Professional Documents
Culture Documents
Chapter 38 - Pediatric and Geriatric Hematology
Uploaded by
Nathaniel SimOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 38 - Pediatric and Geriatric Hematology
Uploaded by
Nathaniel SimCopyright:
Available Formats
1 Chapter 17 Pediatric and Geriatric Hematology PEDIATRIC HEMATOLOGY Dramatic changes occurs in the blood and bone marrow
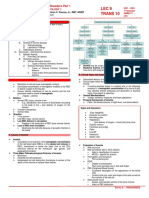
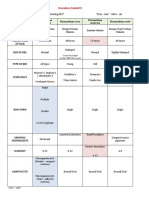
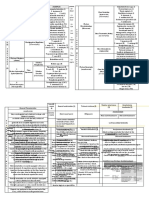
ow of the newborn infant during the first hours and days after birth, and there are rapid fluctuations in the quantities of hematologic elements Significant hematologic differences are seen between term and preterm infants and among newborns, infants, young children, and older children Prenatal Hematopoiesis Begins in the first weeks of embryonic development Three phases of development: a) Mesoblastic (yolk sac) b) Hepatic (liver) c) Myeloid (bone marrow) First cells produced in the developing embryo are primitive erythroblasts formed in the yolk sac By the second month of gestation, hematopoiesis ceases in the yolk sac, and the liver becomes the center for hematopoiesis, reaching its peak activity during the third and fourth gestational month During the fourth and fifth gestational months, the bone marrow emerges as a major site of blood cell production, and it becomes the primary site by birth Hematopoiesis of the New Born Active bone marrow is referred to as the red marrow Inactive fatty bone marrow is referred to as the yellow marrow In a full term infant, hepatic hematopoiesis has ceased and continues to develop in the bone marrow Postembryonic extramedullary hematopoiesis is abnormal in a full term infant In a premature infant, the center of activity of hematopoiesis are frequently seen in the liver and occasionally observed in the spleen, lymph nodes or thymus Pediatric Developmental Stages Neonatal period: first 4 weeks of life Infancy: first year of life Childhood: age 1 to puberty(8 to 12yo) Pediatric patients has higher normal values on hematologic test NRBC are usually found on peripheral blood smears of babies Gestational Age Full term: 37 to 42 weeks Premature or preterm: less than 37 weeks Postterm: 42 weeks Low birth weight (micropreemies): 24 to 26 weeks Birth Weight Classification Appropriate size for gestational age Small for gestational age (2.5 kg or less) Very low birth weight (1.5 kg or less) Extremely low birth weight (0.5 kg or less) Large for gestational age (4kg or more) Red Blood Cell Values at Birth Neonatal hematologic values are affected by the gestational age of the infant, the age in hours after delivery, the presence of illness and the level of support required The presence of fetal hemoglobin (HbF), bilirubin, and lipids in newborn can also interfere with hematology testing Red Blood Cell Count RBC count is increased during the 1st 24 hours of life, and remains steady for 2 weeks, then slowly declines, this is called polycythemia of the newborn Polycythemia of the newborn can be explained by in utero hypoxia Physiologic anemia is seen in 5 to 8 weeks of life
2 RBC reaches its lowest count at 7 weeks of age Hemoglobin reaches its lowest concentration at 9 weeks of age Erythrocyte Morphology of the Neonate Erythrocyte remains macrocytic from the first 11 weeks of gestation until day 5 of postnatal life Orthochromic normoblasts frequently are observed in the full term infant on the first day of life but disappear within postnatal days 3 to 5 NRBC may persist longer than a week in immature infants Average number of NRBCs ranges from 3 to 10 per 100 WBCs in a normal full term infant to 25 NRBCs per 100 WBCs in a premature infant The presence of NRBCs for more than 5 days suggests hemolysis, hypoxic stress or acute infection Additional erythrocytic differences (biconcave disk relative to stomatocytes): a) Neonates (43% disk, 40% stomatocytes) b) Adults (78% disk, 18% stomatocytes) c) Premature infants (40% disk, 30% stomatocytes, 27% additional poikilocytes) Reticulocyte Count 90% reticulocytes during 12 weeks of gestation 15% reticulocytes during 6 months gestation 4% to 6% reticulocytes at birth Reticulocytosis persist for 3 days after birth, then declines abruptly to 0.8% reticulocytes on postnatal day 4 to 7 At 2 months the number of reticulocytes increase slightly, followed by a slight decline from 3 months to 2 years, when adult levels of 0.5% to 1.5% are attained Reticulocyte count of premature infants is typically higher that that of term infants Significant polychromasia is indicative of postnatal Reticulocytosis Hemoglobin Full Term Infants At birth HbF constitutes 70% to 80% of the total hemoglobin HbF declines from (90% - 95%) at 30 weeks to 7% at 12 weeks after birth HbF stabilizes at 3.2 + 2.1% at 16 to 20 weeks after birth The switch from HbF to HbA is genetically controlled and determined by gestational age Capillary samples from new born have higher hemoglobin concentration than venous samples, which can be attributed to circulatory factors The average Hb for a full term infant at birth is 16.5 to 12.5 g/dl Less than 14 g/dl are considered abnormal for full term infants Average Hb value for a preterm infant who is small for gestational age is 17.1 g/dl Hb values less than 13.7 g/dl is considered abnormal for preterm infants Physiologic Anemia for Neonate Hb concentration of term infants decreases during the first 5 to 8 weeks of life, a condition known as physiologic anemia od infancy Infants born prematurely also experience a decrease in Hb concentration, which is termed physiologic anemia of prematurity Contributing to the physiologic anemia is the shortened life span of the fetal RBC Chromium labeled newborn RBCs estimate a survival time of 60 to 70 days Life span of RBCs in premature infants is about 35 to 50 days The more immature the infant, the greater the degree of reduction Hemodilution related to the increased blood volume that accompanies the
3 rapid weight gain can be seen in the first few months of life is not thought to paly a key role in anemia Hb levels of premature infants are typically 1g/dl or more bellow the values of full term infants Very low weight infants show a progressive decline in Hb, RBC count, MCV, MCH, MCHC, and have a slower recovery than other preterm and term infants Hematocrit The average Hct at birth for full term infants is 53% Newborn with increased Hct, especially values greater than 65% experience hyperviscousity of the blood Hct increases approximately 5% during the first 48 postnatal hours followed by a slow linear decline to 46% to 62% at 2 weeks and 32% to 51% between the second and fourth months Normal adult values of 47% (males) and 42% (females) are achieved during adolescence Very low birth weight preterm infants are frequently anemic at birth Red Blood Cell Indices Mean Cell Volume Erythrocytes of newborn infants are marked macrocytic at birth Average MCV for full term infants is 110 + 15 fL A sharp decrease occurs during the first 24 hours of life MCV continues to decrease to 90 + 12fL in 3 to 4 months The more premature the infant, the higher the MCV A newborn with an MCV of less than 94 fL should be evaluated for a-thalassemia or iron deficiency Mean Cell Hemoglobin MCV is 30 to 42 pg in healthy neonates MCV is 27 to 41 pg in premature infants Mean Cell Hemoglobin Concentration Average MCHC is 33 g/dl for infants and adults Red Blood Cell Distribution Width RDW is markedly elevated in newborns, with a range of 14.2% to 19.9% in the first 30 days of life then it gradually decreases and reaches normal adult levels in 6 months Anemia in Infants and Children Iron Deficiency Anemia Most common pediatric hematologic disorder Most frequent cause of anemia on childhood Prevalence is still 2% in toddlers 1 to 2 years of age and 3% in children 3 to 5 days of age Ancillary Tests for Anemia in Infants and Children Haptoglobulin level is low as to be undetected in neonates Transferrin levels are also low in neonates, increasing rapidly after birth and reaching normal adult values in 6 months Serum ferritin and serum iron are high at birth, rise during the first month, drop to their lowest level between 6 months and 4 years of age and remain low through out childhood White Blood Cell Values in the Newborn
You might also like
- Vitamin B12 and FolateDocument12 pagesVitamin B12 and FolateAllessandria DimaggioNo ratings yet
- Enzymes: Concentration, Kinetics, Classification, AssaysDocument13 pagesEnzymes: Concentration, Kinetics, Classification, AssaysAedren TrillanaNo ratings yet
- Aubf Lec - Serous FluidDocument12 pagesAubf Lec - Serous FluidColene MoresNo ratings yet
- (MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Document6 pages(MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)Aisle Malibiran PalerNo ratings yet
- Nemtodes BelizarioDocument7 pagesNemtodes BelizarioMarl EstradaNo ratings yet
- MICROBIOLOGY MEDIADocument3 pagesMICROBIOLOGY MEDIAAisle Malibiran PalerNo ratings yet
- Biochemical - TestsDocument5 pagesBiochemical - TestsMohsen Haleem100% (1)
- Clinical Microscopy Services PDFDocument5 pagesClinical Microscopy Services PDFNaima AmrosiNo ratings yet
- AUBF Finals Vaginal SecretionsDocument37 pagesAUBF Finals Vaginal SecretionsLyra Dennise LlidoNo ratings yet
- Aubf Case Study AbcdefDocument9 pagesAubf Case Study AbcdefChiara Kate CodillaNo ratings yet
- Diagnostic Microbiology - : University of Santo Tomas - Medical TechnologyDocument6 pagesDiagnostic Microbiology - : University of Santo Tomas - Medical TechnologyWynlor AbarcaNo ratings yet
- Red Blood Cell Disorders Part 1Document6 pagesRed Blood Cell Disorders Part 1Claire GonoNo ratings yet
- Understanding Reed-Sternberg Cells and Hodgkin LymphomaDocument9 pagesUnderstanding Reed-Sternberg Cells and Hodgkin LymphomaNico LokoNo ratings yet
- Christian Villahermosa March 4, 2021: Philippine HIV and AIDS Policy ActDocument14 pagesChristian Villahermosa March 4, 2021: Philippine HIV and AIDS Policy ActvenusNo ratings yet
- Clinical Microscopy (Fecalysis)Document2 pagesClinical Microscopy (Fecalysis)Sheng Ramos AglugubNo ratings yet
- Compre-Quiz For MedtechDocument18 pagesCompre-Quiz For MedtechynaellyNo ratings yet
- Parasitology Lecture OverviewDocument17 pagesParasitology Lecture Overviewlouie100% (1)
- Aubf Quiz 2Document8 pagesAubf Quiz 2Gene Narune GaronitaNo ratings yet
- Worksheet #3 Differential White Blood Cell CountDocument5 pagesWorksheet #3 Differential White Blood Cell CountROMAH JANE MENDOZANo ratings yet
- Reviewbasic 130709233435 Phpapp02Document130 pagesReviewbasic 130709233435 Phpapp02Andi Namirah100% (1)
- Clinical Microscopy ReviewerDocument7 pagesClinical Microscopy ReviewerDayledaniel SorvetoNo ratings yet
- Chemical Examination of UrineDocument6 pagesChemical Examination of UrinehermanskyNo ratings yet
- Table of Histopath Stains # 1Document3 pagesTable of Histopath Stains # 1Lou Vernadel ApolloNo ratings yet
- Analysis of Urine and Other Body FluidsDocument52 pagesAnalysis of Urine and Other Body FluidsJoseph VillamorNo ratings yet
- General Approach in Investigation of Haemostasis: Lecture 2: Bleeding TimeDocument28 pagesGeneral Approach in Investigation of Haemostasis: Lecture 2: Bleeding TimeClorence John Yumul FerrerNo ratings yet
- Parasitology ReviewersDocument9 pagesParasitology ReviewersLouije MombzNo ratings yet
- MEDT 19 (Lec)Document17 pagesMEDT 19 (Lec)Erick PanganibanNo ratings yet
- AUBF Notes 1Document9 pagesAUBF Notes 1ChiNo ratings yet
- AUBF P1 Examination Questions (1-8Document39 pagesAUBF P1 Examination Questions (1-8Charmaine BoloNo ratings yet
- ISBB Aaaaa PDFDocument55 pagesISBB Aaaaa PDFSelena de LimaNo ratings yet
- Malarial ParasitesDocument5 pagesMalarial ParasitesZette ArañaNo ratings yet
- Faults Occurring During TrimmingDocument4 pagesFaults Occurring During TrimmingMary Christelle100% (3)
- 1.entamoeba Histolytica - Is The Major Pathogen in This GroupDocument14 pages1.entamoeba Histolytica - Is The Major Pathogen in This GroupJoseph De JoyaNo ratings yet
- Alvine Discharge DiseasesDocument1 pageAlvine Discharge DiseasesApril Rose AlivioNo ratings yet
- Physical Examination of UrineDocument4 pagesPhysical Examination of UrineIceNo ratings yet
- UAReview Landis 2017 Rev1Document17 pagesUAReview Landis 2017 Rev1Dayledaniel SorvetoNo ratings yet
- Mtap2 Bacte 1Document27 pagesMtap2 Bacte 1DENISE MARA�ANo ratings yet
- Examination of Urine Formation and CompositionDocument7 pagesExamination of Urine Formation and CompositionDaniel LamasonNo ratings yet
- HTMLE SEMINAR NOTES DOC. ORTEGA - CompressedDocument35 pagesHTMLE SEMINAR NOTES DOC. ORTEGA - CompressedNISSI JUNE T. UNGABNo ratings yet
- Crystal Appearance/Characteristics Clinical SignificanceDocument4 pagesCrystal Appearance/Characteristics Clinical SignificanceAngela LaglivaNo ratings yet
- BSC Licensure Sample QuestionsDocument144 pagesBSC Licensure Sample QuestionsSAMMY0% (1)
- Abnormal Pedia ReviewerDocument6 pagesAbnormal Pedia ReviewerMarwin OditaNo ratings yet
- A. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)Document19 pagesA. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)IceNo ratings yet
- Concentration Techniques for Parasite DetectionDocument18 pagesConcentration Techniques for Parasite DetectionJackie Lind Talosig100% (4)
- Non-Enteric Gastrointestinal PathogensDocument11 pagesNon-Enteric Gastrointestinal PathogensOrhan AsdfghjklNo ratings yet
- Lipids: DDC Medical Laboratory Science DepartmentDocument48 pagesLipids: DDC Medical Laboratory Science DepartmentMelody PardilloNo ratings yet
- SubcutaneousDocument2 pagesSubcutaneousMary ChristelleNo ratings yet
- Intrinsic RBC DisordersDocument4 pagesIntrinsic RBC DisordersMartin ClydeNo ratings yet
- Lab Evaluation of PlateletsDocument5 pagesLab Evaluation of PlateletsDennis ValdezNo ratings yet
- Serological TestsDocument2 pagesSerological TestsKimberly EspaldonNo ratings yet
- NEMATODES NotesDocument34 pagesNEMATODES NotesbebibobuNo ratings yet
- Anti-Anemia and Hematopoietic Growth FactorsDocument8 pagesAnti-Anemia and Hematopoietic Growth FactorsIsabel CastilloNo ratings yet
- SpirochetesDocument30 pagesSpirochetesDaniel AtiehNo ratings yet
- Common Plating Media For Clinical Bacteriology (From Bailey & Scott's Diagnostic Microbiology, 12th Ed)Document2 pagesCommon Plating Media For Clinical Bacteriology (From Bailey & Scott's Diagnostic Microbiology, 12th Ed)Elizabeth Enjambre HernaniNo ratings yet
- Decalcifying AgentsDocument5 pagesDecalcifying AgentsLe Aura Mari Castillo100% (2)
- Week 5 Fecalysis (Lecture)Document8 pagesWeek 5 Fecalysis (Lecture)Dayledaniel SorvetoNo ratings yet
- Erythroblastosis Case StudyDocument19 pagesErythroblastosis Case StudyMaricel Agcaoili GallatoNo ratings yet
- Rh Factor and Pregnancy: Understanding Rh IncompatibilityDocument22 pagesRh Factor and Pregnancy: Understanding Rh IncompatibilityDrPreeti Thakur ChouhanNo ratings yet
- Neonatal PhysiologyDocument65 pagesNeonatal Physiologyunknownsince1986No ratings yet
- A Premature Infant Is An Infant Born Before 37 WK GestationDocument5 pagesA Premature Infant Is An Infant Born Before 37 WK GestationKamila KawaiiNo ratings yet
- Follicular Variant Papillary Thyroid CancerDocument11 pagesFollicular Variant Papillary Thyroid CancerNathaniel SimNo ratings yet
- CMGG 678Document1 pageCMGG 678Nathaniel SimNo ratings yet
- Hepatitis B, C, HIV and Syphilis Screening and DiagnosisDocument5 pagesHepatitis B, C, HIV and Syphilis Screening and DiagnosisNathaniel SimNo ratings yet
- Chapter 32 - Molecular Diagnosis in The Clinical LaboratoryDocument9 pagesChapter 32 - Molecular Diagnosis in The Clinical LaboratoryNathaniel SimNo ratings yet
- Micro SGD4Document8 pagesMicro SGD4Nathaniel SimNo ratings yet
- Chapter 24 - Extrinsic Defects Leading To Increased Erythrocyte Destruction - Non Immune CausesDocument5 pagesChapter 24 - Extrinsic Defects Leading To Increased Erythrocyte Destruction - Non Immune CausesNathaniel SimNo ratings yet
- TriviaDocument10 pagesTriviaNathaniel SimNo ratings yet
- NeighboorhoodDocument2 pagesNeighboorhoodNathaniel SimNo ratings yet
- OrganizationDocument6 pagesOrganizationNathaniel SimNo ratings yet
- OrganizationDocument5 pagesOrganizationNathaniel SimNo ratings yet
- Chapter 32 - Molecular Diagnosis in The Clinical LaboratoryDocument12 pagesChapter 32 - Molecular Diagnosis in The Clinical LaboratoryNathaniel SimNo ratings yet
- Chapter 25 - Extrinsic Defects Leading To Increased Erythrocyte Destruction - Immune Causes Final DraftDocument2 pagesChapter 25 - Extrinsic Defects Leading To Increased Erythrocyte Destruction - Immune Causes Final DraftNathaniel SimNo ratings yet
- Hematology Laboratory TabulationsDocument6 pagesHematology Laboratory TabulationsNathaniel SimNo ratings yet
- Chapter 29 - Introduction To Leukocyte NeoplasmsDocument4 pagesChapter 29 - Introduction To Leukocyte NeoplasmsNathaniel SimNo ratings yet
- Exfoliative CytologyDocument1 pageExfoliative CytologyNathaniel SimNo ratings yet
- Cytochemistry Chapter SummaryDocument3 pagesCytochemistry Chapter SummaryNathaniel SimNo ratings yet
- Auto ImmunityDocument7 pagesAuto ImmunityNathaniel SimNo ratings yet
- Chapter 43 - Thrombocytopenia and ThrombocytosisDocument6 pagesChapter 43 - Thrombocytopenia and ThrombocytosisNathaniel SimNo ratings yet
- Exfoliative CytologyDocument2 pagesExfoliative CytologyNathaniel Sim100% (2)
- CM Synovial FluidDocument42 pagesCM Synovial FluidNathaniel SimNo ratings yet
- Appendix A - Plasma Coagulation Factors PDFDocument1 pageAppendix A - Plasma Coagulation Factors PDFNathaniel SimNo ratings yet
- Skin Rashes Seen After Eating in A Seafood RestaurantDocument2 pagesSkin Rashes Seen After Eating in A Seafood RestaurantNathaniel SimNo ratings yet
- Chapter 15 - Examination of The Peripheral Blood Film and Correlation With The Complete Blood CountDocument7 pagesChapter 15 - Examination of The Peripheral Blood Film and Correlation With The Complete Blood CountNathaniel SimNo ratings yet
- IgE SI Lab ReportDocument7 pagesIgE SI Lab ReportNathaniel SimNo ratings yet
- HEMATOLOGY Cover PDFDocument10 pagesHEMATOLOGY Cover PDFNathaniel SimNo ratings yet
- BloodDocument2 pagesBloodNathaniel SimNo ratings yet
- Nobel Peace Prize Laureates 1901-2013Document2 pagesNobel Peace Prize Laureates 1901-2013Nathaniel Sim100% (1)
- Manual and Semiautomatic Hematology TestingDocument10 pagesManual and Semiautomatic Hematology TestingNathaniel Sim100% (1)
- MS ExcelDocument4 pagesMS ExcelNathaniel SimNo ratings yet
- Acquired Apraxia of Speech Treatment Overview PDFDocument12 pagesAcquired Apraxia of Speech Treatment Overview PDFHaroun Krilov-Egbert100% (1)
- Bronchial AsthmaDocument46 pagesBronchial AsthmaKhor Kee GuanNo ratings yet
- Medical Training: - Ventilation Options - For Internal Use OnlyDocument43 pagesMedical Training: - Ventilation Options - For Internal Use OnlyKamel HadyNo ratings yet
- Accu-Chek Performa Nano ManualDocument180 pagesAccu-Chek Performa Nano ManualPaula VelandiaNo ratings yet
- 413 Asri Ehs Hospitals List Till NowDocument45 pages413 Asri Ehs Hospitals List Till Nowapi-218060126No ratings yet
- Diverticulosis!!Document10 pagesDiverticulosis!!Nahdah AidahNo ratings yet
- Six Sigma Green BeltDocument57 pagesSix Sigma Green BeltRavi ValiyaNo ratings yet
- 2019 Quality Metrics For The Evaluation of Rapid Response SystemsDocument12 pages2019 Quality Metrics For The Evaluation of Rapid Response Systemsbogeg74816No ratings yet
- NUH Values and Behaviours BookletDocument28 pagesNUH Values and Behaviours BookletEverjoyNo ratings yet
- 10 Review JaiswalDocument7 pages10 Review JaiswalAniket PotnisNo ratings yet
- JumpSTART Training Presentation Instructor Course 2016 FinalDocument109 pagesJumpSTART Training Presentation Instructor Course 2016 FinalvictorioNo ratings yet
- Research Revision Version 10 (Clean Copy)Document27 pagesResearch Revision Version 10 (Clean Copy)Nesty Perez IIINo ratings yet
- Lip Augmentation, Lip Reduction, and Lip Lift Niamtu PDFDocument75 pagesLip Augmentation, Lip Reduction, and Lip Lift Niamtu PDFAbdullah özel100% (1)
- Salivary Gland DisordersDocument50 pagesSalivary Gland DisordersghazyNo ratings yet
- CTGDocument20 pagesCTGjaya ruban100% (1)
- Local Anesthesia Complications in Oral SurgeryDocument24 pagesLocal Anesthesia Complications in Oral SurgeryAlexandroEscamillaNo ratings yet
- Topic 1 What Is Patient Safety?Document14 pagesTopic 1 What Is Patient Safety?Lilik WijayatiNo ratings yet
- Tonsillitis, Tonsillectomy and Hodgkin's LymphomaDocument5 pagesTonsillitis, Tonsillectomy and Hodgkin's LymphomaD.E.P.HNo ratings yet
- Trauma Reactions in ChildrenDocument2 pagesTrauma Reactions in ChildrenAlesha Rose100% (2)
- A Guide To Brain AnatomyDocument7 pagesA Guide To Brain AnatomyPuppa AlexandraNo ratings yet
- Adenovirus DiseasesDocument44 pagesAdenovirus Diseasestummalapalli venkateswara rao100% (1)
- AnginaDocument16 pagesAnginaMc_Lopez_1761No ratings yet
- SchizophreniaDocument4 pagesSchizophreniaapi-315897191No ratings yet
- Mishba +pharmacology + Tapan ShahDocument232 pagesMishba +pharmacology + Tapan ShahRaushan BlakeNo ratings yet
- Sullivan ch03 LectureDocument36 pagesSullivan ch03 LectureNyein Nu Winn100% (1)
- Update On Stemi Management: Dr. Adi Purnawarman, SP - JP (K) - Fiha.,FasccDocument39 pagesUpdate On Stemi Management: Dr. Adi Purnawarman, SP - JP (K) - Fiha.,FasccArfiska Ridha Fausa 'ucha'No ratings yet
- Clinical Chemistry & Immunology GuideDocument4 pagesClinical Chemistry & Immunology GuideMary CabalceNo ratings yet
- ICU AlgorithmsDocument45 pagesICU AlgorithmsHashimIdreesNo ratings yet
- Case Study FIXDocument66 pagesCase Study FIXPatrick Kelvian100% (1)
- Nursing Care Plan for Activity IntoleranceDocument4 pagesNursing Care Plan for Activity IntoleranceShermane Criszen F. SallanNo ratings yet