Professional Documents
Culture Documents
Thyroid Storm
Uploaded by
Cristina CenturionCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Thyroid Storm
Uploaded by
Cristina CenturionCopyright:
Available Formats
Thyroid storm
(thyroid crisis) is a potentially life-threatening condition for people who have hyperthyroidism. Thyroid storm happens when your thyroid gland suddenly releases large amounts of thyroid hormone in a short period of time. If you have thyroid storm, you will need emergency medical treatment. Thyroid storm is more likely to develop when a person has a serious health problem in addition to hyperthyroidism or in people who have untreated or undertreated Graves' disease. The problem usually happens after a stressful event or a serious illness, such as a major infection. It may also be triggered by surgery or by using iodine for a CT scan or in radioactive iodine therapy. Symptoms of thyroid storm include: Feeling extremely irritable or grumpy. High systolic blood pressure, low diastolic blood pressure, and fast heartbeat. Nausea, vomiting, or diarrhea. High fever. Shock and delirium. Feeling confused. Feeling sleepy. Yellow skin or eyes. Symptoms of heart failure, such as breathing problems or feeling very tired. Thyroid storm can lead to coma, heart failure, or death. Thyrotoxic crisis (or thyroid storm) is a rare but severe complication of hyperthyroidism, which may occur when a thyrotoxic patient becomes very sick or physically stressed. Its symptoms can include: an increase in body temperature to over 40 degrees Celsius (104 degrees Fahrenheit), tachycardia, arrhythmia, vomiting, diarrhea, dehydration, coma,[11] and death. Thyroid storm requires prompt treatment and hospitalization. The main treatment is to decrease the circulating thyroid hormone levels and decrease their formation. Propylthiouracil and methimazole are two agents that decrease thyroid hormone synthesis and are usually prescribed in fairly high doses.
To inhibit thyroid hormone release from the thyroid gland, sodium iodide, potassium iodide, and/or Lugol's solution can be given. Beta blockers such as propranolol (Inderal, Inderal LA, Innopran XL) can help to control the heart rate, and intravenous steroids may be used to help support the circulation. Hyperthyroidism:
Antithyroid drugs
Thyrostatics (antithyroid drugs) are drugs that inhibit the production of thyroid hormones, such as carbimazole (used in UK) and methimazole (used in US), and propylthiouracil. Propylthiouracil also works outside the thyroid gland, preventing conversion of (mostly inactive) T4 to the active form T3. Because thyroid tissue usually contains a substantial reserve of thyroid hormone, thyrostatics can take weeks to become effective, and the dose often needs to be carefully titrated over a period of months, with regular doctor visits and blood tests to monitor results.
Beta-blockers
Many of the common symptoms of hyperthyroidism such as palpitations, trembling, and anxiety are mediated by increases in beta adrenergic receptors on cell surfaces. Beta blockers, typically used to treat high blood pressure, are a class of drugs that offset this effect, reducing rapid pulse associated with the sensation of palpitations, and decreasing tremor and anxiety. Thus, a patient suffering from hyperthyroidism can often obtain immediate temporary relief until the hyperthyroidism can be characterized with the Radioiodine test noted above and more permanent treatment take place.
Iodine-131 (radioiodine) radioisotope therapy, which was first
pioneered by Dr. Saul Hertz,[26] radioactive iodine-131 is given orally (either by pill or liquid) on a one-time basis, to severely restrict, or altogether destroy the function of a hyperactive thyroid gland.
Food and diet
Patients cannot have foods high in iodine, such as edible seaweed and kelps.
Stroke:
patients with intracerebral bleeds are more likely to have headache, altered mental status, seizures, nausea and vomiting, and/or marked hypertension, none of these findings reliably distinguishes between hemorrhagic and ischemic stroke. The etiologies of stroke are varied, but they can be broadly categorized into ischemic or hemorrhagic. Approximately 80-87% of strokes are from ischemic infarction caused by thrombotic or embolic cerebrovascular occlusion. Intracerebral hemorrhages account for most of the remainder of strokes, with a smaller number resulting from aneurysmal subarachnoid hemorrhage. Risk factors The risk of hemorrhagic stroke is increased with the following factors: Advanced age Hypertension (up to 60% of cases) Previous history of stroke Alcohol abuse Use of illicit drugs (eg, cocaine, other sympathomimetic drugs) Causes of hemorrhagic stroke include the following[8, 9, 11, 12, 13] : Hypertension Cerebral amyloidosis Coagulopathies Anticoagulant therapy Thrombolytic therapy for acute myocardial infarction (MI) or acute ischemic stroke (can cause iatrogenic hemorrhagic transformation) Arteriovenous malformation (AVM), aneurysms, and other vascular malformations (venous and cavernous angiomas) Vasculitis Intracranial neoplasm Hypertension The most common etiology of primary hemorrhagic stroke (intracerebral hemorrhage) is hypertension. At least two thirds of patients with primary intraparenchymal hemorrhage are reported to have preexisting or newly diagnosed hypertension. Hypertensive small-vessel disease results from tiny lipohyalinotic aneurysms that subsequently rupture and result in intraparenchymal hemorrhage. Typical locations include the basal ganglia, thalami, cerebellum, and pons. Aneurysms and subarachnoid hemorrhage
The most common cause of atraumatic hemorrhage into the subarachnoid space is rupture of an intracranial aneurysm. Aneurysms are focal dilatations of arteries, with the most frequently encountered intracranial type being the berry (saccular) aneurysm.
History
Obtaining an adequate history includes determining the onset and progression of symptoms, as well as assessing for risk factors and possible causative events. Such risk factors include the following: Previous transient ischemic attack (TIA) and stroke Hypertension Diabetes Smoking Arrhythmia and valvular disease Illicit drug use Use of anticoagulants Risk factors for thrombosis A history of trauma, even if minor, may be important, as extracranial arterial dissections can result in ischemic stroke. Hemorrhagic versus ischemic stroke Symptoms alone are not specific enough to distinguish ischemic from hemorrhagic stroke. However, generalized symptoms, including nausea, vomiting, and headache, as well as an altered level of consciousness, may indicate increased intracranial pressure and are more common with hemorrhagic strokes and large ischemic strokes. Seizures are more common in hemorrhagic stroke than in the ischemic kind. Seizures occur in up to 28% of hemorrhagic strokes, generally at the onset of the intracerebral hemorrhage or within the first 24 hours. Focal neurologic deficits The neurologic deficits reflect the area of the brain typically involved, and stroke syndromes for specific vascular lesions have been described. Focal symptoms of stroke include the following: Weakness or paresis that may affect a single extremity, one half of the body, or all 4 extremities Facial droop Monocular or binocular blindness Blurred vision or visual field deficits Dysarthria and trouble understanding speech Vertigo or ataxia, Aphasia
Subarachnoid hemorrhage Symptoms of subarachnoid hemorrhage may include the following: Sudden onset of severe headache Signs of meningismus with nuchal rigidity Photophobia and pain with eye movements Nausea and vomiting Syncope - Prolonged or atypical
Approach Considerations
The treatment and management of patients with acute intracerebral hemorrhage depends on the cause and severity of the bleeding. Basic life support, as well as control of bleeding, seizures, blood pressure (BP), and intracranial pressure, are critical. Medications used in the treatment of acute stroke include the following: Anticonvulsants - To prevent seizure recurrence Antihypertensive agents - To reduce BP and other risk factors of heart disease Osmotic diuretics - To decrease intracranial pressure in the subarachnoid space Management begins with stabilization of vital signs. Perform endotracheal intubation for patients with a decreased level of consciousness and poor airway protection. Intubate and hyperventilate if intracranial pressure is elevated, and initiate administration of mannitol for further control. Rapidly stabilize vital signs, and simultaneously acquire an emergent computed tomography (CT) scan. Glucose levels should be monitored, with normoglycemia recommended.[28] Antacids are used to prevent associated gastric ulcers. Currently, no effective targeted therapy for hemorrhagic stroke exists.
Medication Summary
Medications used in the treatment of acute stroke include anticonvulsants such as diazepam, to prevent seizure recurrence; antihypertensive agents such as labetalol, to reduce blood pressure (BP) and other risk factors for heart disease; and osmotic diuretics such as mannitol, to decrease intracranial pressure in the subarachnoid space. As previously mentioned, the treatment and management of patients with acute intracerebral hemorrhage depends on the cause and severity of the bleeding. However, there is currently no effective targeted therapy for hemorrhagic stroke.
Autonomic dysreflexia (AD) is a syndrome of massive imbalanced reflex sympathetic discharge occurring in patients with spinal cord injury (SCI) above the splanchnic sympathetic outflow (T5-T6). This condition represents a medical emergency, so recognizing and treating the earliest signs and symptoms efficiently can avoid dangerous sequelae of elevated blood pressure. SCI patients, caregivers, and medical professionals must be knowledgeable about this syndrome and its management. Physical Examination A patient with AD may have 1 or more of the following findings on physical examination: Sudden, significant rise in systolic and diastolic blood pressure Profuse sweating above the level of lesion - Especially in the face, neck, and shoulders; rarely occurs below the level of the lesion because of sympathetic cholinergic activity Goose bumps above, or possibly below, the level of the lesion Flushing of the skin above the level of the lesion - Especially in the face, neck, and shoulders; this is a frequent symptom Blurred vision Spots in the patient's visual field Nasal congestion A common symptom With regard to the first item above, the sudden rise in blood pressure in AD is usually associated with bradycardia.
You might also like
- A Simple Guide to Thyrotoxicosis, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Thyrotoxicosis, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Multiple SclerosisDocument6 pagesMultiple SclerosisRonnel Alvin Antonio AdrianoNo ratings yet
- A Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Schizophrenia: Vaisnvi Muthoovaloo 102011430Document18 pagesSchizophrenia: Vaisnvi Muthoovaloo 102011430Vaisnavi MuthoovalooNo ratings yet
- Disorders of the Patellofemoral Joint: Diagnosis and ManagementFrom EverandDisorders of the Patellofemoral Joint: Diagnosis and ManagementNo ratings yet
- Pathophysiology of Depression and Mechanisms of Treatment PDFDocument14 pagesPathophysiology of Depression and Mechanisms of Treatment PDFSantiago Gabriel Ramos GuaidoNo ratings yet
- OsteoarthritisDocument28 pagesOsteoarthritisLydia Lopz MsnrncdNo ratings yet
- Bilateral Knee OADocument35 pagesBilateral Knee OAMu'iz Beatforteen50% (2)
- Amyotrophic Lateral SclerosisDocument24 pagesAmyotrophic Lateral SclerosisJeanessa Delantar QuilisadioNo ratings yet
- Different Diagnostic Procedure of Typhoid Fever ADocument8 pagesDifferent Diagnostic Procedure of Typhoid Fever AdjebrutNo ratings yet
- Spinal Cord Injuries-KyienDocument25 pagesSpinal Cord Injuries-KyienjohnnyienNo ratings yet
- 1MENIEREDocument6 pages1MENIEREsunny_jr_No ratings yet
- Resource Unit On Management of Patients With Manipulative BehaviorsDocument19 pagesResource Unit On Management of Patients With Manipulative BehaviorsPC NNo ratings yet
- STDDocument78 pagesSTDKrupa KarnikNo ratings yet
- Chole Lithia SisDocument55 pagesChole Lithia Sisjaja_gatanNo ratings yet
- Doctor, What 'S This Acupuncture All About?Document7 pagesDoctor, What 'S This Acupuncture All About?Lev KalikaNo ratings yet
- Case Scenarios 3rd Yr Head NursingDocument5 pagesCase Scenarios 3rd Yr Head NursingBianca MaeNo ratings yet
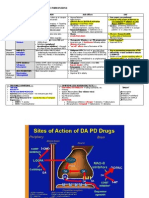
- Pharmacologic TX For Idiopathic Parkinsons: Strategy Class / Drug MOA Side Effects USEDocument2 pagesPharmacologic TX For Idiopathic Parkinsons: Strategy Class / Drug MOA Side Effects USEnicdeepNo ratings yet
- ETOH Case StudyDocument5 pagesETOH Case StudyCharme Jean RaygonNo ratings yet
- Autoimmune DisordersDocument13 pagesAutoimmune Disordersinah krizia lagueNo ratings yet
- DM PhysioDocument24 pagesDM Physiodwi astutiNo ratings yet
- mhGAP Humanitarian Intervention Guide (mhGAP-HIG) - English VersionDocument68 pagesmhGAP Humanitarian Intervention Guide (mhGAP-HIG) - English VersionПламен МинчевNo ratings yet
- Blood Transfusion FinalDocument8 pagesBlood Transfusion FinalejkohNo ratings yet
- Cranial Nerves Assessment FormDocument3 pagesCranial Nerves Assessment FormCristina CenturionNo ratings yet
- Agis Mira Dewi, S.kedDocument35 pagesAgis Mira Dewi, S.kedAgiish EMdeNo ratings yet
- Glasgow Coma ScaleDocument3 pagesGlasgow Coma Scaletoto11885No ratings yet
- Fracture ManagementDocument21 pagesFracture ManagementPatrickk WandererNo ratings yet
- Musculoskeletal System Musculoskeletal System: A. SkeletonDocument23 pagesMusculoskeletal System Musculoskeletal System: A. SkeletonTina TalmadgeNo ratings yet
- Pathophysiology of Schizophrenia: February 2014Document24 pagesPathophysiology of Schizophrenia: February 2014Tuderici IoanaNo ratings yet
- SC2 2015 HyperthyroidismDocument38 pagesSC2 2015 HyperthyroidismShafern TanNo ratings yet
- Hyporeninemic HypoaldosteronismDocument12 pagesHyporeninemic HypoaldosteronismCésar Augusto Sánchez SolisNo ratings yet
- PSYB32 Final Exam ReviewDocument29 pagesPSYB32 Final Exam Reviewraeesah9171No ratings yet
- Palak Khanna Sadhana Shukla Madiha Rehamani Ishwin Tandon: By: (Group 2) (Group 2) (Group 2) (Group 1)Document43 pagesPalak Khanna Sadhana Shukla Madiha Rehamani Ishwin Tandon: By: (Group 2) (Group 2) (Group 2) (Group 1)pal0% (1)
- Mineire'sDocument16 pagesMineire'sShaykh Evangelista BacualNo ratings yet
- DementiaDocument27 pagesDementiaNina OaipNo ratings yet
- Poliomyelitis 1Document13 pagesPoliomyelitis 1Mumin Farah100% (1)
- What Is PolymyositisDocument24 pagesWhat Is PolymyositisAshraf MobyNo ratings yet
- Pagets DiseaseDocument2 pagesPagets DiseaseLov Raj LohaniNo ratings yet
- Skills 116 Finals ROM Assistive Devices PDFDocument64 pagesSkills 116 Finals ROM Assistive Devices PDFMae Arra Gilbao Lecobu-anNo ratings yet
- Barrett's EsophagusDocument10 pagesBarrett's EsophagusaryadroettninguNo ratings yet
- Juvenile Rheumatoid ArthritisDocument21 pagesJuvenile Rheumatoid ArthritisFarry DoankNo ratings yet
- Muscular System ReviewerDocument16 pagesMuscular System ReviewerNicole ZaputNo ratings yet
- Acute GlomerulonephritisDocument14 pagesAcute GlomerulonephritisAnonymous D976HVjqcgNo ratings yet
- Rheumatoid ArthritisDocument29 pagesRheumatoid ArthritisTamim IshtiaqueNo ratings yet
- Types of ParalysisDocument6 pagesTypes of ParalysisLoh Wei ChiehNo ratings yet
- TB Spine OrthopedicsDocument34 pagesTB Spine OrthopedicsHafizah HoshniNo ratings yet
- The Detailed Neurologic Examination in Adults - UpToDate PDFDocument29 pagesThe Detailed Neurologic Examination in Adults - UpToDate PDFMiguel GarciaNo ratings yet
- Reflection About Patients With DementiaDocument2 pagesReflection About Patients With Dementiaalexander abasNo ratings yet
- 1506359236-Assignment 13 - Diagnosing Schizophrenia and Other Psychotic DisordersDocument4 pages1506359236-Assignment 13 - Diagnosing Schizophrenia and Other Psychotic DisordersRita Prince0% (1)
- Cardio NoteDocument17 pagesCardio NoteMustak AhmedNo ratings yet
- Handout Orthopedic Nursing ScoliosisDocument3 pagesHandout Orthopedic Nursing ScoliosisPaul Christian P. Santos, RN100% (3)
- Preoperative Assessment in Diabetic PatientsDocument2 pagesPreoperative Assessment in Diabetic PatientsShilpa Pradhan100% (1)
- STIsDocument8 pagesSTIsJovie Anne BorjaNo ratings yet
- Diabetes NotesDocument10 pagesDiabetes Notestripj33No ratings yet
- Acute Myocardial InfarctionDocument22 pagesAcute Myocardial InfarctionkpsuanNo ratings yet
- What Is AnxietyDocument13 pagesWhat Is AnxietyelaineNo ratings yet
- General Pedia NelsonDocument308 pagesGeneral Pedia Nelsonعمر محمدNo ratings yet
- Rheumatoid Arthritis: Polyarthritis As Its Most Common Feature. in Addition, Other Tissues May Be DamagedDocument8 pagesRheumatoid Arthritis: Polyarthritis As Its Most Common Feature. in Addition, Other Tissues May Be Damagedحنين حسن عبد علي حسينNo ratings yet
- Subacute Combined Degeneration of Spinal CordDocument4 pagesSubacute Combined Degeneration of Spinal CordPriyanka MathurNo ratings yet
- Urinary Stones DiseaseDocument40 pagesUrinary Stones DiseaseRenaldy ThiorisNo ratings yet
- Cranial Nerves Assessment FormDocument3 pagesCranial Nerves Assessment FormCristina CenturionNo ratings yet
- Brother Manual Kh950iDocument199 pagesBrother Manual Kh950iCristina CenturionNo ratings yet
- Nclex MedicationsDocument39 pagesNclex MedicationsCristina Centurion100% (2)
- Emergency DrugsDocument2 pagesEmergency DrugsCristina CenturionNo ratings yet
- Mood Disorders Class & Copy 11-1Document43 pagesMood Disorders Class & Copy 11-1Cristina CenturionNo ratings yet
- Chair ExercisesDocument5 pagesChair ExercisesCristina CenturionNo ratings yet
- Pharmacology OverviewDocument33 pagesPharmacology OverviewCristina CenturionNo ratings yet
- Nclex TermsDocument48 pagesNclex TermsCristina Centurion100% (2)
- Anxiety Class & Copy11-2Document33 pagesAnxiety Class & Copy11-2Cristina CenturionNo ratings yet
- Neurological Stressors III Chronic Neurological Disorders: Joy Borrero, RN, MSN and NUR240 Nursing StudentsDocument38 pagesNeurological Stressors III Chronic Neurological Disorders: Joy Borrero, RN, MSN and NUR240 Nursing StudentsCristina CenturionNo ratings yet
- Nclex Made Incredible Easy - Cardio AnswersDocument16 pagesNclex Made Incredible Easy - Cardio AnswersCristina CenturionNo ratings yet
- Asthma Article CareplanDocument2 pagesAsthma Article CareplanCristina CenturionNo ratings yet
- Sociology: Chapter 1Document4 pagesSociology: Chapter 1Cristina CenturionNo ratings yet
- Sociology 1Document19 pagesSociology 1Cristina CenturionNo ratings yet
- Substance Abuse QuestionsDocument3 pagesSubstance Abuse QuestionsCristina CenturionNo ratings yet
- Ethical Dilemmas in Nursing - Code GrayDocument24 pagesEthical Dilemmas in Nursing - Code GrayCristina Centurion100% (1)
- Cardiac DrugsDocument35 pagesCardiac DrugsCristina Centurion100% (3)
- Sociology: Chapter 1Document4 pagesSociology: Chapter 1Cristina CenturionNo ratings yet
- Sociology: Chapter 1Document4 pagesSociology: Chapter 1Cristina CenturionNo ratings yet
- Child Abuse and NeglectDocument1 pageChild Abuse and NeglectCristina CenturionNo ratings yet
- Impaired Gas Exchange R/T Ventilation-Perfusion Imbalance Care PlanDocument2 pagesImpaired Gas Exchange R/T Ventilation-Perfusion Imbalance Care PlanCristina Centurion100% (10)
- Substance Abuse NclexDocument4 pagesSubstance Abuse NclexCristina Centurion100% (3)
- MCC333E - Film Review - Myat Thu - 32813747Document8 pagesMCC333E - Film Review - Myat Thu - 32813747Myat ThuNo ratings yet
- CH 1 Viscous Fluid Flow Part 1Document29 pagesCH 1 Viscous Fluid Flow Part 1Ammar WahabNo ratings yet
- Group Members: - Muhamad Sahli B Muda - Nurul Hana Balqis Baharom - Napsiah Abdul RahmanDocument18 pagesGroup Members: - Muhamad Sahli B Muda - Nurul Hana Balqis Baharom - Napsiah Abdul RahmanNurul Hana BalqisNo ratings yet
- GR 9 Eng CodebDocument6 pagesGR 9 Eng CodebSharmista WalterNo ratings yet
- 2nd Second Sun of Advent (B)Document4 pages2nd Second Sun of Advent (B)Max PolakNo ratings yet
- Te-Chemical Sem5 CPNM-CBCGS Dec19Document2 pagesTe-Chemical Sem5 CPNM-CBCGS Dec19Mayank ShelarNo ratings yet
- Do Now:: What Is Motion? Describe The Motion of An ObjectDocument18 pagesDo Now:: What Is Motion? Describe The Motion of An ObjectJO ANTHONY ALIGORANo ratings yet
- Chapter 5 IppDocument24 pagesChapter 5 IppRoseann EnriquezNo ratings yet
- UpdateJul2007 3julDocument10 pagesUpdateJul2007 3julAnshul SinghNo ratings yet
- Unit 1 Building A Professional Relationship Across CulturesDocument16 pagesUnit 1 Building A Professional Relationship Across CulturesAlex0% (1)
- LT3845ADocument26 pagesLT3845Asoft4gsmNo ratings yet
- P6 - TT2 - Revision Test 2021-2022 Page 1 of 11Document11 pagesP6 - TT2 - Revision Test 2021-2022 Page 1 of 11Nilkanth DesaiNo ratings yet
- Rare Watches (Christie's) 16. 05. 2016.Document236 pagesRare Watches (Christie's) 16. 05. 2016.Simon LászlóNo ratings yet
- Using Your Digital Assets On Q-GlobalDocument3 pagesUsing Your Digital Assets On Q-GlobalRemik BuczekNo ratings yet
- Operator's ManualDocument110 pagesOperator's ManualAdam0% (1)
- Pull Cord Switch JayashreeDocument1 pagePull Cord Switch JayashreeNCNo ratings yet
- HAF350A User ManualDocument14 pagesHAF350A User ManualUEENo ratings yet
- Kaun Banega Crorepati Computer C++ ProjectDocument20 pagesKaun Banega Crorepati Computer C++ ProjectDhanya SudheerNo ratings yet
- Performance Task 2Document3 pagesPerformance Task 2Edrose WycocoNo ratings yet
- Dress Code19sepDocument36 pagesDress Code19sepapi-100323454No ratings yet
- Gold Loan Application FormDocument7 pagesGold Loan Application FormMahesh PittalaNo ratings yet
- GST RATE LIST - pdf-3Document6 pagesGST RATE LIST - pdf-3Niteesh KumarNo ratings yet
- Bullying Report - Ending The Torment: Tackling Bullying From The Schoolyard To CyberspaceDocument174 pagesBullying Report - Ending The Torment: Tackling Bullying From The Schoolyard To CyberspaceAlexandre AndréNo ratings yet
- Essay On Stem CellsDocument4 pagesEssay On Stem CellsAdrien G. S. WaldNo ratings yet
- STW 44 3 2 Model Course Leadership and Teamwork SecretariatDocument49 pagesSTW 44 3 2 Model Course Leadership and Teamwork Secretariatwaranchai83% (6)
- Collins Ks3 Science Homework Book 3Document5 pagesCollins Ks3 Science Homework Book 3g3pz0n5h100% (1)
- 3DS 2017 GEO GEMS Brochure A4 WEBDocument4 pages3DS 2017 GEO GEMS Brochure A4 WEBlazarpaladinNo ratings yet
- Task of ProjectDocument14 pagesTask of ProjectAbdul Wafiy NaqiuddinNo ratings yet
- Midterm ReviewerDocument20 pagesMidterm ReviewerJonnafe IgnacioNo ratings yet
- Antenatal Care (ANC)Document77 pagesAntenatal Care (ANC)tareNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)