Professional Documents
Culture Documents
Azithromycin, Clarithromycin, and Telithromycin
Uploaded by
Angel Medina MendozaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Azithromycin, Clarithromycin, and Telithromycin
Uploaded by
Angel Medina MendozaCopyright:
Available Formats
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
Official reprint from UpToDate www.uptodate.com 2013 UpToDate
Azithromycin, clarithromycin, and telithromycin Author Amy L Graziani, PharmD Disclosures All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jul 2013. | This topic last updated: May 9, 2013. INTRODUCTION Azithromycin (Zithromax) and clarithromycin (Biaxin) are macrolide antibiotics that are used in the treatment of community-acquired respiratory tract infections, particularly pneumonia. They are derivatives of the older macrolide antibiotic, erythromycin. Structural modifications of erythromycin cause a change in the spectrum of activity, dosing, and administration of the newer macrolides and ketolides. Telithromycin (Ketek) is the first member of the ketolide class of antimicrobials, which is related to the macrolide class. Concerns about postmarketing reports of hepatotoxicity and exacerbations of myasthenia gravis have led to significant restrictions on the use of telithromycin. (See 'Warnings about telithromycin' below.) The spectrum of activity, mechanisms of action and resistance, pharmacokinetics, interactions with other drugs, and adverse effects of these newer macrolide antibiotics will be reviewed here. The use of these drugs for communityacquired pneumonia is discussed separately. (See "Treatment of community-acquired pneumonia in adults in the outpatient setting" and "Treatment of community-acquired pneumonia in adults who require hospitalization".) The macrolides are sometimes used for their antiinflammatory effects. This is discussed in detail separately. (See "Cystic fibrosis: Overview of the treatment of lung disease", section on 'Macrolide antibiotics' and "Chronic lung transplant rejection: Bronchiolitis obliterans", section on 'Treatment' and "Diffuse panbronchiolitis", section on 'Macrolide antibiotics'.) MECHANISM OF ACTION AND CHEMICAL STRUCTURE The mechanism of action of the newer macrolides is similar to that of erythromycin. They bind to the 50S subunit of bacterial ribosomes, leading to inhibition of transpeptidation, translocation, chain elongation and, ultimately, bacterial protein synthesis [1,2]. Clarithromycin has the same macrolide, 14-membered lactone ring as erythromycin; the only difference is that at position six a methoxy group replaces the hydroxyl group [1]. Azithromycin, in comparison, has a 15-membered ring and a methyl-substituted nitrogen replacing the 9A carbonyl group. For this reason, azithromycin is more precisely referred to as an azalide rather than a macrolide [2-4]. These structural changes have made the newer macrolides more acid-stable than erythromycin, providing improved oral absorption, tolerance, and pharmacokinetic properties. The newer macrolides also have a broader spectrum of antibacterial activity than erythromycin [1,2]. The ketolide, telithromycin, was designed to specifically target macrolide-resistant respiratory tract pathogens. It has a keto group substituted for the L-cladinose at C3, a methoxy group at C6, and an N-substituted carbamate at C11/C12. These modifications enable telithromycin to bind more tightly to ribosomal RNA, which increases its potency, decreases the selection of bacterial resistance, increases its activity against erythromycin-resistant strains, and improves the pharmacokinetics. RESISTANCE Acquired macrolide resistance is an increasing problem. As with resistance to other drugs, antibiotic use has been associated with development of resistance. This relationship was directly demonstrated in a randomized,
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teTerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full Page 1 of 15
Section Editor David C Hooper, MD
Deputy Editor Anna R Thorner, MD
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
double-blind trial in which 224 healthy volunteers were assigned to azithromycin, clarithromycin, or placebo; the end point was the development of pharyngeal carriage of macrolide-resistant streptococci [5]. The proportion of macrolideresistant streptococci was 26 to 30 percent at baseline. Both macrolides significantly increased the proportion of macrolide-resistant streptococci compared to placebo, peaking at day four to eight, with a mean increase of about 50 percent (to an absolute proportion of over 80 percent) compared with a 4 percent increase with placebo. The increase in resistance was greater with azithromycin, a possible reflection of its much longer half-life. Two main mechanisms of acquired macrolide resistance have been described [6-8]: Methylases encoded by the erm (erythromycin ribosome methylase) genes (ermA, ermB, ermC) alter the macrolide binding site on the bacterial ribosomal RNA, usually conferring a high degree of macrolide resistance [9]. In a study of selected resistance in volunteers, clarithromycin but not azithromycin selected for this type of resistance [5]. This mechanism also usually confers resistance to clindamycin. (See "Clindamycin: An overview", section on 'Resistance'.) Active macrolide efflux pumps, encoded by the mef (macrolide efflux) msrA and msrB genes, confer a low to moderate degree of macrolide resistance [9-11] These mechanisms are responsible for erythromycin resistance in most gram-positive cocci (eg, Staphylococcus aureus, Streptococcus pneumoniae, other streptococci). In contrast to the mechanisms of acquired resistance, intrinsic resistance exhibited by Enterobacteriaceae, Pseudomonas spp, and Acinetobacter spp is due to decreased permeability of the outer cell envelope. Mechanisms of resistance to azithromycin or clarithromycin are the same as or similar to those of erythromycin. There is complete cross-resistance between erythromycin, azithromycin, and clarithromycin for gram-positive organisms by the alteration in ribosomal RNA mechanism. In contrast, resistance to telithromycin by this mechanism is as yet uncommon; as a result, telithromycin is active against many erythromycin-resistant respiratory pathogens. However, resistance due to ketolide efflux pumps can cause resistance to telithromycin [12]. Telithromycin-resistant isolates have been isolated in vitro, and a case report has documented a telithromycin-resistant S. pneumoniae isolate recovered from blood following telithromycin treatment [13]. The incidence of macrolide-resistant S. pneumoniae isolates increased from 10.6 percent in 1995 to 20.4 percent in 1999. However, in cities in the United States where pneumococcal vaccination of children has been widespread, there was a distinct reduction in the overall prevalence of macrolide resistance among invasive isolates in 2002. (See "Resistance of Streptococcus pneumoniae to the macrolides, azalides, lincosamines, and ketolides", section on 'Prevalence of resistance'.) Azithromycin, clarithromycin, and telithromycin have enhanced gram-negative activity compared with erythromycin. As a result, selected erythromycin-resistant gram-negative organisms may be sensitive to the newer drugs. Increasing resistance to azithromycin has been described in patients with syphilis; the frequency varies with geographic area. (See "Pathogenesis, clinical manifestations, and treatment of early syphilis", section on 'Treatment'.) SPECTRUM OF ACTIVITY Azithromycin, clarithromycin, and telithromycin have a broader spectrum of activity than erythromycin [14]. The greatest use of the macrolides is in upper respiratory tract infections; azithromycin, clarithromycin, and telithromycin have activity against erythromycin-sensitive Streptococcus pneumoniae, Haemophilus spp, Moraxella catarrhalis, and atypical pneumonia pathogens, including Legionella pneumophila, Chlamydophila (formerly Chlamydia) pneumoniae, and Mycoplasma pneumoniae. Telithromycin also has activity against many erythromycin-resistant S. pneumoniae. Azithromycin is more effective in vitro against most strains of H. influenzae, and has more rapid killing and a longer postantibiotic effect than clarithromycin [14,15]. Despite the fact that clarithromycins 14-hydroxy metabolite has activity against H. influenzae, in one study, only 63 percent of H. influenzae isolates were susceptible to clarithromycin, whereas
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teTerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full Page 2 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
96 percent were susceptible to azithromycin [16]. For this reason, azithromycin is preferred over clarithromycin in outpatients with community-acquired pneumonia who have comorbidities, such as chronic obstructive pulmonary disease [15]. Erythromycin does not have activity against H. influenzae. (See "Treatment of community-acquired pneumonia in adults in the outpatient setting" and "Antibiotic studies for the treatment of community-acquired pneumonia in adults", section on 'Macrolide resistance'.) These antibiotics are also usually active against other gram-positive organisms including Staphylococcus aureus (except for methicillin-resistant S. aureus), and Group A, B, C, and G streptococcus. Resistance to either azithromycin or clarithromycin by gram-positive organisms results in cross resistance to the other macrolides; however, this cross resistance is not necessarily true with telithromycin. As an example, telithromycin is active against many erythromycin-resistant S. pneumoniae and Streptococcus pyogenes and is more active than azithromycin and clarithromycin in vitro against erythromycin-sensitive S. aureus [14]. The newer macrolides have enhanced gram-negative activity compared with erythromycin. As a result, an erythromycinresistant gram-negative organism may be sensitive to azithromycin, clarithromycin, and/or telithromycin. The gramnegative spectrum includes activity against Escherichia coli, Salmonella spp, Yersinia enterocolitica, Shigella spp, Campylobacter jejuni, Vibrio cholerae, Neisseria gonorrhoeae, and Helicobacter pylori. Clarithromycin and azithromycin are the primary agents used to treat Mycobacterium avium complex infections. (See "Mycobacterium avium complex (MAC) infections in HIV-infected patients" and "Treatment of nontuberculous mycobacterial infections of the lung in HIV-negative patients".) METABOLISM AND PHARMACOKINETICS Clarithromycin, azithromycin, and telithromycin have improved oral absorption, longer serum half-lives, and better tissue and intracellular penetration than erythromycin. Only azithromycin is available in an intravenous formulation. Acid stability and food Azithromycin, clarithromycin, and telithromycin are stable at gastric pH. As a result, their bioavailability is better than that of erythromycin base (37 versus 25 percent), and enteric coating is not required. All of the newer tablet formulations and oral suspensions, except for extended-release clarithromycin, can be taken with or without food [1,4,17]. The serum concentrations attained with oral azithromycin are much lower than those of clarithromycin. A regimen of 500 mg on day one followed by 250 mg/day for nine days leads to an average plasma azithromycin concentration of 0.21 mcg/mL [2-4,18,19]. The extended-release oral suspension of azithromycin (Zmax, given as a single dose per week) results in a higher peak serum concentration and more systemic exposure than can be achieved with standard regimens of immediate-release azithromycin [20]. The oral bioavailability of the original clarithromycin (dosed every 12 hours) tablets is approximately 50 percent; the mean steady state peak serum concentration following 500 mg orally every 12 hours is 2 to 3 mcg/mL [21]. The newer, extended-release clarithromycin tablets (Biaxin XL, dosed once daily) have inactive ingredients in the tablet that bind to clarithromycin and slow gastric absorption. The peak serum concentration is lower than the original clarithromycin tablets and is delayed until five to eight hours following the dose. Patients should be instructed to take the extended-release tablets with food because fasting decreases the area under the plasma concentration-time curve (AUC) by 30 percent. Telithromycin is well absorbed from the GI tract (90 percent), but a third of the dose is metabolized via first pass metabolism by the liver and intestine, resulting in an oral bioavailability of 57 percent [12]. Peak plasma levels one to two hours after an 800 mg oral dose are 1.8 to 2.2 mcg/mL. The plasma half-life is 9.8 hours at steady state [22]. Food does
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teTerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full Page 3 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
not affect the rate or extent of absorption of telithromycin. Tissue and intracellular penetration All macrolides and ketolides distribute and concentrate well in most body tissues and phagocytic cells. Thus, the tissue levels, epithelial lining fluid, and alveolar macrophage concentrations are usually higher than those in the plasma [1,4]. Telithromycin is the most highly concentrated in tissue, followed by azithromycin, clarithromycin, and erythromycin [1,21]. Telithromycin achieves concentrations in lower respiratory tract infection sites that are higher than the MICs of most respiratory pathogens [17]. As an example, telithromycin concentrates intracellularly in alveolar macrophages (at least 400-fold higher than concomitant serum concentrations) and in polymorphonuclear cells (200 to 300-fold higher than concomitant serum concentrations) [14,23]. Azithromycin levels in sputum and lung are 10 to 100 times those in the plasma; alveolar macrophage and neutrophil concentrations are also higher [2,4,21]. In comparison, clarithromycin levels in the lung are only six to eight times higher than the plasma concentration [19]. These differences in intracellular penetration and plasma concentration are two reasons that comparison of these agents by traditional, in vitro methods (such as MIC) is difficult. The clinical significance of the better tissue penetration but lower plasma levels of telithromycin and azithromycin is not known. Active metabolites Azithromycin is excreted in the bile and then the feces, with very little unchanged drug appearing in the urine [2,4]. Several azithromycin metabolites have been identified, but none is known to be biologically active [4,24]. Clarithromycin is hydroxylated, N-demethylated, and hydrolyzed in the liver, utilizing the cytochrome P450 enzyme system. The major metabolite, 14-hydroxy-clarithromycin, is microbiologically active [1,2], and it is more active than the parent compound against some species. As an example, among H. influenzae isolates from patients with communityacquired pneumonia, the concentration at which 90 percent of organisms are inhibited (MIC90) of the 14-OH metabolite was 3 mcg/mL compared with 9 mcg/mL for the parent compound [16]. This active clarithromycin metabolite is another variable that makes a comparison between clarithromycin and azithromycin difficult in vitro. Twenty to 30 percent of clarithromycin is excreted unchanged in the urine [25]. Telithromycin has multiple routes of elimination: seven percent is eliminated in the feces, 13 percent is excreted unchanged in the urine, and the remainder is metabolized by hepatic CYP450 and non-CYP450 pathways. Up to four major metabolites appear to have antibacterial activity, although the activity is weak, only about 6 percent as potent as telithromycin [23]. DOSING AND ADMINISTRATION Azithromycin Compared to clarithromycin, azithromycin is typically given for a shorter period because of the long intracellular half-life (40 to 68 hours) and slow release from tissue sites. Thus, for many infections, a once-daily, five day regimen is as effective as 10 day courses of the other macrolides. Azithromycin is available in several different formulations, including 250, 500, and 600 mg tablets and a 100 mg/5 mL or 200 mg/5 mL pediatric preparation. Azithromycin is also available as an intravenous formulation. The infusion volumes are relatively large (250 mL to 500 mL) and the infusion rates are long (three hours for the 1 mg/mL concentration and one hour for the 2 mg/mL concentration). The 2 g extended-release oral suspension of azithromycin (Zmax) has an even shorter regimen as it is given as a single dose, because of the long half-life [20]. Clarithromycin Clarithromycin is available in the original tablets (250 and 500 mg) and extended release tablets (Biaxin XL, 500 mg). There is no intravenous formulation.
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teTerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full
Page 4 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
A pediatric formulation is available including tablets or granules for oral suspension (125 mg/5 mL and 250 mg/5 mL) [24]. The suspension should not be refrigerated because it can become very viscous and difficult to shake adequately. Warnings about telithromycin Telithromycin is available in 400 mg tablets. There is no intravenous formulation. Because of reports of potentially fatal hepatotoxicity, potentially fatal exacerbations of myasthenia gravis, and visual disturbances, the United States Food and Drug Administration (FDA) concluded in February 2007 that the risks associated with telithromycin outweigh its benefits for minor illnesses, and that telithromycin should not be used to treat sinusitis or bronchitis [26]. Even among patients with mild to moderate community-acquired pneumonia, the FDA concluded that telithromycin should be a secondary alternative to other antimicrobial drugs. A black box warning was added to the label stating that telithromycin should not be used in patients with myasthenia gravis. There has been some controversy over the review and monitoring of the hepatotoxicity pre- and postmarketing [26,27]. SPECIAL POPULATIONS Renal insufficiency Azithromycin dosing does not require adjustment with decreased creatinine clearance. In patients with a creatinine clearance below 30 mL/min, the dose of clarithromycin should be reduced by half or the dosing interval should be doubled. Telithromycin dosing does not require adjustment with mild-to-moderate renal impairment (creatinine clearance 30 mL/min). No dose has been established for patients with severe renal impairment, but the drug accumulates with decreased renal function. As a result, dose adjustment should be considered in these patients. Pregnancy Erythromycin should be considered the safest macrolide in pregnant women, because of the many years of clinical experience. Of the newer macrolides, there is more experience during pregnancy with azithromycin than clarithromycin, or telithromycin. Azithromycin Azithromycin is a United States Food and Drug Administration (FDA) pregnancy category B drug (ie, no evidence of risk in pregnant humans), the same category as for erythromycin (table 1) [24,28]. There are several reports of the use of azithromycin in pregnant women [29-31]. In two studies, patients with cervical chlamydial infection received a 1 g dose of azithromycin and were followed for efficacy and toxicity [29,30]. Teratogenic effects were not noted, although it is not clear if neonatal examination and follow-up were required. More recently, 123 pregnant women taking azithromycin were prospectively followed along with two groups of matched controls [31]. The incidence of major malformations was similar in the azithromycin-exposed and unexposed groups and was not more than the 1 to 3 percent that would be expected in the general population. All three of the malformations occurred in the infants of azithromycin-exposed women who were treated for five days for upper respiratory tract infections. This study was underpowered to detect a difference between the azithromycin-exposed and unexposed groups. The safety of this agent in pregnant women is not definitively known. Clarithromycin Clarithromycin is a pregnancy category C drug (ie, risk cannot be ruled out) (table 1) [32]. Teratogenic effects (including cleft palate, cardiovascular anomalies, and fetal growth restriction) have occurred in monkeys, rats, mice, and rabbits with plasma clarithromycin concentrations 2 to 17 times the levels normally achieved in humans. The labeling states that no adequate and well-controlled trials in pregnant women have been performed; as a result, clarithromycin should be used in pregnant women only if the potential benefit justifies the potential risk to the fetus [32]. Telithromycin Telithromycin is a pregnancy category C drug (table 1). In rats and rabbits at high doses, maternal toxicity may result in delayed fetal maturation; in rats, it is excreted in breast milk [33]. ADVERSE REACTIONS The newer macrolides are generally better tolerated than erythromycin. Because of its more frequent gastrointestinal side effects and risk of QT prolongation and sudden death, erythromycin is now rarely recommended. Erythromycin was the first macrolide to be associated with QT prolongation, but subsequent reports and studies have also described QT prolongation with clarithromycin, azithromycin, as well as the ketolide, telithromycin.
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teTerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full
Page 5 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
The following provides a brief summary of some of the major adverse effects associated with these drugs. Detail about specific interactions is available by using the Lexi-Interact program included with UpToDate. Hepatotoxicity Azithromycin Postmarketing reports have identified various hepatic abnormalities in patients receiving azithromycin, including abnormal liver function tests, hepatitis, cholestatic jaundice, hepatic necrosis, and hepatic failure; some of these cases have resulted in death [34]. Azithromycin is therefore contraindicated in patients with a history of cholestatic jaundice or hepatic dysfunction associated with prior azithromycin use. It should be discontinued immediately if signs or symptoms of hepatitis occur. Telithromycin Severe hepatotoxicity reported in three patients receiving telithromycin prompted an FDA Public Health Advisory (www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm107824.htm) [35]. All three patients developed jaundice and abnormal liver function. One patient recovered, one required an organ transplant, and one died. Liver histology in the latter two patients showed massive tissue death. Although two patients reported some alcohol use, all three had been previously healthy and were not using other prescription drugs. There have been additional reports of hepatotoxicity, 42 of which were reviewed in detail and published [36]. The onset was short (median 10 days) and mortality was high. Clinicians are cautioned to monitor patients taking telithromycin for signs and symptoms of liver dysfunction and are advised to stop the medication in any patient who develops evidence of liver disease. Telithromycin should not be readministered to patients with a previous history of hepatitis and/or jaundice associated with the use of telithromycin or any macrolide antibiotic. Due to postmarketing reports of hepatotoxicity and other toxicities, the FDA rescinded its approval of telithromycin for bronchitis and sinusitis. It is still approved for the treatment of mild to moderate community-acquired pneumonia, but the FDA concluded that telithromycin should be a secondary alternative to other antimicrobial drugs. (See 'Warnings about telithromycin' above.) Other gastrointestinal Gastrointestinal side effects (nausea, diarrhea, abdominal pain) occur in 2 to 5 percent of patients with oral azithromycin and clarithromycin and about 12 percent with telithromycin [14,33]. Clarithromycin does not form the anhydrohemiketal degradation product thought to be responsible for some of the gastrointestinal side effects associated with erythromycin [19]. Macrolides have a dose-related effect on motilin receptors and can thereby stimulate the smooth muscle of the gastrointestinal tract. In fact, they have been used clinically to stimulate gastric motility [37]. The intravenous formulation of azithromycin also causes gastrointestinal side effects including: nausea (4 to 7 percent), vomiting (1.4 percent), diarrhea (4 to 9 percent), and abdominal pain (2 to 3 percent). The response to one drug does not necessarily predict that to the other. Some patients, for example, have intolerable side effects with clarithromycin but not azithromycin, and vice versa. Abdominal cramping with subsequent loose stools is common with high doses of azithromycin [4,19]. Dysgeusia seems to be a relatively frequent complaint in patients who are treated with clarithromycin, less so with telithromycin, and not with azithromycin. The clarithromycin pediatric suspension is bitter-tasting. QT interval prolongation Erythromycin was the first macrolide to be associated with QT interval prolongation, but subsequent reports and studies have also described QT interval prolongation with clarithromycin and azithromycin, as well as the ketolide, telithromycin. Clinicians should assess the risk of torsades de pointes when considering a macrolide and other antibiotic treatment options for patients at risk for cardiovascular events [38]. In addition to macrolides, certain non-macrolides, such as fluoroquinolones, also have the potential for prolonging the QT interval. (See "Fluoroquinolones", section on 'QT interval prolongation and arrhythmia' and "Acquired long QT syndrome", section on 'Incidence with specific drugs'.)
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teTerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full Page 6 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
In addition, each patient's medication list should be reviewed to determine if he or she is taking more than one drug that can prolong the QT interval (eg, methadone) since such patients are at increased risk of torsades de pointes (table 2). Information regarding the risk of QT prolongation with each macrolide and telithromycin is summarized as follows: Erythromycin Erythromycin is associated with an approximate two-fold increase in the risk of sudden cardiac death overall and a five-fold increase in patients also taking CYP3A4 inhibitors [39]. (See "Acquired long QT syndrome".) Azithromycin In 2013, the US Food and Drug Administration issued a warning about the risk of QT interval prolongation and potentially fatal torsades de pointes among patients taking azithromycin [38]. Patients at particular risk include those with existing QT interval prolongation, hypokalemia, hypomagnesemia, significant bradycardia, bradyarrhythmias, uncompensated heart failure, and those receiving certain antiarrhythmic drugs (eg, class IA [quinidine, procainamide] or class III [dofetilide, amiodarone, sotalol] antiarrhythmic drugs) [38,40,41]. Elderly patients may also be more susceptible to drug-associated QT interval prolongation. The warning was based on a review that followed the publication of a study that showed an increased risk of death in patients receiving azithromycin [42]. In a large database analysis of adults aged 30 to 74 years enrolled in Medicaid in Tennessee, patients receiving a five-day course of azithromycin had an increased risk of cardiovascular mortality (hazard ratio [HR] 2.88, 95% CI 1.79-4.63) and all-cause mortality (HR 1.85, 95% CI 1.25-2.75) compared with those who took no antibiotics [42]. Patients receiving azithromycin also had an increased risk of cardiovascular mortality (HR 2.49, 95% 1.38-4.50) and all-cause mortality (HR 2.02, 95% CI 1.24-3.30) compared with those receiving amoxicillin. In contrast, there was no increase in the risk of death in patients receiving amoxicillin or ciprofloxacin. The risk of cardiovascular mortality and all-cause mortality were similar for azithromycin and levofloxacin. The absolute increase in cardiovascular mortality was small; patients who received azithromycin had an estimated 47 additional cardiovascular deaths per million courses of therapy compared with amoxicillin [42]. The risk of cardiovascular mortality was highest among patients with elevated cardiovascular risk scores; compared with patients receiving amoxicillin, in patients receiving azithromycin, there were nine excess cardiovascular deaths per million five-day courses of antibiotics among those in the lowest cardiovascular risk category versus 245 excess cardiovascular deaths among those in the highest category. Among the 29 cardiovascular deaths that occurred during a five-day course of azithromycin, 22 were sudden cardiac deaths. Although the investigators used propensity analysis to adjust for baseline risk, residual confounding remains a concern since patients prescribed azithromycin may have had a higher risk of death because of their underlying disease and/or comorbidities. A large cohort study used Danish national healthcare data to evaluate the association between azithromycin use and cardiovascular death in adults between the ages of 18 and 64 [43]. The risk of death from cardiovascular causes was significantly increased with current use of azithromycin (defined as a five-day course) compared with no use of antibiotics (rate ratio [RR] 2.85, 95% CI 1.13-7.24). However, in a propensity adjusted analysis, current azithromycin use was not associated with an increased risk of death from cardiovascular causes compared with penicillin V (RR 0.93, 95% CI 0.56-1.55). These results suggest that the increased risk of cardiovascular death observed in patients receiving azithromycin compared with no antibiotic use was attributable to underlying patient factors that led to the prescription of antibiotics. Because there were few events, there was limited power to examine the risk of cardiovascular death in subgroups, including the subgroup of patients with known cardiovascular disease (RR 1.35, 95% CI 0.69-2.64) [43]. Of note, the population in this study was healthier than the Medicaid population evaluated in the database analysis described above [42,44]. The cardiovascular mortality rate in the Medicaid population was 85.2 deaths
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teTerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full
Page 7 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
per million courses of azithromycin compared with 15.4 deaths per million courses in the Danish population. This study suggests that azithromycin does not increase the risk of cardiovascular death in young and middle-aged members of the general population, at least those without preexisting cardiovascular disease. Clarithromycin Clarithromycin has also been associated with QT interval prolongation [45,46], and is metabolized by CYP3A4. Torsades de pointes has primarily been described when clarithromycin is given with other drugs that prolong the QT interval. A few case reports have described torsades de pointes with clarithromycin alone [47]. Telithromycin Telithromycin can also prolong the QT interval. The product labeling specifies that telithromycin should be avoided in patients with congenital long QT syndrome, ongoing proarrhythmic conditions, significant bradycardia, and those taking class 1A or III antiarrhythmic agents (eg, quinidine, procainamide, dofetilide). Other Severe reactions are rare but possible with all three macrolides. These include anaphylaxis, Stevens-Johnson syndrome, and pseudomembranous colitis [24,32]. A severe reaction to azithromycin may persist for several days due to its long half-life. Irreversible hearing loss has been reported with azithromycin, clarithromycin, and erythromycin [48,49]. Reversible hearing loss has also been reported following macrolide use, especially when they have been given at high doses [50-53]. Interstitial nephritis has been reported with erythromycin [54]. In addition, several other rare side effects have occurred with telithromycin, including fatal hepatotoxicity, fatal exacerbation of myasthenia gravis, loss of consciousness, and acute interstitial nephritis [33,55-58]. Visual disturbances (eg, blurry vision, diplopia, difficulty focusing) can also occur and may be related to telithromycin's effects on nicotinic acid receptors [59]. Telithromycin is contraindicated in patients with myasthenia gravis. (See 'Warnings about telithromycin' above.) DRUG INTERACTIONS The macrolides have a variety of drug interactions, many of which are mediated by inhibition of hepatic cytochrome CYP (P450) 3A enzymes [60]. In contrast to the other macrolides, azithromycin does not appear to affect hepatic enzymes significantly, leading to fewer documented drug interactions. However, several clinicallyimportant drug interactions have been reported with all of these agents. For example, fatalities have been reported in patients receiving clarithromycin and colchicine and there are now specific colchicine dose reduction recommendations published [61,62]. Detail about specific interactions is available by using the Lexi-Interact program included with UpToDate. Specific interactions between any two medications may be determined using the drug interaction tool (Lexi-Interact Online). This tool can be accessed from the UpToDate online search page or through the individual drug information topics, section on Drug interactions. SUMMARY Azithromycin (Zithromax) and clarithromycin (Biaxin) are macrolide antibiotics that are used in the treatment of community-acquired respiratory tract infections. They are derivatives of the older macrolide antibiotic, erythromycin. Telithromycin (Ketek) is the first member of the ketolide class of antimicrobials, which is related to the macrolide class. Concerns about postmarketing reports of hepatotoxicity and exacerbations of myasthenia gravis have led to significant restrictions on the use of telithromycin. (See 'Introduction' above and 'Warnings about telithromycin' above.) The mechanism of action of the newer macrolides is similar to that of erythromycin. They bind to the 50S subunit of bacterial ribosomes, leading to inhibition of transpeptidation, translocation, chain elongation and, ultimately, bacterial protein synthesis. (See 'Mechanism of action and chemical structure' above.) Structural changes have made the newer macrolides more acid-stable than erythromycin, providing improved oral absorption, tolerance, and pharmacokinetic properties. The newer macrolides also have a broader spectrum of antibacterial activity than erythromycin. (See 'Mechanism of action and chemical structure' above and 'Dosing and
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teTerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full Page 8 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
administration' above.) Two main mechanisms of acquired macrolide resistance have been described: Methylases encoded by the erm (erythromycin ribosome methylase) genes (ermA, ermB, ermC) alter the macrolide binding site on the bacterial ribosomal RNA, usually conferring a high degree of macrolide resistance as well as resistance to clindamycin. Active macrolide efflux pumps, encoded by the mef (macrolide efflux) msrA and msrB genes, confer a low to moderate degree of macrolide resistance These mechanisms are responsible for erythromycin-resistance in most gram-positive cocci (eg, Staphylococcus aureus, Streptococcus pneumoniae, Staphylococcus aureus, other streptococci). In contrast to the mechanisms of acquired resistance, intrinsic resistance exhibited by Enterobacteriaceae, Pseudomonas spp, and Acinetobacter spp is due to decreased permeability of the outer cell envelope. (See 'Resistance' above.) Azithromycin and clarithromycin have a broader spectrum of activity than erythromycin, and include activity against respiratory tract pathogens such as Streptococcus pneumoniae, Haemophilus spp, Moraxella catarrhalis, and atypical pneumonia pathogens, as well as against various other gram-negative bacteria and Mycobacterium avium complex. (See 'Spectrum of activity' above.) Because of its more frequent gastrointestinal side effects and the earlier appreciation of the risk of QT prolongation and sudden death, erythromycin is rarely recommended. However, subsequent reports and studies have also described QT prolongation with clarithromycin, azithromycin, as well as the ketolide, telithromycin. Postmarketing reports have also identified various hepatic abnormalities in patients receiving azithromycin, including cases that have resulted in death. (See 'Adverse reactions' above.) The macrolides have a variety of drug interactions, many of which are mediated by inhibition of hepatic cytochrome CYP (P450) 3A enzymes. In contrast to the other macrolides, azithromycin does not appear to affect hepatic enzymes significantly, leading to fewer documented drug interactions. (See 'Drug interactions' above.)
Use of UpToDate is subject to the Subscription and License Agreement. REFERENCES 1. Sturgill MG, Rapp RP. Clarithromycin: review of a new macrolide antibiotic with improved microbiologic spectrum and favorable pharmacokinetic and adverse effect profiles. Ann Pharmacother 1992; 26:1099. 2. Rapp RP, McCraney SA, Goodman NL, Shaddick DJ. New macrolide antibiotics: usefulness in infections caused by mycobacteria other than Mycobacterium tuberculosis. Ann Pharmacother 1994; 28:1255. 3. Neu HC. New macrolide antibiotics: azithromycin and clarithromycin. Ann Intern Med 1992; 116:517. 4. Ballow CH, Amsden GW. Azithromycin: the first azalide antibiotic. Ann Pharmacother 1992; 26:1253. 5. Malhotra-Kumar S, Lammens C, Coenen S, et al. Effect of azithromycin and clarithromycin therapy on pharyngeal carriage of macrolide-resistant streptococci in healthy volunteers: a randomised, double-blind, placebo-controlled study. Lancet 2007; 369:482. 6. Leclercq R. Mechanisms of resistance to macrolides and lincosamides: nature of the resistance elements and their clinical implications. Clin Infect Dis 2002; 34:482. 7. Corso A, Severina EP, Petruk VF, et al. Molecular characterization of penicillin-resistant Streptococcus pneumoniae isolates causing respiratory disease in the United States. Microb Drug Resist 1998; 4:325. 8. Shortridge VD, Doern GV, Brueggemann AB, et al. Prevalence of macrolide resistance mechanisms in Streptococcus pneumoniae isolates from a multicenter antibiotic resistance surveillance study conducted in the United States in 1994-1995. Clin Infect Dis 1999; 29:1186. 9. Cetin ES, Gunes H, Kaya S, et al. Distribution of genes encoding resistance to macrolides, lincosamides and
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teTerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full Page 9 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
streptogramins among clinical staphylococcal isolates in a Turkish university hospital. J Microbiol Immunol Infect 2010; 43:524. 10. Aktas Z, Aridogan A, Kayacan CB, Aydin D. Resistance to macrolide, lincosamide and streptogramin antibiotics in staphylococci isolated in Istanbul, Turkey. J Microbiol 2007; 45:286. 11. Lina G, Quaglia A, Reverdy ME, et al. Distribution of genes encoding resistance to macrolides, lincosamides, and streptogramins among staphylococci. Antimicrob Agents Chemother 1999; 43:1062. 12. Chollet R, Chevalier J, Bryskier A, Pags JM. The AcrAB-TolC pump is involved in macrolide resistance but not in telithromycin efflux in Enterobacter aerogenes and Escherichia coli. Antimicrob Agents Chemother 2004; 48:3621. 13. Goldstein F, Vidal B, Kitzis MD. Telithromycin-resistant Streptococcus pneumoniae. Emerg Infect Dis 2005; 11:1489. 14. Zuckerman JM. Macrolides and ketolides: azithromycin, clarithromycin, telithromycin. Infect Dis Clin North Am 2004; 18:621. 15. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007; 44 Suppl 2:S27. 16. O'Doherty B, Muller O. Randomized, multicentre study of the efficacy and tolerance of azithromycin versus clarithromycin in the treatment of adults with mild to moderate community-acquired pneumonia. Azithromycin Study Group. Eur J Clin Microbiol Infect Dis 1998; 17:828. 17. File TM. Telithromycin new product overview. J Allergy Clin Immunol 2005; 115:S1. 18. Bahal N, Nahata MC. The new macrolide antibiotics: azithromycin, clarithromycin, dirithromycin, and roxithromycin. Ann Pharmacother 1992; 26:46. 19. Piscitelli SC, Danziger LH, Rodvold KA. Clarithromycin and azithromycin: new macrolide antibiotics. Clin Pharm 1992; 11:137. 20. Azithromycin extended-release (Zmax) for sinusitis and pneumonia. Med Lett Drugs Ther 2005; 47:78. 21. Sivapalasingam S, Steigbigel NH. Macrolides, clindamycin, and ketolides. In: Principles and Practice of Infectious Diseases, 6th ed, Mandell GL, Bennett JE, Dolin R (Eds), Churchill Livingstone, Philadelphia 2005. p.396. 22. Namour F, Wessels DH, Pascual MH, et al. Pharmacokinetics of the new ketolide telithromycin (HMR 3647) administered in ascending single and multiple doses. Antimicrob Agents Chemother 2001; 45:170. 23. Wellington K, Noble S. Telithromycin. Drugs 2004; 64:1683. 24. Product Information for Zithromax, Biaxin, Physicians' Desk Reference, 1995. 25. Brater, DC. Pocket Manual of Drug Use in Clinical Medicine, 6th ed, Improved Therapeutics, Indianapolis 1994. 26. Ross DB. The FDA and the case of Ketek. N Engl J Med 2007; 356:1601. 27. Soreth J, Cox E, Kweder S, et al. Ketek--the FDA perspective. N Engl J Med 2007; 356:1675. 28. Briggs GG, Freeman RK, Yaffe SJ. A Reference Guide to Fetal and Neonatal Risk: Drugs in Pregnancy and Lactation, 4th ed, Williams & Wilkins, Baltimore 1994. p.335. 29. Bush MR, Rosa C. Azithromycin and erythromycin in the treatment of cervical chlamydial infection during pregnancy. Obstet Gynecol 1994; 84:61. 30. Adair CD, Gunter M, Stovall TG, et al. Chlamydia in pregnancy: a randomized trial of azithromycin and erythromycin. Obstet Gynecol 1998; 91:165. 31. Sarkar M, Woodland C, Koren G, Einarson AR. Pregnancy outcome following gestational exposure to azithromycin. BMC Pregnancy Childbirth 2006; 6:18. 32. Product Information for clarithromycin tablets. Abbott Laboratories, revised January, 1997. 33. Aventis Pharmaceuticals. Ketek product labeling. 2005. 34. Zithromax (azithromycin) tablet, single-dose packet, IV for injection, and oral suspension. Safety labeling changes approved by FDA Center for Drug Evaluation and Research (CDER) http://www.fda.gov/Safety/MedWatch/SafetyInformation/ucm225814.htm (Accessed on March 21, 2011). 35. Clay KD, Hanson JS, Pope SD, et al. Brief communication: severe hepatotoxicity of telithromycin: three case reports and literature review. Ann Intern Med 2006; 144:415. 36. Brinker AD, Wassel RT, Lyndly J, et al. Telithromycin-associated hepatotoxicity: Clinical spectrum and causality
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full Page 10 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
assessment of 42 cases. Hepatology 2009; 49:250. 37. Camilleri M. Clinical practice. Diabetic gastroparesis. N Engl J Med 2007; 356:820. 38. US Food and Drug Administration. Azithromycin (Zithromax or Zmax): Drug safety communication - risk of potentially fatal heart rhythms. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm343350.htm? source=govdelivery (Accessed on March 15, 2013). 39. Ray WA, Murray KT, Meredith S, et al. Oral erythromycin and the risk of sudden death from cardiac causes. N Engl J Med 2004; 351:1089. 40. US Food and Drug Administration. Zmax (azithromycin extended release) for oral suspension. Safety labeling changes approved by FDA Center for Drug Evaluation and Research (CDER). http://www.fda.gov/Safety/MedWatch/SafetyInformation/ucm262866.htm (Accessed on May 18, 2012). 41. ZITHROMAX (azithromycin tablets) and(azithromycin for oral suspension) - prescribing information. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/050710s039,050711s036,050784s023lbl.pdf (Accessed on March 15, 2013). 42. Ray WA, Murray KT, Hall K, et al. Azithromycin and the risk of cardiovascular death. N Engl J Med 2012; 366:1881. 43. Svanstrm H, Pasternak B, Hviid A. Use of azithromycin and death from cardiovascular causes. N Engl J Med 2013; 368:1704. 44. Mosholder AD, Mathew J, Alexander JJ, et al. Cardiovascular risks with azithromycin and other antibacterial drugs. N Engl J Med 2013; 368:1665. 45. Milberg P, Eckardt L, Bruns HJ, et al. Divergent proarrhythmic potential of macrolide antibiotics despite similar QT prolongation: fast phase 3 repolarization prevents early afterdepolarizations and torsade de pointes. J Pharmacol Exp Ther 2002; 303:218. 46. Volberg WA, Koci BJ, Su W, et al. Blockade of human cardiac potassium channel human ether-a-go-go-related gene (HERG) by macrolide antibiotics. J Pharmacol Exp Ther 2002; 302:320. 47. Kamochi H, Nii T, Eguchi K, et al. Clarithromycin associated with torsades de pointes. Jpn Circ J 1999; 63:421. 48. Ress BD, Gross EM. Irreversible sensorineural hearing loss as a result of azithromycin ototoxicity. A case report. Ann Otol Rhinol Laryngol 2000; 109:435. 49. Coulston J, Balaratnam N. Irreversible sensorineural hearing loss due to clarithromycin. Postgrad Med J 2005; 81:58. 50. Swanson DJ, Sung RJ, Fine MJ, et al. Erythromycin ototoxicity: prospective assessment with serum concentrations and audiograms in a study of patients with pneumonia. Am J Med 1992; 92:61. 51. Vasquez EM, Maddux MS, Sanchez J, Pollak R. Clinically significant hearing loss in renal allograft recipients treated with intravenous erythromycin. Arch Intern Med 1993; 153:879. 52. Bizjak ED, Haug MT 3rd, Schilz RJ, et al. Intravenous azithromycin-induced ototoxicity. Pharmacotherapy 1999; 19:245. 53. Hajiioannou JK, Florou V, Kousoulis P, et al. Clarithromycin induced reversible sensorineural hearing loss. B-ENT 2011; 7:127. 54. EES (erythromycin ethylsuccinate) granules for oral suspension and Ery-Ped (erythromycin ethylsuccinate) liquids. Safety labeling changes approved by FDA Center for Drug Evaluation and Research (CDER) January 2011 http://www.fda.gov/Safety/MedWatch/SafetyInformation/ucm243753.htm (Accessed on March 21, 2011). 55. Telithromycin (Ketek) for respiratory infections. Med Lett Drugs Ther 2004; 46:66. 56. Perrot X, Bernard N, Vial C, et al. Myasthenia gravis exacerbation or unmasking associated with telithromycin treatment. Neurology 2006; 67:2256. 57. Jennett AM, Bali D, Jasti P, et al. Telithromycin and myasthenic crisis. Clin Infect Dis 2006; 43:1621. 58. Tintillier M, Kirch L, Almpanis C, et al. Telithromycin-induced acute interstitial nephritis: a first case report. Am J Kidney Dis 2004; 44:e25. 59. Bertrand D. Importance of nicotinic acetylcholine receptors in the visual adverse effects associated with telithromycin. Biochem Pcol 2009; 78:922. 60. Thomason AR, Waldrop BA, Price SO. Nortriptyline cardiac toxicity from a probable interaction with telithromycin.
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full Page 11 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
Hosp Pharm 2009; 44:397. 61. Hung IF, Wu AK, Cheng VC, et al. Fatal interaction between clarithromycin and colchicine in patients with renal insufficiency: a retrospective study. Clin Infect Dis 2005; 41:291. 62. Colcrys. http://www.colcrys.com/ (Accessed on May 24, 2012). Topic 474 Version 13.0
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full
Page 12 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
GRAPHICS
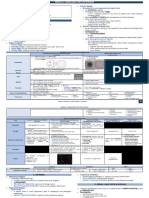
Drug ratings in pregnancy (US Food & Drug Administration)
Category
A
Interpretation
Controlled human studies show no risk Controlled studies in pregnant women fail to demonstrate a risk to the fetus in the first trimester with no evidence of risk in later trimesters. The possibility of fetal harm appears remote.
No evidence of risk in studies Either animal-reproduction studies have not demonstrated a fetal risk but there are no controlled studies in pregnant women, or animal-reproduction studies have shown an adverse effect (other than a decrease in fertility) that was not confirmed in controlled studies in women in the first trimester and there is no evidence of a risk in later trimesters.
Risk cannot be ruled out Either studies in animals have revealed adverse effects on the fetus (teratogenic or embryocidal effects or other) and there are no controlled studies in women, or studies in women and animals are not available. Drugs should be given only if the potential benefits justify the potential risk to the fetus.
Positive evidence of risk There is positive evidence of human fetal risk, but the benefits from use in pregnant women may be acceptable despite the risk (eg, if the drug is needed in a lifethreatening situation or for a serious disease for which safer drugs cannot be used or are ineffective).
Contraindicated in pregnancy Studies in animals or human beings have demonstrated fetal abnormalities or there is evidence of fetal risk based on human experience, or both, and the risk of the use of the drug in pregnant women clearly outweighs any possible benefit. The drug is contraindicated in women who are or may become pregnant.
Reproduced with permission from: Lexicomp Online. Copyright 1978-2013 Lexicomp, Inc. All Rights Reserved.
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full
Page 13 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
Some reported causes and potentiators of the long QT syndrome*
Congenital
Jervell and Lange-Nielsen syndrome (including "channelopathies") Romano-Ward syndrome Idiopathic
Acquired (continued)
Antihistamines Terfenadine Astemizole Psychotropic drugs Thioridazine Phenothiazines Tricyclic or tetracyclic antidepressants Haloperidol and other butyrophenones Antineoplastic agents Crizotinib, dasatinib, eribulin, nilotinib, romidepsin, sorafenib, sunitinib, vandetanib, vemurafenib, vorinostat Other drugs Selective serotonin reuptake inhibitors Risperidone Opioids (methadone, oxycodone) Vasodilators - prenylamine, bepridil, mibefradil Diuretics - via electrolyte changes (esp. hypokalemia or hypomagnesemia) 5HT3-antagonists - ondansetron, granisetron, and dolasetron Motility drugs - cisapride, domperidone Droperidol - may be safe at the low doses used by anesthesiologists (0.625 to 1.25 mg) Ranolazine HIV protease inhibitors Miscellaneous - organophosphate insecticides, probucol, cocaine, terodiline, papaverine, certain Chinese herbs, chloral hydrate, arsenic trioxide, cesium chloride, levomethadyl Other factors Myocardial ischemia or infarction, esp. with prominent T wave inversions Intracranial disease
Acquired
Metabolic disorders Hypokalemia Hypomagnesemia Hypocalcemia Starvation Anorexia nervosa Liquid protein diets Hypothyroidism Bradyarrhythmias Sinus node dysfunction AV block - second or third degree Antiarrhythmic drugs Quinidine Procainamide or N-acetylprocainamide Disopyramide Amiodarone and dronedarone Sotalol Dofetilide, ibutilide, azimilide, sematilide Antimicrobial drugs Erythromycin, clarithromycin, telithromycin, azithromycin Pentamidine Some azole antifungals - voriconazole, posaconazole Some fluoroquinolones (eg, sparfloxacin, gatifloxacin, levofloxacin, moxifloxacin) Other - spiramycin, chloroquine, halofantrine mefloquine
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full
Page 14 of 15
Azithromycin, clarithromycin, and telithromycin
19/08/13 20:27
HIV infection Hypothermia Connective tissue diseases with anti-Ro/SSA antibodies * The long and growing list of medications and other factors capable of prolonging the QT(U) represents an evolving area of clinical research. In some cases of long QT-U two or more factors may be involved. Additional clinical information is provided at the Arizona Center for Education and Research on Therapeutics (CERT) website: http://www.azcert.org/medical-pros/drug-lists/drug-lists.cfm.
http://www.uptodate.com/contents/azithromycin-clarithromycin-and-teerm=macrolides&selectedTitle=1%7E150&view=print&displayedView=full
Page 15 of 15
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Chapter 8 NematodesDocument5 pagesChapter 8 NematodesJuju GalangNo ratings yet
- Nutrition Exam - CanadaDocument93 pagesNutrition Exam - Canadamarco100% (2)
- Zoonoses - Definition, History, Classification, ManagementDocument58 pagesZoonoses - Definition, History, Classification, ManagementJeevan KumarNo ratings yet
- Biology Quarter 1 Unit 2 Day 6 Immune System ArticleDocument4 pagesBiology Quarter 1 Unit 2 Day 6 Immune System ArticleTeachTappyNo ratings yet
- DR L M KhanDocument9 pagesDR L M KhanHomoeopath Aamir Saleem100% (4)
- 05 N318 30162Document21 pages05 N318 30162Dani PhilipNo ratings yet
- Case of ENDocument73 pagesCase of ENHarold Nathan TanNo ratings yet
- Blood Administration and Transfusion Reactions QuizDocument5 pagesBlood Administration and Transfusion Reactions Quizremooheshmat100% (1)
- Kode Diagnosa P-Care - SimpusDocument2 pagesKode Diagnosa P-Care - SimpusiqbalNo ratings yet
- Neonatal PneumoniaDocument11 pagesNeonatal PneumoniaKristine Joy Cadiz AgostoNo ratings yet
- ChromID CPS Brochure Final-1Document2 pagesChromID CPS Brochure Final-1horia96No ratings yet
- Infections and ImmunityDocument35 pagesInfections and ImmunityDr. Ashish JawarkarNo ratings yet
- Lab Report For Micro 210 AJH1Document11 pagesLab Report For Micro 210 AJH1ahathaw17No ratings yet
- The Client With Urinary Tract InfectionDocument4 pagesThe Client With Urinary Tract InfectionMarisol Jane JomayaNo ratings yet
- Dengue Fever: Centre For Health Protection, Department of Health July 2019Document17 pagesDengue Fever: Centre For Health Protection, Department of Health July 2019Melissa Marie CustodioNo ratings yet
- Fungi, Viruses and ParasitesDocument31 pagesFungi, Viruses and ParasitesIraqiNo ratings yet
- Hydronephrosis LWDocument8 pagesHydronephrosis LWvitauxianaNo ratings yet
- Chapter 14: Normal Human Microbiota: A Delicate Balance of PowerDocument94 pagesChapter 14: Normal Human Microbiota: A Delicate Balance of PowerAqsa MuzammilNo ratings yet
- Self LigationDocument2 pagesSelf Ligationdavidrocks81No ratings yet
- Intestinal Helminthes Among Children in Orphanages in Some Parts of Kaduna State, NigeriaDocument6 pagesIntestinal Helminthes Among Children in Orphanages in Some Parts of Kaduna State, Nigeriawilolud2059No ratings yet
- Karsinoma Serviks & Vagina SlideshowDocument21 pagesKarsinoma Serviks & Vagina SlideshowFardzli MatjakirNo ratings yet
- ImmunoSeroLab M4Document3 pagesImmunoSeroLab M4ela kikayNo ratings yet
- Burton's Microbiology For The Health Sciences Section V. Environmental and Applied MicrobiologyDocument32 pagesBurton's Microbiology For The Health Sciences Section V. Environmental and Applied MicrobiologyMitzi Audrey100% (1)
- Reporting Draft For PPT InputsDocument2 pagesReporting Draft For PPT InputsPhaestus ReverseNo ratings yet
- A& P II Assignment 2Document5 pagesA& P II Assignment 2hepnandeNo ratings yet
- 1º Atividade para Os 4º Anos - GABARITODocument3 pages1º Atividade para Os 4º Anos - GABARITOChrisNo ratings yet
- Enamel: Click To Edit Master Subtitle StyleDocument106 pagesEnamel: Click To Edit Master Subtitle StyleManva MonishNo ratings yet
- Asexual Rep and Sex RepDocument35 pagesAsexual Rep and Sex RepJen NyNo ratings yet
- Biology Practical Part 2Document23 pagesBiology Practical Part 2jiya singh100% (2)
- Fevers: Usually A Positive Sign That The Body Is Fighting Infection."Document3 pagesFevers: Usually A Positive Sign That The Body Is Fighting Infection."Theresa OsmerNo ratings yet