Professional Documents
Culture Documents
ALLERGOLOGY Removals Review by Alec Maquiling: Aureus, E. Coli, C. Difficile), Toxins (Scombroid
Uploaded by
Alec MaquilingOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ALLERGOLOGY Removals Review by Alec Maquiling: Aureus, E. Coli, C. Difficile), Toxins (Scombroid
Uploaded by
Alec MaquilingCopyright:
Available Formats
ALLERGOLOGY Removals Review By Alec Maquiling
OUTLINE I. Adverse Food Reactions II. Anaphylaxis III. Urticaria and Angioedema C4. Cross-reactivity: when an antibody reacts not only with the original allergen but also with a similar allergen -NOTE: LATEX cross reacts with banana, avocado, kiwi, and chestnuts C5. Correlation with other diseases - FA coexists with asthma, atopic dermatitis, eosinophilic esophagitis, and exercise-induced anaphylaxis -Coexistence of FA and ASTHMA is a risk factor for asthma exacerbations - Exercise-induced anaphylaxis: it happens when you eat a certain food (most common triggers: shellfish, alcohol, tomatoes, cheese, celery), then you exercise. The food triggers mentioned can be eaten WITHOUT symptoms in the absence of exercise. - 75% of patients who experience this are females! C6. Natural History of Food Allergy - Most FA will tolerate milk, egg, soy and wheat (but time course varies and may occur as late as teenage years) - A higher initial level of serum IgE against a certain food is associated with a lower rate of resolution C7. Types of Food Allergy (REMEMBER THIS) C7.1 IgE-MEDIATED FOOD ALLERGY C7.1.1 Clinical Features: -RAPID onset (within 1-2 hours) -Resolve quickly (within minutes to few hours) -Several symptoms involved: MOST COMMONLY INVOLVED: SKIN, 2nd most commonly involved: Gastrointestinal C7.1.2 Examples Allergy of IgE-Mediated Food
I. ADVERSE FOOD REACTIONS Definition: ANY reaction following the ingestion of a food. A. ORAL FOOD TOLERANCE: suppression of adverse immune responses to nonharmful food antigens. A1. Mechanisms: 1. Mucosal Barrier (Intestinal Intraepithelial cells, secretory IgA, Regulatory T cells, Commensal Flora) 2. Balance of Th1 and Th2 cells B. FOOD INTOLERANCE: adverse WITHOUT a clear immune mechanism event
B1. HOST factors: enzyme deficiencies, GI disorders, idiosyncratic reaction, psychologic, migraines B2. FOOD factors: infectious organisms (S. aureus, E. coli, C. difficile), toxins (scombroid poisoning [histamine]), pharmacologic agents, contaminants C. FOOD ALLERGY (FA): a reaction WITH an immune mechanism C1. Prevalence - 2.5% of newborn infants have hypersensitivity to COW MILK in the FIRST year of life. -About 1.5% of young children are allergic to EGGS. C2. Common food allergens (in the Philippines) - Seafood, fish, eff, milk, soy, peanuts (Note: Chicken allergy is NOT common) - PEANUT allergy: most common cause of anaphylaxis in children leading to an ER consultation. - REMEMBER: PROTEIN component is responsible for causing food allergy C3. Genetics (chance of getting food allergy) - If both parents both have food allergy: 50-80% - If both parents are atopic: 40-60% - If one of the parents have food allergy: 40% - If neither parent has food allergy: 15%
1. Oral Allergy Syndrome -aka POLLEN-associated FA syndrome (because it also commonly affects those who are allergic to pollens) -allergy usually to RAW fruits and vegetables - confined to LIPS, MOUTH, THROAT 2. Acute Urticaria - rapid onset after ingestion of food characterized by round or irregular shaped PRURITIC WHEALS
ALLERGOLOGY Removals Review By Alec Maquiling
3. Angioedema -often occurs in combination with urticaria -NON-pitting, NON-pruritic, well-defined edematous swelling that involves subcutaneous, abdominal organs or upper airway. C7.1.3 Examples of Non-IgE-Mediated Food Allergy 1. Food Protein-Induced Allergic Proctocolitis -in healthy infants who have visible specks or streaks of blood with mucus in the stool -many infants present while being breast-fed 2. Food Protein-Induced Enterocolitis Syndrome - presents as chronic emesis, diarrhea, failure to thrive - in young people, most common cause are milk and soy protein -in adults, most often related crustacean shellfish ingestion. C7.1.4 Mixed Conditions (both IgE and NonIgE-mediated) 1. Eosinophilic Esophagitis - LOCALIZED inflammation of the esophagus 2. Esophageal Gastroenteritis -pathologic infiltration of the GI tract by eosinophils 3. Atopic Dermatitis - skin barrier dysfunction - mutation on the protein FILAGGRIN - Atopic March (Atopic Dermatitis then Asthma then Allergic Rhinitis) C8. Diagnosis of Food Allergy -FA should be considered in patients with anaphylaxis or any combination of symptoms that occur within minutes to hours of ingesting food. - Although History and PE can aid in the diagnosis, they CANNOT be considered diagnostic of FA. Moreover, parent and patient reports must be CONFIRMED because 50 to 90% of presumed FAs are not allergies. - IgE-mediated Skin Prick Test: cannot be diagnostic BUT can be used to confirm ABSENCE of IgE-mediated reaction - Double Blind Placebo Controlled Oral Food Challenge (Gold Standard) C9. Management of Food Allergy - currently NO CURE exists - standard of care: STRICT ALLERGEN AVOIDANCE -NOTE: VERY IMPORTANT to memorize Labels that Indicate Egg Protein (particularly ALBUMIN, binder, coagulant, egg white, egg yolk, emulsifier, globulin, lecithin, livetin, lysozyme, OVALBUMIN, OVAMUCIN, OVOVITELLIN, powdered egg, vitellin, whole egg) and food that may contain egg protein (baked goods, baking mixes, boullion, breakfast cereals, cake flours, candy, cookies, egg noodles, French toast, ice cream, macaroni, cocoa, marshmallows, MEATBALLS, SAUSAGES,
You might also like
- Drummond Methods For The Economic Evaluation of Health Care Programmes PDFDocument461 pagesDrummond Methods For The Economic Evaluation of Health Care Programmes PDFGerman Camilo Viracacha Lopez80% (10)
- Labor Pain ManagementDocument1 pageLabor Pain ManagementKenneth Sy100% (5)
- Cns 765 Final Case StudyDocument10 pagesCns 765 Final Case Studyapi-581708536No ratings yet
- Pre-Op Case Protocol #4Document2 pagesPre-Op Case Protocol #4IC BNo ratings yet
- Laboratory Administration For Pathologists: Wagar, Horowitz & Siegal's Second Edition (PUB312)Document1 pageLaboratory Administration For Pathologists: Wagar, Horowitz & Siegal's Second Edition (PUB312)Alec MaquilingNo ratings yet
- CASE 28 Recurrent Abdominal PainDocument5 pagesCASE 28 Recurrent Abdominal PainRoseNo ratings yet
- Case Presentation: NeurologyDocument19 pagesCase Presentation: NeurologySydrex SarmientoNo ratings yet
- Becoming A Teacher Someday: Group 4 2G-MTDocument14 pagesBecoming A Teacher Someday: Group 4 2G-MTSophia SaquilayanNo ratings yet
- Pharmacology - Chapter 29Document5 pagesPharmacology - Chapter 29Ashley-Michelle LewisNo ratings yet
- Histology QuestionsDocument3 pagesHistology QuestionsAlec Maquiling100% (1)
- Cerebral Concussion - PresentationDocument19 pagesCerebral Concussion - PresentationAira AlaroNo ratings yet
- MCQ1FULLDocument176 pagesMCQ1FULLtheintrov100% (11)
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- 06.2 Inborn Error of Metabolism - Iii B - Trans PDFDocument10 pages06.2 Inborn Error of Metabolism - Iii B - Trans PDFAshim AbhiNo ratings yet
- Approach To The Child With Anemia - UpToDateDocument41 pagesApproach To The Child With Anemia - UpToDateDaniel Enrique CardenasNo ratings yet
- Critical Appraisal RCTDocument7 pagesCritical Appraisal RCTAisya FikritamaNo ratings yet
- Protein Energy MalnutritionDocument16 pagesProtein Energy MalnutritionAisha Abdullah ManzurNo ratings yet
- DIC Case StudyDocument7 pagesDIC Case StudyRobertNo ratings yet
- PulmoconDocument64 pagesPulmoconapi-3704562100% (1)
- Oral Cases Study Guide - PediatricsDocument68 pagesOral Cases Study Guide - PediatricsJohn100% (1)
- Metabolic Syndrome GuideDocument15 pagesMetabolic Syndrome GuideMariaEllyNobetaHutabarat100% (1)
- Surgery Case AppendicitisDocument30 pagesSurgery Case AppendicitisSarahNo ratings yet
- GP Reg - Asthma and Spirometry 2011Document114 pagesGP Reg - Asthma and Spirometry 2011minerva_stanciuNo ratings yet
- Oral Revalida Im Cases Dec. 12 and 13 2020Document16 pagesOral Revalida Im Cases Dec. 12 and 13 2020Bea Y. Bas-ongNo ratings yet
- Detecting Dengue Hemorrhagic FeverDocument4 pagesDetecting Dengue Hemorrhagic FeverPatrick DeeNo ratings yet
- Disturbances in Respiratory FunctionDocument6 pagesDisturbances in Respiratory FunctionSeff CausapinNo ratings yet
- DR Kumar Ponnusamy Biochemistry-Genetics USMLE Preparatory Course BIOGEN Reusable On-Line Resources For Large Group Teaching-Learning in Relatively Short TimeDocument1 pageDR Kumar Ponnusamy Biochemistry-Genetics USMLE Preparatory Course BIOGEN Reusable On-Line Resources For Large Group Teaching-Learning in Relatively Short TimeDr Kumar Ponnusamy100% (1)
- AntibioticsDocument30 pagesAntibioticsRoza RahbeniNo ratings yet
- Typhoid FeverDocument68 pagesTyphoid FeverLd Rachel PableoNo ratings yet
- Evaluation and Management of Pediatric Community-Acquired PneumoniaDocument46 pagesEvaluation and Management of Pediatric Community-Acquired PneumoniaJan Marvin Lichauco MendozaNo ratings yet
- Clinical CaseDocument17 pagesClinical CaseDev ROYNo ratings yet
- Eustachian Tube Guide - Anatomy, Function, Otitis MediaDocument8 pagesEustachian Tube Guide - Anatomy, Function, Otitis MediamuhammadridhwanNo ratings yet
- Pku AlkDocument33 pagesPku AlkSharf WangNo ratings yet
- Consensus guidelines for treatment of pediatric nephrotic syndromeDocument14 pagesConsensus guidelines for treatment of pediatric nephrotic syndromeSara Ilyas KhanNo ratings yet
- Taking History in PaediatricsDocument7 pagesTaking History in PaediatricsNikola IgnjatovicNo ratings yet
- Acute Pneumonia: Richard T. Ellison III and Gerald R. DonowitzDocument30 pagesAcute Pneumonia: Richard T. Ellison III and Gerald R. DonowitzNilay ChatterjeeNo ratings yet
- Chapter6 TB MeningitisDocument50 pagesChapter6 TB MeningitisAldwin BagtasNo ratings yet
- Neonatal Jaundice Clinical Presentation - History, Physical Examination PDFDocument5 pagesNeonatal Jaundice Clinical Presentation - History, Physical Examination PDFPaola Méndez NeciosupNo ratings yet
- 9-13 1 PM Structure, Classification & ReplicationDocument26 pages9-13 1 PM Structure, Classification & ReplicationsepuluhtigaNo ratings yet
- Stevens Johnson DiseaseDocument5 pagesStevens Johnson DiseaseShammy RNNo ratings yet
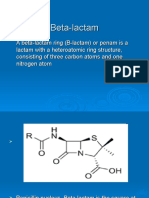
- Beta LactamDocument18 pagesBeta LactamCesar Saba0% (1)
- Pyogenic Liver AbscessDocument10 pagesPyogenic Liver AbscessErnesto Sebastian GarcíaNo ratings yet
- Pae-Central Nervous SystemDocument17 pagesPae-Central Nervous SystemMegha ProjectsNo ratings yet
- Acute DiarrheaDocument32 pagesAcute Diarrheashesh100% (1)
- Not Mine Survival GuideDocument21 pagesNot Mine Survival GuideJestin AquinoNo ratings yet
- Hormon GDSDocument23 pagesHormon GDSBRI KUNo ratings yet
- Parasitic Diseases at a GlanceDocument2 pagesParasitic Diseases at a GlanceStarrie94No ratings yet
- Infectious Diseases GuideDocument30 pagesInfectious Diseases GuideSarahNo ratings yet
- PedsCases - Anaphylaxis Emergency TreatmentDocument5 pagesPedsCases - Anaphylaxis Emergency TreatmentSara Ilyas KhanNo ratings yet
- 9th Semester Paediatrics NotesDocument84 pages9th Semester Paediatrics NotesJeevan VijayNo ratings yet
- Childhood Asthma Etiology and EpidemiologyDocument24 pagesChildhood Asthma Etiology and EpidemiologyEstella100% (1)
- Medical Case 1: Language Centre of Malahayati University at 2010Document16 pagesMedical Case 1: Language Centre of Malahayati University at 2010putri1114No ratings yet
- Exam 1 DiseasesDocument1 pageExam 1 DiseasesSolomon Seth SallforsNo ratings yet
- Malassezia Furfur An-An Ap-Ap Naturally Found On The SkinDocument48 pagesMalassezia Furfur An-An Ap-Ap Naturally Found On The SkinNikki ValerioNo ratings yet
- Pathophysiology of AsthmaDocument71 pagesPathophysiology of AsthmaChin ChanNo ratings yet
- Enterovirus & PoliomyelitisDocument17 pagesEnterovirus & PoliomyelitisAbdulsalam HashiNo ratings yet
- Parapneumonic Pleural Effusions and Empyema Thoracis: Causes, Symptoms and TreatmentDocument4 pagesParapneumonic Pleural Effusions and Empyema Thoracis: Causes, Symptoms and TreatmentLorentina Den PanjaitanNo ratings yet
- DiabeticcasestudyDocument7 pagesDiabeticcasestudyapi-272773859No ratings yet
- Omphalocele and GastroschisisDocument12 pagesOmphalocele and Gastroschisisluisisea100% (1)
- Case Presentation Og HyperthyroidismDocument7 pagesCase Presentation Og HyperthyroidismMegan Mendoza0% (2)
- Pulmonary Atresia With Ventricular Septal Defect: Systematic ReviewDocument10 pagesPulmonary Atresia With Ventricular Septal Defect: Systematic ReviewIvan VeriswanNo ratings yet
- Asthma Pathophysiology and Risk FactorsDocument98 pagesAsthma Pathophysiology and Risk FactorsyayayanizaNo ratings yet
- Diarrhea 2016Document37 pagesDiarrhea 2016oli garkiNo ratings yet
- Peptic Ulcer DiseaseDocument14 pagesPeptic Ulcer DiseasePernel Jose Alam MicuboNo ratings yet
- Practice Guidelines: For Family PhysiciansDocument0 pagesPractice Guidelines: For Family PhysiciansMuhammad GoharNo ratings yet
- CP Nonhodgkinlymph 13protocol 3201 PDFDocument15 pagesCP Nonhodgkinlymph 13protocol 3201 PDFAlec MaquilingNo ratings yet
- Microbiology MMV-Sample-MCQsDocument8 pagesMicrobiology MMV-Sample-MCQsMuhammad AttiqueNo ratings yet
- CP Hematologic Bonemarrow 19 4000 PDFDocument15 pagesCP Hematologic Bonemarrow 19 4000 PDFAlec MaquilingNo ratings yet
- Education System Bosnia and Herzegovina PDFDocument21 pagesEducation System Bosnia and Herzegovina PDFAlec MaquilingNo ratings yet
- Handwashing, Gowning, GlovingDocument3 pagesHandwashing, Gowning, GlovingAlec MaquilingNo ratings yet
- Handwashing, Gowning, GlovingDocument3 pagesHandwashing, Gowning, GlovingAlec MaquilingNo ratings yet
- Psych - Mood DisordersDocument46 pagesPsych - Mood DisordersAlec MaquilingNo ratings yet
- ParagonimusDocument2 pagesParagonimusAlec MaquilingNo ratings yet
- MannitolDocument2 pagesMannitolAlec MaquilingNo ratings yet
- Piezosurgery: By, Prathusha.U CRI Department of Public Health Dentistry Chettinad Dental CollegeDocument36 pagesPiezosurgery: By, Prathusha.U CRI Department of Public Health Dentistry Chettinad Dental CollegePrathusha Umakhanth100% (1)
- Malnutrition in Critical Illness and Beyond A Narrative Review PDFDocument9 pagesMalnutrition in Critical Illness and Beyond A Narrative Review PDFEsteban DavidNo ratings yet
- Mindful Practice: Ronald M. EpsteinDocument8 pagesMindful Practice: Ronald M. EpsteinphilosophienNo ratings yet
- N120 Final Review PDFDocument7 pagesN120 Final Review PDFsutopianoNo ratings yet
- Diabetes TrackerDocument1 pageDiabetes Trackerwildlifewarrior_zrsNo ratings yet
- Agni Dagdha. Group-T Patients Were Treated With Indigenous Drugs and Group-C PatientsDocument14 pagesAgni Dagdha. Group-T Patients Were Treated With Indigenous Drugs and Group-C PatientsKrishnaNo ratings yet
- Medical Design BriefsDocument62 pagesMedical Design Briefsneto512No ratings yet
- Patient'S Peripheral Arterial Disease Risk FactorsDocument2 pagesPatient'S Peripheral Arterial Disease Risk FactorsKrystel BatinoNo ratings yet
- Health Apps - A ToolkitDocument3 pagesHealth Apps - A ToolkitAlexandra WykeNo ratings yet
- AntacidsDocument2 pagesAntacidsMa Corazon MelecioNo ratings yet
- ReferatDocument26 pagesReferatAtikahNo ratings yet
- Juvenile Idiopathic Arthritis (Jia) : IAP UG Teaching Slides 2015-16Document15 pagesJuvenile Idiopathic Arthritis (Jia) : IAP UG Teaching Slides 2015-16KathirNo ratings yet
- Therapeutically Aspects in Esophageal Atresia: RI Spataru, Niculina Bratu, A NicaDocument4 pagesTherapeutically Aspects in Esophageal Atresia: RI Spataru, Niculina Bratu, A Nicanatacha479No ratings yet
- Drugs Induce Hematologic DisordersDocument3 pagesDrugs Induce Hematologic DisorderspaymanmatinNo ratings yet
- Prasugrel and RosuvastatinDocument7 pagesPrasugrel and RosuvastatinMohammad Shahbaz AlamNo ratings yet
- Chapter 38 - Pediatric and Geriatric HematologyDocument3 pagesChapter 38 - Pediatric and Geriatric HematologyNathaniel Sim100% (2)
- Electrical Burn PathophysiologyDocument1 pageElectrical Burn PathophysiologydanicaNo ratings yet
- Cytotoxins Pose Risks for Healthcare WorkersDocument2 pagesCytotoxins Pose Risks for Healthcare WorkersMaria Nesen NuezNo ratings yet
- Chapter 10Document45 pagesChapter 10Hannah BuquironNo ratings yet
- Virtual Hematology Slide AtlasDocument57 pagesVirtual Hematology Slide Atlasdangrabell86% (7)
- Lincomycin: Drug Information: ALERT: US Boxed WarningDocument12 pagesLincomycin: Drug Information: ALERT: US Boxed WarningsadiaNo ratings yet
- Trigeminal Neuralgia GuideDocument15 pagesTrigeminal Neuralgia Guideandreas kevinNo ratings yet
- A History of Prostate Cancer Cancer, Men and Medicine First Edition PDFDocument248 pagesA History of Prostate Cancer Cancer, Men and Medicine First Edition PDFMarcela Osorio DugandNo ratings yet
- Practices of Self-Medication Among Tribal Population North Maharashtra (Khandesh)Document5 pagesPractices of Self-Medication Among Tribal Population North Maharashtra (Khandesh)Latasha WilderNo ratings yet
- Poster ProjectDocument1 pagePoster Projectapi-291204444No ratings yet