Professional Documents
Culture Documents
Case 9 2007 Intra-Abdominal Focus Infection
Uploaded by
Anonymous 4txA8N8etOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Case 9 2007 Intra-Abdominal Focus Infection
Uploaded by
Anonymous 4txA8N8etCopyright:
Available Formats
Case 9: Bacteraemic infection with an intra-abdominal focus Clinical outline 92 yr old man Presented with RUQ pain and
vomiting (x5) over one day. Pain was severe, radiating across abdomen to LUQ. Gave history of episodic yellowing for many years. Acute dyspnoea developed while in ED: nebulisers given Past history includes CVA, LVF (moderate), CAL, AAA repair 1979. Medications: verapamil, diuretic, inhalers. O/E: unwell, having rigors, mild jaundice, alert HR 120/m regular, 140/80, Temp 38 O2sat 94% on 24% mask Soft BS bilaterally; prolonged exp wheeze, some bi-basal creps Soft abdomen, distended +, tender over RUQ . No stigmata of liver disease. No splenomegaly.
What is your provisional diagnosis and differential? Pause to think and compose your own answer before proceeding.
Differential diagnosis 1. Ascending cholangitis with bacteraemia; probable gall stone in the common bile duct The most likely diagnosis . This patient displays the syndrome called Charcots Triad. 2. Acute cholecystitis 3. Alcoholic hepatitis: the degree of pain is out of keeping with this diagnosis. Rigors implies secondary infection. Tenderness consistent. 4. Early RLZ pneumococcal pneumonia : may present with an acute abdomen, usually with UQ pain, usually pleuritic. Jaundice not infrequently occurs in pneumococcal pneumonia. Pneumonia may not be clinically apparent at presentation. Absence of cough unusual. In all likelihood decompensation of LVF and CAL probably responsible for dyspnoea. Absence of signs of peritonism make perforation less likely though not impossible in an elderly person.
What investigations would be useful to confirm your clinical suspicions?
Initial investigation results Hb 142g/l WCC 13.6 Plt 127 Film comment: Left shift with mild toxic changes. Mild macrocytosis (102fL). Consistent with liver disease. bilirubin 69 GGT 223 Alk phos 185 ALT 294 AST 317
Blood cultures taken: Gram negative rods isolated after 2 hrs of incubation CXR : increase interstitial markings c/w LVF Abdominal U/S arranged: CBD 9mm in diameter (was 5mm on previous u/s in May 1998). No gall stones seen.
What is your interpretation of these results?
Interpretation of initial results The patient has moderately deranged LFTs with a mixed picture c/w cholangitis Blood cultures confirm bacteraemia; there is a high incidence of bacteraemia in cholangitis The ultrasound is very suggestive of CBD obstruction with diameter of CBD at the upper limit of normal. CBD stones may easily be missed on u/s.
What are the management principles for this condition? Management principles 1. EMPIRIC antibiotic therapy: Patient given gentamicin and ticarcillin/clavualate (Timentin). More usual protocol is ampicillin/gentamicin with metronidazole (see Antibiotic guidelines). Principle is to cover aerobic gram negatives and enteric streptococci (S. milleri group and others) well. Anaerobic cover also important particularly in patients with malignant biliary obstruction. Usual protocol also covers enterococci which may also contribute though these are seldom the major pathogens and antibiotics such as timentin that do not cover enterococci usually work. Temperature, pain and rigors settled over next 48 hrs. Have a look at the relevant section of the antibiotic guidelines for cholangitis. Are there particular problems with giving gentamicin in the presence of liver disease or jaundice?
1. Early ERCP to relieve CBD obstruction: Relief of obstruction is as crucial as providing antibiotic therapy. Patient underwent ERCP on day 2; the ampulla of vater was inflamed and after cholangiogram, spincterotomy was performed. A small gall stone liberated together with dirty-looking bile. A gastric ulcer, possibly malignant was also found and biopsied. 2. Supportive care: judicious hydration, monitor observations closely etc 3. Modify antibiotic therapy in the light of susceptibility of cultures: = DIRECTED THERAPY Culture from blood identified as E. coli resistant to ampicillin, timentin, cefotaxime and sensitive to gentamicin, ciprofloxacin, imipenem. Patient was changed to oral ciprofloxacin 500mg bd and did well. Note that gentamicin not advisable beyond a few doses in elderly patients and does not penetrate well into bile. However it has a good initial impact on the bacteraemic component of this disease which is most important. Ciprofloxacin was the only oral choice available based on susceptibilities. However some elderly can develop an acute confusional state or tremor while on ciprofloxacin, especially at higher doses, so beware. This bacterial isolate is probably making an extended spectrum -lactamase (ESBL) enzyme that is able to destroy ampicillin and third generation cephalosporins. Whilst this enzyme is inhibited by the clavulanate in timentin, this bacteria is probably producing enough -lactamase to overcome the effect of clavulanate. Only relatively simple mutations in the usual plasmid-mediated -lactamase (penicillinase responsible for ampicillin resistance) of E. coli is required to extend its spectrum to include cefotaxime. Further reading Antibiotic guidelines 13th Edition
You might also like
- Bowels Open 6 Times Per 24 Hours: Document ControlDocument7 pagesBowels Open 6 Times Per 24 Hours: Document ControlKeith PohlNo ratings yet
- Case PresentationDocument26 pagesCase Presentationhamid murtazaNo ratings yet
- Pediatrics MS WordDocument13 pagesPediatrics MS WordSamhitha SharmaNo ratings yet
- Gallbladder Carcinoma Presenting As Right Upper Quadrant Pain: A Case ReportDocument19 pagesGallbladder Carcinoma Presenting As Right Upper Quadrant Pain: A Case ReportMacky YongcoNo ratings yet
- Inflammatory Bowel DiseaseDocument4 pagesInflammatory Bowel DiseaseJustisia PadmiyatiNo ratings yet
- Case Protocol M&MDocument5 pagesCase Protocol M&Mcharmaine BallanoNo ratings yet
- Congenitally-Acquired Advanced Hiv With Ois: Medical and Social ComplexitiesDocument25 pagesCongenitally-Acquired Advanced Hiv With Ois: Medical and Social ComplexitiesKing MazingaNo ratings yet
- Step 3 NotesDocument20 pagesStep 3 NotesHunter Ross100% (1)
- Paeds Crack Notes-1Document111 pagesPaeds Crack Notes-1Ashutosh Krishna JadhavNo ratings yet
- Gastroenterology MCQS: Primary Biliary Cholangitis: FeaturesDocument96 pagesGastroenterology MCQS: Primary Biliary Cholangitis: FeaturesOmar HamdyNo ratings yet
- Surgery Class Biliary System SurgeryDocument69 pagesSurgery Class Biliary System SurgeryKashif BurkiNo ratings yet
- Acute ColitisDocument8 pagesAcute ColitisKhurram NadeemNo ratings yet
- 178 Med Gastro DiverticulitisDocument4 pages178 Med Gastro DiverticulitisqurbanNo ratings yet
- Pancreatic Disease1Document24 pagesPancreatic Disease1Hero StoreNo ratings yet
- Inflammatory DisturbancesDocument63 pagesInflammatory DisturbancesWang Ming YaNo ratings yet
- December09, Paper 1Document16 pagesDecember09, Paper 1Ismail SialaNo ratings yet
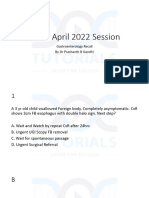
- INI SS April 2022 Gastro RecallDocument106 pagesINI SS April 2022 Gastro Recallgirishkiran23No ratings yet
- Inflammatory Colitis - A RecapDocument34 pagesInflammatory Colitis - A RecapanahitaasharmaNo ratings yet
- Surgical Management of Inflammatory Bowel Disease: Robert R. Cima, MD John H. Pemberton, MDDocument11 pagesSurgical Management of Inflammatory Bowel Disease: Robert R. Cima, MD John H. Pemberton, MDBernadett FarkasNo ratings yet
- TMP 12 E9Document5 pagesTMP 12 E9FrontiersNo ratings yet
- Ziad Aro, MD Internal MedicineDocument100 pagesZiad Aro, MD Internal MedicineAli Aborges Jr.No ratings yet
- 28-Year-Old Man With Crohn Disease and Hematuria: Residents ' ClinicDocument5 pages28-Year-Old Man With Crohn Disease and Hematuria: Residents ' ClinicDesi HutapeaNo ratings yet
- Residents Notes GuatloDocument2 pagesResidents Notes GuatloRizielle MendozaNo ratings yet
- UlcerativecolitisDocument27 pagesUlcerativecolitisMohamed Abdulrazaq100% (1)
- 10.1053@j.gastro DiverticulitisDocument20 pages10.1053@j.gastro DiverticulitisCarlos CaicedoNo ratings yet
- INTRO - Types: Chron'sDocument47 pagesINTRO - Types: Chron'sfadliNo ratings yet
- Upper GI Malignancy - TutorDocument28 pagesUpper GI Malignancy - Tutoramoody95No ratings yet
- Acute Kidney Injury Case Study FinalDocument46 pagesAcute Kidney Injury Case Study FinalSalwa KaramanNo ratings yet
- GroupA RenalDisordersDocument13 pagesGroupA RenalDisordersPaulNo ratings yet
- Journal of Pharmaceutical and Scientific Innovation: Case StudyDocument3 pagesJournal of Pharmaceutical and Scientific Innovation: Case StudyDinoCsbrowNo ratings yet
- Case 1Document4 pagesCase 1Irsanti SasmitaNo ratings yet
- 2016 Visceral Leishmaniasis Turning Into CLDDocument4 pages2016 Visceral Leishmaniasis Turning Into CLDPratyay HasanNo ratings yet
- Antibiotics by Clinical CasesDocument59 pagesAntibiotics by Clinical CasesNikNo ratings yet
- 2 AppendicitisDocument9 pages2 AppendicitisPavi MuruganathanNo ratings yet
- Loose Motion and Weight LossDocument40 pagesLoose Motion and Weight LossneptorNo ratings yet
- Tip: Urinary Proteins Less Than 300 MG Is Not Detectable by Urine DipstickDocument11 pagesTip: Urinary Proteins Less Than 300 MG Is Not Detectable by Urine DipstickAsif Newaz100% (2)
- Management of Severe Malaria: Paul N HarijantoDocument62 pagesManagement of Severe Malaria: Paul N Harijantostivana26No ratings yet
- EMQs For Medical Students Volume 2 2eDocument30 pagesEMQs For Medical Students Volume 2 2ePasTestBooks50% (2)
- BevacizumabDocument4 pagesBevacizumabMartínez Roldán Johana Yadira 3EZNo ratings yet
- Ulcerative Colitis HandoutDocument1 pageUlcerative Colitis HandoutevedgebahNo ratings yet
- Surgery 3 White Part 1Document87 pagesSurgery 3 White Part 1Håíthãm KhãtïßNo ratings yet
- Case Presentation: Cagayan Valley Medical CenterDocument57 pagesCase Presentation: Cagayan Valley Medical CenterGian PagadduNo ratings yet
- Critically Ill 75 Year Old Man With ComplicationsDocument20 pagesCritically Ill 75 Year Old Man With ComplicationssummiyaNo ratings yet
- MR GastroDocument31 pagesMR GastroAdefuye AbiolaNo ratings yet
- Carrick 2018Document7 pagesCarrick 2018Edwin AlvarezNo ratings yet
- (Mayo Clinic Proceedings, Dec 2022) - 82 Year Old Man With Chest Pain and Shortness of BreathDocument5 pages(Mayo Clinic Proceedings, Dec 2022) - 82 Year Old Man With Chest Pain and Shortness of BreathNigelyulNo ratings yet
- PracticeExam CCSDocument12 pagesPracticeExam CCSBehrouz Yari75% (4)
- MIS C Algorithim Version 2Document8 pagesMIS C Algorithim Version 2Saima UmairNo ratings yet
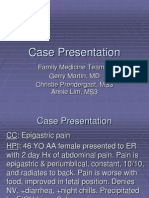
- Case Presentation: Family Medicine Team C Gerry Martin, MD Christie Prendergast, MS3 Annie Lim, MS3Document24 pagesCase Presentation: Family Medicine Team C Gerry Martin, MD Christie Prendergast, MS3 Annie Lim, MS3Aditya Sonal Mahajan100% (1)
- Gastro ExamDocument12 pagesGastro ExamAllison Eunice ServandoNo ratings yet
- Case Presentation: Clostridium DifficileDocument35 pagesCase Presentation: Clostridium DifficileDnse LucidoNo ratings yet
- 260-Article Text-875-1-10-20220728Document4 pages260-Article Text-875-1-10-20220728hasan andrianNo ratings yet
- CT Week9Document4 pagesCT Week9Princess Laira CañeteNo ratings yet
- April Morbidity and Mortality Case Conference: Roxanne Jeen L. FornollesDocument30 pagesApril Morbidity and Mortality Case Conference: Roxanne Jeen L. FornollesAyen FornollesNo ratings yet
- Ipi 82603Document18 pagesIpi 82603Megawati LiwangNo ratings yet
- Toxic Megacolon Presentation FinalDocument33 pagesToxic Megacolon Presentation FinalHendra SetyawanNo ratings yet
- INP CU 10 GlomeruloDocument5 pagesINP CU 10 GlomeruloMichelle Gliselle Guinto MallareNo ratings yet
- AACE Clinical Case ReportsDocument4 pagesAACE Clinical Case ReportsShuaib AhmedNo ratings yet
- H IsselbacherDocument5 pagesH IsselbacherAnonymous 4txA8N8etNo ratings yet
- Pass Paces EbDocument10 pagesPass Paces EbAnonymous 4txA8N8etNo ratings yet
- Hp165-02b-Nash (FF 050816v) ProtegidoDocument9 pagesHp165-02b-Nash (FF 050816v) ProtegidoAnonymous 4txA8N8etNo ratings yet
- Topics Runtime: Subjects AnatomyDocument2 pagesTopics Runtime: Subjects AnatomyAnonymous 4txA8N8etNo ratings yet
- Hanzi Pinyin English: HSK Level 2Document5 pagesHanzi Pinyin English: HSK Level 2Anonymous 4txA8N8etNo ratings yet
- Adpkd: Autosomal Dominant Polycystic Kidney DiseaseDocument7 pagesAdpkd: Autosomal Dominant Polycystic Kidney DiseaseAnonymous 4txA8N8etNo ratings yet
- Genetics 50qDocument62 pagesGenetics 50qAnonymous 4txA8N8etNo ratings yet
- Brunicardi-1996-Time Management - A RDocument7 pagesBrunicardi-1996-Time Management - A RAnonymous 4txA8N8etNo ratings yet
- 6 Steps in Assisting in Cardiac Rhythm InterpretationDocument1 page6 Steps in Assisting in Cardiac Rhythm InterpretationAnonymous 4txA8N8etNo ratings yet
- EMQExample RacpDocument5 pagesEMQExample RacpAnonymous 4txA8N8etNo ratings yet
- Abdominal Exam DATEDocument3 pagesAbdominal Exam DATEAnonymous 4txA8N8etNo ratings yet
- Radiology Reviewed Meds Reviewed Pathology Reviewed Micro Reviewed "FASTHUG" CheckedDocument1 pageRadiology Reviewed Meds Reviewed Pathology Reviewed Micro Reviewed "FASTHUG" CheckedAnonymous 4txA8N8etNo ratings yet
- Effective Feedback Skills: Sally Santen MD, PHDDocument9 pagesEffective Feedback Skills: Sally Santen MD, PHDAnonymous 4txA8N8etNo ratings yet
- Ganong - Physiology Self - Assessment Questions - 03Document46 pagesGanong - Physiology Self - Assessment Questions - 03Anonymous 4txA8N8et100% (3)
- Lymphoproliferative Disorders Part 2Document7 pagesLymphoproliferative Disorders Part 2Anonymous 4txA8N8etNo ratings yet
- Mmvr19 / Nextmed Conference ScheduleDocument21 pagesMmvr19 / Nextmed Conference SchedulepvaldastriNo ratings yet
- Annotated BibDocument3 pagesAnnotated Bibapi-489789428No ratings yet
- Efavirenz Chem OlympicsDocument1 pageEfavirenz Chem OlympicsdreamingsnowNo ratings yet
- A Review of Conjoint Family Therapy and The Theories of Virginia SatirDocument9 pagesA Review of Conjoint Family Therapy and The Theories of Virginia SatirLORETO CNo ratings yet
- Interferential Stimulation For The Treatment of Musculoskeletal PainDocument15 pagesInterferential Stimulation For The Treatment of Musculoskeletal PainCTAFDocumentsNo ratings yet
- Lymphoma HandoutDocument5 pagesLymphoma Handoutapi-244850728No ratings yet
- Perioperative NursingDocument12 pagesPerioperative Nursingtheglobalnursing100% (12)
- Module 4 (Basics of Sti, Hiv & Aids)Document37 pagesModule 4 (Basics of Sti, Hiv & Aids)Marky RoqueNo ratings yet
- Examination of Orthopedic and Athletic Injuries Starkey PDFDocument2 pagesExamination of Orthopedic and Athletic Injuries Starkey PDFJenny0% (4)
- Renal Parenchymal TumorsDocument45 pagesRenal Parenchymal TumorsDaniel100% (1)
- Panic StationsDocument9 pagesPanic Stationsdaneen naqviNo ratings yet
- Tetralogy Hypercyanotic SpellDocument3 pagesTetralogy Hypercyanotic SpellJunior PratasikNo ratings yet
- Running Head: VICTIM ADVOCACYDocument5 pagesRunning Head: VICTIM ADVOCACYCatherineNo ratings yet
- The Healthy Bones Nutrition Plan and Cookbook - IntroductionDocument10 pagesThe Healthy Bones Nutrition Plan and Cookbook - IntroductionChelsea Green PublishingNo ratings yet
- An Insight Into Pericoronitis PDFDocument4 pagesAn Insight Into Pericoronitis PDFNarissaporn ChaiprakitNo ratings yet
- Emphasis On Non-Pharmacologic Aspect: Key Principles: o Gate Control & Neuromatrix Theory of PainDocument3 pagesEmphasis On Non-Pharmacologic Aspect: Key Principles: o Gate Control & Neuromatrix Theory of PainJudy Ignacio EclarinoNo ratings yet
- Roots 1 - 2015Document60 pagesRoots 1 - 2015Ovidiu100% (1)
- BasicsOfRadiopharmacy PDFDocument205 pagesBasicsOfRadiopharmacy PDFFithriana RachmawatiNo ratings yet
- PHD Thesis On Medical Tourism in IndiaDocument4 pagesPHD Thesis On Medical Tourism in IndiaBuyingCollegePapersPittsburgh100% (1)
- Dr. Nyoman - Neuropsychiatric Systemic Lupus Erythematosus (NPSLE) .Document41 pagesDr. Nyoman - Neuropsychiatric Systemic Lupus Erythematosus (NPSLE) .hum2No ratings yet
- PsychSim 4 Activities Psychopathology and TherapyDocument6 pagesPsychSim 4 Activities Psychopathology and TherapyCarolineNo ratings yet
- Surgery TCVS SGD Guide KKDocument7 pagesSurgery TCVS SGD Guide KKFu Xiao ShanNo ratings yet
- Abscess Incision and Drainage NEJMDocument4 pagesAbscess Incision and Drainage NEJMMarcela CharryNo ratings yet
- History: Nara Period Toilet PaperDocument13 pagesHistory: Nara Period Toilet PaperHà MyNo ratings yet
- Global Practicesand Policiesof Organ Transplantationand Organ TraffickingDocument15 pagesGlobal Practicesand Policiesof Organ Transplantationand Organ TraffickingM Asif NawazNo ratings yet
- HBN 07-01 FinalDocument34 pagesHBN 07-01 FinalYahya Hammoudeh100% (1)
- Prevention of Hypotension After Spinal Anaesthesia For Caesarean SectionDocument13 pagesPrevention of Hypotension After Spinal Anaesthesia For Caesarean SectionANGELICANo ratings yet
- Volume3 Issue8 (4) 2014Document342 pagesVolume3 Issue8 (4) 2014iaetsdiaetsdNo ratings yet
- CBE - Platelet AbnormalitiesDocument3 pagesCBE - Platelet AbnormalitiesRuxandra MesarosNo ratings yet
- EyeDocument11 pagesEyeSyed Ali HaiderNo ratings yet