Professional Documents
Culture Documents
Abdominal Pain
Uploaded by
salamredOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abdominal Pain
Uploaded by
salamredCopyright:
Available Formats
Abdominal Pain Kurt A. Brown M.D. Database DEFINITION Abdominal pain is a frequent complaint in the pediatric age group.
Pain may be acute or chronic, focal, or nonspecific. A child's complaint of abdominal pain can originate from gastrointestinal (GI) and non-GI causes but also commonly can be the manifestation of referred pain from extraabdominal sites. Differential Diagnosis CONGENITAL/ANATOMIC Incarcerated hernia Intestinal adhesions
Intussusception Malrotation with volvulus Ovarian torsion Testicular torsion Uteropelvic junction obstruction
INFECTIOUS Cystitis and urinary tract infections Fitz-Hugh-Curtis syndrome
Gastroenteritis (bacterial, viral, or parasitic) Helicobacter pylori gastritis Mononucleosis with splenic enlargement/rupture Otitis media Pharyngitis Pelvic inflammatory disease Peritonitis Pneumonia Psoas abscess Sepsis Tuboovarian abscess Varicella
TOXIC, ENVIRONMENTAL DRUGS Anticholinergic drugs Caustic ingestions
Intestinal foreign body
Heavy metal (i.e., lead) ingestion Mushroom poisoning Sympathomimetic drugs
TRAUMA Child abuse Duodenal hematoma
Perforated viscus Splenic hematoma/rupture
TUMOR Any tumor, benign or malignant, leading to viscous obstruction Leukemia
Lymphoma Nephroblastoma Wilms tumor
GENETIC/METABOLIC Diabetic ketoacidosis ALLERGIC/INFLAMMATORY Appendicitis Cholecystitis
Eosinophilic gastroenteritis Hemolytic-uremic syndrome Henloch-Schonlein purpura Hepatitis Inflammatory bowel disease Mesenteric adenitis Necrotizing enterocolitis Pancreatitis Peptic ulcer or gastritis Esophagitis or duodenitis
FUNCTIONAL Depression Functional abdominal pain
Malingering
Munchausen syndrome (+/- by proxy)
MISCELLANEOUS Abdominal migraine Cholelithiasis
Colic Constipation Dysmenorrhea Ectopic pregnancy Endometriosis Ileus Intestinal pseudoobstruction Irritable bowel syndrome Lactose intolerance Mittelschmerz Nephrolithiasis Ovarian cyst Pregnancy Porphyria Sickle-cell disease Typhlitis
Approach to the Patient GENERAL GOALS One must decide if abdominal pain complaints require emergent, urgent, or nonimmediate intervention. Phase 1: Careful and complete history and physical examination to narrow this extensive DDx.
Phase 2: Directed laboratory evaluations should be made to support more likely portions of the DDx. If a narrowed differential is difficult to formulate, every effort should be made to assure that the patient is clinically stable. A limited blood and/or radiographic evaluation screening with: CBC ESR Comprehensive metabolic panel (i.e., Na+, K+, Cl, CO2, BUN, Creatinine, glucose, total protein, albumin, ALT, Uric acid, LDH)
Abdominal x-ray for significant abnormalities could be made to ensure there are no significant abnormalities above one's clinical suspicion. Phase 3: Institute appropriate therapy related to diagnosis.
P.5 Data Gathering HISTORY Question: Location of pain? Significance: Pain etiology. See Table 2. Question: Duration of pain? Significance: Acute versus chronic illness Question: Onset and progression of symptoms? Significance: Evolution of painful process Question: Frank hematochezia? Significance: Colonic bleeding or massive upper GI bleeding Question: Abdominal distension? Significance: Distension of an abdominal viscus by air, stool, or fluid Question: Radiation of pain? Significance: Certain entities characteristically have radiation of pain (i.e., pancreatitis to the back, appendicitis to the right lower quadrant) Question: Pain relieved by bowel movements? Significance: Etiology may be related to colonic distension (by air or stool) or inflammation (colitis) Question: Bowel movement pattern, decrease in frequency or change in caliber? Significance: Constipation Question: Relationship to emesis Significance: Usually upper intestinal tract disorders Physical Examination Finding: Location of pain Significance: See Table 2.
Finding: Reexamination by the same healthcare provider for changing characteristics Significance: Evolution of abdominal process Finding: Rebound tenderness Significance: Peritonitis and the potential need for surgical intervention Finding: Rectal examination Significance: Peritoneal irritation, further localization of pain, masses, presence and consistency of stool, and/or occult heme Laboratory Aids Test: CBC with differential
Significance: Total white count is nonspecific and may be a poor indicator of intestinal inflammation Test: ESR Significance: Nonspecific indicator of systemic inflammation Test: Urinalysis Significance: General screen for urinary tract abnormalities Test: Two position abdominal x-ray Significance: Possible clue to ileus, intussusception, intestinal obstruction, retained feces or gas
Emergency Care Every effort should be made to ensure that the patient is clinically stable. Frequent evaluation of vital signs and physical examination are a means of assessing evolving pain and ensuring that the patient is well enough for potential discharge. ISSUES FOR REFERRAL Persistent abdominal pain without clear etiology or chronic gastrointestinal diseases should be referred to a pediatric gastroenterologist. CLINICAL PEARLS The farther the complaint of pain is away from the periumbilical region, the more likely the pain etiology represents organic disease. True nighttime waking with pain is more often correlated with organic disease than functional pain.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Chronic DiarrheaDocument6 pagesChronic DiarrheasalamredNo ratings yet
- MCQ On MenopauseDocument4 pagesMCQ On Menopausesalamred100% (3)
- ةعومجم نم لا Reports ةيطغم جهنملا ءاشنا لا مكبجعت: Report of toxicologyDocument14 pagesةعومجم نم لا Reports ةيطغم جهنملا ءاشنا لا مكبجعت: Report of toxicologysalamredNo ratings yet
- MCQ Net 3Document5 pagesMCQ Net 3salamredNo ratings yet
- 33Document7 pages33salamred100% (1)
- HemoptysisDocument3 pagesHemoptysissalamredNo ratings yet
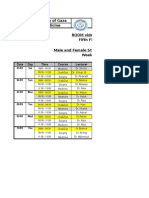
- Islamic University of Gaza Faculty of Medicine ROOM Video Conf. Fifth Floor Male and Female Students - 6th Year Week 1Document2 pagesIslamic University of Gaza Faculty of Medicine ROOM Video Conf. Fifth Floor Male and Female Students - 6th Year Week 1salamredNo ratings yet
- Ortho OSCE 2008Document3 pagesOrtho OSCE 2008salamredNo ratings yet
- Psychiatry Final Exam 2014Document2 pagesPsychiatry Final Exam 2014Ibrahem Y. NajjarNo ratings yet
- Solutions To The Test CasesDocument11 pagesSolutions To The Test CasessalamredNo ratings yet
- MCQs Psy Exam44 First GroupDocument7 pagesMCQs Psy Exam44 First Groupsalamred100% (3)
- MCQs Psy Exam44 First GroupDocument7 pagesMCQs Psy Exam44 First Groupsalamred100% (3)
- MCQ Psy Exam Group BDocument17 pagesMCQ Psy Exam Group BsalamredNo ratings yet
- امتحان الاشعة العملي النهائيDocument1 pageامتحان الاشعة العملي النهائيsalamredNo ratings yet
- MSQU Course MontadaDocument39 pagesMSQU Course MontadasalamredNo ratings yet
- RadiologyDocument5 pagesRadiologysalamredNo ratings yet
- اسبيرو طويل مهم جدا الثلاثاءDocument22 pagesاسبيرو طويل مهم جدا الثلاثاءsalamredNo ratings yet
- Longitudinal Esophagotomy (Hellers) 4 Frey"s Syndrome: Sever InfectionDocument4 pagesLongitudinal Esophagotomy (Hellers) 4 Frey"s Syndrome: Sever InfectionsalamredNo ratings yet
- 333Document13 pages333salamredNo ratings yet
- 6th Year Surgery Final ExamDocument21 pages6th Year Surgery Final Examlinaleen67% (3)
- Choose The Best Appropriate Answerfor Each of The Following QuestionsDocument12 pagesChoose The Best Appropriate Answerfor Each of The Following QuestionssalamredNo ratings yet
- The Answer KeyDocument1 pageThe Answer KeysalamredNo ratings yet
- PMC Exam 2006Document27 pagesPMC Exam 2006salamredNo ratings yet
- SurgeryDocument10 pagesSurgeryIbrahem Y. NajjarNo ratings yet
- breastطباعةDocument3 pagesbreastطباعةsalamredNo ratings yet
- A) Basic Surgical SciencesDocument27 pagesA) Basic Surgical SciencessalamredNo ratings yet
- Choose The Best Appropriate Answerfor Each of The Following QuestionsDocument12 pagesChoose The Best Appropriate Answerfor Each of The Following QuestionssalamredNo ratings yet
- MCQDocument11 pagesMCQsalamredNo ratings yet
- A) Basic Surgical SciencesDocument27 pagesA) Basic Surgical SciencessalamredNo ratings yet
- Dr:-Ashraf .I. ObaidDocument22 pagesDr:-Ashraf .I. ObaidsalamredNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Honda IzyDocument16 pagesHonda IzyTerry FordNo ratings yet
- Stonehell Dungeon 1 Down Night Haunted Halls (LL)Document138 pagesStonehell Dungeon 1 Down Night Haunted Halls (LL)some dude100% (9)
- Internship Format HRMI620Document4 pagesInternship Format HRMI620nimra tariqNo ratings yet
- CAREDocument11 pagesCARELuis SementeNo ratings yet
- [18476228 - Organization, Technology and Management in Construction_ an International Journal] Adaptive Reuse_ an Innovative Approach for Generating Sustainable Values for Historic Buildings in Developing CountriesDocument15 pages[18476228 - Organization, Technology and Management in Construction_ an International Journal] Adaptive Reuse_ an Innovative Approach for Generating Sustainable Values for Historic Buildings in Developing Countrieslohithsarath bethalaNo ratings yet
- Guided-Discovery Learning Strategy and Senior School Students Performance in Mathematics in Ejigbo, NigeriaDocument9 pagesGuided-Discovery Learning Strategy and Senior School Students Performance in Mathematics in Ejigbo, NigeriaAlexander DeckerNo ratings yet
- Java Complete Collection FrameworkDocument28 pagesJava Complete Collection FrameworkkhushivanshNo ratings yet
- E-Mobility and SafetyDocument77 pagesE-Mobility and SafetySantosh KumarNo ratings yet
- Just in Time and TQMDocument8 pagesJust in Time and TQMBhramadhathNo ratings yet
- Paul Spicker - The Welfare State A General TheoryDocument162 pagesPaul Spicker - The Welfare State A General TheoryTista ArumNo ratings yet
- KCG-2001I Service ManualDocument5 pagesKCG-2001I Service ManualPatrick BouffardNo ratings yet
- Chapter 20 AP QuestionsDocument6 pagesChapter 20 AP QuestionsflorenciashuraNo ratings yet
- Tài Liệu Hướng Dẫn Cài Đặt Rơ Le MPS 3000Document55 pagesTài Liệu Hướng Dẫn Cài Đặt Rơ Le MPS 3000nguyenquangtonNo ratings yet
- ST3 ManualDocument48 pagesST3 ManualRon FosterNo ratings yet
- Rights of Parents in IslamDocument11 pagesRights of Parents in Islamstoneage989100% (2)
- De Thi Chon Hoc Sinh Gioi Cap Tinh Mon Tieng Anh Lop 12 So GD DT Thanh Hoa Nam Hoc 2015 2016Document11 pagesDe Thi Chon Hoc Sinh Gioi Cap Tinh Mon Tieng Anh Lop 12 So GD DT Thanh Hoa Nam Hoc 2015 2016Thuy LinggNo ratings yet
- Spare Part PhilosophyDocument27 pagesSpare Part Philosophyavaisharma50% (2)
- WBCS 2023 Preli - Booklet CDocument8 pagesWBCS 2023 Preli - Booklet CSurajit DasNo ratings yet
- Extract The .Msi FilesDocument2 pagesExtract The .Msi FilesvladimirNo ratings yet
- The Rock Reliefs of Ancient IranAuthor (Document34 pagesThe Rock Reliefs of Ancient IranAuthor (mark_schwartz_41No ratings yet
- Ancient Sumer Flip BookDocument9 pagesAncient Sumer Flip Bookapi-198624210No ratings yet
- I Pmtea 2020 HandoutDocument94 pagesI Pmtea 2020 HandoutAbhijeet Dutta100% (1)
- Toshiba MotorsDocument16 pagesToshiba MotorsSergio Cabrera100% (1)
- Bossypants Autobiography and Womens SelvesDocument26 pagesBossypants Autobiography and Womens SelvesCamila Paz GutiérrezNo ratings yet
- SavannahHarbor5R Restoration Plan 11 10 2015Document119 pagesSavannahHarbor5R Restoration Plan 11 10 2015siamak dadashzadeNo ratings yet
- Quanta To QuarksDocument32 pagesQuanta To QuarksDaniel Bu100% (5)
- Omnitron CatalogDocument180 pagesOmnitron Catalogjamal AlawsuNo ratings yet
- Chapter 2.3.3 History of Visual Arts Modernism Post ModernismDocument17 pagesChapter 2.3.3 History of Visual Arts Modernism Post ModernismKim Ashley SarmientoNo ratings yet
- DNA Vs RNA - Introduction and Differences Between DNA and RNADocument10 pagesDNA Vs RNA - Introduction and Differences Between DNA and RNAKienlevyNo ratings yet
- Philhis 1blm Group 6 ReportDocument19 pagesPhilhis 1blm Group 6 Reporttaehyung trashNo ratings yet







































































![[18476228 - Organization, Technology and Management in Construction_ an International Journal] Adaptive Reuse_ an Innovative Approach for Generating Sustainable Values for Historic Buildings in Developing Countries](https://imgv2-1-f.scribdassets.com/img/document/422064728/149x198/344a5742a7/1565947342?v=1)
























