsurgeryDocument9 pagesOperativenotesinsurgerySakib EhsanNo ratings yet
- DR Walsh Autism Ocd Pandas Depression MethylationDocument6 pagesDR Walsh Autism Ocd Pandas Depression MethylationAnupama PouloseNo ratings yet
- Roselet Medical Lab Blood and Urine Test ResultsDocument6 pagesRoselet Medical Lab Blood and Urine Test ResultsDaniel DasNo ratings yet
- Mcmaster Nursing Anatomy 1H06 Tutorial Assignment 3Document6 pagesMcmaster Nursing Anatomy 1H06 Tutorial Assignment 3NTRisforthinkersNo ratings yet
- Patient A (Click On The Link To "Complete Patient A's Karyotype")Document2 pagesPatient A (Click On The Link To "Complete Patient A's Karyotype")ZzaiRraNo ratings yet
- Vital Signs Procedures ChecklistDocument3 pagesVital Signs Procedures ChecklistharpreetNo ratings yet
- Falls in the Elderly: A Practical Guide for Family PhysiciansDocument6 pagesFalls in the Elderly: A Practical Guide for Family PhysiciansrmkNo ratings yet
- Tugas Baca Jurnal BT ShuntDocument53 pagesTugas Baca Jurnal BT ShuntVashNo ratings yet
- Periorbital and Orbital CellulitisDocument51 pagesPeriorbital and Orbital CellulitisJoanne BlancoNo ratings yet
- Magic Touch PDFDocument2 pagesMagic Touch PDFtomNo ratings yet
- Ohio Voter Rights CoalitionDocument19 pagesOhio Voter Rights CoalitionsrichardsonNo ratings yet
- A Look at Bipolar Disorder in Michael ClaytonDocument9 pagesA Look at Bipolar Disorder in Michael ClaytonRichard Moore0% (1)
- Streptococcus Pneumoniae (Pneumococcus) - OverviewDocument4 pagesStreptococcus Pneumoniae (Pneumococcus) - OverviewstarykNo ratings yet
- Management of The Infant With Atypical Genitalia (Disorder of Sex Development) - UpToDateDocument31 pagesManagement of The Infant With Atypical Genitalia (Disorder of Sex Development) - UpToDateNicolle SchioNo ratings yet
- Pharmacy Formulary - Booklet - 2016Document178 pagesPharmacy Formulary - Booklet - 2016pcartercNo ratings yet
- Con TovaDocument2 pagesCon Tovasheik muhtasimNo ratings yet
- Please Note: Slower Titration May Be Appropriate For Some PatientsDocument1 pagePlease Note: Slower Titration May Be Appropriate For Some PatientsSholehuddin MunajjidNo ratings yet
- Teeter FitSpine X1 Inversion Table Owners ManualDocument6 pagesTeeter FitSpine X1 Inversion Table Owners ManualhawkjohnNo ratings yet
- Balance and Fall Prevention: By, Sankari Nedunsaliyan Physiotherapist Dip in PT (MAL), BSC Hons Applied Rehab (UK)Document63 pagesBalance and Fall Prevention: By, Sankari Nedunsaliyan Physiotherapist Dip in PT (MAL), BSC Hons Applied Rehab (UK)Ali ImranNo ratings yet
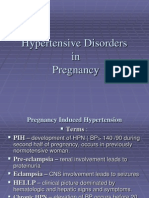
- 001hypertensive Disorders in Pregnancy PDFDocument23 pages001hypertensive Disorders in Pregnancy PDFRosechelle Bas SamsonNo ratings yet
- International Healthcare Conference IHCON 2021 (Virtual) - Free RegistrationDocument8 pagesInternational Healthcare Conference IHCON 2021 (Virtual) - Free RegistrationDr Kishore Kumar D100% (1)
- Postpartum BluesDocument17 pagesPostpartum BluesVeliani Putri anggrainiNo ratings yet
- Understanding Toxic Goiter and Its Nursing CareDocument22 pagesUnderstanding Toxic Goiter and Its Nursing CareJohn Matley Caampued100% (2)