Professional Documents
Culture Documents
JDM Care Plan
Uploaded by
gopscharanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JDM Care Plan
Uploaded by
gopscharanCopyright:
Available Formats
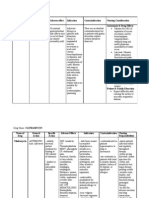
Sr. No.
Nursing Assessment
Child is having Endotracheal Tube in situ and is on Positive Pressure Ventilation with the help of AMBU.
Nursing Diagnosis
Ineffective breathing pattern r/t loss of consciousness as evidenced by irregular breathing and inability to maintain SpO2 WNL Potential for infection r/t Endotracheal tube in situ Potential for altered gas exchange r/t inappropriate manual breaths delivered and pooling of secretions
Expected Outcome
Child follows a regular breathing pattern Child maintain SpO2 WNL Child maintain adequate tissue oxygenation Child develops no signs of infection
Nursing Intervention Planning
Assess the respiratory status by monitoring the rate and depth of respiration. Put the patient on continuous cardiac monitoring and hourly record the readings. Monitor and record SpO2 Give the child semi-fowlers position Monitor and record Vital signs q 1hly Nebulize the child as prescribed
Evaluation
Implementation
Assessed the rate and depth of respiration and recorded them SpO2 :89% every two hourly. No e/o excess Patient is on continuous SpO2 ET secretion or infection monitoring and it is recorded hourly Child is given semi-fowlers position Vital signs monitored and recorded manually every 2hourly Child is being nebulized 4 hourly Oral and ET suction done as needed.
Perform endotracheal suction as needed Two care givers are available and they are doing AMBU Administer antibiotics as alternatively. prescribed Antibiotics given as Ensure always the prescribed availability of a spare care giver in case of emergency
Sr. No.
Nursing Asessment Child is on continuous insulin infusion and has a Bld.Sugar of 192mg/dl
Nursing Diagnosis Altered body functioning r/t impaired glucose metabolism (IDDM) as evidenced by very high blood glucose levels. Potential for Hypo/ Hperglycemia r/t over/ under medication
Expected Outcome Child maintains Blood Glucose levels within normal limits. Planning
Nursing Intervention
Evaluation
Implementation Blood Glucose level monitored and recorded 1 hly and insulin rate titrared accordingly A new chart is maintained where the blood glucose levels and corresponding rate of insulin infusion is recorded hourly. I/O chart maintained. Urine specific gravity monitored once in every shift. Finger tips punctured for glucose monitoring are closely monitored for any pain or redness. Insulin as well as I/V fluids are administered as prescribed.
Assess the Blood Glucose levels frequently Administer Insulin Infusion as prescribed
Blood Glucose: 220mg/dl Insulin infusion :3 units/hr Insulin dose is titrated hourly according to the sliding scale.
Monitor for signs of Hypo/ Child doesnot Hyperglycemia show any s/s Maintain I/O chart of Hypo/ Hyperglycem Measure Urine Specific ia Gravity regularly Record the blood glucose levels and corresponding rate of insulin infusion hourly. Look for any redness or pain at the finger tips punctured for glucose monitoring.
Sr. No.
Nursing Asessment Chid is kept NPO
Nursing Diagnosis Altered fluid electrolyte balance r/t IDDM as evidenced by altered blood electrolyte levels, Polyuria and signs of moderate dehydration
Expected Outcome Child maintains a normal fluidelectrolyte balance
Nursing Intervention
Evaluation
Planning Assess the childs fluidelectrolyte balance Assess the Serum electrolyte levels Connect the child to a continuous cardiac monitor and closely monitor ECG. Administer fluid as prescribed N/2 DNS 5 ml/kg/hr Look for signs of dehydration Maintain Hourly I/O chart Monitor urine o/p and urine specific gravity frequently Assess the nutritional status of the child daily
Implementation Assess the childs fluidelectrolyte balance I/O chart maintained 2hly Electrolyte levels monitored daily Child is on continuous cardiac monitoring. Vital signs are monitored and recorded every 4 hourly Administered fluid as prescribed (N/2 DNS 150ml/hr) Urine op is measured hourly and urine specific gravity is checked in every shift.
Child is maintaining adequate fluid electrolyte balance
Sr. No.
Nursing Asessment Child is bedridden
Nursing Diagnosis Potential for altered skin integrity r/t bed ridden status Self care deficit r/t LoC.
Expected Outcome Child maintains normal skin integrity Childs personal hygiene is maintained
Nursing Intervention
Evaluation
4.
Planning Assess the skin over potential sites of bed sore
Implementation The childs skin is assessed for any redness, blisters or any other early signs of bed sore
Demonstrate to the parents 2 hly back care and Demonstrated to the parents 2 positioning hly back care and positioning Maintain good personal hygiene of the child. Always ensure the linen is dry Avoid pulling the linen under the child which may lead to skin breakdown. Administer high protein diet as prescribed. Demonstrate to the parents bed bath and how to change the childs clothes daily.
Childs personal hygiene is maintained No e/o bed sore
Demonstrated to the parents the technique of changing wet linen while the child is on the bed (Closed bed making) Administered high protein diet as prescribed. Demonstrated to the parents bed bath and how to change the childs clothes daily. Encouraged the parents to do regular back care and change position 2 hourly.
REFERENCES 1. Kliengman and et al; Nelson Textbook of Pediatrics; 18th edition; vol.2; 2404-2429 2. OP Ghai and et al; Ghai Essential Pediatrics; 7th Edition; 434-440 3. Isselbacher et al; Harrisons Principles of Internal Medicine; 16thdition;1252-69 4. Donna L Wong; Essentials of Pediatric Nursing; 5th edition; Pages: 1050-1064. 5. Diabetes Mellitus, Type 1: eMedicine Pediatrics: General Medicine1.mht
You might also like
- Tieraona Low Dog, MD, With and Marc S. Micozzi, MD, PHD (Auth.) - Women's Health in Complementary and Integrative Medicine. A Clinical Guide (2005)Document353 pagesTieraona Low Dog, MD, With and Marc S. Micozzi, MD, PHD (Auth.) - Women's Health in Complementary and Integrative Medicine. A Clinical Guide (2005)Marfu'ah Mar'ahNo ratings yet
- Case No 45: of Intermittent Abdominal Pain Abdominal Bloating and Nausea and Vomiting (NVDocument17 pagesCase No 45: of Intermittent Abdominal Pain Abdominal Bloating and Nausea and Vomiting (NVPremiums of the RoseNo ratings yet
- Health Promotion Model ExplainedDocument6 pagesHealth Promotion Model ExplainedgopscharanNo ratings yet
- NCP DM and HCVDDocument3 pagesNCP DM and HCVDMAYBELINE OBAOB100% (1)
- Roy's Adaptation Model in NursingDocument15 pagesRoy's Adaptation Model in Nursinggopscharan100% (1)
- Valdez Reflective-Questions PDFDocument3 pagesValdez Reflective-Questions PDFDexel Lorren ValdezNo ratings yet
- Ophthalmia Neonatorum: Causes, Symptoms, and Treatment of Neonatal ConjunctivitisDocument30 pagesOphthalmia Neonatorum: Causes, Symptoms, and Treatment of Neonatal ConjunctivitisLing TaerahkunNo ratings yet
- Application of Theory in Nursing ProcessDocument4 pagesApplication of Theory in Nursing ProcessgopscharanNo ratings yet
- Evidence Based Practice FinalDocument22 pagesEvidence Based Practice Finalgopscharan100% (1)
- NCP QuizonDocument2 pagesNCP QuizonChe ValenzuelaNo ratings yet
- Mtap - Virology NotesDocument7 pagesMtap - Virology NotesMoira Pauline LibroraniaNo ratings yet
- Working PhaseDocument7 pagesWorking PhaseSytrose MoralesNo ratings yet
- Abdellah TheoryDocument12 pagesAbdellah TheorygopscharanNo ratings yet
- Nursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermDocument4 pagesNursing Care Plan: Risk For Ineffective Airway Clearance Related To Bleeding From Tonsillectomy Short TermErika Danalle ArceoNo ratings yet
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliNo ratings yet
- NCP PainDocument2 pagesNCP PainApril_Ivy_Raga_3835No ratings yet
- Drug StudyDocument24 pagesDrug Studyabulan100% (1)
- Case 1 - Pneumonia (Final)Document4 pagesCase 1 - Pneumonia (Final)Joegie ArioNo ratings yet
- Nursing Care Plan On Platelet DisordersDocument8 pagesNursing Care Plan On Platelet DisordersbhavanaNo ratings yet
- Nursing Care PlansDocument5 pagesNursing Care PlansMargaret SibugNo ratings yet
- Nursing Diagnosis: Impaired Comfort—pruritisDocument5 pagesNursing Diagnosis: Impaired Comfort—pruritisBondan PalestinNo ratings yet
- Managing Electrolyte Imbalances: A Case of Self-Induced HyperkalemiaDocument3 pagesManaging Electrolyte Imbalances: A Case of Self-Induced HyperkalemiaPaul JacksonNo ratings yet
- Nursing Care Plan EportfolioDocument14 pagesNursing Care Plan Eportfolioapi-279212367No ratings yet
- Chest Pain Care PlanDocument2 pagesChest Pain Care Planapi-545292605No ratings yet
- PROM Guide - Written RequirementsDocument22 pagesPROM Guide - Written RequirementsDarla Janyll RegañonNo ratings yet
- Date/ Time/ Shift Cues Need Nursing Diagnosis With Rationale Objectives of Care Nursing Interventions With Rationale EvaluationDocument2 pagesDate/ Time/ Shift Cues Need Nursing Diagnosis With Rationale Objectives of Care Nursing Interventions With Rationale EvaluationPauleen Trisha SamparaniNo ratings yet
- Lab 5 Diabetes InsipidusDocument6 pagesLab 5 Diabetes InsipidusLisa EkapratiwiNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationFredie O HadjimudinNo ratings yet
- Healthcare - Nursing Care Plan - Excess Fluid VolumeDocument4 pagesHealthcare - Nursing Care Plan - Excess Fluid VolumeBenjamin CañalitaNo ratings yet
- Drug Study PneumoniaDocument2 pagesDrug Study Pneumoniamadelaine_espirituNo ratings yet
- NCP M7Document3 pagesNCP M7rjalavazo1989No ratings yet
- NCP Risk InfectionDocument1 pageNCP Risk InfectionEni RahmawatiNo ratings yet
- Nutrition diagnosis: Imbalanced nutrition less than requirementsDocument3 pagesNutrition diagnosis: Imbalanced nutrition less than requirementsIlisa ParilNo ratings yet
- Case CHFDocument10 pagesCase CHFAgnes Erlita Distriani Patade50% (2)
- NCP AnxietyDocument1 pageNCP AnxietyUnang MagnayeNo ratings yet
- Subjective: "Sumikip Ang Dibdib Ko at Hindi Ako Makahinga NG Maayos" As IndependentDocument2 pagesSubjective: "Sumikip Ang Dibdib Ko at Hindi Ako Makahinga NG Maayos" As IndependentCorinneNo ratings yet
- Nursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleDocument8 pagesNursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleTrysna Ayu SukardiNo ratings yet
- Risk For Falls As Evidence by Loss of BalanceDocument4 pagesRisk For Falls As Evidence by Loss of BalanceAlexandrea MayNo ratings yet
- NCP Proper CholecystectomyDocument2 pagesNCP Proper CholecystectomyGail Lian SantosNo ratings yet
- Drug StudyDocument8 pagesDrug StudyRizzi DeveraNo ratings yet
- Primaxin (Imipenem - Cilistatin)Document2 pagesPrimaxin (Imipenem - Cilistatin)ENo ratings yet
- NCP GeDocument14 pagesNCP GeSuluhTriUtomoNo ratings yet
- Renal Failure NCPDocument3 pagesRenal Failure NCPjsksNo ratings yet
- Pharmacologic management of bleomycinDocument1 pagePharmacologic management of bleomycinKim ApuradoNo ratings yet
- Polycythemia in NewbornDocument25 pagesPolycythemia in NewbornTheva Thy100% (2)
- 6 Nursing Care Plan 1Document2 pages6 Nursing Care Plan 1Denise Louise PoNo ratings yet
- Nursing Care Plan: Acute Pain Related To Inflammatory Response Secondary To InfectionDocument2 pagesNursing Care Plan: Acute Pain Related To Inflammatory Response Secondary To InfectionTammy De GuzmanNo ratings yet
- Nursing Care for Victims of AbuseDocument5 pagesNursing Care for Victims of AbuseNaomi VirtudazoNo ratings yet
- Drug Classification: Antacid & Antihistamine Student ReportDocument2 pagesDrug Classification: Antacid & Antihistamine Student ReportKish AmoreNo ratings yet
- Sas 34Document3 pagesSas 34Sistine Rose LabajoNo ratings yet
- Lack of Knowledge On Diabetes Management or Blood Glucose ManagementDocument2 pagesLack of Knowledge On Diabetes Management or Blood Glucose ManagementDanica Kate GalleonNo ratings yet
- NSTEMIDocument33 pagesNSTEMIwaazalimahwahidNo ratings yet
- Nursing Care Plan Pr/Annex: Saint Louis University Baguio City, Philippines School of NursingDocument7 pagesNursing Care Plan Pr/Annex: Saint Louis University Baguio City, Philippines School of NursingKAREN DAOAYNo ratings yet
- Hypertension NclexDocument5 pagesHypertension Nclexハニファ バランギNo ratings yet
- Nursing Care Plan for Diabetic KetoacidosisDocument3 pagesNursing Care Plan for Diabetic KetoacidosisHanz AlecNo ratings yet
- NCP For COPDDocument3 pagesNCP For COPDcy belNo ratings yet
- Nursing Care Plan for TonsillitisDocument11 pagesNursing Care Plan for TonsillitisJorgia SalardaNo ratings yet
- NCP PainDocument1 pageNCP PaindwightciderNo ratings yet
- HypopituitarismDocument2 pagesHypopituitarismAnne de VeraNo ratings yet
- Nursing Care Plan for Hypokalemia: Monitoring and Maintaining Serum Potassium LevelsDocument2 pagesNursing Care Plan for Hypokalemia: Monitoring and Maintaining Serum Potassium LevelsDoneva Lyn MedinaNo ratings yet
- NCPDocument5 pagesNCPMcmc Ryan Ferdinand GutierrezNo ratings yet
- PneumoniaDocument2 pagesPneumoniaPia MedinaNo ratings yet
- Drug PepcidDocument2 pagesDrug PepcidSrkocher0% (1)
- Acute Pyelonephritis Nursing Care PlansDocument2 pagesAcute Pyelonephritis Nursing Care PlansJoannah Marie Juloya Kiat-ong100% (1)
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanNo ratings yet
- Ranitidine, ParacetamolDocument3 pagesRanitidine, ParacetamoltaekadoNo ratings yet
- A Client With Cushing's Syndrome: Nursing Care PlanDocument1 pageA Client With Cushing's Syndrome: Nursing Care PlanJulius Caesar ColladoNo ratings yet
- Rheumatoid Arthritis Nursing Care PlanDocument22 pagesRheumatoid Arthritis Nursing Care PlanLorelyn Santos Corpuz100% (1)
- Tool 2Document5 pagesTool 2gopscharanNo ratings yet
- V LBW UpdateDocument46 pagesV LBW UpdategopscharanNo ratings yet
- Extremely Low Birth Weight GopalDocument20 pagesExtremely Low Birth Weight GopalgopscharanNo ratings yet
- SyphilisDocument25 pagesSyphilisgopscharanNo ratings yet
- Very Low and Extremely Low Birthweight Infants: Intensive Care Nursery House Staff ManualDocument4 pagesVery Low and Extremely Low Birthweight Infants: Intensive Care Nursery House Staff ManualRobert-Eugen AsproniuNo ratings yet
- Multan MushtaqDocument53 pagesMultan MushtaqBayu Mario GintingNo ratings yet
- Ophthalmia neonatorumIIDocument29 pagesOphthalmia neonatorumIIgopscharanNo ratings yet
- IschemiaDocument81 pagesIschemiagopscharanNo ratings yet
- DDocument4 pagesDgopscharanNo ratings yet
- NeisseriaDocument62 pagesNeisseriaTohidul Islam NomanNo ratings yet
- Physiology of The Coronary Blood FlowDocument14 pagesPhysiology of The Coronary Blood FlowgopscharanNo ratings yet
- Lecture 11Document43 pagesLecture 11gopscharanNo ratings yet
- Opthalmia UmDocument23 pagesOpthalmia Umnanu-jenuNo ratings yet
- Statistics 542 Introduction To Clinical TrialsDocument108 pagesStatistics 542 Introduction To Clinical TrialsDrvinay GoudNo ratings yet
- Polymerase Chain ReactionDocument17 pagesPolymerase Chain Reactionabisantiago6131No ratings yet
- Patients Receive Blood and Blood Products For A Number of ReasonsDocument4 pagesPatients Receive Blood and Blood Products For A Number of ReasonsgopscharanNo ratings yet
- ADocument4 pagesAgopscharanNo ratings yet
- Human BehaviourDocument15 pagesHuman BehaviourgopscharanNo ratings yet
- Tyler Objective Model Group PresentationDocument23 pagesTyler Objective Model Group PresentationAbhi JainNo ratings yet
- What Is Evidence-Based Medicine?: Supported by Sanofi-AventisDocument10 pagesWhat Is Evidence-Based Medicine?: Supported by Sanofi-Aventisapi-273771932No ratings yet
- Advanced Concepts Paper 2Document10 pagesAdvanced Concepts Paper 2Biju AntonyNo ratings yet
- Urinary Tract Infections in Children: Diagnostic Imaging Based On Clinical Practice GuidelinesDocument60 pagesUrinary Tract Infections in Children: Diagnostic Imaging Based On Clinical Practice GuidelinesgopscharanNo ratings yet
- HDocument6 pagesHgopscharanNo ratings yet
- Fast Hugs BidDocument2 pagesFast Hugs Bidgopscharan50% (2)
- New Roles Pharmacists: Value-Based Pay Creates OpportunitiesDocument33 pagesNew Roles Pharmacists: Value-Based Pay Creates OpportunitiesAnonymous EAPbx6No ratings yet
- Reimbursement Claim Form of National Insurance CompnayDocument4 pagesReimbursement Claim Form of National Insurance CompnayVidya Sagar TamminaNo ratings yet
- Handwashing Poster PresentationDocument1 pageHandwashing Poster Presentationapi-372418362100% (1)
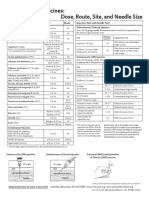
- Injection Site and Needle Size Vaccine Dose RouteDocument1 pageInjection Site and Needle Size Vaccine Dose RouteDr Ambana GowdaNo ratings yet
- Pengaruh Deep Breathing Terhadap Kecemasan Pra OperasiDocument14 pagesPengaruh Deep Breathing Terhadap Kecemasan Pra OperasiAch ThungNo ratings yet
- IV Power PointDocument60 pagesIV Power PointJoseph RadislaoNo ratings yet
- Deafness & Hearing LossDocument39 pagesDeafness & Hearing LossjialeongNo ratings yet
- A Study To Assess The Effectiveness of Hibiscus Sabdariffa On Hypertensive Patients in Rural AreaDocument6 pagesA Study To Assess The Effectiveness of Hibiscus Sabdariffa On Hypertensive Patients in Rural AreaEditor IJTSRDNo ratings yet
- Definition of Cancer and ChemotherapyDocument1 pageDefinition of Cancer and ChemotherapymegamarwaNo ratings yet
- Cultural Factors in Epidemiology - RobiDocument13 pagesCultural Factors in Epidemiology - RobiHasan AnikNo ratings yet
- Focal Infection Theory: A Focus On Current AspectsDocument7 pagesFocal Infection Theory: A Focus On Current AspectsDiandra Puspa WidyasariNo ratings yet
- Medigroup Proposal For ICU BedsDocument13 pagesMedigroup Proposal For ICU Bedsmohyeb padamshiNo ratings yet
- AbstractDocument30 pagesAbstractข้าวเม่า ทอดNo ratings yet
- Philippine Health Care Providers Vs Commissioner of Internal Revenue 554 SCRA 411Document9 pagesPhilippine Health Care Providers Vs Commissioner of Internal Revenue 554 SCRA 411Clarinda MerleNo ratings yet
- Drug Discovery & Clinical Evaluation of New DrugsDocument19 pagesDrug Discovery & Clinical Evaluation of New DrugsKeerthi Sagar100% (1)
- Drug Study Paracetamol Ambroxol Ascorbic Acid CefuroximeDocument6 pagesDrug Study Paracetamol Ambroxol Ascorbic Acid CefuroximeJaymark LambinoNo ratings yet
- OET Writing Referral Letter for Michelle BennettDocument3 pagesOET Writing Referral Letter for Michelle BennettJigesh JosephNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationMary Hope BacutaNo ratings yet
- Radiofrequency AblationDocument7 pagesRadiofrequency AblationRohit singhNo ratings yet
- Pedia Tickler Update 2017Document2 pagesPedia Tickler Update 2017Tani BokNo ratings yet
- M. Sc. Nursing Programme Analysis: Post-Graduate Education-Msc NursingDocument11 pagesM. Sc. Nursing Programme Analysis: Post-Graduate Education-Msc NursingMallika JoonNo ratings yet
- UK Patient Metoclopramide Medication LeafletDocument3 pagesUK Patient Metoclopramide Medication Leafletmarisa apriliaNo ratings yet
- Observational Studies Lecture - ReviewDocument3 pagesObservational Studies Lecture - ReviewKelsey AndersonNo ratings yet
- CASE ANALYSIS - Nasopharyngeal CancerDocument8 pagesCASE ANALYSIS - Nasopharyngeal CancerTerry Mae Atilazal SarciaNo ratings yet
- GSK's ceedd Pioneers New Medicine QuestDocument2 pagesGSK's ceedd Pioneers New Medicine QuestGeorge DupontNo ratings yet
- The Periodontal Abscess: A ReviewDocument10 pagesThe Periodontal Abscess: A ReviewRENATO SUDATINo ratings yet
- Vaccines For Corona Virus Project-1Document28 pagesVaccines For Corona Virus Project-1Ananya PuhanNo ratings yet