Professional Documents
Culture Documents
Deep Breath Exercise PDF
Uploaded by
Aroef PoenyaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Deep Breath Exercise PDF
Uploaded by
Aroef PoenyaCopyright:
Available Formats
ORIGINAL ARTICLE
Regular slow-breathing exercise effects
on blood pressure and breathing
patterns at rest
DE Anderson, JD McNeely and BG Windham
Clinical Research Branch, Intramural Research Program, National Institute on Aging, National Institutes
of Health, Baltimore, MD, USA
Previous studies reported that a device-guided slow-
breathing (DGB) exercise decreases resting blood
pressure (BP) in hypertensive patients. This study
investigated the effects of daily practice of DGB on (a)
24-h BP and breathing patterns in the natural environ-
ment, as well as (b) BP and breathing pattern during
clinic rest. Altogether, 40 participants with pre-hyperten-
sion or stage 1 hypertension were trained to decrease
breathing rate through DGB or to passively attend
to breathing (control, CTL) during daily 15-min sessions.
The participants practiced their breathing exercise at
home for 4 weeks. The DGB (but not the CTL) interven-
tion decreased clinic resting BP, mid-day ambulatory
systolic BP (in women only) and resting breathing
rate, and increased resting tidal volume. However, 24-h
BP level was not changed by DGB or CTL interventions,
nor was overnight breathing pattern. These findings
are consistent with the conclusion that a short-term,
autonomic mechanism mediated the observed changes
in resting BP, but provided no evidence that regular
DGB affected factors involved in long-term BP regu-
lation. Additional research will be needed to determine
whether 24-h BP can be lowered by a more prolonged
intervention.
Journal of Human Hypertension advance online publication,
4 March 2010; doi:10.1038/jhh.2010.18
Keywords: BP; breathing; tidal volume
Introduction
Several previous studies have reported that
regular practice of device-guided breathing (DGB)
decreases resting blood pressure (BP) of hyper-
tensive patients.
18
However, only three of the
studies reported to date involved randomized
clinical trials. Two of those did not measure BP in
the natural environment,
3,8
and the third was unable
to confirm greater effects than in a control group.
7
Whether the effects of DGB observed in the clinic
setting extend to the natural environment is an
important issue that needs to be investigated in a
randomized clinical trial with 24-h BP monitoring
preceding and following the DGB intervention.
A study with 24-h BP monitoring would also be
relevant to the mechanism by which the enduring
BP changes are generated. Performance of DGB
itself is accompanied by increased cardiopulmonary
stretch receptor stimulation that reduces sympathetic
efferent fibre discharge, resulting in peripheral
vasodilation.
9
Thus, acute decreases in BP during
DGB are mediated, at least in part, by decreases
in sympathetic and increases in parasympathetic
nervous system activity.
10
Long-term changes in BP
are mediated, however, not by changes in autonomic
nervous system activity, but by factors that change
the set point for BP.
11
Renal sodium regulation is sensitive to changes in
breathing pattern that alter blood gas concentrations.
Previous studies of DGB have found not only that tidal
volume increases as breathing rate falls, but also that
end tidal CO
2
(PetCO
2
) decreases, apparently because of
improved gas transfer associated with deeper breath-
ing.
12
To date, however, no studies have examined
possible changes in resting breathing rate, tidal volume,
minute ventilation or PetCO
2
in response to regular
practice of DGB. If PetCO
2
chronically decreased in
response to regular DGB, long-term effects on BP could
involve alterations in blood gases and acidbase
balance that alter total body sodium levels.
The effectiveness of DGB depends on the fre-
quency of practice. For example, Elliott et al.
6
found
that a 180-min practice of DGB over an 8-week
interval was a threshold for the occurrence of
significant decreases in systolic BP. Although pre-
vious interventions were each of 8 weeks duration,
several found that BP decreased during the first 34
weeks before levelling off.
35
Received 11 June 2009; revised 11 September 2009; accepted 5
November 2009
Correspondence: Dr DE Anderson, Osher Center for Integrative
Medicine, Campus Box 1726, University of California at San
Francisco, San Francisco, CA 94143-1726, USA.
E-mail: Andersod@mail.nih.gov
Journal of Human Hypertension (2010), 17
& 2010 Macmillan Publishers Limited All rights reserved 0950-9240/10 $32.00
www.nature.com/jhh
This study was designed to determine whether a
daily, 4-week DGB intervention decreased resting
and 24-h BP in a series of subjects with pre-
hypertension or stage 1 hypertension. This study
also investigated whether the effects of DGB on BP
are accompanied by concurrent changes in breath-
ing patterns at rest. The effects of DGB on BP and
breathing patterns were compared with those ob-
served in a randomized control group who attended
to the breathing rhythm without attempting to
control its rate.
Materials and methods
Participants
In total, 102 men and women from the surrounding
community responded to local advertising for a
clinical trial (Clinicaltrial.gov ID # NCT00328016),
and were screened over the telephone. In all, 72
respondents were invited to the National Institute
on Aging Clinical Research Unit, where the purpose
of the study was explained, and informed consent
was obtained. A physical examination was perfor-
med, and blood and urine samples were collected to
ensure that the participants were free of respiratory,
cardiovascular and renal diseases. Additional ex-
clusion criteria were diabetes or the use of tobacco,
steroids, hormone-replacement therapy, angiotensin
II receptor blockers, angiotensin-converting enzyme
inhibitors, b-blockers or any other medications that
would interfere with central nervous system activ-
ity. The protocol was approved by the Institutional
Review Board of the Medstar Research Institute.
Subjects with pre-hypertension or mild hyperten-
sion were studied to eliminate the complicating
effects of antihypertensive medication. A total of 30
subjects were eliminated who reported hypertensive
BP over the telephone, but were found to have BP
below criterion levels in the clinic. Two subjects
who completed the study were removed from the
data analysis because of noncompliance with inter-
vention instructions (one in each group). The
remaining 40 participants were assigned to either
DGB or control (CTL) group using an open randomi-
zation procedure, and introduced to their respective
breathing exercise. Table 1 shows the effectiveness
of this randomization procedure in terms of the
nonsignificance of differences between groups in
the various pre-study measures.
Experimental design, randomization and interventions
This design had three basic phases: a period of pre-
intervention monitoring, a 4-week intervention
period for each of the two groups (DGB and CTL),
and a period of post-intervention monitoring. Two
screening sessions were scheduled to determine
eligibility and establish pre-intervention baseline
data, after which qualifying participants were
randomized to their intervention condition. Each
group practiced their respective breathing exercise
daily throughout the 4-week intervention phase,
after which they returned to the clinic for post-
intervention monitoring.
During the pre-intervention monitoring period,
each participant visited the clinic on two occasions
within a 1-week interval during which breathing
pattern and PetCO
2
were monitored continuously,
and BP was measured every 6 min for 25min, as
described below. Candidates were declared eligible
for participation if mean systolic BP of the 10
measurements during the two sessions was 4130
and o160mmHg and mean diastolic BP o100mmHg.
Between the two pre-intervention sessions, BP was
recorded for 24 h in the natural environment, and
breathing pattern was recorded continuously during
overnight sleep.
Eligible participants were randomized to the DGB
or CTL condition. The DGB condition involved the
use of a commercially available device (RES-
PeRATE, Lod, Israel) that guides breathing by
auditory stimulation.
12
The device includes a micro-
computer that is connected to a band worn around
the torso and a set of earphones. The band senses
individual breathing rhythm, and calculates an
initial rate to which the subject entrains breathing
cycle in accord with a series of ascending and
descending tones presented over the earphones.
Over time, the duration of each tone increases, and
breathing rate is systematically slowed, usually o10
breaths per min, and often as low as p6 breaths per
min. Each participant was encouraged to breathe as
comfortably and effortlessly as possible, while keeping
the lungs moving in accord with the tones. The device
contains software that enabled subsequent assessment
of adherence and quantification of performance.
The control (CTL) group performed a meditative
relaxation exercise.
13
Participants were instructed to
sit comfortably with eyes closed and legs and arms
uncrossed, and to observe their natural breathing
rhythm for 15min, without consciously controlling it.
Table 1 Means and s.e. of demographic and clinical character-
istics during seated rest at screening visit for participants in the
device-guided breathing (DGB) and control groups
Characteristic DGB
(n20)
Control
(n20)
P-value
Age (year) 53.42.8 52.92.8 0.900
Males/females 12/8 9/11
Body weight (kg) 82.79
4.4 83.3
2.8 0.939
BMI (kg m
2
) 27.9
1.3 29.4
1.2 0.402
Heart rate (b.p.m.) 68.1
2.3 66.3
2.8 0.622
Breathing rate (b.p.m.) 14.10.8 13.61.0 0.698
Tidal volume (ml) 46234 41944 0.444
Minute ventilation (l min
1
) 6.20.4 5.20.4 0.085
End tidal CO
2
(mmHg) 39.3
1.0 37.5
0.7 0.148
Systolic BP (mmHg) 141.8
2.4 140.1
2.1 0.597
Diastolic BP (mmHg) 88.2
1.6 85.2
1.8 0.221
Abbreviations: BP, blood pressure; BMI, body mass index; b.p.m.,
breaths per min.
Blood pressure effects of guided slow breathing
DE Anderson et al
2
Journal of Human Hypertension
They were instructed to silently repeat the word
one during each exhalation interval. Daily perfor-
mance at home was documented in a diary. All
participants were called at home weekly to record
adherence data.
Participants were instructed to practice their
breathing exercise daily throughout the 4-week
intervention phase. Both groups reported excellent
adherence to the task instructions. Data recorded in
the device showed that DGB was practiced for
27.90.3 of the 28 days, during which mean
breathing rate was o10 per min for 11.5
1.0 of
the 15 min. The DGB group synchronized their
breathing with the tones 81.915.3% of the time.
The CTL group reported practicing on 27.90.3 of
the 28 days for an average of 17.52
0.8 min per day.
During the post-intervention period, each partici-
pant returned to the clinic for a single session of
25 min of monitoring of breathing pattern, PetCO
2
,
and BP, as during the pre-intervention period. In
addition, BP was monitored for 24 h, and overnight
breathing pattern was recorded.
BP monitoring
BP was recorded in the clinic and in the natural
environment using an inflatable arm cuff attached to
an oscillometric device (Spacelabs, Redmond, WA,
USA). During screening sessions, BP was recorded
every 6min for a total of five measurements
per session. During 24-h monitoring in the natural
environment, BP was recorded every 30 min for
16-h (daytime), and every 60 min for 8-h (nighttime).
The BP recorder was regularly calibrated in the
laboratory using sphygmomanometer.
Breathing pattern and end tidal CO
2
(PetCO
2
)
Breathing rate, tidal volume and minute ventilation
were recorded from an elasticized vest that summed
chest and abdominal expansion on a breath-to-
breath basis through inductive plethysmography
(Lifeshirt, Vivometrics, Ventura, CA, USA).
14
The
vest was used for both clinic sessions and for
overnight recording at home. Tidal volume was
calibrated before each monitoring session by exhal-
ing a fixed volume of air into an inflatable bag. Data
from the recorder were downloaded onto a desktop
computer (Dell Computer, Round Rock, TX, USA).
PetCO
2
was monitored continuously during clinic
sessions using a nasal cannula connected to a
respiratory gas monitor (Datex-Ohmeda, Fairfield,
CT, USA). Data were recorded over successive 10-s
intervals on a desktop computer (Dell Computer).
Data analysis
Independent two-tailed t-tests were used to deter-
mine whether there were any differences in biometric
and physiological measurements between the two
groups at baseline. The significance of the mean
differences between screening sessions, the pre-
intervention and post-intervention sessions was
analysed for each clinic resting cardiovascular and
respiratory measure through repeated measures two-
way analysis of variance using Bonferroni multiple
comparison tests. The significance of the differences
between the pre-intervention and post-intervention
measures of 24-h BP, night time BP (midnight
0800h), ambulatory daytime BP (08001600h), and
evening breathing measures (1600hmidnight) for all
participants, for men and women, were also deter-
mined by repeated measures two-way analysis of
variance using Bonferroni multiple comparison tests.
Results
Intervention effects on clinic resting BP
Figure 1 shows means and s.d. of resting clinic
systolic BP during the two screening sessions
(weeks 1 and 2) and the post-intervention session
(week 6). Significant effects for time (F
2,38
6.37;
Po0.002) and a significant interaction between
group and time were observed, indicating a signi-
ficantly greater decrease in systolic BP following the
intervention for DGB than in the CTL group
(F
1,38
3.72; Po0.029). The systolic BP of the DGB
group was significantly lower after the intervention
compared with both pre-intervention levels, which
were not significantly different from each other.
Figure 1 also shows means and s.e. of resting
clinic diastolic BP during the two screening sessions
Figure 1 Means and s.e. of systolic and diastolic BP for DGB and
control (CTL) groups during two screening, pre-intervention
sessions (weeks 1 and 2) and after 4 weeks of the intervention
(week 6).
Blood pressure effects of guided slow breathing
DE Anderson et al
3
Journal of Human Hypertension
and the post-intervention session. A significant
effect for time (F
2,38
9.85; Po0.002), but no
interaction between time and group (F
1,38
0.22;
Po0.803) was observed. Multiple comparison tests
showed that resting diastolic BP of the DGB (but not
CTL) group was significantly lower after the inter-
vention than during both pre-interventions session.
Intervention effects on clinic respiratory measures
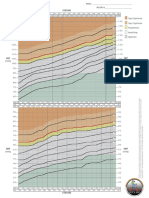
Figure 2 shows means and s.e. of resting clinic
breathing rate during the two screening sessions
(weeks 1 and 2) and the post-intervention session
(week 6). A significant interaction between time and
group was observed (F
1,38
16.24; Po0.001), indi-
cating that breathing rate of the DGB group
decreased more than in the CTL group. Breathing
rate of the DGB group was significantly lower after
the intervention than during both pre-intervention
sessions.
Figure 2 also shows means and s.e. of resting
clinic tidal volume during the two screening
sessions and the post-intervention session. Signifi-
cant effects of time (F
2,38
6.73; Po0.002), and a
significant interaction between time and group
(F
1,38
7.83; Po0.001) were observed, indicating
that tidal volume of the DGB group increased more
than in the CTL group. Tidal volume of the DGB
group was significantly larger after the intervention
than during both pre-intervention sessions.
Figure 2 also shows means and s.e. of resting
clinic minute ventilation during the two screening
sessions and the post-intervention session. No
significant effect of time (F
2,38
3.07; Po0.052), or
interaction between time and group (F
1,38
0.02;
Po0.976) were observed, indicating no difference
between DGB and CTL groups in change in minute
ventilation.
Figure 2 also shows means and s.e. of resting
clinic PetCO
2
during the two screening sessions and
the post-intervention session. A significant effect of
time (F
2,38
5.31; Po0.007), but no significant inter-
action between time and group (F
1,38
1.97;
Po0.146) was observed, indicating no differences
between groups in change in PetCO
2
. Multiple
comparison tests showed that PetCO
2
of the DGB
(but not CTL) group was significantly lower follow-
ing the intervention than during the first pre-
intervention session.
Intervention effects on 24 h, overnight, daytime
and evening BP
Table 2 shows means and standard errors of 24h,
daytime and night time systolic and diastolic BP of
the DGB and CTL groups before and after the
intervention. No significant differences between
groups, over time, or in the interaction of group
and time were observed for 24-h systolic
(F
1,38
0.12; Po0.73) or diastolic (F
1,38
0.55;
Po0.46) BP.
Figure 3 shows the diurnal variation in hourly
mean systolic BP preceding and following the DGB
and CTL interventions, plotted separately for wo-
men and for men. Figure 3 and Table 3 show that for
women in the DGB group, the post-intervention
daytime systolic (t 6.11; Po0.001) and diastolic
(t 3.47; Po0.05) BP mean were significantly lower
than the pre-intervention daytime levels. Table 3
also shows that no significant pre- to post-interven-
tion differences were observed for overnight or
evening systolic BP for women, or overnight, day-
Figure 2 Means and s.e. of breathing rate, tidal volume, minute ventilation and end tidal CO
2
for DGB and control (CTL) groups during
two screening, pre-intervention sessions (weeks 1 and 2) and after 4 weeks of the post-intervention session (week 6).
Blood pressure effects of guided slow breathing
DE Anderson et al
4
Journal of Human Hypertension
time or evening systolic BP for men. Similarly, no
significant pre- to post-intervention differences in
systolic BP for women or men in the CTL group were
observed in night, day, or evening segments of the
24-h BP cycle (Table 3).
Intervention effects on overnight breathing patterns
Table 2 also shows means and s.e. of overnight
breathing rate, tidal volume, and minute ventilation
for DGB and CTL groups before and after the
intervention. No significant differences between
groups, over time, or in the interaction between
group and time were found for overnight breathing
rate (F
1,38
0.48; Po0.49), tidal volume (F
1,38
0.01;
Po0.91) or minute ventilation (F
1,38
0.21; Po0.65).
Discussion
The DGB (but not the CTL) intervention decreased
clinic resting BP, mid-day ambulatory systolic BP (in
women only) and resting breathing rate, and
increased resting tidal volume. However, 24-h BP
level was not changed by the DGB or CTL interven-
tions, nor was overnight breathing pattern.
The findings on resting BP are consistent with
those in previous studies of longer duration,
18
and
support the view that the antihypertensive effects of
DGB on BP operate over a pathway in which a
prolonged expiratory phase of the respiratory cycle
exert reflex effects that decrease peripheral vasocon-
striction and increase peripheral blood flow.
9
As the
magnitude of BP effects of regular DGB has been
Figure 3 Mean hourly systolic BP over the 24-h day (beginning at midnight) preceding and following the DGB and CTL interventions
for men and women.
Table 2 Means and s.e. of 24-h systolic and diastolic blood pressure (BP), night time breathing rate, tidal volume and minute ventilation
preceding (pre) and following (post) the 4-week intervention phase for the device-guided breathing (DGB) and control (CTL) groups
Characteristic DGB CTL
Pre Post Pre Post
24-h systolic BP (mmHg) 138.2
1.9 137.7
2.3 137.3
1.9 137.8
2.2
24-h diastolic BP (mmHg) 84.6
1.1 83.8
1.5 80.4
1.7 81.8
1.7
Night time breathing rate ( per min) 15.70.4 15.70.4 15.70.6 16.00.6
Night time tidal volume (ml) 36127 36649 33030 32627
Night time min ventilation (l min
1
) 5.7
0.5 5.8
0.9 5.1
0.4 5.3
0.6
Blood pressure effects of guided slow breathing
DE Anderson et al
5
Journal of Human Hypertension
shown previously to depend on pre-intervention BP,
4
the magnitude of the effects reported here may also
reflect the borderline hypertensive condition of
the sample. The findings are also consistent with
the effects in a previous study that daytime BP in the
natural environment is decreased by regular practice
of DGB.
2
In this study, this finding was confined to
female subjects, but as discussed below, is consistent
with the results of other research, which suggests that
the associations of breathing pattern with BP may be
more marked in women than in men. That the effects
of DGB on daytime BP in women were related to
decreases in autonomic arousal is also consistent
with the results of a previous study with women
showing that acute increases in BP in the workplace
were accompanied by increases in perceived stress
and urinary catecholamines.
15
The findings in this study do not, however, support
the view that regular practice of DGB has effects on
mediators of long-term BP level. According to
Guytons formulation of hypertension pathogenesis,
neither changes in cardiac output or peripheral
resistance that accompany changes in sympathetic
nervous system activity can result in long-term
changes in BP because of the infinite ability of the
kidneys to adjust blood volume up or down to
maintain BP around its set point.
16
The development
of chronic hypertension necessarily involves changes
in the set point around which BP fluctuates, the locus
of which has variously been ascribed to the kidneys
11
or central nervous system.
17
Previous research found that sustained salt-sensi-
tive hypertension could be generated in laboratory
animals by intermittent suppression of breathing
that increased pCO
2
and generated a cascade of
responses involving transient changes in acidbase
balance and renal regulation of sodium.
18
From
those findings, it was speculated that regular
practice of DGB might alter renal regulation of
sodium and long-term BP through a respiratory
mechanism that includes sustained decreases in
pCO
2
.
19
In this study, resting PetCO
2
was measured
before and after the DGB and CTL interventions as
an index of possible changes in pCO
2
. In fact, a
significant decrease in resting PetCO
2
was observed
from the first screening session to the post-interven-
tion session in the DGB group. Positive associations
between resting PetCO
2
and resting BP have been
observed in previous studies with women. Higher
resting PetCO
2
has been associated with higher
resting systolic BP in women over 50 years of
age,
20
and especially if they scored low on trait
anger.
21
It has been hypothesized that high resting
PetCO
2
might have a permissive role in the devel-
opment of sodium-sensitive form of hypertension.
22
Although 24-h BP did not decrease in this study, it
would be premature to conclude that regular DGB
could not decrease 24-h BP under other conditions.
For example, the present intervention was 4 weeks
in duration, and at least two of the previous studies
of DGB continued to show a progression of
decreases in BP after the first 4 weeks.
3,5
The
adherence in this study was excellent, but 15min
per day is only a small fraction of the waking hours
during which deeper, slower breathing might exert
its effects. It is conceivable that an intervention that
encouraged deeper breathing over a greater percen-
tage of the day could affect the set point for BP.
In summary, the finding of no changes in 24-h BP
in response to repeated practice of DGB in the
context of significant changes in resting BP is poten-
tially important because of its implications for the
pathways mediating short- and long-term BP regu-
lation. It remains to further research to clarify the
Table 3 Means and s.e. of systolic and diastolic blood pressure (BP) (mmHg) for each of three 8-h intervals of the 24-h day preceding
(pre) and following (post) the device-guided breathing (DGB) and control (CTL) interventions for men and women
Group DGB CTL
Time Night
(00000800h)
Day
(08001600h)
Evening
(16002400h)
Night
(00000800h)
Day
(08001600h)
Evening
(16002400 h)
Systolic BP
Women
Pre 130.21.7 146.81.2 138.10.8 127.91.1 139.40.7 137.40.6
Post 131.6
1.0 141.4
0.6** 137.9
1.0 128.3
1.2 137.3
0.7 137.7
0.7
Men
Pre 123.7
0.8 137.8
0.8 137.7
1.7 128.7
0.9 142.3
0.9 138.3
1.0
Post 128.50.7 138.01.2 142.40.6 128.41.5 141.20.9 142.70.6
Diastolic BP
Women
Pre 79.9
1.7 89.8
0.5* 83.2
0.8 72.6
1.3 80.4
0.6 77.6
0.7
Post 79.2
0.8 87.2
0.6 82.3
1.0 71.8
0.9 81.6
0.8 81.7
0.7
Men
Pre 72.40.5 84.71.0 82.61.5 74.01.3 86.10.9 82.01.6
Post 76.4
0.4 84.8
0.9 83.9
0.8 77.1
1.5 84.1
1.2 85.7
0.7
**Po0.001; *Po0.05.
Blood pressure effects of guided slow breathing
DE Anderson et al
6
Journal of Human Hypertension
extent to which retraining in breathing patterns is
capable of producing salutary effects on mechan-
isms involved in long-term BP regulation.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
This research was solely supported by the Intramural
Research Program of the NIH, National Institute
on Aging. The authors are indebted to Dr Deborah
Grady for calling our attention to the guided brea-
thing device, and to Drs Benjamin Gavish, S Mortesa
Farasat and Margaret A Chesney for review of the
paper.
References
1 Grossman E, Grossman A, Schein MH, Zimlichman R,
Gavish B. Breathing control lowers blood pressure.
J Hum Hypertens 2001; 15: 263269.
2 Rosenthal T, Alter A, Peleg E, Gavish B. Device-guided
breathing exercises reduce blood pressure: ambulatory
and home measurements. Am J Hypertens 2001; 14:
7476.
3 Schein MH, Gavish B, Herz M, Rosner-Kahan D, Naveh
P, Knishkowy B et al. Treating hypertension with a
device that slows and regularizes breathing: a rando-
mized, double-blind controlled study. J Human
Hypertens 2001; 15(4): 271278.
4 Viskoper R, Shapira I, Priluck R, Mindlin R, Chornia L,
Laszt A et al. Nonpharmacologic treatment of resistant
hypertensives by device-guided slow breathing exer-
cises. Amer J Hypert 2003; 16: 484487.
5 Meles E, Giannattasio C, Failla M, Gentile G, Capra A,
Mancia G. Nonpharmacologic treatment of hyper-
tension by respiratory exercise in the home setting.
Am J Hypertens 2004; 17: 370374.
6 Elliott WJ, Izzo JL, White WB, Rosing DR, Snyder CS,
Alter A et al. Graded blood pressure reduction in
hypertensive outpatients associated with use of a
device to assist with slow breathing. J Clin Hypertens
2004; 6: 553559.
7 Logtenberg SJ, Kleefstra N, Houweling ST, Groenier
KH, Bilo HJ. Effect of device-guided breathing ex-
ercises on blood pressure in hypertensive patients with
type 2 diabetes mellitus: a randomized clinical trial.
J Hypertens 2007; 25: 241246.
8 Schein MH, Gavish B, Baevsky T, Kaufman M, Levine
S, Nessing A et al. Treating hypertension in type II
diabetic patients with device-guided breathing: a
randomized controlled trial. J Hum Hypertens 2008;
23: 325331.
9 Parati G, Izzo JL, Gavish B. Respiration and blood
pressure. In: Izzo JL, Sica DA, Black HR (eds). Hyper-
tension Primer. American Heart Association: Dallas,
TX, 2008, pp 136138.
10 Joseph CN, Porta C, Casucci G, Casiraghi N, Maffeis M,
Rossi M et al. Slow breathing improves barorefex
sensitivity and decreases blood pressure in essential
hypertension. Hypertens 2005; 46(4): 714718.
11 Cowley AW. Long-term control of arterial blood
pressure. Physiol Rev 1992; 72: 231300.
12 Anderson DE, McNeely JD, Windham BG. Device-guided
slow breathing effects on end tidal CO
2
and heart rate
variability. Psychol Health Med 2009; 14: 667679.
13 Benson H, Klipper MZ. The Relaxation Response.
Wings Books: New York, NY, 1992.
14 Wilhelm FH, Roth WT, Sackner MA. The LifeShirt. An
advanced system for ambulatory measurement of
respiratory and cardiac function. Behav Modif 2003;
27: 671691.
15 Kario K, James GD, Marion RM, Ahmed M, Pickering
TG. The influence of work- and home-related stress on
the levels and diurnal variation of ambulatory blood
pressure and neurohumoral factors in employed
women. Hypertens Res 2002; 25: 499506.
16 Guyton AC. Dominant role of the kidneys and the
accessory role of whole-body autoregulation in the
pathogenesis of hypertension. Amer J Hypertens 1989;
2: 575585.
17 Julius S, Weder AB. Brain and the regulation of blood
pressure: a hemodynamic perspective. Clin Exper
Hypertens 1989; 11(Suppl): 119.
18 Anderson DE. Behavior analysis and the search for the
origins of hypertension. J Exp Anal Behav 1994; 61:
255261.
19 Honig A. Peripheral arterial chemoreceptors and reflex
control of sodium and water homeostasis. Am J Physiol
Integ Comp Physiol 1989; 257(26): R1282R1302.
20 Anderson DE, Parsons D. Association of end tidal CO
2
with longitudinal blood pressure elevation. Am J
Hypertens 1999; 17: 10731079.
21 Scuteri A, Parsons DJ, Chesney MA, Anderson DE.
Anger Inhibition potentiates the association of high
end tidal CO
2
with blood pressure of women. Psycho-
som Med 2001; 63: 470475.
22 Anderson DE, Scuteri A, Agalakova N, Parsons DJ,
Bagrov AY. Racial differences in resting end tidal
CO
2
and sodium pump inhibitor. Amer J Hypert 2001;
14(8 part 1): 761767.
What is known about this topic
K Several previous studies have reported that regular practice
of device-guided slow breathing exercises decrease resting
blood pressure (BP) in hypertensive patients.
K Device-guided slow breathing is known to be accompanied
by decreases in peripheral vasoconstriction, but whether
they produce decreases in 24-h BP remains to be
determined.
What this study adds
K This study shows that daily practice of device-guided slow
breathing exercises decreases resting, but not 24-h BP in
patients with mild hypertension.
K The decreases in resting BP are accompanied by decreases
in breathing rate and increases in tidal volume at rest.
K These results raise the issue of whether the salutary effects
of slow breathing exercises address the root causes of
hypertension, or merely decrease the autonomic influence
on BP.
Blood pressure effects of guided slow breathing
DE Anderson et al
7
Journal of Human Hypertension
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Postpartum Discharge PlanDocument3 pagesPostpartum Discharge PlanCassey CamamaNo ratings yet
- ICMRDocument12 pagesICMRAnil KumarNo ratings yet
- hf305 00 Dfu DeuDocument54 pageshf305 00 Dfu DeuMauro EzechieleNo ratings yet
- Thesis On Hypertension in PregnancyDocument7 pagesThesis On Hypertension in Pregnancydwt29yrp100% (2)
- Autonomic Dysfunction and Hypotension: Christopher J. MathiasDocument28 pagesAutonomic Dysfunction and Hypotension: Christopher J. MathiaswaltercarvalhoNo ratings yet
- Fi H 0840 004 ParDocument16 pagesFi H 0840 004 ParNathaniel Roi BalbarinoNo ratings yet
- PED 001 Module (Prelim)Document37 pagesPED 001 Module (Prelim)Keith Ian JulianNo ratings yet
- TB4-Frag A Collection of StudiesDocument20 pagesTB4-Frag A Collection of StudiesscribdNo ratings yet
- Management of Chronic Kidney Disease (Mutraghata) Through Ayurveda Regimen: A Case ReportDocument12 pagesManagement of Chronic Kidney Disease (Mutraghata) Through Ayurveda Regimen: A Case ReportakhilkgNo ratings yet
- BP Chart Boys Color WideDocument1 pageBP Chart Boys Color WidealbertNo ratings yet
- Combination of Lisinopril and Nifedipine GITS.10Document7 pagesCombination of Lisinopril and Nifedipine GITS.10Andi PermanaNo ratings yet
- Health and Vastu Shastra Tips For Happy Life - SubhaVaastuDocument14 pagesHealth and Vastu Shastra Tips For Happy Life - SubhaVaastuMadhu46dNo ratings yet
- Management of Acute Ischemic Stroke.13Document10 pagesManagement of Acute Ischemic Stroke.13Juan fernando Torres pavaNo ratings yet
- ACOG Practice Bulletin No 202Document25 pagesACOG Practice Bulletin No 202Berri RahmadhoniNo ratings yet
- Merck Interest AreasDocument40 pagesMerck Interest AreasPhil MurrayNo ratings yet
- EMS Field Handbook (Revision 1) PDFDocument61 pagesEMS Field Handbook (Revision 1) PDFAnonymous qAEhQo1No ratings yet
- Understanding Cardiomyopathies and Cardiac Conduction DisordersDocument86 pagesUnderstanding Cardiomyopathies and Cardiac Conduction DisordersStarr Newman100% (1)
- Dental Care For Patients With Heart Failure: An UpdateDocument9 pagesDental Care For Patients With Heart Failure: An UpdateGustavo A OrtegonNo ratings yet
- Hypertension Topic DiscussionDocument13 pagesHypertension Topic Discussionapi-665372449No ratings yet
- Aprovel TabletDocument7 pagesAprovel Tabletramesh4321No ratings yet
- Diabetes Among HIV-Infected Patients On Antiretroviral Therapy at Mulago National Referral Hospital in Central UgandaDocument6 pagesDiabetes Among HIV-Infected Patients On Antiretroviral Therapy at Mulago National Referral Hospital in Central UgandaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 56 JOE Hypert Peria Cond 2010Document6 pages56 JOE Hypert Peria Cond 2010nurima diyahNo ratings yet
- Jurnal InternationalDocument9 pagesJurnal InternationalRulix SevenfoldNo ratings yet
- User Manual: Blood Pressure Monitor EBP-095 Arm TypeDocument14 pagesUser Manual: Blood Pressure Monitor EBP-095 Arm TypeRhea Jane B. CatalanNo ratings yet
- Ritalin LaDocument20 pagesRitalin Lamichele.siciliano4467No ratings yet
- Chlorthalidone, Not Hydrochlorothiazide, Is The Right Diuretic For ComparisonDocument2 pagesChlorthalidone, Not Hydrochlorothiazide, Is The Right Diuretic For ComparisonZeba Sohel KhatriNo ratings yet
- Serpentina Treatment: A Review of LiteratureDocument11 pagesSerpentina Treatment: A Review of LiteraturedanisterNo ratings yet
- Vegan Soul Food Cookbook Plant-Based, No-Fuss Southern Favorites by Nadira Jenkins-ElDocument209 pagesVegan Soul Food Cookbook Plant-Based, No-Fuss Southern Favorites by Nadira Jenkins-ElRomylar Dee100% (3)
- Textbook Geriatric Psychiatry 09 PDFDocument23 pagesTextbook Geriatric Psychiatry 09 PDFLydia AmaliaNo ratings yet
- Roth 10e Nclex Chapter 11Document4 pagesRoth 10e Nclex Chapter 11jennaaahhhNo ratings yet