Professional Documents
Culture Documents
Robbins Ch. 20 The Kidney Review Questions
Uploaded by
PA2014Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Robbins Ch. 20 The Kidney Review Questions
Uploaded by
PA2014Copyright:
Available Formats
Robbins Ch.
20 The Kidney
Study online at quizlet.com/_enqxa
1.
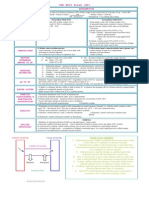
BRS Pathology - Table 17-1 Glomerular Diseases
(memorize this table)
2.
Tubular and interstitial disorders are frequently caused by what? Glomerular diseases are frequently caused by what? 1. What is azotemia? 2. What is it related to? Nephritic syndrome?
toxins or infectious agents
3.
immunologically mediated 1. elevated of BUN and creatinine 2. decreased glomerular filtration rate HEMATURIA, mild proteinuria, oliguria, azotemia, and hypertension - is due to glomerular disease and is dominated by the acute onset of usually grossly visible hematuria (red blood cells in urine), mild to moderate proteinuria, and hypertension; it is the classic presentation of acute poststreptococcal glomerulonephritis. *Hallmark = glomerular inflammation and bleeding -limited proteinuria <3.5g/day -oliguria and azotemia -salt retention with periorbital edema and HTN -RBC casts and dysmorphic RBCs in urine*** *Biopsy = hypercellular, inflamed glomeruli -immune-complex deposition activates complement -C5a attracts neutrophils, which mediate damage Examples = Post-strep GN, RPGN, IgA neph, Alport syndrome
4.
5.
6.
Nephrotic syndrome?
heavy PROTEINURIA, hypoalbuminemia, severe edema, hyperlipidemia, lipiduria - due to glomerular disease, is characterized by heavy proteinuria (more than 3.5 gm/day), hypoalbuminemia, severe edema, hyperlipidemia, and lipiduria (lipid in the urine). nephrotic syndrome is worse
7.
Which is worse, nephritic syndrome or nephrotic syndrome? 4 stages of renal failure:
8.
- diminished renal reserve - renal insufficiency - chronic renal failure - end-stage renal disease
9.
Basement membrane thickening in EM, how does the thickening happen?
immune complex deposition, synthesis of protein components Basement Membrane Thickening: - By light microscopy, this change appears as thickening of the capillary walls, best seen in sections stained with periodic acid-Schiff (PAS). - By electron microscopy such thickening takes one of two forms: 1) Deposition of amorphous electron-dense material, most often immune complexes, on the endothelial or epithelial side of the basement membrane or within the GBM itself. Fibrin, amyloid, cryoglobulins, and abnormal fibrillary proteins may also deposit in the GBM. 2) Thickening of the basement membrane due to increased synthesis of its protein components, as occurs in diabetic glomerulosclerosis. pink (eosinophilic) - Hyalinosis, as applied to the glomerulus, denotes the accumulation of material that is homogeneous and eosinophilic by light microscopy
10.
Hyalinosis, what do you seen microscopically?
11.
What is hyalinosis a common feature of? What is sclerosis characterized by? As kidney disease progresses, what are the 2 major histologic characteristics seen? What are the 3 types of Rapidly Progressive (Crescentic) Glomerulonephritis?
focal segmental glomerulosclerosis accumulations of extracellular collagenous matrix, either confined to mesangial areas as is often the case in diabetic glomerulosclerosis, or involving the capillary loops, or both. - focal segmental glomerulosclerosis - tubulointersitital fibrosis Type 1, 2, and 3: 1) Anti-GBM antibody 2) Immune complex 3) Pauci-immune - lack of immune anti-GBM or immune complexes by immunofluorescence and electron microscopy. - Most patients with this type of RPGN have circulating antineutrophil cytoplasmic antibodies (ANCAs) that produce cytoplasmic (c) or perinuclear (p) staining patterns, and play a role in some vasculitides. 1. nothing much 2. loss of foot processes (podocytes) - Electron microscopy discloses deposits in those cases due to immune complex deposition (type II). - Regardless of type, electron microscopy may show distinct ruptures in the GBM, the severe injury that allows leukocytes, proteins, and inflammatory mediators to reach the urinary space, where they trigger the crescent formation 3. nephrotic syndrome 1. effaced foot processes & sclerosis of focal segments (portions of structures are involved) 2. Nephrotic - alterations in glomerular basement membrane - proliferation of glomerular cells - leukocyte infiltration IgA Berger disease (IgA Nephropathy)
12.
13.
14.
15.
1. What would you see via light microscopy (LM) for RPGN? 2. What would you see via electric microscopy (EM) for RPGN? 3. What would you see, nephritic or nephrotic syndrome? 1. What do you seen in focal segmental glomerulosclerosis? 2. Nephritic or nephrotic? Histologically what do you seen in membranoproliferative glomerulonephritis? In Berger disease, what kind of deposits would you see? What is the most common type of glomerulonephritis worldwide? In Alport syndrome, what type of abnormal collagen do you have?
16.
17.
18.
19.
20.
Type IV collagen
21.
Alport syndrome:
- thin basement membrane lesion - the most common cause of benign familial hematuria - is manifest by hematuria with progression to chronic renal failure, accompanied by nerve deafness and various eye disorders, including lens dislocation, posterior cataracts, and corneal dystrophy no, the disease can be suspected by LM, but the Dx is made only by immunocytochemical techniques
22.
Can you diagnosis Berger disease with light microscopy? Acute kidney injury or acute tubular necrosis is caused by what? Table 20-5 - pg 918 (highlighted)
23.
- ischemia - toxic injury - urinary obstruction - acute tubulointerstitial nephritis
24.
25.
What is a neoplasm that can cause tubuleinterstitial nephritis? Most common cause of clinical pyelonephritis? 1) Vesicoureteral reflux: 2) What do you seen because of that?
multiple myeloma
26.
ascending infection
27.
1) urine goes back from bladder to ureters - Although obstruction is an important predisposing factor in ascending infection, it is incompetence of the vesicoureteral valve that allows bacteria to ascend the ureter into the renal pelvis. An incompetent vesicoureteral orifice allows the reflux of bladder urine into the ureters (vesicoureteral reflux) 2) increased infection - The effect of vesicoureteral reflux is similar to that of an obstruction in that there is residual urine in the urinary tract after voiding, which favors bacterial growth. acute suppurative inflammation of kidneys caused mostly by bacteria - Acute pyelonephritis is caused by bacterial infection and is the renal lesion associated with urinary tract infection. E. coli (O157:H7)
28.
What is acute pyelonephritis? Most common bacteria that causes pyelonephritis is what?
29.
30.
Figure 20-32 "know what is going on there"
Typical coarse scars of chronic pyelonephritis associated with vesicoureteral reflux. The scars are usually polar and are associated with underlying blunted calyces. - Chronic pyelonephritis is a disorder in which chronic tubulointerstitial inflammation and renal scarring are associated with pathologic involvement of the calyces and pelvis
31.
Benign nephrosclerosis is a term used to describe what? Know what kind of a histologic picture you would see with benign nephrosclerosis / Figure 20-38 "know why that happens"
renal pathology associated with renal sclerosis of renal arterioles and small arteries
32.
Close-up of the gross appearance of the cortical surface in benign nephrosclerosis illustrating the fine, leathery granularity of the surface. - The kidneys are either normal or moderately reduced in size, with average weights between 110 and 130 gm. The cortical surfaces have a fine, even granularity that resembles grain leather (Fig. 20-38). The loss of mass is due mainly to cortical scarring and shrinking - On histologic examination there is narrowing of the lumens of arterioles and small arteries, caused by thickening and hyalinization of the walls (hyaline arteriolosclerosis) (Fig. 20-39). Corresponding to the fine surface granulations are microscopic subcapsular scars with sclerotic glomeruli and tubular dropout, alternating with better preserved parenchyma. In addition, the interlobular and arcuate arteries show a characteristic lesion that consists of medial hypertrophy, reduplication of the elastic lamina, and increased myofibroblastic tissue in the intima, which combine to narrow the lumen. This change, called fibroelastic hyperplasia, often accompanies hyaline arteriolosclerosis and increases in severity with age and in the presence of hypertension - Consequent to the vascular narrowing, there is patchy ischemic atrophy, which consists of (1) foci of tubular atrophy and interstitial fibrosis and (2) a variety of glomerular alterations. The latter include collapse of the GBM, deposition of collagen within the Bowman space, periglomerular fibrosis, and total sclerosis of glomeruli. When the ischemic changes are pronounced and affect large areas of parenchyma, they can produce regional scars and histologic alterations that may resemble those seen in renal ablation injury
33.
Malignant hypertension (+ gross morphology): Malignant Hypertension. What would you see histologically?
Malignant nephrosclerosis is the form of renal disease associated with the malignant or accelerated phase of hypertension; - Morphology. On gross inspection the kidney size depends on the duration and severity of the hypertensive disease. Small, pinpoint petechial hemorrhages may appear on the cortical surface from rupture of arterioles or glomerular capillaries, giving the kidney a peculiar "flea- bitten" appearance.
34.
Two histologic alterations characterize blood vessels in malignant hypertension (Fig. 20-40): - Fibrinoid necrosis of arterioles. This appears as an eosinophilic granular change in the blood vessel wall, which stains positively for fibrin by histochemical or immunofluorescence techniques. This change represents an acute event; it may be accompanied by limited inflammatory infiltrate within the wall, but prominent inflammation is not seen. Sometimes the glomeruli become necrotic and infiltrated with neutrophils, and the glomerular capillaries may thrombose. - In the interlobular arteries and arterioles, there is intimal thickening caused by a proliferation of elongated, concentrically arranged smooth muscle cells, together with fine concentric layering of collagen and accumulation of pale-staining material that probably represents accumulations of proteoglycans and plasma proteins. This alteration has been referred to as onion-skinning because of its concentric appearance. The lesion, also called hyperplastic arteriolitis, correlates well with renal failure in malignant hypertension. There may be superimposed intraluminal thrombosis. The arteriolar and arterial lesions result in considerable narrowing of all vascular lumens, ischemic atrophy and, at times, infarction distal to the abnormal vessels.
35.
Shigga-like toxin E. coli strain? Hereditary disorder characterized by multiple expanding cysts of kidneys, destroys parenchyma, and caused renal failure? Be able to tell difference between childhood and adult polycystic kidney disease, grossly (Figure 20-47 AD)
O157:H7 polycystic kidney disease
36.
37.
Figure 20-47: A and B) Autosomal-dominant adult polycystic kidney disease (ADPKD) viewed from the external surface and bisected. The kidney is markedly enlarged and contains numerous dilated cysts. D) Liver cysts in adult PKD
38.
Figure 20-47c: ARPKD
Fig. 20-47 C) Autosomal-recessive childhood PKD, showing smaller cysts and dilated channels at right angles to the cortical surface.
39.
Hydropnephrosis of the kidney what does it look like grossly? (Figure 20-50)
- Hydronephrosis of the kidney, with marked dilation of the pelvis and calyces and thinning of the renal parenchyma. - Hydronephrosis is the term used to describe dilation of the renal pelvis and calyces associated with progressive atrophy of the kidney due to obstruction to the outflow of urine. - The kidney may be slightly to massively enlarged, depending on the degree and the duration of the obstruction. The earlier features are those of simple dilation of the pelvis and calyces, but in addition there is often significant interstitial inflammation, even in the absence of infection. In chronic cases the picture is one of cortical tubular atrophy with marked diffuse interstitial fibrosis. Progressive blunting of the apices of the pyramids occurs, and these eventually become cupped. In far-advanced cases the kidney may become transformed into a thin-walled cystic structure having a diameter of up to 15 to 20 cm (Fig. 20-50) with striking parenchymal atrophy, total obliteration of the pyramids, and thinning of the cortex
40.
1. Benign tumor consisting of vessels, smooth muscle, and fat 2. What do you usually see it in? Kidney tumor "mahogany brown"
1. angiomyolipoma 2. tuberous sclerosis
41.
Oncocytoma - This is an epithelial tumor composed of large eosinophilic cells having small, round, benign-appearing nuclei that have large nucleoli. It is thought to arise from the intercalated cells of collecting ducts. - In gross appearance the tumors are tan or MAHOGANY BROWN, relatively homogeneous, and usually well encapsulated. However, they may achieve a large size (up to 12 cm in diameter). There are some familial cases in which these tumors are multicentric rather than solitary.
42.
Major types of renal cell carcinoma (adenocarcinoma of the kidney) Which type of renal cell carcinoma is associated with von Hippel Lindau syndrome? Morphology of Acute Pyelonephritis (pg 941 Blue box)
- clear cell carcinoma - papillary carcinoma - Chromophobe renal carcinoma - Collecting duct (Bellini duct) carcinoma clear cell carcinoma - current studies implicate the VHL gene in the development of both familial and sporadic clear cell tumors
43.
44.
The hallmarks of acute pyelonephritis are patchy interstitial suppurative inflammation, intratubular aggregates of neutrophils, and tubular necrosis. The suppuration may occur as discrete focal abscesses involving one or both kidneys, which can extend to large wedge-shaped areas of suppuration (Fig. 20-28). The distribution of these lesions is unpredictable and haphazard, but in pyelonephritis associated with reflux, damage occurs most commonly in the lower and upper poles. - Figure 20-28 Acute pyelonephritis. Cortical surface shows grayish white areas of inflammation and abscess formation.
45.
Three complications of acute pyelonephritis are encountered in special circumstances.
- Papillary necrosis is seen mainly in diabetics and in those with urinary tract obstruction. Papillary necrosis is usually bilateral but may be unilateral. One or all of the pyramids of the affected kidney may be involved. On cut section, the tips or distal two thirds of the pyramids have areas of gray-white to yellow necrosis (Fig. 20-30). On microscopic examination the necrotic tissue shows characteristic coagulative necrosis, with preservation of outlines of tubules. The leukocytic response is limited to the junctions between preserved and destroyed tissue. - Pyonephrosis is seen when there is total or almost complete obstruction, particularly when it is high in the urinary tract. The suppurative exudate is unable to drain and thus fills the renal pelvis, calyces, and ureter with pus. - Perinephric abscess is an extension of suppurative inflammation through the renal capsule into the perinephric tissue
46.
Figure 20-38
Figure 20-38 Close-up of the gross appearance of the cortical surface in benign nephrosclerosis illustrating the fine, leathery granularity of the surface.
47.
Autosomaldominant (adult) polycystic kidney disease (ADPKD) ADPKD Morphology.
is a hereditary disorder characterized by multiple expanding cysts of both kidneys that ultimately destroy the renal parenchyma and cause renal failure
48.
- In gross appearance, the kidneys are usually bilaterally enlarged and may achieve enormous sizes; weights as high as 4 kg for each kidney have been reported. The external surface appears to be composed solely of a mass of cysts, up to 3 to 4 cm in diameter, with no intervening parenchyma (Fig. 20-47A and B). - However, microscopic examination reveals functioning nephrons dispersed between the cysts. - The cysts may be filled with a clear, serous fluid or, more usually, with turbid, red to brown, sometimes hemorrhagic fluid. As these cysts enlarge, they may encroach on the calyces and pelvis to produce pressure defects. The cysts arise from the tubules throughout the nephron and therefore have variable lining epithelia. On occasion, papillary epithelial formations and polyps project into the lumen. Bowman capsules are occasionally involved in cyst formation, and glomerular tufts may be seen within the cystic space - About 40% have one to several cysts in the liver (polycystic liver disease) that are usually asymptomatic. is genetically distinct from adult polycystic kidney disease. Perinatal, neonatal, infantile, and juvenile subcategories have been defined, depending on the time of presentation and presence of associated hepatic lesions. The first two are the most common; serious manifestations are usually present at birth, and the young infant might succumb rapidly to renal failure
49.
Autosomalrecessive (childhood) polycystic kidney disease (ARPKD)
50.
ARPKD Morphology.
- The kidneys are enlarged and have a smooth external appearance. On cut section, numerous small cysts in the cortex and medulla give the kidney a spongelike appearance. Dilated elongated channels are present at right angles to the cortical surface, completely replacing the medulla and cortex (Fig. 20-47C). - On microscopic examination, there is cylindrical or, less commonly, saccular dilation of all collecting tubules. The cysts have a uniform lining of cuboidal cells, reflecting their origin from the collecting ducts. - In almost all cases the liver has cysts associated with portal fibrosis (Fig. 20-47D) and proliferation of portal bile ducts.
51.
Typical Hemolytic Uremic Syndrome: Atypical Hemolytic Uremic Syndrome:
- This is the best-characterized form of HUS. Most cases occur following intestinal infection with strains of E. coli (the most common being O157:H7) that produce Shiga-like toxins - Atypical HUS occurs mainly in adults in a number of different settings. More than half of those affected have an inherited deficiency of complement-regulatory proteins, most commonly factor H, which normally breaks down the alternative pathway C3 convertase and protects cells from damage by uncontrolled complement activation. 1. The antiphospholipid syndrome, either primary or secondary to SLE (lupus anticoagulant). In this setting the microangiopathy tends to follow a chronic course. 2. Complications of pregnancy or the postpartum period. So-called postpartum renal failure is a form of HUS that usually occurs after an uneventful pregnancy, 1 day to several months after delivery. The condition has a grave prognosis, although recovery can occur in milder cases. 3. Vascular diseases affecting the kidney, such as systemic sclerosis and malignant hypertension. 4. Chemotherapeutic and immunosuppressive drugs, such as mitomycin, cyclosporine, cisplatin, and gemcitabine. 5. Irradiation of the kidney. - TTP is classically manifested by the pentad of fever, neurologic symptoms, microangiopathic hemolytic anemia, thrombocytopenia, and renal failure. it is usually caused by antibodies (either autoimmune or drug-induced) or genetic defects that lead to functional deficits in ADAMTS13. - The most common cause of deficient ADAMTS13 activity is inhibitory autoantibodies, and the majority of those with such antibodies are women. central nervous system involvement is the dominant feature, whereas renal involvement occurs in only about 50% of patients.
52.
53.
A variety of miscellaneous conditions or exposures are occasionally associated with atypical forms of HUS. These include:
54.
Thrombotic thrombocytopenic purpura (TTP) - pg 952-953
55.
Nephrolithiasis: (figure 20-51)
Nephrolithiasis (renal stones) is manifested by severe spasms of pain (renal colic) and hematuria, often with recurrent stone formation.
56.
Table 20-12: Types of Kidney Stones
57.
Table 20-3: The Glomerular Syndromes
58.
Table 20-7: Causes of Nephrotic Syndrome
59.
Table 20-11: Summary of Renal Cystic Diseases
You might also like
- Non-Profit Organization Funds Gregory Grabovoi TeachingsDocument95 pagesNon-Profit Organization Funds Gregory Grabovoi Teachingsssss87va93% (27)
- Free AssociationDocument10 pagesFree AssociationimorkzoneNo ratings yet
- UW Path NoteDocument218 pagesUW Path NoteSophia Yin100% (4)
- CPT ComprehensiveDocument14 pagesCPT Comprehensivesha100% (1)
- Nbme 13Document22 pagesNbme 13Schi WeiNo ratings yet
- Endocrine Pathology p17-32Document16 pagesEndocrine Pathology p17-32zeroun24No ratings yet
- Robbin's SummariesDocument98 pagesRobbin's SummariesnopedontsuemepleaseNo ratings yet
- Patho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Document12 pagesPatho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Grant GarcesNo ratings yet
- NbmeDocument5 pagesNbmeRahul ShuklaNo ratings yet
- (Mebooksfree Com) Rev&Pat&Gen&Gar&Gup&8thDocument633 pages(Mebooksfree Com) Rev&Pat&Gen&Gar&Gup&8thcharlie100% (7)
- Infectious Disease Pathology p56-75Document20 pagesInfectious Disease Pathology p56-75zeroun24No ratings yet
- Lung Head and NeckDocument26 pagesLung Head and Neckzeroun24100% (2)
- Ebook Download LinksDocument13 pagesEbook Download LinksPA201467% (3)
- General pathology reviewDocument93 pagesGeneral pathology reviewPrarthanaNo ratings yet
- Nbme 18 AnswersDocument27 pagesNbme 18 AnswersUsmle Usmle100% (1)
- Table of Genetic Disorders: Download A Copy of This Study GuideDocument11 pagesTable of Genetic Disorders: Download A Copy of This Study Guideerica perezNo ratings yet
- Ch.1 Baby Robbins OutlineDocument11 pagesCh.1 Baby Robbins OutlinePA2014100% (3)
- Lymphomas and Leukemias ChartDocument2 pagesLymphomas and Leukemias ChartPA2014No ratings yet
- Lymphomas and Leukemias ChartDocument2 pagesLymphomas and Leukemias ChartPA2014No ratings yet
- Step 1 Uworld PDFDocument25 pagesStep 1 Uworld PDFRegents Park Business Center100% (1)
- MBBS Pathology MCQsDocument8 pagesMBBS Pathology MCQsShahzad Asghar Arain80% (5)
- EHSMS Performance and Incident ReportingDocument38 pagesEHSMS Performance and Incident ReportingravimanasNo ratings yet
- GI PathologyDocument22 pagesGI Pathologyzeroun24100% (5)
- Hemodynamic Disorders, Thromboembolic Disease and ShockDocument13 pagesHemodynamic Disorders, Thromboembolic Disease and Shockpjcanero100% (5)
- Patho4-6 - Liver (Dr. Dy)Document13 pagesPatho4-6 - Liver (Dr. Dy)miguel cuevas100% (1)
- 480 MCQs With Answers of Goljan PathologyDocument382 pages480 MCQs With Answers of Goljan PathologySana Sheikh96% (28)
- Secret Pathology NotesDocument60 pagesSecret Pathology NotesJamee MmsNo ratings yet
- Top 100 Pathology Secrets List W/ NotesDocument6 pagesTop 100 Pathology Secrets List W/ NotesPA2014100% (4)
- Top 100 Pathology Secrets List W/ NotesDocument6 pagesTop 100 Pathology Secrets List W/ NotesPA2014100% (4)
- CNS Pathology SummaryDocument38 pagesCNS Pathology Summaryimeds100% (2)
- Pathology Qbank ChecklistDocument12 pagesPathology Qbank Checklistdr_sadiq100% (1)
- Hematologic Pathology p36-47Document12 pagesHematologic Pathology p36-47zeroun24No ratings yet
- Usmle SuperDocument239 pagesUsmle SupermaksventileNo ratings yet
- General Pathology Bimonthly Exam Compilation Updated 2Document197 pagesGeneral Pathology Bimonthly Exam Compilation Updated 2Cherry Rahima100% (1)
- SURGPATH - 2.1 The Gastrointestinal Tract (Robbins) - TableDocument8 pagesSURGPATH - 2.1 The Gastrointestinal Tract (Robbins) - TableAngela Caguitla100% (1)
- International Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessFrom EverandInternational Medical Graduate and the United States Medical Residency Application: A Guide to Achieving SuccessRaghav GovindarajanNo ratings yet
- Endocrine System - Part 1 (Robbins)Document28 pagesEndocrine System - Part 1 (Robbins)sarguss14100% (2)
- Infectious Disease Pathology p31-55Document25 pagesInfectious Disease Pathology p31-55zeroun2450% (2)
- Robbins Ch. 26 Bones Joints and Soft-Tissue Tumors Review QuestionsDocument7 pagesRobbins Ch. 26 Bones Joints and Soft-Tissue Tumors Review QuestionsPA2014100% (1)
- Chapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of DiseaseDocument12 pagesChapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of DiseaseArun Nayak86% (7)
- Aapi Ebook June 19 2017Document621 pagesAapi Ebook June 19 2017AAPIUSANo ratings yet
- ASCP Safety - All Exercises (1-13)Document28 pagesASCP Safety - All Exercises (1-13)PA2014No ratings yet
- Pathology Slides 1Document28 pagesPathology Slides 1SydNo ratings yet
- High Yield ReviewDocument8 pagesHigh Yield ReviewfrabziNo ratings yet
- Robbins Pathology Chapter 13 - White Blood CellsDocument7 pagesRobbins Pathology Chapter 13 - White Blood Cellsscorpiosphinx7980% (5)
- Pathology A - The Cell As A Unit of Health and DiseaseDocument13 pagesPathology A - The Cell As A Unit of Health and DiseaseYui VainNo ratings yet
- Chapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of Disease PDFDocument12 pagesChapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of Disease PDFRitz Celso100% (1)
- 2001 GuidelinesDocument195 pages2001 Guidelinesrzahid86% (7)
- NASAL SEPTUM DEVIATION: CAUSES, SYMPTOMS AND SURGICAL CORRECTIONDocument105 pagesNASAL SEPTUM DEVIATION: CAUSES, SYMPTOMS AND SURGICAL CORRECTIONNguyễn ThànhNo ratings yet
- Chapter 2 (Questions 2008-2009 Compiled)Document89 pagesChapter 2 (Questions 2008-2009 Compiled)vetpathforum100% (1)
- SURVIVOR’S GUIDE Quick Reviews and Test Taking Skills for USMLE STEP 1From EverandSURVIVOR’S GUIDE Quick Reviews and Test Taking Skills for USMLE STEP 1Rating: 5 out of 5 stars5/5 (2)
- Notes Pathoma Webinar PDF PDFDocument84 pagesNotes Pathoma Webinar PDF PDFNosheen Hafeez100% (1)
- Pathology of Liver, Biliary, and PancreasDocument52 pagesPathology of Liver, Biliary, and PancreasHassan.shehri100% (11)
- Hematologic Pathology p65-87Document23 pagesHematologic Pathology p65-87zeroun24100% (1)
- LABORATORY SAFETY: A Self-Assessment Workbook - CHAPTERS 1 & 2Document5 pagesLABORATORY SAFETY: A Self-Assessment Workbook - CHAPTERS 1 & 2PA2014No ratings yet
- Nephrotic Syndrome - NotesDocument22 pagesNephrotic Syndrome - NotesHampson Malekano100% (1)
- Chapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFDocument9 pagesChapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFChethranNo ratings yet
- Model Questions on PathologyDocument4 pagesModel Questions on PathologyBhopesh Kadian100% (3)
- Chapter 10 - Diseases of Infancy and ChildhoodDocument17 pagesChapter 10 - Diseases of Infancy and ChildhoodAgnieszka WisniewskaNo ratings yet
- MidtermDocument22 pagesMidtermEmvie Loyd Pagunsan-ItableNo ratings yet
- 200 Points in Special PathologyDocument15 pages200 Points in Special Pathologyjihadeqitaal100% (1)
- GASTROINSTINAL TRACT Robbins 8th EditionDocument4 pagesGASTROINSTINAL TRACT Robbins 8th EditionLim EricNo ratings yet
- Liver - RobbinsDocument25 pagesLiver - Robbinssarguss14100% (2)
- Pathology MBBS MCQsDocument7 pagesPathology MBBS MCQsShahzad Asghar Arain100% (3)
- P.G. Curriculum M.D. Pathology Index: 1. GoalDocument18 pagesP.G. Curriculum M.D. Pathology Index: 1. GoalAvwan DududNo ratings yet
- 'Aliah's Physio NotesDocument30 pages'Aliah's Physio NotesLuqman Al-Bashir FauziNo ratings yet
- Nbme 18Document49 pagesNbme 18Romina GomezNo ratings yet
- Pathology Description/Buzz Words DiseaseDocument5 pagesPathology Description/Buzz Words Diseasebea manzanoNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Wheater's Histology Table 14.1 GI TractDocument1 pageWheater's Histology Table 14.1 GI TractPA2014No ratings yet
- Wheater's Table 11.1 - Major Components of Innate ImmunityDocument1 pageWheater's Table 11.1 - Major Components of Innate ImmunityPA2014No ratings yet
- Grossing OutlinesDocument16 pagesGrossing OutlinesPA2014No ratings yet
- Common Histology/ Pathology Special StainsDocument1 pageCommon Histology/ Pathology Special StainsPA2014No ratings yet
- Transplant Autopsy SectionsDocument1 pageTransplant Autopsy SectionsPA2014No ratings yet
- Table of Common Acid Decalcification MethodsDocument1 pageTable of Common Acid Decalcification MethodsPA2014No ratings yet
- Review of Respiratory System Epithelium TableDocument1 pageReview of Respiratory System Epithelium TablePA2014No ratings yet
- Pathology CPT Code PracticeDocument4 pagesPathology CPT Code PracticePA2014No ratings yet
- Table of Common FixativesDocument1 pageTable of Common FixativesPA2014100% (1)
- Tissue Banking Power PointDocument21 pagesTissue Banking Power PointPA2014No ratings yet
- ABO Blood TypingDocument1 pageABO Blood TypingPA2014No ratings yet
- Kidney Biopsy ProcedureDocument2 pagesKidney Biopsy ProcedurePA2014No ratings yet
- Surgical Pathology CPT CodesDocument3 pagesSurgical Pathology CPT CodesPA2014No ratings yet
- Adult Normal Range Organ WeightsDocument1 pageAdult Normal Range Organ WeightsPA2014No ratings yet
- CNS Microanatomy NotesDocument8 pagesCNS Microanatomy NotesPA2014No ratings yet
- Gross Pathology Skin DictationsDocument1 pageGross Pathology Skin DictationsPA2014No ratings yet
- Nephron and Renin-AngiotensinDocument1 pageNephron and Renin-AngiotensinPA2014No ratings yet
- Bacterial Meningitis Chart PDFDocument1 pageBacterial Meningitis Chart PDFPA2014No ratings yet
- VDJv5 Home Edition User GuideDocument68 pagesVDJv5 Home Edition User GuidePA2014No ratings yet
- E. Coli Types Summary PDFDocument1 pageE. Coli Types Summary PDFPA2014No ratings yet
- ROBBINS Ch. 21-28 Most Commons List HightlightsDocument4 pagesROBBINS Ch. 21-28 Most Commons List HightlightsPA2014100% (1)
- Table of MusclesDocument4 pagesTable of MusclesPA2014No ratings yet
- Descriptive Terms PDFDocument15 pagesDescriptive Terms PDFPA2014No ratings yet
- Robbins Table 7-2 Benign Vs Malignant CharacteristicsDocument1 pageRobbins Table 7-2 Benign Vs Malignant CharacteristicsPA2014No ratings yet
- Table 6-2 RobbinsDocument1 pageTable 6-2 RobbinsPA2014No ratings yet
- Photosensitizing Agents and Their Applications in PhototherapyDocument26 pagesPhotosensitizing Agents and Their Applications in PhototherapyMagesh SNo ratings yet
- Med 1 Block 2 - Wet Lab NotesDocument36 pagesMed 1 Block 2 - Wet Lab NotesluckyNo ratings yet
- Neonatal Disease Severity Scoring SystemsDocument6 pagesNeonatal Disease Severity Scoring Systemsida ayu agung WijayantiNo ratings yet
- Essential Health Services and PlansDocument4 pagesEssential Health Services and Planszahara mahalNo ratings yet
- 3rd Periodical Grade 10Document3 pages3rd Periodical Grade 10diomedescolar.13No ratings yet
- Mu 089Document4 pagesMu 089Rahul RaiNo ratings yet
- Case Analysis Tool (CAT) Worksheet: Student's NameDocument7 pagesCase Analysis Tool (CAT) Worksheet: Student's NameDina KristevaNo ratings yet
- Faecal AnalysisDocument83 pagesFaecal AnalysisJoseph SabidoNo ratings yet
- Lesson 1: Health and Skill Related FitnessDocument2 pagesLesson 1: Health and Skill Related FitnessCrhystal Joy ReginioNo ratings yet
- Science Magazine, Issue 6657 (August 4, 2023)Document175 pagesScience Magazine, Issue 6657 (August 4, 2023)Kim LevrelNo ratings yet
- Kelas 3Document5 pagesKelas 3RojNo ratings yet
- BBL™ Mueller Hinton Broth: - Rev. 02 - June 2012Document2 pagesBBL™ Mueller Hinton Broth: - Rev. 02 - June 2012Manam SiddiquiNo ratings yet
- Answer Key - Asepsis Study Guide NURS 122Document2 pagesAnswer Key - Asepsis Study Guide NURS 122leiaroseNo ratings yet
- Basic Life Support Field GuideDocument56 pagesBasic Life Support Field GuidelmaoheartsNo ratings yet
- Yellow Fever Vaccination Requirements From India - Chalo AfricaDocument148 pagesYellow Fever Vaccination Requirements From India - Chalo AfricaAbishek ChandranNo ratings yet
- Ranula: A Review of LiteratureDocument6 pagesRanula: A Review of LiteratureNicco MarantsonNo ratings yet
- Pharmacy SyllabusDocument89 pagesPharmacy SyllabusDivvela ManoharNo ratings yet
- 4446 16364 1 PBDocument8 pages4446 16364 1 PBSafira Rosyadatul AissyNo ratings yet
- CDC's HIV Infection Through Oral Sex, Fact SheetDocument2 pagesCDC's HIV Infection Through Oral Sex, Fact SheetCésar E. ConcepciónNo ratings yet
- Dystocia - Case ReportDocument51 pagesDystocia - Case ReportPaijo SusenoNo ratings yet
- Superannuation Benefits SessionDocument49 pagesSuperannuation Benefits SessionfunshareNo ratings yet
- Expressed Emotion and RelapseDocument31 pagesExpressed Emotion and RelapseshivangifbscNo ratings yet