Professional Documents
Culture Documents
Research Resource Scientists
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Research Resource Scientists
Copyright:
Available Formats
pp696-700 BMSJul05
17/6/05
10:29 AM
Page 1
A R T I C L E
Unclear about how to introduce a new diagnostic test in your laboratory? Daunted by the prospect of involvement in a research exercise? Help is now at hand as Victoria Bradley has produced a resource pack that deals with all aspects of the research process.
Research resource for biomedical scientists
The majority of research carried out by biomedical scientists is related to or directly concerns diagnostic tests. Before a new diagnostic test can be introduced in the laboratory it must be researched thoroughly and tested rigorously to ensure that results are both valid and reliable. This article is based on a research resource pack designed to help those who wish to introduce a new diagnostic test to identify the appropriate research question, select the appropriate research study design and plan the research using appropriate resources and guidelines. When evaluating a new diagnostic test for use in the laboratory, the research should pass through four phases1 before the test is introduced. Phase 1: Do test results in affected patients differ from those in normal individuals? Phase 2: Are patients with certain test results more likely to have the target disorder? Phase 3: Do test results distinguish patients with and without the target disorder among those in whom it is clinically sensible to suspect the disorder? Phase 4: Do patients undergoing the diagnostic test fare better than similar untested patients? The research question selected for investigating the validity and reliability of a diagnostic test will naturally fit into one of these four phases, and will depend on the area of research and what, if any, research has been undertaken before. The four phases follow a natural progression, which can be followed by an individual researcher or used to carry on where others stopped. An example of a phase 1 research study is work carried out on the use of faecal calprotectin as a new marker to differentiate between irritable bowel syndrome (IBS) and Crohns disease.2 Calprotectin levels were measured in samples collected at random from patients attending a gastroenterology clinic with a diagnosis of IBS or Crohns disease. Controls were collected from healthy volunteers who had no symptoms of bowel disease, had not undergone previous bowel resection, and were not on medication. After blind completion of analyses it was noted that there was a large difference in median calprotectin concentration in the Crohns disease group compared to that in the control group and the IBS group. There was overlap between the ranges but the group concluded that a single calprotectin measurement could aid gastroenterologists in the differential diagnosis of Crohns disease and IBS.
Research in phases
Research question
There are many different types of clinical research question; however, the majority are covered by the acronym PICO: P = population; I = intervention/risk factor; C = comparison; and O = outcome. All four points will not necessarily be included in every clinical question. An example of a question might be: Do antimicrobials increase the carriage rate of penicillin-resistant pneumococci in children? Here, the population is children, the risk factor is the use of antimicrobials, and the outcome is penicillin-resistant pneumococci infection. Research begins with the question, which gives the research direction and should make the purpose of the study quite clear. The question should be guided by PICO and identify the participants, intervention, comparison and outcome of interest. Research questions can be interpretive or objective. An interpretive question might ask: How do parents make decisions about immunisation? An objective question might ask: Is there a link between immunisation of infants with measles/mumps/rubella (MMR) vaccine and the development of autism? the majority of research in biomedical science involves objective questions (ie quantitative research).
This is typical of a phase 1 research study, whereby the subjects are a group of people known to have the conditions of interest and the control group consists of healthy individuals. The results of this research would not automatically warrant the introduction of calprotectin as a diagnostic tool, but encouraging initial results suggest that further investigation would be appropriate. Phase 1 research studies involve relatively little cost and are fairly quick to carry out. Therefore if a less positive outcome had been achieved then little money and time would have been wasted in the pursuit of information regarding the worth of the proposed new diagnostic test. If this research example continued to the next logical step then a phase 2 study would be performed. Here, the direction of interpretation is reversed such that results of the diagnostic test (ie calprotectin) are obtained before the diagnosis is known. An example of the relevant research question would be: Are patients with high levels of calprotectin more likely to have Crohns disease than patients with lower levels? The best strategy for this research would be to test all new patients presenting with chronic diarrhoea, classic symptoms of IBS and Crohns disease for faecal calprotectin and compare the results against the final clinical outcome. If positive results were obtained from this research it would still not warrant introduction as a diagnostic tool as it is comparing a group of people with severe symptoms, chronic diarrhoea, and a perfectly normal control group. But it would indicate whether or not the test showed promise as a diagnostic tool under ideal conditions. An example of a phase 3 research study is work carried out into the validity of heart fatty acid-binding protein (hFABP) and myoglobin as early diagnostic markers of myocardial infarction (MI).3 In this study,
696
THE BIOMEDICAL SCIENTIST July 2005
pp696-700 BMSJul05
17/6/05
10:30 AM
Page 2
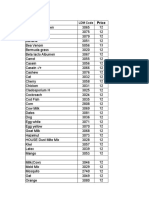
Table 1. Reliability of high Test A levels in diagnosing Pathology B.
RISK FACTOR (HIGH LEVELS OF TEST A) 1 = Yes 2 = No Total OUTCOME CASE CONTROL 80 40 120 60 200 260 TOTAL 140 240 380
Case-control studies in validating diagnostic tests
Table 2. Proportions and ORs calculated from data in Table 1.
Group 1 (high Test A levels) Proportion (p) OR p1 = 80/140 = 0.571 (57.1%) OR1 = 80/60 = 1.333 Group 2 (low Test A levels) Overall p2 = 40/240 = 0.167 (16.7%) OR2 = 40/200 = 0.200 p =120/380 = 0.316 (31.6%) OR = 120/260 = 0.462
In biomedical science, there are several strategies for researching the diagnostic worth of a laboratory test. However, the current phase of the research will dictate which research strategy should be employed. Research into diagnostic testing is undertaken for several reasons, and may involve a new test utilising a new analytical method, a new test utilising an existing analytical method, or an existing test and analytical method for a new diagnostic use. For the purposes of this article, a phase 1 research project utilising a case control structure will be considered.
Designing a case-control study
Proportion (risk) = number experiencing event (Pathology B with high Test A levels) subgroup size (total of subjects and controls with high Test A levels) OR = number experiencing event number not experiencing event
patients admitted to the accident and emergency department with chest pain were selected. In such a cohort it would be clinically reasonable to suspect that they had suffered an MI. All patient samples were analysed for troponin I (a marker widely accepted as the gold standard for diagnosing MI), hFABP and myoglobin on admission and again 12 hours later. This research concluded that hFABP and myoglobin offered no diagnostic advantage over the use of troponin I alone. The true worth of a diagnostic test can be distorted easily in a phase 3 study. An important question that needs to be answered is: Has there been an independent, blind comparison with a gold standard of diagnosis?4 In the phase 3 study described here, all patients' samples were analysed for troponin I (the gold standard) and only these results were reported back to the clinicians. Therefore, the hFABP and myoglobin results had no influence on the diagnosis of MI. In this study it is difficult to determine what cut-off values were used for the three markers and on what evidence the cut-off values were based. This is another potential area of error that can be introduction in a phase 3 study, as another group could perform similar research but increase their sensitivity and specificity by employing different cut-off values. Phase 3 research is also affected by the setting in which it is carried out. If research is carried out in a primary care setting it may have a much higher specificity than similar research undertaken on tertiary referrals. In order to take account of this, similar studies should be carried out in the different settings in which the diagnostic test may be used. The true worth of a diagnostic test cannot usually be measured until it has undergone a phase 4 research study. Here, the benefit, if
any, to the health outcome of the patient is followed. If the study of hFABP and myoglobin as early diagnostic markers for MI had proved to be more promising then a phase 4 study would have been the next logical step. Patients would have been assigned randomly to undergo troponin I or hFABP and myoglobin analysis and then have had their health outcomes compared. The case series structure is not suitable for researching a new diagnostic test, as this is assessing patient outcome (ie symptoms or pathology) following a specific event, and therefore is not relevant. Although examination of series can provide hypotheses that can be investigated by further study, one such study could provide the research question for a new diagnostic test. The cross-sectional structure would be best suited to phase 3 research when evaluating a new diagnostic test. Returning to the example used earlier,3 samples from patients with chest pain (ie suspected of MI) are analysed for two different sets of markers and their diagnostic worth compared. The case-control structure is ideal when carrying out phase 1 and phase 2 investigations into the worth of a diagnostic test. In both instances a control group is required for comparison. Cohort structures are used to study the incidence of outcome. A diagnostic test could be utilised in such a study but is not relevant to testing the validity and reliability of that test. The randomised control trial structure would be best utilised in a phase 4 investigation of a diagnostic test. Patients would be randomly selected to have the new test or the old test and then followed to determine which group had the best health outcome.
Appropriate research structure
The first stage is to determine how the cases will be selected. They should cover the entire spectrum of the disease under investigation. The source population should be defined (eg patients diagnosed with a specific pathology) and it is imperative that there are sufficient cases for the sample size calculation. Consideration of the source of the cases is the next stage in the design, and this will be determined to some extent by the source population. Examples include patients admitted or discharged from a hospital within a specified time period (eg all patients diagnosed with subarachnoid haemorrhage within a calendar year), and incident or newly diagnosed patients (eg all newly diagnosed diabetic patients). Selection of controls needs careful consideration, as they must not have the pathology or outcome of interest and they must also be representative of the population from which the cases were obtained. If there is uncertainty about whether or not the controls are representative of the reference population then there should be more than one control group. Controls can be matched on an individual or group basis. Individually, controls are matched by age (to within a five-year range) and sex. In a group where 55% of cases are female with a mean age of 52 then the control group should be selected to match these figures. Caution should always be used when matching, as a study can be overmatched and therefore mask the association between exposure and outcome. At this stage, it is important that an appropriate reference standard be selected and that all subjects and controls be subjected to it. In most cases it should be the gold standard for diagnosing the pathology of interest. The next stage it to analyse the subject and control samples using the new diagnostic test. This should be performed blind to the results of the reference standard, in order not to introduce bias. In summary: determine how cases will be selected; determine how controls will be selected; decide whether controls should be matched or not; select an appropriate reference standard; and then perform the analyses
THE BIOMEDICAL SCIENTIST July 2005
697
pp696-700 BMSJul05
17/6/05
10:30 AM
Page 3
Data collection techniques
First, how the outcome will be measured must be decided and will depend on the type of outcome, which in this case is the pathology of interest. The most convenient information for a biomedical scientist to obtain is the clinical details of the patient provided to the laboratory on the request form. However, this could introduce information bias, as the diagnosis may not be definitive at the time the patients sample is collected (eg patient is admitted with a severe headache, and a tentative diagnosis of meningitis initially may be given to the laboratory). Use of a patients medical records would decrease this informational bias significantly (eg patient with a headache and an initial diagnosis of meningitis ultimately diagnosed with a subarachnoid haemorrhage). Care should always be taken when obtaining information from this source, as the order of information may not be uniform, there may be uncertainties and inconsistencies in and between records and data may be based on self-report or come from proxy respondents (eg a patient or their spouse reporting on smoking habits). Measurement of exposure is much simpler. These are the test results obtained by the case group and the control group, using the new diagnostic test. Hence, these results will only be as good or as bad as the researchers technique and the sensitivity and specificity of the diagnostic test in question.
While analysing data from a case-control study, it is important to take into account any confounding factors. For example, serum creatinine level, which can be used to assess kidney function, is affected by both age and gender. In order to take this into account the data can be stratified, whereby the OR is calculated for males and females separately and then compared to the OR for males and females combined (eg OR [males] = 2.50; OR [females] = 2.17; OR [combined] = 2.34). In the Test A/Pathology B example the ORs for the subgroups are not markedly different and using the combined data gives a more accurate estimate of the OR for the entire population. However, caution needs to be exercised because confounding can introduce bias by making it appear that there is a false association between exposure and outcome or by masking an association. The effectiveness of the diagnostic test under investigation is best represented using sensitivity and specificity. Sensitivity indicates how good the test is at finding those who have the pathology, and specificity indicates how good the test is at excluding those who do not have the pathology. Sensitivity = number both disease positive and test positive number disease positive Specificity = number both disease negative and test negative number disease negative If this is applied to the Test A/Pathology B example used above then sensitivity = 80/120 (0.67) and specificity = 200/260 (0.77). Sensitivity and specificity are often multiplied by 100 to give a percentage, so in this case high levels of Test A are 67% sensitive and 77% specific in detecting Pathology B. To the majority of biomedical scientists, this is a measure of the real worth of the diagnostic test and provides the best information about whether or not the test is suitable for introduction into routine use in the laboratory. Of course, sensitivity and specificity are determined by the cut-off value selected. Sensitivity could be improved by lowering the cut-off value, but this will reduce the specificity (ie there must be a compromise between sensitivity and specificity). In order to examine this compromise, it is often helpful to plot sensitivity against specificity. This is called a receiver operating characteristic (ROC) curve, in which sensitivity is plotted against 1-specificity. If the cut-off is estimated and tested in the same sample group then the estimates will be biased. Thus, the cut-off should be tested in a different sample of subjects and controls.
but a good framework is that provided by the Critical Appraisal Skills Programme (CASP). This was developed by the Public Health Resource Unit (www.phru.nhs.uk/learning) as a learning and development tool. The programme was set up in 1993 and aims to assist individuals to develop an evidencebased approach to health and social care. Two separate criteria provided by CASP are relevant to a phase 1 research study into the introduction of a diagnostic test, and these are the case control study appraisal6 and the diagnostic test study appraisal.7 As might be expected, there is much overlap between the two and some of the points could only be addressed by readers of the study. But there are a number of extremely pertinent points that will aid the potential researcher in ensuring that they produce the best quality research study possible. The majority of points set out by both criteria have been covered already. One important point that has not, however, relates to the write up of the research, which should be sufficiently detailed to enable other researchers to carry out research under the same conditions. Detailed information about the methodology used to perform the diagnostic test, which standards and controls were used, what the cut-off level was and how it was arrived at should all be included.
Ethical approval
Data analysis techniques
Data analysis for a case-control study is usually expressed as the odds ratio (OR) of exposure (test results) in cases compared with controls.5 For example, the data in Table 1 were collected while investigating the reliability of high Test A levels in diagnosing Pathology B. A total of 120 samples from patients with Pathology B and 260 samples from patients known not to have Pathology B (controls) were analysed for diagnostic Test A. The layout of the table is very important in case-control studies. The first row identifies the risk factor of interest (high Test A levels) and the first column identifies the outcome of interest (Pathology B). Using data from Table 1, the proportions and ORs can be calculated (Table 2). As proportion or OR increases, the likelihood of the event increases (ie the likelihood of subjects with Pathology B having high Test A levels). In a case-control study, the likelihood of subjects with Pathology B having high Test A levels (relative to the control group) are quantified by the OR. Taking the figures from Table 2, OR = OR1/OR2 (1.333/0.200 = 6.665). If OR = 1.0 then outcome (ie presence or absence of Pathology B) is not influenced by the risk factor (high Test A levels). If OR > 1.0 then outcome is more likely if the risk factor is present. If OR < 1.0 then outcome is less likely if the risk factor is present. Therefore, in the example given, subjects with high Test A levels are more likely to have Pathology B.
As of 1 March 2004 a new standard operating procedure for research ethics committees came into force. This has been implemented following the issue of EU Directive 2001/20/EC. Requirements set by this directive for the ethical review of research include the following: to deliver a decision on a valid application within 60 days one decision to be valid for the whole of the UK restriction of one written request for clarification or further information to applicants. The application form and instructions on how to apply for ethical review can be found on the Central Office for Research Ethics Committee (COREC) website.11 This is a lengthy document which usually must be completed online. It does not need to be completed all at one sitting, as the form can be saved and a user name and password provided for future access. The form covers a number of different areas of the intended research, all of which aim to provide a local research ethics committee (LREC) with sufficient information to make an informed decision. There is a document available on the COREC website that provides advice on how to complete the application form.12 The main concern of the LREC will be that patients are not taken advantage of or exposed to any unnecessary harm. In order to comply with this it is best (if at all possible) to avoid using vulnerable groups
Quality criteria
In order to ensure that the intended research is of a good quality it is important to consider the criteria that others will use to judge the final article. There are a number of criteria
THE BIOMEDICAL SCIENTIST July 2005
699
pp696-700 BMSJul05
17/6/05
10:31 AM
Page 4
of patients such as children or adults who may not be able to make an informed choice to participate in the research. In the majority of cases informed consent will need to be obtained from individual patients. This will usually involve an explanation of what it is they are being asked to participate in, provision of an information sheet, and written consent. This may not be necessary in circumstances where, for example, no extra samples are required from the patient, all samples are analysed anonymously and no new diagnostic information will be gained. Legislation of research carried out in the NHS has undergone some change recently and it is now mandatory that research is registered with a trusts research and development office. Also included under this legislation are research projects led by individuals or organisations that are not part of the trust, and commercially sponsored research. In brief: a review of the scientific quality of the proposed research must take place, in addition to review by an ethics committee; all interventional research must have a designated sponsor; the research must comply with Caldicott guidelines,8 the Data Protection Act 19989 and the health and safety regulations;10 and lead researchers must be aware of, and sign up to, their responsibilities under research governance. The research and development office within a trust is responsible for ensuring that all research proposals submitted comply with requirements of research governance and all other legislative requirements prior to trust approval being granted. Furthermore, it is the responsibility of the researcher to ensure that the correct procedures for the submission of a research project have been followed, and, most importantly, that the research and development office is provided with all the necessary documentation to enable the study to be properly reviewed and registered. All research involving human subjects (including human tissue) must have appropriate ethical approval. In some trusts, submission for ethical review can take place in parallel with submission for trust registration, but final approval will usually not be given until ethical approval has been given. In general, when submitting a research study for registration with a trust, the following documentation is required: study protocol evidence of ethical approval, or that ethical approval has been applied for copies of parts A, B and C of the NHS ethics application form, available online copy of the trust research registration form copies of the patient information sheet and consent form, if applicable brief summary of the study in terms that a lay person can understand. Depending upon local arrangements, there will be a mixture of requirements for
electronic or hard copies of the above documentation. All of the above information is required so that the research project can be registered properly and that costs can be estimated in order to determine the direct impact on trust services. The trust will also want to assess what benefits it will gain from the research and will be particularly interested in benefits to patient care.
offering the researcher funding or other support. Department of Heath The Department of Health has a very useful website13 that provides information for research and development. It provides an overview of the department's research and development funding policies, priorities and organisation. There is also an AZ list of research within the NHS. REFERENCES 1 Sackett DL, Haynes RB. The architecture of diagnostic research. BMJ 2002; 324: 53941. 2 Wassell J, Dolwani S, Metzner M, Losty H, Hawthorne A. Faecal calprotectin: a new marker for Crohns disease? Ann Clin Biochem 2004; 41: 2302. 3 Alansari SE, Croal BL. Diagnostic value of heart fatty acid binding protein and myoglobin in patients admitted with chest pain. Ann Clin Biochem 2004; 41: 3916. 4 Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical epidemiology, a basic science for clinical medicine (2nd edn). Boston: Little Brown, 1991: 83. 5 Bland M. An introduction to medical statistics (3rd edn). Oxford: University Press; 2000. 6 Critical Appraisal Skills Programme: making sense of evidence. Eleven questions to help you make sense of a case-control study. 2004. www.phru.nhs.uk/casp/case_control _studies.htm 7 Critical Appraisal Skills Programme: making sense of evidence. Twelve questions to help you make sense of a diagnostic test study. 1998. www.phru.nhs.uk/casp/diagtest.htm 8 Caldicott Report. 1997. www.dh.gov.uk/PolicyAndGuidance/Infor mationPolicy/PatientConfidentialityAndCal dicottGuardians/Caldicott/fs/en 9 Data Protection Act 1998. http://hmso.gov.uk/acts/acts1998/199800 29.htm. 10 Health and Safety at Work Act 1974. www.healthandsafety.co.uk/hasawa.htm. 11 NHS Central Office for Research Ethics Committees (COREC) website. www.corec.org.uk. 12 NHS Central Office for Research Ethics Committees (COREC). Question-specific advice for applicants. www.corec.org.uk/applicants/apply/docs/ Qustions-specific_Advice.doc. 13 Department of Health website. www.dh.gov.uk.
Victoria Bradley CSCI FIBMS is a biomedical scientist working in the Department of Chemical Pathology at Morriston Hospital, Swansea. For further information email victoria.bradley@swansea-tr.wales.nhs.uk.
Available resources
Research regulations
There are a number of resources available to the potential researcher, and a by no means exhaustive list includes advice from colleagues, the departmental research and development committee, trust research and development committee, local research ethics committee, diagnostic companies (for possible funding and support) and the Department of Heath. Colleagues Colleagues are an indispensable source of information, ideas and advice. It is advisable to consult colleagues first when considering embarking on a new research project. The researcher cannot be in the laboratory 24 hours a day so the assistance of wellinformed colleagues in, for example, sample collection and storage is essential. Discussion of ideas with colleagues may also provide a new direction if the intended research runs into problems. Departmental research and development committee It is essential that the departmental research and development committee is consulted at a very early stage when planning a research project. There may be other research planned or in progress with which samples and data collection could run in tandem. Not only will this make the task of the individual researcher much easier but it will also enable departmental resources to be used more efficiently. Trust research and development committee Advice from the trust research and development committee is invaluable when planning what resources will be required for the research. It will be able to provide guidance about where missing resources may be obtained and if the proposed use of resources is feasible within their remit. Local research ethics committee Essential advice can be obtained from the LREC about designing the research in the most ethical manner. This would be especially useful if the research involved subjects classed as vulnerable (eg children or patients suffering from Alzheimers disease). Diagnostic companies Some diagnostic companies may be interested in the research for future marketing prospects and may consider
700
THE BIOMEDICAL SCIENTIST July 2005
You might also like
- ChessDocument3 pagesChessLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- ChemDocument1 pageChemLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Troponin I Normal RangeDocument1 pageTroponin I Normal RangeLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- MicroDocument1 pageMicroLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Microalbumin EvaluationDocument2 pagesMicroalbumin EvaluationLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- How to Play ChessDocument22 pagesHow to Play Chessraj202987_47312067No ratings yet
- Haematology Analyser Comparison 2019+Document2 pagesHaematology Analyser Comparison 2019+Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Single AllergenDocument2 pagesSingle AllergenLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Alfa Test ProfilesDocument1 pageAlfa Test ProfilesLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- 8 Metabolic Conditioning Workouts MMA FightersDocument5 pages8 Metabolic Conditioning Workouts MMA FightersLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Kumon'S Recommended Reading List - Level 7A Level 3ADocument6 pagesKumon'S Recommended Reading List - Level 7A Level 3ALuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- MicroDocument4 pagesMicroLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Jose CapangyarihanDocument1 pageJose CapangyarihanLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Parameters LDM Machine Print Out CAP Result Ref Range Proficiency MIC Pol 2Document3 pagesParameters LDM Machine Print Out CAP Result Ref Range Proficiency MIC Pol 2Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Toshiba Canvio BasicsDocument201 pagesToshiba Canvio BasicsMattiaVNo ratings yet
- Coulter AC.T 5 Diff ProcedureDocument12 pagesCoulter AC.T 5 Diff ProcedureLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- OEC Exemption 2019Document1 pageOEC Exemption 2019Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Formaldehyde MSDS Mallinckrodt PDFDocument8 pagesFormaldehyde MSDS Mallinckrodt PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Chest Day: Gaspari Nutrition: 7 Day Split Workout Workout Example 1Document3 pagesChest Day: Gaspari Nutrition: 7 Day Split Workout Workout Example 1Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- The Aggressive Strength Solution by Mike MahlerDocument124 pagesThe Aggressive Strength Solution by Mike Mahlermirocvet100% (3)
- The Vert Specific Conditioning Guide : How Hard Can You Go and For How Long?.Document20 pagesThe Vert Specific Conditioning Guide : How Hard Can You Go and For How Long?.Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Team THUMP Txtbook PDFDocument20 pagesTeam THUMP Txtbook PDFLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Dr. Fooke SOPDocument1 pageDr. Fooke SOPLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Genetics For Dummies, 2nd Edition - WikispacesDocument23 pagesGenetics For Dummies, 2nd Edition - WikispacesSundas ZahraNo ratings yet
- MicroDocument1 pageMicroLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Dhoha R. HDocument1 pageDhoha R. HLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Troponin I Normal RangeDocument1 pageTroponin I Normal RangeLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Confirmed Result First Batch Urine CultureDocument4 pagesConfirmed Result First Batch Urine CultureLuis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Title: Microbiology Urine Screening Effective Date: 05/08/2013Document14 pagesTitle: Microbiology Urine Screening Effective Date: 05/08/2013Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Microbiology Urine Culture 2019 2Document1 pageMicrobiology Urine Culture 2019 2Luis Ferdinand Dacera-Gabronino Gamponia-NonanNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- LGFL Service GuideDocument24 pagesLGFL Service GuideThe Return of the NoiristaNo ratings yet
- Impact of Recruitment & Selection on Employee RetentionDocument39 pagesImpact of Recruitment & Selection on Employee RetentiongizawNo ratings yet
- Front Cover Short Report BDA27501Document1 pageFront Cover Short Report BDA27501saperuddinNo ratings yet
- Design and Analysis of Algorithms Prof. Madhavan Mukund Chennai Mathematical Institute Week - 01 Module - 01 Lecture - 01Document8 pagesDesign and Analysis of Algorithms Prof. Madhavan Mukund Chennai Mathematical Institute Week - 01 Module - 01 Lecture - 01SwatiNo ratings yet
- Marksmanship: Subject: III. Definition of TermsDocument16 pagesMarksmanship: Subject: III. Definition of TermsAmber EbayaNo ratings yet
- Principles of Management NotesDocument61 pagesPrinciples of Management Notestulasinad123No ratings yet
- Write 10 Lines On My Favourite Subject EnglishDocument1 pageWrite 10 Lines On My Favourite Subject EnglishIrene ThebestNo ratings yet
- English Skills BookDocument49 pagesEnglish Skills BookAngela SpadeNo ratings yet
- Flexible AC Transmission SystemsDocument51 pagesFlexible AC Transmission SystemsPriyanka VedulaNo ratings yet
- Week 6Document7 pagesWeek 6Nguyễn HoàngNo ratings yet
- LLM DissertationDocument94 pagesLLM Dissertationjasminjajarefe100% (1)
- Long Run Average Cost (LRAC) : Economies of ScaleDocument3 pagesLong Run Average Cost (LRAC) : Economies of ScaleA PNo ratings yet
- Wika Type 111.11Document2 pagesWika Type 111.11warehouse cikalongNo ratings yet
- ArtigoPublicado ABR 14360Document14 pagesArtigoPublicado ABR 14360Sultonmurod ZokhidovNo ratings yet
- Exam Ref AZ 305 Designing Microsoft Azure Infrastructure Sol 2023Document285 pagesExam Ref AZ 305 Designing Microsoft Azure Infrastructure Sol 2023maniNo ratings yet
- EQ - Module - Cantilever MethodDocument17 pagesEQ - Module - Cantilever MethodAndrea MalateNo ratings yet
- Euro4 vehicle diesel engines 199 - 397 kW (270 - 540 hpDocument6 pagesEuro4 vehicle diesel engines 199 - 397 kW (270 - 540 hpBranislava Savic63% (16)
- Voltaire's Candide and the Role of Free WillDocument3 pagesVoltaire's Candide and the Role of Free WillAngy ShoogzNo ratings yet
- Guidelines 2.0Document4 pagesGuidelines 2.0Hansel TayongNo ratings yet
- Analysis of VariancesDocument40 pagesAnalysis of VariancesSameer MalhotraNo ratings yet
- Ipo Exam Revised SyllabusDocument1 pageIpo Exam Revised Syllabusজ্যোতিৰ্ময় বসুমতাৰীNo ratings yet
- CIGB B164 Erosion InterneDocument163 pagesCIGB B164 Erosion InterneJonathan ColeNo ratings yet
- UT Dallas Syllabus For Ee3311.002.07f Taught by Gil Lee (Gslee)Document3 pagesUT Dallas Syllabus For Ee3311.002.07f Taught by Gil Lee (Gslee)UT Dallas Provost's Technology GroupNo ratings yet
- 9AKK101130D1664 OISxx Evolution PresentationDocument16 pages9AKK101130D1664 OISxx Evolution PresentationfxvNo ratings yet
- Maximizing modular learning opportunities through innovation and collaborationDocument2 pagesMaximizing modular learning opportunities through innovation and collaborationNIMFA SEPARANo ratings yet
- Raychem Price ListDocument48 pagesRaychem Price ListramshivvermaNo ratings yet
- Hastrof Si Cantril. 1954. The Saw A Game. A Case StudyDocument6 pagesHastrof Si Cantril. 1954. The Saw A Game. A Case Studylandreea21No ratings yet
- Future Design of Accessibility in Games - A Design Vocabulary - ScienceDirectDocument16 pagesFuture Design of Accessibility in Games - A Design Vocabulary - ScienceDirectsulaNo ratings yet
- Oracle Fusion Financials Book Set Home Page SummaryDocument274 pagesOracle Fusion Financials Book Set Home Page SummaryAbhishek Agrawal100% (1)
- Obsolescence 2. Book Value 3. Depreciation 4. Depletion EtcDocument9 pagesObsolescence 2. Book Value 3. Depreciation 4. Depletion EtcKHAN AQSANo ratings yet