Professional Documents
Culture Documents
Prediction and Prevention of Type 1 Diabetes Mellitus
Uploaded by
dwifit3Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Prediction and Prevention of Type 1 Diabetes Mellitus
Uploaded by
dwifit3Copyright:
Available Formats
Journal of Diabetes 3 (2011) 4857
REVIEW ARTICLE
Prediction and prevention of Type 1 diabetes mellitus
Li ZHANG and George S. EISENBARTH
Barbara Davis Center for Childhood Diabetes, University of Colorado Denver, Aurora, Colorado, USA
Correspondence George S. Eisenbarth, Barbara Davis Center for Childhood Diabetes, University of Colorado Denver, Aurora, CO 80045, USA. Tel: +1 303 724 6847 Fax: +1 303 724 6839 Email: George.Eisenbarth@UCDENVER.EDU Received 9 August 2010; revised 20 September 2010; accepted 24 October 2010. doi: 10.1111/j.1753-0407.2010.00102.x
Abstract Type 1A diabetes mellitus (T1DM) is caused by autoimmune islet b-cell destruction with consequent severe insulin deciency. We can now predict the development of T1DM by determining four biochemically characterized islet autoantibodies, namely those antibodies against insulin, glutamic acid decarboxylase 65, insulinoma antigen (IA)-2 (ICA512) and the zinc transporter ZnT8. We can also prevent T1DM in animal models, but the nal goal is the prevention of T1DM in humans. Multiple clinical trials are underway investigating methods to prevent b-cell destruction. Keywords: immunotherapy, prediction, prevention, Type 1 diabetes.
Introduction Type 1A diabetes mellitus (T1DM) is characterized by autoimmune-mediated selective destruction of pancreatic b-cells, with consequent severe insulin deciency. There are other forms of insulin-decient diabetes, including monogenic forms.1 T1DM is commonly diagnosed in children and adolescents, but can occur at any age. T1DM presents with hyperglycemia and usually a need for immediate exogenous insulin treatment. The incidence of T1DM in many developed countries is now twice as high among children as it was in the 1980s.2,3 In north Italy, the overall incidence rate from 1984 to 2004 in the 029 years age group has been reported to be 11.3 100 000 personyears.4 Furthermore, both the 014 and 1529 year age groups had a 60% higher risk in 20002004 compared with the period 19841989.5 During the past two decades, improved understanding of the natural history and pathogenesis of T1DM have led to the ability to predict the disease in humans and to prevent it in animal models. Clinical trials for the prevention of T2DM in humans are underway. Prediction of diabetes Anti-islet autoimmunity precedes the development of T1DM (usually by years) and is associated with
48
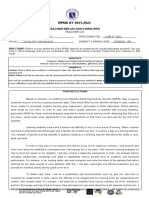
progressive metabolic abnormalities. The ability to predict the development of T1DM has been improved markedly with the combined use of genetic, islet autoantibody and metabolic testing.6 Genetic prediction T1DM has a strong genetic component, reected by the observation that rst-degree relatives have a higher risk than the general population, siblings have a higher risk (6% vs 0.4%; sibling kS 15)7 than offspring8 and there is a high concordance rate in identical twins with diabetes (approximately 50%).9 When initially nondiabetic monozygotic twins of patients with T1DM are followed prospectively, the cumulative incidence for anti-islet autoimmunity and diabetes may exceed 70% and there is no duration of discordance at which monozygotic twins are not at risk for progression.10 Diabetes susceptibility in the non-obese diabetic (NOD) mouse model results from the interaction of multiple loci (>40),11 with the strongest predisposing effect deriving from genes within the major histocompatibility complex (MHC), namely human leukocyte antigen (HLA) in humans.12,13 Similarly, with recent genome-wide association studies, >40 loci associated with T1DM have been identied, with by far the most important determinants of disease in the MHC (HLA region of humans; Fig. 1).14,15 There are three classes
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
L. ZHANG and G.S. EISENBARTH
Type 1 diabetes prediction and prevention
6.50
Odds ratio
2.25 2.00 1.75 1.50 1.25 1.00 HLA INS PTPN22 ILR2A SH2BE ERBB3 PTPN2 CLEC16A CTLA4 IL18RAP PTPN2 OCR5 IFIHI CTSH CD226 IL2RA PRKCQ IL2 BACH2 UBASH3A RGS1 IL7RA CITNF6 TNFAIP3 TNFAIP3 TAGAP
Locus
Figure 1 Loci associated with risk of Type 1 diabetes identied in genome-wide association studies.14,15 (h), insulin protection and metabolism; ( ), immunity; ( ), b-cell apoptosis protection; ( ), unknown function.
of HLA genes, with Class II HLA molecules (DP, DQ, and DR) having the strongest association with T1DM. Class II HLA genes encode molecules that participate in antigen presentation to CD4 T cells. Polymorphic variants of Class II HLA genes determine 4060% of genetic susceptibility.1618 DQ molecules are formed by two polymorphic genes (a and b) and each amino acid variant of a and b is given a four digit number preceded by the gene designation (e.g. DQB1*0302). Two of the most common high-risk DQ haplotypes (DQa and b) are DQA1*0301 with DQB1*0302 and DQA1*0501 with DQB1*0501. Many studies have veried that DQB1*0302 is a strong susceptibility allele and that the heterozygous combination of DQA1*0301DQB1*0302 on an HLA-DR4 haplotype and DQA1*0501-DQB1*0201 on an HLADR3 haplotype results in enhanced risk of T1DM.13,19 In Denver (CO, USA), 2.4% of newborns from the general population are DR3 4 heterozygote with DQB1*0302. These individuals have an absolute risk of developing T1DM of approximately 1 15 compared with a risk of 1 300 in the general population.19 The genetic screening for susceptible HLA-DQB1 alleles and the follow-up of higher-risk newborn Finnish children identied 77% of those who developed the disease before 3 years of age.20 A screening strategy based on HLA-DQA1-DQB1 typing identied four susceptible genotypes (DQ*0301-0302 DQ*0501-0201, DQ*03010302 DQ*03010302, DQ*0501-0201 DQ*0501-0201, and DQ*03010302 Y) that accounted for 9% of the population and included approximately 60% of future diabetic patients diagnosed before 40 years of age and up to 70% of those diagnosed before 5 years of age.21 Class II HLA is strongly associated with T1DM in both Asian and Caucasian populations, but haplotypes
associated with T1DM are markedly different due to differences in the presence and absence of haplotypes in each population.2224 Standard HLA molecular typing is too costly for population screening at this time, but simplied molecular testing is possible. A rapid test to identify DR3 4-DQ8 subjects analyzed two single nucleotide polymorphisms (SNPs), specically rs2040410 and rs7454108, which are associated with DR3-DQB1*0201 and DR4DQB1*0302.25 These SNPs were analyzed in samples from 143 HLA-typed children who participated in the Diabetes Autoimmunity Study of the Young (DAISY), as well as in 5019 subjects from the Type 1 Diabetes Genetic Consortium (T1DMGC). In the T1DMGC samples, the two SNPs were found to have a sensitivity of 98.5% (1173 1191) and a specicity of 99.7% (3815 3828) for DR3 4-DQB1*0302. In the DAISY population, the test was 100% sensitive (69 69) and 100% specic (74 74). Lavant and Carlson26 have developed a high-throughput HLA-typing method that accurately distinguishes risk alleles. This method allows screening of several thousand samples per week, consuming 32 ng DNA template, low reagent volumes, and minimal time for data review.26 Autoantibody prediction The presence of autoantibodies against multiple islet antigens with specic assays (specicity 99%) predicts the development of T1DM. In the 1970s, using frozen sections of human pancreas, antibodies to islet cells (ICA) was identied as the rst autoantibody.27 Following the discovery of ICA, multiple biochemical antibodies were identied before or at the onset of diabetes and used to diagnose diabetes, as well as in research settings to predict diabetes. Standard well-characterized autoantibodies react with insulin [i.e. anti-insulin antibodies (IAA)], the tyrosine phosphatases insulinoma antigen (IA)-2 and IA-2b, and glutamic acid decarboxylase (GAD).2830 More recently, antibodies against the zinc transporter (ZnT8) were discovered and are now used for the prediction and diagnosis of diabetes.31 Table 1 summarizes basic information concerning the autoantibodies used to predict diabetes. Prospective population-based studies, such as DAISY,32 the German BabyDIAB study,33 and the Finnish diabetes prediction and prevention (DIPP) study,34,35 have established that the autoantibody markers appear months or years before the onset of diabetes and can occur as early as in the rst year of life.32,36 The presence of a single islet autoantibody is associated with relatively low risk on long-term follow-up (<5%), whereas individuals expressing two
49
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
Type 1 diabetes prediction and prevention
L. ZHANG and G.S. EISENBARTH
Table 1 Major autoantibody markers for type 1 diabetes Sensitivity (%) 70
Autoantibody ICA
Description Multiple and variable target molecules, major antigen specicity: GAD and IA-2 IA-2b Proteins of 65 kDa 67 kDa anchored within membranes of small synaptic-like microvesicles of islet cells or synaptic vesicles of neurons The only b-cell-specic antigen so far identied Highly evolutionarily conserved protein 40-kDa tryptic fragment of IA-2, a member of the protein tyrosine phosphatase-like proteins Expressed in secretory granules of b-cells and neuroendocrine cells Islet zinc transporter
Implication in diagnosis prediction High ICA-titer correlated with increased risk of diabetes in relatives Difcult to standardize pancreatic sections Major antigenic region: middle and carboxy-terminal regions of GAD65 Epitope recognition conformationally dependent Prevalence of GADA increase with age IAA rst to appear during insulitis in young children
GADA
6575
mIAA
4992
IA-2
Anti-ZnT8
Immunodominant region: intracellular domain Epitope recognition conformationally dependent Presence of IA-2A in multiple antibody-positive relatives predicts rapid progression to diabetes Present in most patients with Type 1 diabetes There are two major polymorphic variants of ZnT8, one with a tryptophan and the other with an arginine at position 325 of the molecule Most patients have autoantibodies recognizing both variants
74
6575
GAD, glutamic acid decarboxylase; GADA, antibodies to GAD; IA-2, insulinoma antigen 2; ICA, antibodies to islet cells; mIAA, microinsulin autoantibody.
or more of the autoantibodies almost always progress given long enough follow-up. It is not clear whether those with single islet autoantibodies who do not progress have islet-directed autoimmunity or simply the development of an antibody that cross-reacts with an islet autoantigen. Given screening for autoantibodies reacting with four islet autoantigens, and specicities of 99%, approximately 4% of normal controls express a single islet autoantibody whereas <1 in 300 would express two or more autoantibodies. The antigens recognized by ICA staining of pancreatic sections include GAD, IA-2 and ZnT8, but are not limited to these. In some studies of general populations, the predictive value of ICA was low (13%).37,38 The large Diabetes Prevention Trial Type 1 (DPT-1) tested autoantibodies in relatives of patients with T1DM.39 The occurrence of T1DM was only 3.9% in relatives expressing ICA only and negative for biochemical autoantibodies [IAA, autoantibodies to GAD (GADA), and ICA512 (IA-2)]. Among those with single positivity for GAD65 and ICA, increased incidence of T1DM was related to higher antibody titer. By 7 years of follow-up, ICA-positive schoolchildren and relatives (i.e. those with ICA titers 10 Juvenile Diabetes Foundation units) had similar progression to diabetes (45% vs 43%).40 In most studies, ICA has been combined with other autoantibodies to predict diabetes. The data from the large DPT-1 study39 demonstrated that ICA autoantibodies, as well as GAD and
50
IA-2 autoantibodies, in relatives were relatively stable, with 7585% of all positivity (9095% with high levels) conrmed during follow-up. Given the difculty of standardizing the immunouorescent islet cell antibody assay that uses frozen sections of normal human pancreas, this assay is no longer commonly used. IA-2, also known ICA512, is a transmembrane protein localized to the secretory vesicles of both endocrine and neuroendocrine tissues. T1DM-associated autoantibodies to IA-2 (IA-2A) react with the intracellular section of the protein. In particular, it has been reported that sera from T1DM patients recognize either amino acids 771979 of the carboxyl terminal domain or the amino terminal part of the intracellular domain.41,42 Recently, it was reported that antibodies reactive with the extracellular domain of IA-2 (1577) are associated with faster T1DM progression.42 In the Childhood Diabetes in Finland (DiMe) study, siblings who progressed to clinical diabetes had IA-2 antibodies specic to the juxtamembrane region more often than siblings who did not progress to T1DM.43 These ndings suggest that juxtamembrane region-specic IA-2 antibodies are associated with an increased risk of progression to overt T1DM, whereas an IgE response to IA-2 confers relative protection against clinical disease.43 Makinen et al.44 compared epitope- and isotype-specic IA-2 antibodies between children with a humoral immune response restricted to IA-2 and children with a broad response including
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
L. ZHANG and G.S. EISENBARTH
Type 1 diabetes prediction and prevention
IAA and GADA in addition to IA-2A. Children with newly diagnosed T1DM, who test positive to IA-2A only of the three molecular antibodies predictive of T1DM, had a broader IA-2-specic isotype response and stronger association with the high-risk HLA haplotype than did those children testing positive for all three molecular antibodies. GADA, a 64-kDa antigen,45 is found in approximately 70% of newly diagnosed T1DM patients.46 GAD has two isoforms. Both human and rat islets predominantly express GAD65, whereas GAD67 is the major GAD isoform in mouse islets.47 The presence of anti-GAD65 antibodies along with anti-IA-2 antibodies is a highly predictive marker for the development of T1DM in humans. The prevalence of anti-GAD65 and anti-IA-2 antibodies is approximately 90% in newly diagnosed T1DM patients and prediabetic individuals.48 LaGasse et al.37 recommended the combined use of GADA, IA2-A, and IAA for screening, but ZnT8 autoantibodies should now also be considered to complete the panel of well-characterized assays. A combination of GADA and IA-2A for primary screening has been described to be as sensitive as the combination of IAA and GADA.49 In 1983, Palmer et al.30 discovered the presence of IAA in patients with new-onset T1DM prior to the administration of exogenous insulin. Further studies revealed the presence of IAA in rst-degree relatives of diabetic patients.5052 The insulin antibody afnity and epitope specicity for insulin autoantibodies can predict which children are at high risk of progressing to diabetes. Children with high genetic risk who develop insulin antibodies (IAAs) early in life often subsequently develop multiple antibodies and eventually diabetes29 and insulin autoantibodies are usually the rst autoantibody to appear in young children developing T1DM.51,53,54 In the BabyDIAB study,51 a high percentage of children who went on to develop multiple anti-islet autoantibodies and or progress to diabetes expressed high-afnity autoantibodies (>109 L mol). The levels of insulin autoantibodies are inversely correlated with the age at which T1DM develops. Thus, levels >2000 nU mL are almost exclusively found in patients who progress to T1DM prior to 5 years of age; less than half the individuals developing T1DM after 15 years of age have anti-insulin autoantibodies levels exceeding those in controls.51 To some extent, the levels of these antibodies are genetically inuenced and are associated with DR4 and DQ8.51 There are data suggesting that the levels of anti-insulin autoantibodies among ICA-positive rst-degree relatives are correlated with the rate at which individuals progress to overt diabetes.55 However, those relatives
who only express anti-insulin autoantibodies progress to overt diabetes infrequently.51 The islet b-cell zinc cation efux transporter ZnT8 (Scl30A8) is a newly dened target of islet autoantibodies.31 This transporter was discovered as an autoantigen because it is specically expressed in islet b-cells, where it is associated with the regulated pathway of insulin secretion. ZnT8 facilitates the transportation of Zn2+ from the cytoplasm into the insulin secretory granule, where zinc is complexed with insulin, forming insulin crystals. Autoantibodies reacting with ZnT8 are present in most patients with T1DM and assay specicity and sensitivity are similar to those for GAD65 autoantibodies.31 For at-risk populations, such as relatives of patients with T1DM and individuals with high-risk HLA alleles from the general population, we measure ZnT8 autoantibodies in those expressing a single anti-islet autoantibody. If ZnT8 autoantibodies are present, these individuals would have two or more anti-islet autoantibodies and thus have a much higher risk of progressing to diabetes.5658 The presence of >1 persistently positive antibody has been shown to reliably predict the development of T1DM.32,59 If four markers are measured (i.e. GADA, IA-2A, IAA, and ZnT8A), <10% of patients with T1DM are autoantibody negative, fewer than 10% have only one marker, and approximately 70% have three or four markers.60 There is a general consensus that the presence of multiple autoantibodies (i.e. two or more) is associated with a high risk of developing diabetes while the presence of single islet cell-related autoantibodies has usually a low predictive value (<1 4). The DPT-1 study demonstrated that there was a signicant association between the increasing occurrence of T1DM and increasing autoantibody number.39 The TrialNet study estimated 5-year diabetes risk by measuring GADA, ICA512A, microinsulin autoantibody (mIAA), or ICA.61 In summary, in T1DM relatives as well in the general population, the risk of developing disease increases with the number of positive autoantibodies.38,62 T1DM relatives with two or more antibodies had a 39% and 68% risk of developing T1DM within 3 and 5 years, respectively; relatives positive for three autoantibodies have an estimated >90% risk of developing T1DM within 5 years.62 For diabetes prediction, a combination of GADA and IA-2 for primary screening, followed by ICA and IAA testing, has been proposed.49,63,64 Data from DPT-1 indicate that screening based on two antibodies and testing individuals positive for one of the remaining markers results in a sensitivity of 96.7% for GADA and ICA512, 96.7% for mIAA and GADA, 93% for ICA and ICA512, and
51
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
Type 1 diabetes prediction and prevention
L. ZHANG and G.S. EISENBARTH
99% for the combination of GADA and ICA.65 As the assay methodology becomes simpler, we believe simply measuring all four biochemical autoantibodies will become standard. Clinical trials for the prevention of b-cell destruction Prevention of T1DM, based on the prevention of islet b-cell destruction, can be considered at different stages of the disease, from stages prior to or following the onset of hyperglycemia. More specically, primary prevention would be applied in genetically susceptible individuals (or whole populations if the modality was safe enough; for example, vaccination) prior to the presence of islet autoantibodies. This could be accomplished by eliminating exposure to triggering factors or immune intervention. The Trial to Reduce IDDM in the Genetically at Risk (TRIGR) study is evaluating the elimination of bovine milk products early in life,6669 whereas the PrePoint study is evaluating oral insulin in very high-risk children.70 Secondary prevention is performed after autoantibodies develop (at present T cell assays do not have a high enough positive predictive value to be used for prediction), but before the onset of hyperglycemia to prevent further b-cell loss and to induce immunologic remission. Tertiary prevention seeks to stop further b-cell destruction after its clinical manifestation with hyperglycemia present. Antigen-specic therapy The most extensively studied antigens used in trials for the prevention of immunologic b-cell destruction are insulin and GAD. The National Institutes of Health (NIH) Diabetes Prevention Trial (DPT) was started with the goal of nding out whether insulin-based therapies (i.e. low-dose parenteral insulin therapy to high-risk relatives or oral insulin to intermediate-risk relatives to induce oral tolerance) would prevent or delay the onset of diabetes in cytoplasmic islet autoantibody-positive relatives of patients with T1DM. Relatives were staged in terms of their expression of insulin autoantibodies, metabolic abnormalities, and the presence of the protective HLA allele DQB1*0602. In addition, GAD65 and ICA512 autoantibodies were measured, although not included as entry criteria. These large studies, as well as the European Nicotinamide Diabetes Intervention Trial (ENDIT) using nicotinamide, demonstrated the ability to predict T1DM on a relatively large scale and to assign various levels of risk for disease.7173 Unfortunately, overall none of these studies demonstrated a delay in or the
52
prevention of progression to diabetes. In one subgroup of the oral insulin trial, namely those with high levels of insulin autoantibodies, oral insulin signicantly slowed progression to diabetes (by approximately 4.5 years).74 Given this subgroup analysis, the NIH TrialNet group is now seeking to conrm whether oral insulin can ameliorate progression to diabetes of relatives with multiple islet autoantibodies and high levels of insulin autoantibodies. GAD65 is a prominent autoimmune target in humans, with GAD65 autoantibodies one of the best predictors of progression to diabetes. To assess the ability of alum-formulated GAD (GAD-alum) to reverse recent-onset T1DM in patients 1018 years of age, Ludvigsson et al.75 administered 20 lg GAD-alum to 35 patients with recent-onset T1DM and examined with the autoantigen could reduce or halt the loss of residual insulin secretion. In this trial GAD-alum vaccination delayed the loss of fasting C-peptide compared with a placebo group, although there was no improvement in HbA1c or a decrease in insulin requirements.75 Conrmatory studies of GAD65 vaccination are underway in Europe and the US, including a new-onset TrialNet study, with plans for a prevention study (detailed information is available at http:// clinicaltrial.gov). Anti-CD3 The clinical use of the original anti-CD3 (OKT3) monoclonal antibody has been limited by its induction of cytokine release syndrome with, in severe cases, pulmonary edema developing within hours of treatment.76 Two specic humanized FcR non-binding anti-CD3 antibodies, namely teplizumab and otelixizumab, have been investigated in patients with recent-onset T1DM. Herold et al.76 recruited 24 subjects with new-onset T1DM. In that open-label study, the 12 subjects randomized to test therapy were given daily infusions of teplizumab for 14 days. The control group underwent the same metabolic and immunologic studies as the drug-treated group, but the patients did not receive an infusion and were not hospitalized. The treatment group had maintenance of C-peptide responses for 1 year, whereas the control group showed signicant decline.76 Longer follow-up of patients treated with anti-CD3 indicates that, after 1 year, C-peptide loss resumes in the anti-CD3-treated patients but that C-peptide secretion exceeds that in controls. In keeping with the maintained b-cell function, the treatment group had lower HbA1c levels and lower insulin requirements compared with the control group.76 In addition, decreased insulin utilization was associated
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
L. ZHANG and G.S. EISENBARTH
Type 1 diabetes prediction and prevention
with decreased loss of C-peptide. In a multicenter European study of a second modied anti-CD3,77 80 patients with new-onset T1DM were randomly assigned to receive placebo or otelixizumab for six consecutive days and patients were followed for 18 months. At 6, 12, and 18 months, residual b-cell function was better maintained with otelixizumab than with placebo. Twelve of 16 patients who received otelixizumab (75%) needed minimal doses of insulin (0.25 IU kg per day) compared with none of the 21 patients who received placebo. Short-term treatment with CD3 antibody preserves residual b-cell function for over 48 months in patients with recent-onset T1DM.78 B Lymphocyte-targeted therapies Rituximab (anti-CD20) is a monoclonal antibody that is a chimeric murine human monoclonal IgG1 kappa antibody. It selectively targets and depletes human CD20-expressing B cells. Anti-CD20 has been used as therapy for B cell lymphoma and shows efcacy in multiple sclerosis and rheumatoid arthritis.79,80 A transgenic NOD mouse expressing human CD20 (hCD20) on B cells has been generated.81 In this mouse model, a single cycle of treatment with an antibody specic for hCD20 temporarily depleted B cells and signicantly delayed and or reduced the onset of diabetes.81 In addition, anti-CD20 treatment of B cell depletion prolongs syngeneic islet graft survival, delays the onset of recurrent autoimmune diabetes, and may reverse the disease in hCD20 NOD mice.82,83 TrialNet investigators conducted a randomized double-blind placebo-controlled study with a single course of antiCD20.83 At 1 year, the mean level of C-peptide was signicantly higher in the rituximab-treated group than in the placebo group. In addition, the rituximabtreated group had signicantly lower HbA1c levels and required less insulin. Between 3 and 12 months, the rate of decline in C-peptide levels in the rituximab-treated group was signicantly less than in the placebo group,83 but thereafter C-peptide loss continued. Nevertheless, further investigations are essential (including more than a single drug course) to evaluate both efcacy and safety of rituximab as a single agent in people at risk of developing diabetes, as well as in new-onset diabetes patients. Summary Given the observation that one in 300 random cadaveric donors express two or more islet autoantibodies,84,85 it is likely that approximately 1 million
individuals in the US are in the process of developing T1DM. If safe and effective preventive therapy were developed that could prevent the progression to diabetes, even currently available islet autoantibody assays could provide the basis for large-scale screening. It is very likely that assays will improve and, indeed, the Immunology of Diabetes Society, in collaboration with the US Centers for Disease Control (CDC), has a program in place to improve worldwide assay standardization, namely the Diabetes Autoantibody Standardization Program (DASP) workshops.86 In the absence of such therapy, the screening of large populations for islet autoantibodies is performed primarily for research, although the detection of islet autoantibodies does allow the prevention of life-threatening ketoacidosis at diabetes onset.87 Large Phase III trials of both GAD65 immunization and anti-CD3 infusion in patients with recent-onset diabetes are now underway. The mechanism by which either of these therapies may delay b-cell destruction in humans at this time is poorly understood, with initial evidence pointing to enhancement of regulatory T cell responses.88,89 A major goal will be the long-term (measured in years), safe prevention of b-cell loss. It is likely that none of the agents in the current trials by themselves will provide long-term protection for most patients if given as a single course. Thus, there remains a need for both the development of novel therapeutic approaches and trials of combined therapies.90,91 Acknowledgments The authors work reported herein was supported by grants from the Brehm coalition and the Childrens Diabetes Foundation. LZ is supported by an ADA postdoctoral fellowship (7-06-MN-17). Disclosure GSE has consulted for Bayhill Therapeutics, Genetech, Glaxo Smith Kline, and Eli Lilly. This manuscript has not been published or submitted for publication elsewhere. References
1. Grulich-Henn J, Wagner V, Thon A et al. Entities and frequency of neonatal diabetes: data from the diabetes documentation and quality management system (DPV). Diabet Med. 2010; 27: 70912. 2. Eurodiab ACE Study Group. Variation and trends in incidence of childhood diabetes in Europe. EURODIAB ACE Study Group. Lancet. 2000; 355: 8736.
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
53
Type 1 diabetes prediction and prevention
L. ZHANG and G.S. EISENBARTH
3. Vehik K, Hamman RF, Lezotte D et al. Increasing incidence of Type 1 diabetes in 0- to 17-year-old Colorado youth. Diabetes Care. 2007; 30: 5039. 4. Carle F, Gesuita R, Bruno G et al. Diabetes incidence in 0- to 14-year age-group in Italy: a 10-year prospective study. Diabetes Care. 2004; 27: 27906. 5. Bruno G, Novelli G, Panero F et al. The incidence of type 1 diabetes is increasing in both children and young adults in Northern Italy: 19842004 temporal trends. Diabetologia. 2009; 52: 25315. 6. Atkinson MA, Eisenbarth GS. Type 1 diabetes: new perspectives on disease pathogenesis and treatment. Lancet. 2001; 358: 2219. 7. Spielman RS, Baker L, Zmijewski CM. Gene dosage and susceptibility to insulin-dependent diabetes. Ann Hum Genet. 1980; 2: 13550. 8. Risch N. Assessing the role of HLA-linked and unlinked determinants of disease. Am J Hum Genet. 1987; 40: 114. 9. Kumar D, Gemayel NS, Deapen D et al. North-American twins with IDDM. Genetic, etiological, and clinical signicance of disease concordance according to age, zygosity, and the interval after diagnosis in rst twin. Diabetes. 1993; 42: 135163. 10. Redondo MJ, Jeffrey J, Fain PR, Eisenbarth GS, Orban T. Concordance for islet autoimmunity among monozygotic twins. N Engl J Med. 2008; 359: 284950. 11. Rainbow DB, Esposito L, Howlett SK et al. Commonality in the genetic control of Type 1 diabetes in humans and NOD mice: variants of genes in the IL-2 pathway are associated with autoimmune diabetes in both species. Biochem Soc Trans. 2008; 36: 3125. 12. Todd JA, Bell JI, McDevitt HO. HLA-DQB gene contributes to susceptibility and resistance to insulin-dependent diabetes mellitus. Nature. 1987; 329: 599604. 13. She J-X. Susceptibility to Type I diabetes: HLA-DQ and DR revisited. Immunol Today. 1996; 17: 3239. 14. Concannon P, Rich SS, Nepom GT. Genetics of Type 1A diabetes. N Engl J Med. 2009; 360: 164654. 15. Eisenbarth GS. Banting Lecture 2009: an unnished journey: molecular pathogenesis to prevention of Type 1A diabetes. Diabetes. 2010; 59: 75974. 16. Qiao Q, Osterholm AM, He B et al. A genome-wide scan for Type 1 diabetes susceptibility genes in nuclear families with multiple affected siblings in Finland. BMC Genet. 2007; 8: 84. 17. Zhang XM, Wang HY, Luo YY, Ji LN. HLA-DQ, DR allele polymorphism of Type 1 diabetes in the Chinese population: a meta-analysis. Chin Med J. 2009; 122: 9806. 18. Stayoussef M, Benmansour J, Al-Irhayim AQ et al. Autoimmune Type 1 diabetes genetic susceptibility encoded by human leukocyte antigen DRB1 and DQB1 genes in Tunisia. Clin Vaccine Immunol. 2009; 16: 1146 50.
19. Rewers M, Bugawan TL, Norris JM et al. Newborn screening for HLA markers associated with IDDM: diabetes autoimmunity study in the young (DAISY). Diabetologia. 1996; 39: 80712. 20. Kupila A, Muona P, Simell T et al. Feasibility of genetic and immunological prediction of Type I diabetes in a population-based birth cohort. Diabetologia. 2001; 44: 2907. 21. van der Auwera BJ, Schuit FC, Weets I, Ivens A, Van Autreve JE, Gorus FK. Relative and absolute HLADQA1-DQB1 linked risk for developing Type I diabetes before 40 years of age in the Belgian population: implications for future prevention studies. Hum Immunol. 2002; 63: 4050. 22. Ikegami H, Kawabata Y, Noso S, Fujisawa T, Ogihara T. Genetics of Type 1 diabetes in Asian and Caucasian populations. Diabetes Res Clin Pract. 2007; 77 (Suppl. 1): S11621. 23. Thomson G, Robinson WP, Kuhner MK et al. Genetic heterogeneity, modes of inheritance, and risk estimates for a joint study of Caucasians with insulindependent diabetes mellitus. Am J Hum Genet. 1988; 43: 799816. 24. Kawabata Y, Ikegami H, Kawaguchi Y et al. Asianspecic HLA haplotypes reveal heterogeneity of the contribution of HLA-DR and -DQ haplotypes to susceptibility to Type 1 diabetes. Diabetes. 2002; 51: 54551. 25. Barker JM, Triolo TM, Aly TA et al. Two single nucleotide polymorphisms identify the highest-risk diabetes HLA genotype: potential for rapid screening. Diabetes. 2008; 57: 31525. 26. Lavant EH, Carlson JA. A new automated human leukocyte antigen genotyping strategy to identify DRDQ risk alleles for celiac disease and Type 1 diabetes mellitus. Clin Chem Lab Med. 2009; 47: 148995. 27. Bottazzo GF, Florin-Christensen A, Doniach D. Isletcell antibodies in diabetes mellitus with autoimmune polyendocrine deciencies. Lancet. 1974; 2: 127983. 28. Baekkeskov S, Aanstoot H-J, Christgau S et al. Identication of the 64K autoantigen in insulin-dependent diabetes as the GABA-synthesizing enzyme glutamic acid decarboxylase [published erratum appears in Nature. 1990; 347: 782]. Nature. 1990; 347: 1516. 29. Achenbach P, Bonifacio E, Williams AJ, Ziegler AG, Gale EA, Bingley PJ. Autoantibodies to IA-2beta improve diabetes risk assessment in high-risk relatives. Diabetologia. 2008; 51: 48892. 30. Palmer JP, Asplin CM, Clemons P et al. Insulin antibodies in insulin-dependent diabetics before insulin treatment. Science. 1983; 222: 13379. 31. Wenzlau JM, Juhl K, Yu L et al. The cation efux transporter ZnT8 (Slc30A8) is a major autoantigen in human Type 1 diabetes. Proc Natl Acad Sci U S A. 2007; 104: 1704045.
54
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
L. ZHANG and G.S. EISENBARTH
Type 1 diabetes prediction and prevention
32. Barker JM, Barriga K, Yu L et al. Prediction of autoantibody positivity and progression to Type 1 diabetes: Diabetes Autoimmunity Study in the Young (DAISY). J Clin Endocrinol Metab. 2004; 89: 3896 902. 33. Ziegler A-G, Hummel M, Schenker M, Bonifacio E. Autoantibody appearance and risk for development of childhood diabetes in offspring of parents with Type 1 diabetes. The 2-year analysis of the German BabyDIAB study. Diabetes. 1999; 48: 4608. 34. Nejentsev S, Sjoroos M, Soukka T et al. Populationbased genetic screening for the estimation of Type 1 diabetes mellitus risk in Finland: selective genotyping of markers in the HLA-DQB1, HLA-DQA1 and HLADRB1 loci. Diabet Med. 1999; 16: 98592. 35. Kimpimaki T, Kulmala P, Savola K et al. Natural history of beta-cell autoimmunity in young children with increased genetic susceptibility to Type 1 diabetes recruited from the general population. J Clin Endocrinol Metab. 2002; 87: 45729. 36. Kimpimaki T, Kupila A, Hamalainen AM et al. The rst signs of beta-cell autoimmunity appear in infancy in genetically susceptible children from the general population: The Finnish Type 1 Diabetes Prediction and Prevention Study. J Clin Endocrinol Metab. 2001; 86: 47828. 37. LaGasse JM, Brantley MS, Leech NJ et al. Successful prospective prediction of Type 1 diabetes in schoolchildren through multiple dened autoantibodies: an 8-year follow-up of the Washington State Diabetes Prediction Study. Diabetes Care. 2002; 25: 50511. 38. Bingley PJ, Bonifacio E, Williams AJ, Genovese S, Bottazzo GF, Gale EA. Prediction of IDDM in the general population: strategies based on combinations of autoantibody markers. Diabetes. 1997; 46: 170110. 39. Orban T, Sosenko JM, Cuthbertson D et al. Pancreatic islet autoantibodies as predictors of Type 1 diabetes in the Diabetes Prevention Trial-Type 1 (DPT-1). Diabetes Care. 2009; 32: 226974. 40. Schatz D, Krischer J, Horne G et al. Islet cell antibodies predict insulin-dependent diabetes in United States school age children as powerfully as in unaffected relatives. J Clin Invest. 1994; 93: 24037. 41. Leslie RD, Atkinson MA, Notkins AL. Autoantigens IA-2 and GAD in Type I (insulin-dependent) diabetes. Diabetologia. 1999; 42: 314. 42. Morran MP, Casu A, Arena VC et al. Humoral autoimmunity against the extracellular domain of the neuroendocrine autoantigen IA-2 heightens the risk of Type 1 diabetes. Endocrinology. 2010; 151: 2528 37. 43. Hoppu S, Harkonen T, Ronkainen MS, Akerblom HK, Knip M. IA-2 antibody epitopes and isotypes during the prediabetic process in siblings of children with Type 1 diabetes. J Autoimmun. 2004; 23: 36170.
44. Makinen A, Harkonen T, Ilonen J, Knip M. Characterization of the humoral immune response to islet antigen 2 in children with newly diagnosed Type 1 diabetes. Eur J Endocrinol. 2008; 159: 1926. 45. Baekkeskov S, Nielsen JH, Marner B, Bilde T, Ludvigsson J, Lernmark A. Autoantibodies in newly diagnosed diabetic children immunoprecipitate human pancreatic islet cell proteins. Nature. 1982; 298: 1679. 46. Baekkeskov S, Landin M, Kristensen JK et al. Antibodies to a 64 000 Mr human islet cell antigen precede the clinical onset of insulin-dependent diabetes. J Clin Invest. 1987; 79: 92634. 47. Kim J, Richter W, Aanstoot HJ et al. Differential expression of GAD65 and GAD67 in human, rat, and mouse pancreatic islets. Diabetes. 1993; 42: 1799808. 48. Aanstoot HJ, Kang SM, Kim J et al. Identication and characterization of glima 38, a glycosylated islet cell membrane antigen, which together with GAD65 and IA2 marks the early phases of autoimmune response in Type 1 diabetes. J Clin Invest. 1996; 97: 277283. 49. Bingley PJ, Williams AJK, Gale EAM. Optimized autoantibody-based risk assessment in family members: implications for future intervention trials. Diabetes Care. 1999; 22: 1796801. 50. Wilkin T, Hoskins PJ, Armitage M et al. Value of insulin autoantibodies as serum markers for insulin-dependent diabetes mellitus. Lancet. 1985; 1: 4801. 51. Achenbach P, Koczwara K, Knopff A, Naserke H, Ziegler AG, Bonifacio E. Mature high-afnity immune responses to (pro)insulin anticipate the autoimmune cascade that leads to Type 1 diabetes. J Clin Invest. 2004; 114: 58997. 52. Wilkin TJ. Insulin autoantibodies as markers for Type I diabetes. Endocr Rev. 1990; 11: 92104. 53. Yu L, Robles DT, Abiru N et al. Early expression of antiinsulin autoantibodies of humans and the NOD mouse: evidence for early determination of subsequent diabetes. Proc Natl Acad Sci U S A. 2000; 97: 17016. 54. Hummel M, Bonifacio E, Schmid S, Walter M, Knopff A, Ziegler AG. Brief communication: early appearance of islet autoantibodies predicts childhood Type 1 diabetes in offspring of diabetic parents. Ann Intern Med. 2004; 140: 8826. 55. Vardi P, Ziegler AG, Matthews JH et al. Concentration of insulin autoantibodies at onset of type I diabetes. Inverse log-linear correlation with age. Diabetes Care. 1988; 11: 7369. 56. Wenzlau JM, Moua O, Sarkar SA et al. SlC30A8 is a major target of humoral autoimmunity in Type 1 diabetes and a predictive marker in prediabetes. Ann NY Acad Sci. 2008; 1150: 2569. 57. De GJ, Asanghanwa M, Nouthe B et al. Predictive power of screening for antibodies against insulinoma-associated protein 2 beta (IA-2beta) and zinc
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
55
Type 1 diabetes prediction and prevention
L. ZHANG and G.S. EISENBARTH
58.
59.
60. 61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
transporter-8 to select rst-degree relatives of Type 1 diabetic patients with risk of rapid progression to clinical onset of the disease: implications for prevention trials. Diabetologia. 2010; 53: 51724. Achenbach P, Lampasona V, Landherr U et al. Autoantibodies to zinc transporter 8 and SLC30A8 genotype stratify Type 1 diabetes risk. Diabetologia. 2009; 52: 18818. Verge CF, Gianani R, Kawasaki E et al. Number of autoantibodies (against insulin, GAD or ICA512 IA2) rather than particular autoantibody specicities determines risk of Type I diabetes. J Autoimmun. 1996; 9: 37983. Bingley PJ. Clinical applications of diabetes antibody testing. J Clin Endocrinol Metab. 2010; 95: 2533. Mahon JL, Sosenko JM, Rafkin-Mervis L et al. The TrialNet natural history study of the development of Type 1 diabetes: objectives, design, and initial results. Pediatr Diabetes. 2009; 10: 97104. Verge CF, Gianani R, Kawasaki E et al. Prediction of Type I diabetes in rst-degree relatives using a combination of insulin, GAD, and ICA512bdc IA-2 autoantibodies. Diabetes. 1996; 45: 92633. Bonifacio E, Yu L, Williams AK et al. Harmonization of glutamic acid decarboxylase and islet antigen-2 autoantibody assays for National Institute of Diabetes and Digestive and Kidney Diseases Consortia. J Clin Endocrinol Metab. 2010; 95: 33607. Pastore MR, Bazzigaluppi E, Bonfanti R et al. Twostep islet autoantibody screening for risk assessment of Type 1 diabetes in relatives. Diabetes Care. 1998; 21: 144550. Krischer JP, Cuthbertson DD, Yu L et al. Screening strategies for the identication of multiple antibodypositive relatives of individuals with Type 1 diabetes. J Clin Endocrinol Metab. 2003; 88: 1038. Karges W, Hammond-McKibben D, Cheung RK et al. Immunological aspects of nutritional diabetes prevention in NOD mice: a pilot study for the cows milk-based IDDM prevention trial. Diabetes. 1997; 46: 55764. Akerblom HK, Virtanen SM, Ilonen J et al. Dietary manipulation of beta cell autoimmunity in infants at increased risk of Type 1 diabetes: a pilot study. Diabetologia. 2005; 48: 82937. TRIGR Study Group. Study design of the Trial to Reduce IDDM in the Genetically at Risk (TRIGR). Pediatr Diabetes. 2007; 8: 11737. Luopajarvi K, Savilahti E, Virtanen SM et al. Enhanced levels of cows milk antibodies in infancy in children who develop Type 1 diabetes later in childhood. Pediatr Diabetes. 2008; 9: 43441. Achenbach P, Barker J, Bonifacio E. Modulating the natural history of Type 1 diabetes in children at high genetic risk by mucosal insulin immunization. Curr Diab Rep. 2008; 8: 8793.
71. Skyler JS, Brown D, Chase HP et al. Effects of insulin in relatives of patients with Type 1 diabetes mellitus. N Engl J Med. 2002; 346: 16851691B. 72. Bingley PJ, Gale EA. Progression to Type 1 diabetes in islet cell antibody-positive relatives in the European Nicotinamide Diabetes Intervention Trial: the role of additional immune, genetic and metabolic markers of risk. Diabetologia. 2006; 49: 88190. 73. Harrison LC, Honeyman MC, Steele CE et al. Pancreatic beta-cell function and immune responses to insulin after administration of intranasal insulin to humans at risk for Type 1 diabetes. Diabetes care. 2004; 27: 2348 55. 74. Skyler JS, Krischer JP, Wolfsdorf J et al. Effects of oral insulin in relatives of patients with Type 1 diabetes: The Diabetes Prevention Trial Type 1. Diabetes Care. 2005; 28: 106876. 75. Ludvigsson J, Faresjo M, Hjorth M et al. GAD treatment and insulin secretion in recent-onset Type 1 diabetes. N Engl J Med. 2008; 359: 190920. 76. Herold KC, Gitelman SE, Masharani U et al. A single course of anti-CD3 monoclonal antibody hOKT3{gamma}1(Ala-Ala) results in improvement in C-peptide responses and clinical parameters for at least 2 years after onset of Type 1 diabetes. Diabetes. 2005; 54: 17639. 77. Keymeulen B, Vandemeulebroucke E, Ziegler AG et al. Insulin needs after CD3-antibody therapy in new-onset Type 1 diabetes. N Engl J Med. 2005; 352: 2598608. 78. Keymeulen B, Walter M, Mathieu C et al. Four-year metabolic outcome of a randomised controlled CD3antibody trial in recent-onset Type 1 diabetic patients depends on their age and baseline residual beta cell mass. Diabetologia. 2010; 53: 61423. 79. Zhang B. Ofatumumab. MAbs. 2009; 1: 32631. 80. Robak T. Ofatumumab, a human monoclonal antibody for lymphoid malignancies and autoimmune disorders. Curr Opin Mol Ther. 2008; 10: 294309. 81. Hu CY, Rodriguez-Pinto D, Du W et al. Treatment with CD20-specic antibody prevents and reverses autoimmune diabetes in mice. J Clin Invest. 2007; 117: 385767. 82. Hu C, Deng S, Wong FS, Wen L. Anti-CD20 treatment prolongs syngeneic islet graft survival and delays the onset of recurrent autoimmune diabetes. Ann N Y Acad Sci. 2008; 1150: 2179. 83. Pescovitz MD, Greenbaum CJ, Krause-Steinrauf H et al. Rituximab, B-lymphocyte depletion, and preservation of beta-cell function. N Engl J Med. 2009; 361: 214352. 84. Maniatis AK, Yu L, Miao D, Nelson K, Eisenbarth GS. Rapid assays for detection of anti-islet autoantibodies: implications for organ donor screening. J Autoimmun. 2001; 16: 716. 85. Gianani R, Putnam A, Still T et al. Initial results of screening of nondiabetic organ donors for expression of
56
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
L. ZHANG and G.S. EISENBARTH
Type 1 diabetes prediction and prevention
islet autoantibodies. J Clin Endocrinol Metab. 2006; 91: 185561. 86. Schlosser M, Mueller PW, Torn C, Bonifacio E, Bingley PJ. Diabetes Antibody Standardization Program: evaluation of assays for insulin autoantibodies. Diabetologia. 2010; 53: 261120. 87. Triolo TM, Chase HP, Barker JM. Diabetic subjects diagnosed through the Diabetes Prevention TrialType 1 (DPT-1) are often asymptomatic with normal A1C at diabetes onset. Diabetes Care. 2009; 32: 769 73. 88. Cernea S, Herold KC. Monitoring of antigen-specic CD8 T cells in patients with Type 1 diabetes treated
with antiCD3 monoclonal antibodies. Clin Immunol. 2010; 134: 1219. 89. Herold KC, Gitelman S, Greenbaum C et al. Treatment of patients with new onset Type 1 diabetes with a single course of anti-CD3 mAb teplizumab preserves insulin production for up to 5 years. Clin Immunol. 2009; 132: 16673. 90. von Herrath M. Combination therapies for Type 1 diabetes: why not now? Immunotherapy. 2010; 2: 289 91. 91. Boettler T, von Herrath M. Immunotherapy of Type 1 diabetes: how to rationally prioritize combination therapies in T1D. Int Immunopharmacol. 2010; 10: 14915.
2011 Ruijin Hospital, Shanghai Jiaotong University School of Medicine and Blackwell Publishing Asia Pty Ltd
57
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Starship Troopers Skinnies Army BookDocument66 pagesStarship Troopers Skinnies Army BookDougBirtles100% (5)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Biology of Implant OsseointegrationDocument11 pagesBiology of Implant OsseointegrationAmIrNo ratings yet
- Stress BreakerDocument7 pagesStress BreakerEshan Verma33% (3)
- Biology Investigatory ProjectDocument17 pagesBiology Investigatory ProjectAnmol Dhungel100% (6)
- Turbidimetry and Nephelometry1Document3 pagesTurbidimetry and Nephelometry1maxim_crank6101100% (1)
- Pain PathwayDocument17 pagesPain PathwaySalsabila Al-BasheerNo ratings yet
- COT TRF Science G8 - Food ChainDocument8 pagesCOT TRF Science G8 - Food ChainRAMIR BECOYNo ratings yet
- Antibiotic Prophylaxis in Surgery PDFDocument74 pagesAntibiotic Prophylaxis in Surgery PDFHugo GuadarramaNo ratings yet
- 11 BPHDocument59 pages11 BPHبدرول هشام100% (1)
- ACG Guideline GERD March 2013 Plus CorrigendumDocument22 pagesACG Guideline GERD March 2013 Plus Corrigendumdwifit3No ratings yet
- Ostitis Media - PnemoniaDocument7 pagesOstitis Media - Pnemoniadwifit3No ratings yet
- 11 BPHDocument59 pages11 BPHبدرول هشام100% (1)
- HPLC Triterpenes Centella AsiaticaDocument3 pagesHPLC Triterpenes Centella Asiaticadwifit3No ratings yet
- Alprazolam With Other Anxiety DrugDocument14 pagesAlprazolam With Other Anxiety Drugdwifit3No ratings yet
- Centella Type 1 and 2Document9 pagesCentella Type 1 and 2dwifit3No ratings yet
- Plant For Skin ConditionDocument6 pagesPlant For Skin Conditiondwifit3No ratings yet
- Genomic Diversity of The Human Intestinal Parasite Entamoeba HistolyticaDocument13 pagesGenomic Diversity of The Human Intestinal Parasite Entamoeba Histolyticadwifit3No ratings yet
- Genomic Diversity of The Human Intestinal Parasite Entamoeba HistolyticaDocument13 pagesGenomic Diversity of The Human Intestinal Parasite Entamoeba Histolyticadwifit3No ratings yet
- Jurnal 1Document5 pagesJurnal 1dwifit3No ratings yet
- Equitable System of Health Workers in Indonesia: (Essay)Document3 pagesEquitable System of Health Workers in Indonesia: (Essay)dwifit3No ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaAdnanNo ratings yet
- Short Periods of Incubation During Egg Storage - SPIDESDocument11 pagesShort Periods of Incubation During Egg Storage - SPIDESPravin SamyNo ratings yet
- Molecular Genetics of Colorectal Cancer - UpToDateDocument41 pagesMolecular Genetics of Colorectal Cancer - UpToDateToweran ToweraneNo ratings yet
- JCM 08 00217 v3Document23 pagesJCM 08 00217 v3Sumit BediNo ratings yet
- Ap Environmental Science Free-Response QuestionsDocument6 pagesAp Environmental Science Free-Response Questionsapi-234419767No ratings yet
- Paul Atriedes (PL 6/181pp) : Bene Gesserit Training (Container, Active 11)Document2 pagesPaul Atriedes (PL 6/181pp) : Bene Gesserit Training (Container, Active 11)dfgdfNo ratings yet
- Pemphigus Subtypes Clinical Features Diagnosis andDocument23 pagesPemphigus Subtypes Clinical Features Diagnosis andAnonymous bdFllrgorzNo ratings yet
- 03 Chapter 3Document148 pages03 Chapter 3arghaNo ratings yet
- Food Chain QsDocument3 pagesFood Chain QsOliver SansumNo ratings yet
- Follicular Dynamics in Bovine and Ovine 1Document19 pagesFollicular Dynamics in Bovine and Ovine 1israr yousafNo ratings yet
- 1.4 - Diffusion and Osmosis - CrosswordPuzzleDocument1 page1.4 - Diffusion and Osmosis - CrosswordPuzzlemmssthNo ratings yet
- Sickle Cell AnemiaDocument7 pagesSickle Cell AnemiaJuma AwarNo ratings yet
- Lesson 7 - Organ TransplantationDocument14 pagesLesson 7 - Organ TransplantationJosee100% (1)
- Plant Transport - IGCSE Biology Notes (2020)Document6 pagesPlant Transport - IGCSE Biology Notes (2020)Zhi En LeeNo ratings yet
- MR Spectroscopy: Technical Aspects and Clinical ApplicationsDocument5 pagesMR Spectroscopy: Technical Aspects and Clinical ApplicationsNotariana Kusuma ANo ratings yet
- Analisis Kualitatif Dan Kuantitatif Kandungan Kimia Dari Ekstrak Heksan, Aseton, Etanol Dan Air Dari Umbi Bawang Putih (Allium Sativum Linn.)Document11 pagesAnalisis Kualitatif Dan Kuantitatif Kandungan Kimia Dari Ekstrak Heksan, Aseton, Etanol Dan Air Dari Umbi Bawang Putih (Allium Sativum Linn.)Tari PratiwiNo ratings yet
- Young Children's Biological Predisposition To Learn in Privileged DomainDocument6 pagesYoung Children's Biological Predisposition To Learn in Privileged DomainVeronica Dadal0% (1)
- Brigitte King - InformativeDocument2 pagesBrigitte King - Informativeapi-262025468No ratings yet
- Ssac 2104Document100 pagesSsac 2104Amrutha amrNo ratings yet
- Presented By:-Dr. Sushma Tomar Associate Professor Department of AnatomyDocument20 pagesPresented By:-Dr. Sushma Tomar Associate Professor Department of AnatomyCristine EchaveNo ratings yet
- 2nd Periodic Test (Science)Document1 page2nd Periodic Test (Science)mosarbas0950% (2)
- Checkerboard Microdilution AssayDocument5 pagesCheckerboard Microdilution AssayClaudio Luis Venturini0% (1)
- 2 Part 1Document99 pages2 Part 1m_luchianNo ratings yet