Professional Documents
Culture Documents
Autonomic Nervous System
Uploaded by
Bobet ReñaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Autonomic Nervous System
Uploaded by
Bobet ReñaCopyright:
Available Formats
Many of the great achievements of the world were accomplished by tired and discouraged men who kept on working.
DLS-HSI medicine 2016
Subject: PHARMACOLOGY Topic: AUTONOMIC NERVOUS SYSTEM - 1 Lecturer: MARIA LUISA D. DELACRUZ, MD Date of Lecture: August 5, 2013; 10:00 am READ AT YOUR OWN RISK!
is a set of pathways to and from the central nervous system (CNS) that innervates and regulates smooth muscle, cardiac muscle, and glands is distinct from the somatic nervous system, which innervates skeletal muscle has two divisions: sympathetic and parasympathetic
Dual innervation, which occurs at most sites, means that a body organ receives neural innervation from both sympathetic and parasympathetic neurons on the ANS. Usually the effects are opposing except in the sex organs, in which the effects of SNS and PNS are complementary.
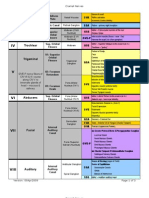
Characteristic Origin of Preganglionic Nerve
Sympathetic Nuclei of spinal cord segments T1T12; L1-L2 (thoracolumbar) Short
Length of preganglionic nerve axon Length of postganglionic nerve axon Preganglionic: Postganglionic fiber Response Location of ganglia
Parasympathetic Nuclei of cranial nerves III, VII, IX, and X; spinal cord segments S2-S4 (craniosacral) Long
Long
Short
1:20 Diffuse Paravertebral ganglia located on the either side of the vertebral column; prevertebral ganglia located anterior to the vertebral column Acetylcholine (Ach) Nicotinic Smooth and cardiac muscles; glands Norepinephrine (except sweat glands, which use Ach) 1, 2, 1, and 2 Prepares the body to cope with emergencies and intense physical activity Fight, flight, fright reaction
1:1 Discrete/Localized Near or in the wall of the target organ
SNS Action Pupillary dilation Eyes (mydriasis) Heart heart rate contractility AV node conduction Vascular smooth Constricts blood muscle vessels in skin; splanchnic Dilates blood vessels in skeletal muscle Gastro-intestinal motility tract Constricts sphincters Bronchioles Dilates bronchiolar smooth muscle Bladder Relaxes bladder wall Constricts sphincters sweating sweating lipolysis Ejaculation
NS;
Organ
PNS Action Pupillary constriction (miosis) heart rate contractility (Atria) AV node conduction -
motility Relaxes sphincters Constricts bronchiolar smooth muscle Contracts bladder wall Relaxes sphincters Erection
NS
Sweat glands Kidney Fat cells Male sex organs
Point and Shoot:
oint erection
hoot Ejaculation
Neurotransmitter in pre-ganglion fiber Receptor type in ganglion Effector organs
Acetylcholine (Ach) Nicotinic Smooth and cardiac muscles; glands Acetylcholine (Ach)
Neurotransmitter in effector organs (post-ganglionic) Receptor types in effector organs Functions
Muscarinic Conserves energy and replenishes energy stores; maintains homeostasis Rest and digest
Neurons do not act in isolation. They are connected via cell - cell interactions called SYNAPSES.
PHARMACOLOGY: AUTONOMIC NERVOUS SYSTEM 1
| Page 1 of 8
DLS-HSI medicine 2016
There are two types of synapses: Chemical makes use of neurotransmitters Electrical utilizes ions b. HETERORECEPTOR respond to neurotransmitters, neuromodulator or neurohormones released from neurons or cells in the other system may be inhibitory or excitatory Examples: o Ach acting on M2 and M4 receptors inhibit release of NE from sympathetic neurons o NE acting on a2 receptors stimulate the release of Ach from parasympathetic neurons o NE acting on a2 receptors stimulate the release of serotonin from serotonergic neurons respond to neurotransmitter released by another neuron; may be inhibitory or excitatory
Structure of Chemical Synapse
2.
1921 Otto Loewi stimulate vagus nerve heart rate decreases Loewi hypothesized that stimulation of the vagus released a chemical first proof of chemical mediation of nerve action 1926 - Acetylcholine
POSTSYNAPTIC RECEPTORS located in the outer membrane of the postsynaptic neuron interaction with neurotransmitter result in localized increase in ionic permeability or conductance of the membrane Examples: o 1adrenoceptors o muscarinic receptors
Interaction with postsynaptic receptors
Production of post junctional potential
permeability to Na+ and Ca++ EPSP permeability to Cl IPSP permeability to K+ IPSP
EPSP results in depolarization while IPSP results in hyperpolarization
Before Loewi's experiments, it was unclear whether signalling across a synapse was bioelectrical or chemical. Loewi's famous experiment, published in 1921, largely answered this question. According to Loewi, the idea for his key experiment came to him in his sleep. He dissected out of frogs two beating hearts: one with the vagus nerve which controls heart rate attached, the other heart on its own. Both hearts were bathed in a saline solution (i.e. Ringer's solution). By electrically stimulating the vagus nerve, Loewi made the first heart beat slower. Then, Loewi took some of the liquid bathing the first heart and applied it to the second heart. The application of the liquid made the second heart also beat slower, proving that some soluble chemical released by the vagus nerve was controlling the heart rate. He called the unknown chemical Vagusstoff. It was later found that this chemical corresponded to Acetylcholine.
1. 2. Axonal conduction Junctional transmission 2.1 Release of neurotransmitter 2.2 Interaction with receptors 2.3 Production of response Termination of neurotransmitter action
a. b.
Reuptake (primarily) Enzymatic degradation Acetylcholinesterase (AChE) in PSNS Catechol-O-methyltransferase (COMT), monoamine oxidase (MAO) in SNS
3.
1.
PRESYNAPTIC RECEPTORS a. AUTORECEPTOR located in or close to axon terminals of a neuron through which the neurons own neurotransmitter can modify neurotransmitter synthesis and release Examples: o Acetylcholine (Ach) released from parasympathetic neurons interact with M 2 or M4 receptors to enhance Ach release o Norepinephrine (NE) released from sympathetic neurons interact with a2 receptors to inhibit release of NE inhibit or enhance release of neurotransmitter by the same neuron
Synthesis of Acetylcholine from Acetyl-CoA and Choline and its enzymatic degradation by acetylcholinesterase (AChE)
Enzymatic degradation of catecholamines by COMT and MAO
PHARMACOLOGY: AUTONOMIC NERVOUS SYSTEM 1
| Page 2 of 8
DLS-HSI medicine 2016
MUSCARINIC RECEPTORS Subtype Location M1 CNS, gastric parietal cells, autonomic ganglia M2 Heart a. b. c. Inhibits Acetylcholine transport to the neuron terminal Hemicholinium Vesamicol Inhibits Acetylcholine release Botulinum toxin Stimulate Acetylcholine release Acetylcholine Latrotoxin o black widow spider Agonist / Antagonist at receptor site Interferes with destruction of neurotransmitter Acetylcholinesterase Inhibitor M3 M4 M5 smooth muscles, eye, secretory gland, endothelium CNS CNS G protein Gq PLC pathway Gi cAMP pathway Gq PLC pathway Gi cAMP pathway Gq PLC pathway
d. e.
Hemicholinium
NICOTINIC RECEPTORS Subtype Location Nm Neuromuscular junction Nn Autonomic ganglia, adrenal medulla Nn CNS (post synaptic / presynaptic
Signal Transduction permeability to Na+ permeability to Na+ permeability to Na+ permeability to Ca++
Vesamicol
Botulinum toxin
DIRECTLY-ACTING Natural and Naturally Synthetic Choline Occurring esters Cholinomimetic Alkaloids Acetylcholine Muscarine Methacholine Pilocarpine (Acetyl-b-methyl Arecoline choline) Nicotine Carbachol (Carbamyl choline) Bethanechol (Carbamyl methyl choline)
INDIRECTLY-ACTING Acetylcholinesterase Inhibitors
(do not directly act on the receptors)
M1 and M3
Activation of Gq-PLC pathway Hydrolysis of phosphoinositides to IP3 and DAG Mobilization of intracellular Ca++
M2 and M4
Activation of Gi cAMP pathway inhibit adenyl cyclase cAMP enhanced K+ conductance
hyperpolarization
a. Specific (True acetylcholinesterase) Neurons Synaptic clefts Neuromuscular junction Red blood cells Nonspecific (Pseudo-butyryl cholinesterase) Glial cells Plasma Liver Other organs
Subtype M1
Receptor Type
Postsynaptic
Location CNS
b.
Autonomic ganglia Gastric parietal cells Heart
M2
MUSCARINIC RECEPTORS
90% of cholinergic receptors in peripheral nervous system and brain slow, either excitatory or inhibitory G-protein coupled
NICOTINIC RECEPTORS
10% of cholinergic receptors in peripheral nervous system and brain fast, excitatory Ligand gated ion channels (sodium) activation increase permeability to Na+
Presynaptic Inhibitory (auto/hetero receptor)
M3
Postsynaptic
M4
Presynaptic Inhibitory
(auto/hetero receptor)
Smooth muscles Eye Secretory gland Endothelium CNS
Action memory, arousal, attention and analgesia Nicotinic cholinergic transmission in the ganglia Increase gastric acid secretion Decrease conduction velocity at sinoatrial and atrioventricular nodes decreased heart rate Contraction of smooth muscles miosis secretion of glands vasodilatation
M5
Postsynaptic
CNS
PHARMACOLOGY: AUTONOMIC NERVOUS SYSTEM 1
| Page 3 of 8
DLS-HSI medicine 2016
3. 1. Central nervous system all muscarinic receptor subtypes present cognitive function, motor control, appetite regulation, nociception, memory, arousal, attention Cardiovascular system Direct effect o activation of M2 receptor in the SA node and atrial muscles Indirect effect o inhibition of NE release from sympathetic nerve terminals Remember, the muscarinic receptor present in the heart is M2, a presynaptic inhibitory type of receptor, which when acted upon by acetylcholine leads to hyperpolarization. Hyperpolarization of SA node: o (-)chronotropic effect decreased heart rate bradycardia Hyperpolarization of cardiac muscles: o (-) inotropic effect decreased force of contraction more effect on atrial muscles less dense cholinergic innervation of ventricles decrease rate of conduction in sinoatrial (SA) and atrioventricular (AV) nodes (-) dromotropic effect dilatation of blood vessels o Direct effect mediated by nitric oxidase synthase which synthesizes nitric oxide M3 is the muscarinic receptor found in endothelial cells Ocular M3 receptors in the constrictor pupillae and ciliary muscles
M3 in the constrictor pupillae
Contraction of constrictor pupillae muscle
2.
Miosis (pupillary constriction)
contraction of ciliary muscles accommodation loss of accommodation for far vision decrease IOP
4.
Gastrointestinal tract increase tone and amplitude of contraction increase secretory activity of glands in the stomach and intestines Genitourinary tract increase tone of detrusor muscle increase voiding pressure increase ureteral peristalsis relaxation of trigone and sphincter Respiratory increase secretion of tracheobronchial glands contraction of bronchial smooth muscles Other Glands increase secretions salivary sweat lacrimal pancreatic Sexual Function stimulate penile and clitoral arousal erection
5.
Activation of M3 by acetylcholine
Activation of nitric oxide synthase (NOS) NOS converts arginine to nitric oxide Nitric Oxide (NO) Nitric oxide (NO) will activate guanyl cyclase Guanyl cyclase converts GTP to cGMP cGMP Smooth muscle relaxation Vasodilation
8. 7. 6.
Acetylcholine Metacholine Carbachol Bethanechol Muscarine Pilocarpine
CVS ++ +++ + ++ +
GIT ++ ++ +++ +++ +++ +++
GUT ++ ++ +++ +++ +++ +++
RT ++ +++ -
Eye + + ++ ++ ++ ++
Glands ++ ++ ++ ++ +++ +++
Indirect Effect inhibition of the release of NE from adrenergic nerve endings mediated by Ach Net effect on BP: decreased BP hypotension o Vasodilation can lead to decreased total peripheral resistance (TPR) o The negative chronotropic effect can lead to decreased heart rate hence decrease in cardiac output (CO) o
Subtype Nm
Location Neuromuscular junction
Signal Transduction permeability to Na+
Effects Excitatory: Depolarization muscle contraction Excitatory: Depolarization of postganglionic neuron Secretion of catecholamine s Postsynaptic: Excitatory (depolarization of postsynaptic neuron) Presynaptic: control neurotransmitter release ( release)
Nn
Autonomic ganglia, adrenal medulla
permeability to Na+
Nn
CNS (post synaptic / presynaptic
permeability to Na+
permeability to Ca++
PHARMACOLOGY: AUTONOMIC NERVOUS SYSTEM 1
| Page 4 of 8
DLS-HSI medicine 2016
Amanita muscaria - a poisonous mushroom produce mycetism contains the alkaloid muscarine and amatoxins from which was derived the name muscarinic receptor
1. 2. 3.
Autonomic ganglia PSNS and SNS adrenal medulla Epinephrine Neuromuscular junction depolarization contraction Central nervous system low dose excitatory high dose inhibitory
fatal dose of nicotine is approximately 40 mg, or 1 drop of the pure liquid equivalent to two regular cigarettes most of the nicotine in cigarettes is destroyed by burning or escapes via the "sidestream" smoke
Presence of methyl group less activity at nicotinic receptors Examples: o Methacholine o Bethanechol Carbamic acid esters are RESISTANT to hydrolysis by Acetylcholinesterase Examples: o Bethanechol o Carbachol
ACUTE NICOTINE TOXICITY 1. CNS stimulation Convulsions Coma respiratory arrest 2. Neuromuscular blockade skeletal muscle paralysis respiratory failure 3. Hypertension and cardiac arrhythmias CHRONIC NICOTINE TOXICITY 1. Addiction 2. Increase risk for coronary artery disease 3. Increase incidence of recurrences of peptic ulcer 4. Increase risk for malignancy
Susceptibility to Acetylcholinesterase Acetylcholine Methacholine Carbachol Betanechol Pilocarpine Muscarine +++ + -
Receptor Specificity Muscarinic +++ +++ ++ +++ ++ +++ Nicotinic ++ + +++ -
prevent hydrolysis of acetylcholine produce accumulation of acetylcholine at the cholinergic nerve terminals enhance cholinergic neurotransmission
Lipid solubility Oral absorption CNS penetration Excretion Examples
Quarternary Amine Less lipid soluble Poor Limited Kidneys (rapidly) Acetylcholine Betanechol Carbachol Metacholine Muscarine
Tertiary Amine More lipid soluble Good Good Kidneys; enhanced by acidification Arecholine Pilocarpine
Quarternary Amine Edrophonium Neostigmine Pyridostigmine Echothiphate
Tertiary Amine Tacrine/Donepezil Physostigmine Diisopfluorophosphate
Drug Acetylcholine
* has very short duration of action
Formulation 1% Ophthalmic solution Powder Diluted with 0.9% sodium chloride and administered via a nebulizer 0.01-3% Ophthalmic solution 5 mg, 10 mg, 25 mg or 50 mg Tablet
Methacholine
Therapeutic Use Induction of miosis during ophthalmologic surgery Diagnosis of bronchial airway hyperreactivity
Free AChE
Treatment of glaucoma; Induction of miosis during surgery Treatment of urinary retention (postoperative urinary retention, diabetic autonomic neuropathy, neurogenic bladder); postoperative abdominal distention, gastric atony, gastroparesis, adynamic ileus, and gastroesophageal reflux Treatment of glaucoma and as a miotic agent Xerostomia
Acetylated AChE
Carbachol
Bethanechol
Phosphorylated AChE
Carbamoylated AChE
Site of Action Central Peripheral Peripheral Peripheral Peripheral Peripheral Peripheral and Central
Pilocarpine
0.5-6% Ophthalmic solution or Ocular insert 5-10 mg Tablet
Tacrine / Donepezil Edrophonium Physostigmine Nesotigmine Pyridostigmine Echothiophate Diisopfluorophosphate (DFP)
Resultant Acetylcholinesterase Acetylated Acetylated Carbamoylated Carbamoylated Carbamoylated Phosphorylated Phosphorylated
PHARMACOLOGY: AUTONOMIC NERVOUS SYSTEM 1
| Page 5 of 8
DLS-HSI medicine 2016
synthetic quaternary ammonium compound more polar do not pass thru the BBB 2-4 hrs duration of action dual action o reversible acetylcholinesterase inhibitor o direct activation of nicotinic receptor at the motor end plate beneficial in Myasthenia Gravis antidote for toxicity to Non-depolarizing Neuromuscular blocker
Edrophonium Tacrine Donepezil
Edrophonium binds to the ionic site of acetylcholinesterase. It is a short-acting inhibitor of acetylcholinesterase. EDROPHONIUM Quarternary amine Moderate Peripheral nervous system Rapid (10-20 mins) Diagnosis of myasthenia gravis (MG) TACRINE/DONEPEZIL Tertiary amine High Central Long Alzheimers Disease
Chemical structure Affinity for Acetylcholinesterase Site of action Duration of action Therapeutic use
synthetic quarternary ammonium compound used for long term treatment of Myasthenia gravis longer duration of action (4-6 hrs)
Carbamate Inhibitors o reversible Organophosphate Inhibitors o irreversible
inihibitory effect onacetylcholinesterase similar to organophosphates Pralidoxime use in carbamate toxicity can reduce the clinical severity mixed poisoning with organophosphorus compounds is common
These agents are esters of carbamic acid. The general formula is below.
Basic structure of Organophosphate Inhibitors react covalently with the enzyme at the esteratic site serve as true hemisubstrates Phosphorylated enzyme is extremely stable loss of physiologic function of the enzyme return of AchE activity depends on the synthesis of new enzyme stability of the phosphorylated enzyme is enhanced through aging which results from the loss of one alkly group
Carbamic acid
Basic structure of carbamyl inhibitors
Carbamylation and phosphorylation of AChE
react covalently with the enzyme at the esteratic site act as alternate substrate for Acetylcholinesterase hydrolyzed by Acetylcholinesterase much more slowly than Ach carbamylated enzyme is more stable; half-life is 15-30 minutes in vivo, the duration of inhibition by the carbamoylating agents is 3-4 hours enzyme function is NOT altered carbamoylated enzyme does not undergo aging spontaneous hydrolysis with consequent inactivation of the compound recovery of enzyme activity within several hours Examples: o Physostigmine o Neostigmine o Pyridostigmine o Ambenonium o Demecarium o Carbamate Insecticides: Propoxur Carbaryl Aldicarb
AChE, phosphorylated and inhibited by DFP
Examples: o Diisofluorophosphate (DFP) o Insecticides Malathion Parathion Diazinon Chlorpyrifos Malaoxon Paraoxon o Nerve gases Sarin Tabun Soman o Echothiophate iodide
Aged AChE
an alkaloid obtained from Physostigma venenosum tertiary amine 2-4 hours duration of action Topical formulation for treatment of glaucoma Systemic formulation for treatment of myasthenia
PHARMACOLOGICAL PROPERTIES OF ORGANOPHOSPHATES highly lipid soluble EXCEPT Echothiophate effectively absorbed from all routes endogenous Ach stimulates all cholinergic receptors (peripheral and CNS) low volatility and stability in aqueous solutions widely used as insecticides employed for home, garden and agricultural use converted to active metabolites by CYPs Malaoxon is derived from Malathion Paraoxon is derived from Parathion Parathion now phase out due to severe toxicity also use in suicide attempts or deliberate poisoning also used topically in the treatment of Pediculosis (lice infestations)
PHARMACOLOGY: AUTONOMIC NERVOUS SYSTEM 1
| Page 6 of 8
DLS-HSI medicine 2016
high lipid solubility low molecular weight highly volatile absorbed from all routes: inhalation, transdermal and GIT absorption CNS penetration Antidote for Toxicity to: Anticholinergic drugs Tricyclic antidepressants Nondepolarizing (Competitive) neuromuscular blockers Pediculosis treatment of head and body lice Physostigmine, Neostigmine
Carbaryl Malathion
most potent synthetic toxins known extremely toxic used in warfare and terrorism attacks o March 20, 1995 Tokyo Sarin Attack
MYSTHENIC CRISIS vs CHOLINERGIC CRISIS
MYASTHENIC CRISIS extreme muscle weakness occurs due to inadequate medication (insufficient Ach at NMJ) There is improvement when given with Edrophonium (Tensilon) Treatment: Neostigmine, Pyridostigmine CHOLINERGIC CRISIS extreme muscle weakness caused by an overdose of a cholinesterase inhibitor (excessive cholinergic stimulation) Symptoms worsen when given with Edrophonium (Tensilon) Treatment: Atropine
only organophosphate used clinically ophthalmic use low lipid solubility non volatile
may be sequestered in lipids for long periods of time lipid soluble organophosphates are well absorbed from the skin volatile agents are transferred readily across the alveolar membrane COMPARISON OF ORGANOPHOSPHATES AND CARBAMATES
1.
2.
3.
Pesticides Propoxur Malathion Parathion Chemical warfare Sarin Soman Tabun Suicide (Deliberate poisoning)
1. 2. 3. 4.
Cholinergic syndrome Intermediate syndrome Organophosphate-induced delayed neuropathy (OPIDN) Organophosphorus-ester-induced chronic neurotoxicity (OPICN)
acute phase of acetylcholinesterase poisoning signs and symptoms result from activation of both muscarinic and nicotinic receptors vary depending on the balance bet muscarinic and nicotinic stimulation
CONDITIONS Glaucoma Xerostomia Gastrointestinal tract conditions Postoperative abdominal distension Gastric atony or gastroparesis adynamic ileus due to toxic states congenital megacolon Genitourinary tract conditions postoperative or postpartum urinary retention chronic hypotonic, myogenic, or neurogenic bladder partial sensory or motor paralysis of the bladder after spinal injury Myasthenia gravis neuromuscular disease characterized by severe weakness and fatigability of skeletal muscles loss of nicotinic receptors due to autoimmune mechanisms use of acetylcholinesterase inhibitors to increase Ach to stimulate limited receptors Alzheimers disease a neurodegenerative disease believed to be associated with decrease functioning of the cholinergic system in the brain
CHOLINERGIC AGONISTS Acute: Pilocarpine Chronic: Echothiophate Pilocapine Bethanechol Neostigmine
MANIFESTATIONS: 1. Clinical Signs due to Muscarinic Stimulation D diarrhea, diaphoresis U urination M miosis (pupillary constriction) B bradycardia, bronchospasm E emesis L lacrimation S salivation 2. Clinical Signs due to Nicotinic stimulation Mnemonic Monday Mydriasis Tuesday Tachycardia Wednesday Weakness and paralysis Thursday Hypertension Friday Fasciculations CNS effects confusion ataxia slurred speech generalized convulsions respiratory depression coma
Bethanechol Neostigmine 3.
For Diagnosis: Edrophonium (Tensilon Test) For Treatment: Neostigmine, Pyridostigmine
DIAGNOSIS: History of exposure Characteristic signs and symptoms Determination of RBC Cholinesterase activity
Tacrine Donezepil
PHARMACOLOGY: AUTONOMIC NERVOUS SYSTEM 1
| Page 7 of 8
DLS-HSI medicine 2016
TREATMENT: 1. Prevention of secondary exposure 2. Supportive care 3. Antidote Atropine o Administer Atropine until full atropinization is achieved o Atropine effects are observed when there is increased heart rate and mydriasis Pralidoxime
4. The decrease in total peripheral resistance produced by cholinergic agonists is mediated by: a. Decrease in heart rate b. Release of cyclic GMP c. Blockade of alpha 1 receptors d. All of the above A decreased in blood pressure is observed after acetylcholine administration. This is attributed to: a. A decrease in total peripheral resistance b. A decrease in heart rate c. Decrease in cardiac output d. All of the above e. A and B only Hyperpolarization of the SA node results from activation of which of the cholinergic receptor? a. M3 b. M2 c. Nm d. Nn This choline ester has a long duration because it is resistant to hydrolysis by acetylcholinesterase? a. Methacholine b. Carbachol c. Bethanechol d. All of the above e. B and C only The cholinomimetic alkaloid that activate the muscarinic receptor but does not activate the nicotinic receptor: a. Pilocarpine b. Carbachol c. Neostigmine d. Acetylcholine Cholinergic agonist/s with less effects on the cardiovascular system will include: a. Pilocarpine b. Muscarine c. Carbachol d. All of the above e. A and C only This drug is used to regenerate phosphorylated acetylcholinesterase: a. Atropine b. Pralidoxime c. Both A and B d. Neither A nor B Which ion channel is linked to the nicotinic receptor? a. Na+ b. Clc. K+ d. Ca++ Which muscarinic receptor is linked to the cyclic AMP system? a. M1 b. M2 c. M3 d. All of the above e. A and C only The best recommended treatment for cholinergic crisis will include: a. pyridostigmine b. neostigmine c. atropine d. A and B only e. All of the above Drug/s that deplete the cholinergic nerve ending of its neurotransmitter include/s: a. Vesamicol b. Botulinum toxin c. Latrotoxin d. All of the above e. A and B only Fatality from organophosphate poisoning is usually due to: a. Cardiac arrhythmias b. Respiratory depression c. Anaphylactic shock d. All of the above e. A and B only
5.
ENZYME REACTIVATORS
Pralidoxime Obidoxime
6.
PRALIDOXIME 2-PAM (2-pyridine aldoxime methyl chloride) belongs to a class of chemicals, called oximes reverse the binding of cholinesterase inhibitors with acetylcholinesterase reverses the phosphorylation of cholinesterase improves neural synaptic transmission corrects muscle weakness and paralysis should be used within 24 hours of exposure early
7.
delayed onset of muscular weakness and paralysis occur between 24-96 hrs (1-4 days) after resolution of acute cholinergic syndrome and onset of OPIDN attributed to recirculation of cholinesterase inhibitors from adipose tissue major cause of morbidity and mortality Without hypoxic damage, spontaneously resolves in 1-2 weeks
8.
9.
rare delayed neurotoxic effect occurs 1-5 weeks after acute cholinergic syndrome symmetrical degeneration of spinal cord and peripheral nerves initial symptoms: sharp, crampy pain in the legs followed by stepping gait, quadriplegia damage to pyramidal tracts motor loss can be permanent
10.
11.
long term, persistent neuropsychiatric disorder Clinical findings consistent with brain damage due to hypoxia and seizures no specific treatment
12.
13.
JOHN PAUL II
14.
PRACTICE QUESTIONS
1. The activation of muscarinic receptors in bronchiolar smooth muscle is associated with a. activation of adenylyl cyclase b. decrease in CAMP formation mediated by G-proteins c. increase in IP3 and DAG d. inhibition of protein kinase C e. opening of Na+/K+ cation channels This organophosphate is a nerve gas commonly used in terrorist attack or for chemical warfare? a. carbaryl b. propoxur c. sarin d. malathion e. all of the above Activation of cholinergic receptors in the adrenal medulla will produce: a. Increased total peripheral resistance b. Increased cardiac output c. Neither A nor B d. Both A and B
15.
2.
3.
Itsmebob8
| Page 8 of 8
PHARMACOLOGY: AUTONOMIC NERVOUS SYSTEM 1
You might also like
- Nervous System: A Tutorial Study GuideFrom EverandNervous System: A Tutorial Study GuideRating: 5 out of 5 stars5/5 (1)
- Introduction To ANS PharmacologyDocument34 pagesIntroduction To ANS PharmacologySebontu HasenNo ratings yet
- Effects of Autonomic Nervous System on OrgansDocument29 pagesEffects of Autonomic Nervous System on Organssanaya100% (1)
- (See Next Diagram) : Autonomic Nervous System Rashelle Lopez-Salvatierra, MD Somatic DivisionDocument7 pages(See Next Diagram) : Autonomic Nervous System Rashelle Lopez-Salvatierra, MD Somatic Divisionemely p. tango100% (4)
- Autonomic Nervous SystemDocument6 pagesAutonomic Nervous SystemSUTHAN100% (4)
- Autonomic: System E ReviewDocument93 pagesAutonomic: System E ReviewokNo ratings yet
- ANS Pharmacology - Introduction - Review of The Autonomic Nervous SystemDocument79 pagesANS Pharmacology - Introduction - Review of The Autonomic Nervous SystemMarc Imhotep Cray, M.D.100% (1)
- Cholinergic DrugsDocument32 pagesCholinergic DrugsApt FianNo ratings yet
- Adrenergic AgentsDocument57 pagesAdrenergic AgentsAn Lo100% (1)
- ANS PharmacologyDocument58 pagesANS Pharmacologyalemu100% (1)
- Cardiovascular Pharmacology: - Hypertension - Angina Pectoris - Cardiac Arrhythmias - Heart FailureDocument31 pagesCardiovascular Pharmacology: - Hypertension - Angina Pectoris - Cardiac Arrhythmias - Heart Failurelynch775100% (2)
- Autonomic Nervous System: Parasympathetic and Sympathetic DivisionsDocument107 pagesAutonomic Nervous System: Parasympathetic and Sympathetic DivisionsMaria Mercedes LeivaNo ratings yet
- Introduction to Autonomic PharmacologyDocument24 pagesIntroduction to Autonomic PharmacologyChacha ChachaNo ratings yet
- Drugs Affecting The Autonomic Nervous SystemDocument53 pagesDrugs Affecting The Autonomic Nervous SystemMatt Stone100% (1)
- Cholinergic Drug MnemonicsDocument1 pageCholinergic Drug Mnemonicssunshine151100% (1)
- Autonomic Nervous System - HandoutsDocument5 pagesAutonomic Nervous System - HandoutsKelly Trainor100% (1)
- Pharmacodynamics BDS97Document42 pagesPharmacodynamics BDS97Dr.U.P.Rathnakar.MD.DIH.PGDHM100% (2)
- Topic 2 - Adrenergic DrugsDocument52 pagesTopic 2 - Adrenergic DrugsAngeli Gregorio100% (1)
- Neurotransmitter Cheat Sheet AP ReviewDocument2 pagesNeurotransmitter Cheat Sheet AP ReviewNathania DawitNo ratings yet
- Onco PharmacologyDocument9 pagesOnco Pharmacologyarn0ld21No ratings yet
- Spinal Tracts: DR - Krishna Madhukar Dept. of Orthopaedics Bharati HospitalDocument65 pagesSpinal Tracts: DR - Krishna Madhukar Dept. of Orthopaedics Bharati HospitalKrishna Madhukar100% (1)
- Cardiovascular SystemDocument10 pagesCardiovascular SystemGlen DaleNo ratings yet
- Medical and Surgical Nursing Notes For NLEDocument63 pagesMedical and Surgical Nursing Notes For NLEBel Zeta DonaireNo ratings yet
- Cranial Nerves SummaryDocument3 pagesCranial Nerves SummaryJoash F. Pacquing75% (4)
- Anatomy and Physiology of BrainDocument21 pagesAnatomy and Physiology of BrainNavjot BrarNo ratings yet
- Autonomic Nervous System AgentsDocument14 pagesAutonomic Nervous System AgentsRhenier S. Ilado100% (1)
- Cranial NervesDocument9 pagesCranial Nervesangrypandasaredangerous100% (4)
- ANS Pharmacology-Cholinergic AgentsDocument55 pagesANS Pharmacology-Cholinergic AgentsMarc Imhotep Cray, M.D.No ratings yet
- Adrenergics & Adrenergic BlockersDocument5 pagesAdrenergics & Adrenergic Blockersapi-3739910100% (4)
- Reflex PhysiologyDocument46 pagesReflex Physiologysharmaine_ting100% (1)
- Autonomic Nervous SystemDocument55 pagesAutonomic Nervous SystemtiiandiNo ratings yet
- Anatomy Cranial NervesDocument3 pagesAnatomy Cranial NervesMedShare100% (1)
- ANS-Pharmacology Adrenergic DrugsDocument65 pagesANS-Pharmacology Adrenergic DrugsMarc Imhotep Cray, M.D.75% (4)
- Introduction To CNS PharmacologyDocument13 pagesIntroduction To CNS PharmacologyDr.U.P.Rathnakar.MD.DIH.PGDHM100% (1)
- Receptor Pharmacology Cheat Sheet (4f6203b546fa5)Document5 pagesReceptor Pharmacology Cheat Sheet (4f6203b546fa5)sinthreckNo ratings yet
- Basic Principles of PharmacologyDocument13 pagesBasic Principles of Pharmacologyemmanuel100% (1)
- 05 Cardiovascular System PhysiologyDocument34 pages05 Cardiovascular System PhysiologyKaye Alyssa EnriquezNo ratings yet
- Beta Lactam AntibioticsDocument28 pagesBeta Lactam AntibioticsHassan.shehri100% (11)
- Adrenergic Receptor ChartDocument1 pageAdrenergic Receptor ChartAnkit Mehta75% (4)
- Adrenergic and Anti-Adrenergic DrugsDocument54 pagesAdrenergic and Anti-Adrenergic DrugsChittaranjan Padhy100% (1)
- Renal PhysiologyDocument87 pagesRenal PhysiologyQusaiBadrNo ratings yet
- PHARMACOLOGY of ANS (Synopsis For Students)Document16 pagesPHARMACOLOGY of ANS (Synopsis For Students)JIEHASMARTNo ratings yet
- Drug ChartDocument8 pagesDrug Chartstudentalwaysstudy100% (1)
- Physiology Cardiovascular Physiology NotesDocument13 pagesPhysiology Cardiovascular Physiology Noteshedayatamin44No ratings yet
- Mnemonics For PharmacologyDocument14 pagesMnemonics For Pharmacologyloftysingh100% (8)
- Common Cardiac Drugs for Angina and StentingDocument13 pagesCommon Cardiac Drugs for Angina and StentingDonna Deala100% (2)
- Tracts of The Spinal CordDocument21 pagesTracts of The Spinal Corddr.a.k.gupta6924100% (10)
- Central Nervous System Pharmacology: Elly Nurus SakinahDocument64 pagesCentral Nervous System Pharmacology: Elly Nurus Sakinahkareem92No ratings yet
- Antiarrhythmic Agents Lecture NotesDocument6 pagesAntiarrhythmic Agents Lecture NotesErnest Patrick MatiasNo ratings yet
- Nervous SystemDocument4 pagesNervous SystemEllanny GloriaNo ratings yet
- Endocrine PharmacologyDocument42 pagesEndocrine PharmacologyAhmed El SharkawyNo ratings yet
- NeurotransmittersDocument92 pagesNeurotransmittersClare DucutNo ratings yet
- X.0Y Control of Peripheral CirculationDocument4 pagesX.0Y Control of Peripheral CirculationAya ARNo ratings yet
- Regulation RespirationDocument34 pagesRegulation Respirationkiedd_04100% (2)
- (OS 213) LEC 03 Drugs Acting On The Respiratory System (1) - 1Document16 pages(OS 213) LEC 03 Drugs Acting On The Respiratory System (1) - 1Yavuz DanisNo ratings yet
- Anti-Epileptic Drugs GuideDocument48 pagesAnti-Epileptic Drugs GuideShubha DiwakarNo ratings yet
- Visually Memorable Neuroanatomy for BeginnersFrom EverandVisually Memorable Neuroanatomy for BeginnersRating: 5 out of 5 stars5/5 (1)
- SSTIDocument1 pageSSTIBobet ReñaNo ratings yet
- CRBSI QUIZ - ANSWER KEY (With Rationale)Document7 pagesCRBSI QUIZ - ANSWER KEY (With Rationale)Bobet ReñaNo ratings yet
- Lung Abscess Causes and TreatmentDocument28 pagesLung Abscess Causes and TreatmentBobet ReñaNo ratings yet
- Names PDFDocument1 pageNames PDFBobet ReñaNo ratings yet
- Anatomy of The BrainDocument46 pagesAnatomy of The BrainBobet ReñaNo ratings yet
- Cheat Sheet in Research: The 2X2 Table / Contingency TableDocument6 pagesCheat Sheet in Research: The 2X2 Table / Contingency TableBobet ReñaNo ratings yet
- RITM Advisory NCOVDocument33 pagesRITM Advisory NCOVBobet ReñaNo ratings yet
- Crbsi Quiz - Answer KeyDocument2 pagesCrbsi Quiz - Answer KeyBobet ReñaNo ratings yet
- Skin Infections, Cellulitis, and Subcutaneous Tissue DiseasesDocument75 pagesSkin Infections, Cellulitis, and Subcutaneous Tissue DiseasesBobet ReñaNo ratings yet
- Graduation Programme 2020Document1 pageGraduation Programme 2020Bobet ReñaNo ratings yet
- NIHSSDocument1 pageNIHSSBobet Reña100% (1)
- Mary Mediatrix Medical Center: Department of Internal MedicineDocument4 pagesMary Mediatrix Medical Center: Department of Internal MedicineBobet ReñaNo ratings yet
- Names PDFDocument1 pageNames PDFBobet ReñaNo ratings yet
- Problem List: Date Entered Date ResolvedDocument1 pageProblem List: Date Entered Date ResolvedBobet ReñaNo ratings yet
- Finals QuestionsDocument10 pagesFinals QuestionsBobet ReñaNo ratings yet
- BelieveDocument1 pageBelieveBobet ReñaNo ratings yet
- Harrison's Hour Lung and Urinary QuestionsDocument2 pagesHarrison's Hour Lung and Urinary QuestionsBobet ReñaNo ratings yet
- MyxedemaDocument3 pagesMyxedemaBobet ReñaNo ratings yet
- Harrison's Hour - Sepsis Bundle 2016Document5 pagesHarrison's Hour - Sepsis Bundle 2016Bobet Reña100% (1)
- Find the value of xDocument1 pageFind the value of xBobet ReñaNo ratings yet
- Tuberculoid vs Lepromatous Leprosy FeaturesDocument1 pageTuberculoid vs Lepromatous Leprosy FeaturesBobet ReñaNo ratings yet
- Bartter Syndrome Vs Gitelman SyndromeDocument1 pageBartter Syndrome Vs Gitelman SyndromeBobet ReñaNo ratings yet
- Ralph Reña's Grade IV Math Word ProblemsDocument1 pageRalph Reña's Grade IV Math Word ProblemsBobet ReñaNo ratings yet
- Pancit Canton IngredientsDocument1 pagePancit Canton IngredientsBobet ReñaNo ratings yet
- Orientation CourseDocument46 pagesOrientation CourseBobet Reña82% (11)
- Adrenergic ReceptorsDocument1 pageAdrenergic ReceptorsBobet ReñaNo ratings yet
- Harrison's Hour - Sepsis Bundle 2016Document5 pagesHarrison's Hour - Sepsis Bundle 2016Bobet Reña100% (1)
- Ralph Reña's Grade IV Math Word ProblemsDocument1 pageRalph Reña's Grade IV Math Word ProblemsBobet ReñaNo ratings yet
- Ralph Reña's Grade IV Math Word ProblemsDocument1 pageRalph Reña's Grade IV Math Word ProblemsBobet ReñaNo ratings yet
- Water Soluble VitaminsDocument1 pageWater Soluble VitaminsBobet ReñaNo ratings yet
- PHA3801 Short Answer QuestionsDocument5 pagesPHA3801 Short Answer QuestionsFarhana Azmira AsmadiNo ratings yet
- Autonomic Nervous System DrugsDocument111 pagesAutonomic Nervous System DrugsCres Padua QuinzonNo ratings yet
- CFNP TAP Review - AtropineDocument43 pagesCFNP TAP Review - AtropineJunmajNo ratings yet
- MediaDocument659 pagesMediaMahima FamousNo ratings yet
- Pharma Final ModuleDocument139 pagesPharma Final ModuleQuantum XavierNo ratings yet
- Cosmeceutical Peptides in The Framework of Sustainable Wellness EconomyDocument8 pagesCosmeceutical Peptides in The Framework of Sustainable Wellness EconomyNgọc NguyễnNo ratings yet
- Pumhs Pharma McqsDocument3 pagesPumhs Pharma McqsAzra BalochNo ratings yet
- Biology Notes For Unit 5Document84 pagesBiology Notes For Unit 5nhmerali7860% (1)
- Facial Asymmetry in Patients With Hemifacial SpasmDocument7 pagesFacial Asymmetry in Patients With Hemifacial Spasmkleitons NoguerjpaNo ratings yet
- Katzung SummaryDocument60 pagesKatzung Summaryedwarbc1No ratings yet
- HyperhidrosisDocument7 pagesHyperhidrosisNurhafizahImfistaNo ratings yet
- Introduction To Autonomic PharmacologyDocument55 pagesIntroduction To Autonomic PharmacologyMuammar Alfarouq100% (1)
- Ball - Quaternary Ammonium Salts - Possible Chemical AgentsDocument23 pagesBall - Quaternary Ammonium Salts - Possible Chemical AgentsLuděk SpurnýNo ratings yet
- Chapter 8 - Nervous SystemDocument105 pagesChapter 8 - Nervous SystemAllisya HaneeNo ratings yet
- Organophospha Te (Op) Poisining: Presented byDocument44 pagesOrganophospha Te (Op) Poisining: Presented byShantanu Kr VatsyayanNo ratings yet
- WK 4 Pharma CNS Drugs A Sympha, Parasympha, Stimulant, Depressant, Anticonvulsive Neuromuscular AgentsDocument56 pagesWK 4 Pharma CNS Drugs A Sympha, Parasympha, Stimulant, Depressant, Anticonvulsive Neuromuscular AgentsYzel Vasquez AdavanNo ratings yet
- Pharma NotesDocument38 pagesPharma NotesJose Luis AlmonedaNo ratings yet
- MCQDocument6 pagesMCQJames PerianayagamNo ratings yet
- NMJ Full OspeDocument2 pagesNMJ Full OspeDR AbidNo ratings yet
- Tut Physiology 2Document7 pagesTut Physiology 2Ghaidaa SadeqNo ratings yet
- PharmacologyAnesthesiology RevalidaDocument166 pagesPharmacologyAnesthesiology RevalidaKENT DANIEL SEGUBIENSE100% (1)
- The Fluorine Group of Organophosphates and Their Anticholinesterase Effects On The Central Nervous SystemDocument10 pagesThe Fluorine Group of Organophosphates and Their Anticholinesterase Effects On The Central Nervous SystemBrockeNo ratings yet
- Generic Name Classification Dosage Mechanism of Action Indication Contraindication Adverse Reaction Nursing ResponsibilitiesDocument7 pagesGeneric Name Classification Dosage Mechanism of Action Indication Contraindication Adverse Reaction Nursing ResponsibilitiesFlor Anne De JesusNo ratings yet
- Skeletal Muscle RelaxantsDocument34 pagesSkeletal Muscle RelaxantsLohithNo ratings yet
- Guide to Pharmacology 2013/14: EnzymesDocument71 pagesGuide to Pharmacology 2013/14: EnzymesLourdesNo ratings yet
- Lecture 1 Snake BiteDocument30 pagesLecture 1 Snake BiteZartasha KhanNo ratings yet
- The Neuromuscular Junction Physiology: November 2016Document8 pagesThe Neuromuscular Junction Physiology: November 2016Garima PrakashNo ratings yet
- Acetylcholinesterase Inhibitors As Alzheimer Therapy From Nerve Toxins To NeuroprotectionDocument24 pagesAcetylcholinesterase Inhibitors As Alzheimer Therapy From Nerve Toxins To NeuroprotectionLucasBritoNo ratings yet
- USMLE Step I Comprehensive review quizlet.com printDocument222 pagesUSMLE Step I Comprehensive review quizlet.com printJay KJNo ratings yet
- Anti Cholinergic Drugs Block Muscarinic and Nicotinic ReceptorsDocument2 pagesAnti Cholinergic Drugs Block Muscarinic and Nicotinic ReceptorsFNo ratings yet