Professional Documents
Culture Documents
Qi NCP
Uploaded by
Jesse Israel TadenaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Qi NCP
Uploaded by
Jesse Israel TadenaCopyright:
Available Formats
Cues
Nursing Diagnosis
Analysis
Goal & Objectives GOAL:
Nursing Intervention INDEPENDENT:
Rationale
Evaluation
SUBJECTIVE: - Pangatlong beses ko na kasi dito, kaya ayoko na talaga bumalik. Gusto ko na umuwi
Anxiety related
EFFECTIVENESS 1. Was the
patient calmed and relaxed ?
to
Changes in environmen t and routines
OBJECTIVE: >Anger and Irritability > Dark circles under eyes >Flushed >Dry mouth >v/s taken and recorded as follows: BP: 130/80 mmHg PR: 89bpm RR: 14cpm Temp: 36.1 degrees Celsius
Anxiety is a vague uneasy feeling of discomfort or dread accompanied by an autonomic response (the source often nonspecific or unknown to the individual); a feeling of apprehension caused by anticipation of danger. It is an alerting signal that warns of impending danger and enables the individual to take measures to deal with the threat.
After 2 hours of nursing interventions,
Patient will appear calmed and relaxed
OBJECTIVES:
Acknowledge but do not reinforce use of denial. Avoid confrontation s as much as possible.
__Yes __No Why?_____________ EFFICIENCY
Denial can be beneficial in reducing anxiety but can delay dealing with the truth or reality of the current situation. Confronta tion can promote anger and boost use of denial which eventually reduces
Patient will exhibit behaviors of acceptance
2. Were the interventions done within the timeframe? __Yes __No Why?_____________ APPROPRIATENESS Were the interventions realistic to the norms? __Yes __No Why?_____________ ACCEPTABILITY Was the patient cooperative and willing to the interventions
Patient will be able to demonstrat e relaxation techniques ( deep breathing, positive visualizatio n) Patient will be able to recall
positive behaviors to reduce stress
Acknowledge patients awareness anxiety.
cooperatio n and recovery may be delayed. Acknowledgment of the patients feelings confirms the feelings and corresponds acceptance of those feelings.
done? __Yes __No Why?_____________
of
Answer all questions truthfully. Provide information that is consistent; repeat as necessary.
Acknowledgment of the patients feelings confirms the feelings and corresponds acceptance of those feelings.
As patients level of anxiety subsides, encourage exploration of specific events prior to both the beginning and reduction of the anxious feelings.
Recognition and exploration of causative factors leading to or reducing anxious feelings are essential steps in developing alternative reactions.
Assist the patient in developing anxiety-reducing
Using anxietyreduction
skills (e.g., relaxation, deep breathing, positive visualization, and reassuring selfstatements).
strategies enhances patients sense of personal mastery and confidence.
Assist the patient to identify or recall positive coping behaviors used in the past. Be empathic and nonjudgmental while working with patient and family.
Successful behaviors in the past can be reinforced in dealing with current problems/stress, enhancing patients sense of self-control. Showing empathy and nonjudgmental attitude enhances cooperation of the patient and family.
Given this symptom profile, it is quite possible that Teddy is suffering from Dissociative Identity Disorder. However, some symptoms do not directly match those which are set out in the DSM. According to the DSM, a person may be officially diagnosed with Dissociative Identity Disorder if the following criteria are met; "A. The presence of two or more distinct identities or personality states (each with its own relatively enduring pattern of perceiving, relating to, and thinking about the environment and self). B. At least two of these identities or personality states recurrently take control of the person's behaviour. C. Inability to recall important personal information that is too extensive to be explained by ordinary forgetfulness. D. The disturbance is not due to the direct physiological effects of a substance."
Based on these criteria, it is quite evident that Teddy is in-fact suffering with Dissociative Identity Disorder. Teddy's other symptoms can also be accounted for. It is known that persons suffering with this illness may be vulnerable to auditory and visual hallucinations, in Teddy's case these are mostly visual. "An identity that is not in control may nonetheless gain access to consciousness by producing auditory or visual hallucinations (e.g., a voice giving instructions)". (DSM-IV-TR, 2000). Also, Teddy's recurrent migraines can also be seen as a common feature of Dissociative Identity Disorder. "Individuals with this type of disorder may have migraine and other types of headaches, irritable bowel syndrome and asthma". (DSM-IV-TR, 2000). "Behavioural theorists generally consider dissociation as an avoidance response that protects the person from stressful events and memories of these events. Because the person does not consciously confront these painful memories, the fear they elicit has no opportunity to extinguish". (Davison et al, 2004). It seems apparent then, that the case of Teddy Daniels fits mostly with the behavioural model. There is no evidence in the film that suggests that Teddy was physically or sexually abused as a child. It may simply be that Teddy is avoiding the stressful and traumatic memories of his wife and children's murder by creating this personality in which he believes his wife died in a fire. Teddy may simply be avoiding the stress of recognising that he in fact murdered his wife. It can be said then that the etiology of Teddy's mental illness is an accurate portrayal of real life understanding.
There are three major models proposed which attempt to account for the etiology of Dissociative Identity Disorder. The sociocognitive model describes Dissociative Identity Disorder as a result of a therapists influence during therapy. Spanos (1994) developed the idea that Dissociative Identity Disorder is merely a role-play. This doesn't necessarily mean that the patient is faking the illness but that they are responding to cues that are given during the course of therapy. Simply, if the therapist suggests to a patient that they may have multiple personalities, the patient can easily take this idea on board and begin to show more evidence as a result. "According to this view, some therapists may provide their patients with information and suggestions about multiple personality, subtly and unconsciously encouraging them to behave in ways that are consistent with these expectations, and rewarding them with extra attention and care when they adopt the role". (Oltmanns et al, 1999).
You might also like
- NCPDocument2 pagesNCPAnne De VeraNo ratings yet
- Pathophysiology of mesenchymal chondrosarcomaDocument7 pagesPathophysiology of mesenchymal chondrosarcomaMaria Grace Raquel Ormeneta100% (1)
- Novilyn C. Pataray Bsn-Ii Retinophathy: St. Paul College of Ilocos SurDocument1 pageNovilyn C. Pataray Bsn-Ii Retinophathy: St. Paul College of Ilocos SurCharina AubreyNo ratings yet
- Jake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersDocument8 pagesJake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersJake Yvan DizonNo ratings yet
- Premenstrual Dysphoric DisorderDocument11 pagesPremenstrual Dysphoric Disorderapi-3764215No ratings yet
- NCP 2Document2 pagesNCP 2ampalNo ratings yet
- NSG Care Plan SchizophreniaDocument1 pageNSG Care Plan SchizophreniaLisa LopezNo ratings yet
- The Ebn A. Evidence Based Nursing For Level III General QuestionDocument7 pagesThe Ebn A. Evidence Based Nursing For Level III General QuestionAvyNo ratings yet
- Cu 3 Week 3Document3 pagesCu 3 Week 3Maica LectanaNo ratings yet
- NCPDocument6 pagesNCPNik Rose ElNo ratings yet
- Final Case Study OutputDocument50 pagesFinal Case Study Outputudntnid2knwmeNo ratings yet
- Nursing Prioritization (Schizophrenia)Document6 pagesNursing Prioritization (Schizophrenia)Elaine Dionisio TanNo ratings yet
- Acute Confusion Nursing DiagnosisDocument4 pagesAcute Confusion Nursing Diagnosisasmika danaNo ratings yet
- Huntingtons Disease NCPDocument4 pagesHuntingtons Disease NCPJerich Mark SalasNo ratings yet
- HypopituitarismDocument2 pagesHypopituitarismAnne de VeraNo ratings yet
- NCP PainDocument1 pageNCP PaindwightciderNo ratings yet
- Nursing Diagnosis: Impaired Physical Mobility Assessment Planning Intervention Rationale EvaluationDocument3 pagesNursing Diagnosis: Impaired Physical Mobility Assessment Planning Intervention Rationale EvaluationSheril Sularte CasanesNo ratings yet
- A Beautiful Mind ReviewDocument9 pagesA Beautiful Mind ReviewPatriciaChristieNo ratings yet
- CASE PRESENTATION PP - Anxiety. Tiffany GordonDocument6 pagesCASE PRESENTATION PP - Anxiety. Tiffany GordonTiffany GordonNo ratings yet
- Case Report No1Document9 pagesCase Report No1Menn PetchuayNo ratings yet
- Running Head: Comprehensive Case Study 1Document11 pagesRunning Head: Comprehensive Case Study 1api-546355462No ratings yet
- I. General ObjectiveDocument5 pagesI. General ObjectiveMr. BQNo ratings yet
- NCP ImmobiltyDocument4 pagesNCP ImmobiltyAlizza Therese Severo AnzanoNo ratings yet
- Knowledge DeficitDocument5 pagesKnowledge DeficitteamstrocaNo ratings yet
- Psychiatric Nursing Care Plans for Developing Social SupportDocument8 pagesPsychiatric Nursing Care Plans for Developing Social Supportchiki08No ratings yet
- Spontaneous Abortion Final PaperDocument11 pagesSpontaneous Abortion Final Paperapi-241242357No ratings yet
- Therapeutic CommunicationDocument3 pagesTherapeutic CommunicationPhilip Gene II Malacas100% (1)
- PathophysiologyDocument9 pagesPathophysiologySuzette PipoNo ratings yet
- X. Nursing Care Plan: ObjectiveDocument6 pagesX. Nursing Care Plan: ObjectiveRenea Joy ArruejoNo ratings yet
- Scizophrenia NCP1Document13 pagesScizophrenia NCP1Kholid Abu Mohammad AlfaizinNo ratings yet
- Subjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationDocument2 pagesSubjective:: Assessment Diagnosis Planning Implementation Rationale EvaluationAyra PunzalanNo ratings yet
- College of Nursing Case Study on Gestational DiabetesDocument32 pagesCollege of Nursing Case Study on Gestational DiabetesRich-Anne LagarasNo ratings yet
- Cultural Competence Among Filipino NursesDocument7 pagesCultural Competence Among Filipino NursesChristine Elaine Batusin IlaganNo ratings yet
- Nursing Care Plan for Low Self EsteemDocument9 pagesNursing Care Plan for Low Self EsteemCarmelita SaltNo ratings yet
- Novilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationDocument1 pageNovilyn C. Pataray BSN - Ii: Assessment Diagnosi S Pathophysiolog Y Planning Interevention Rationale EvaluationCharina AubreyNo ratings yet
- Cholelithiasis GRAND CASE PRESDocument52 pagesCholelithiasis GRAND CASE PRESKyle Cholo CholoNo ratings yet
- A Client With Cushing's Syndrome: Nursing Care PlanDocument1 pageA Client With Cushing's Syndrome: Nursing Care PlanJulius Caesar ColladoNo ratings yet
- NCPDocument4 pagesNCPKath SicatNo ratings yet
- Psych NCPDocument1 pagePsych NCPEliza Joy Franco RNNo ratings yet
- Concept Map - Colon CancerDocument2 pagesConcept Map - Colon Cancerbea pegadNo ratings yet
- Nursing Care Plan: Acute Pain Related To Inflammatory Response Secondary To InfectionDocument2 pagesNursing Care Plan: Acute Pain Related To Inflammatory Response Secondary To InfectionTammy De GuzmanNo ratings yet
- Module 1 Am Activity On Prioritization v2Document5 pagesModule 1 Am Activity On Prioritization v2KeanuNo ratings yet
- The Silver Lining Playbook Issue #21Document3 pagesThe Silver Lining Playbook Issue #21Jerome AndresNo ratings yet
- Nursing Care Plan: Subjective: Nabalaka Ko Short Term: Independent: Goal Met Short TermDocument3 pagesNursing Care Plan: Subjective: Nabalaka Ko Short Term: Independent: Goal Met Short Termgeng gengNo ratings yet
- Final Major Case StudyDocument17 pagesFinal Major Case Studyapi-546876878No ratings yet
- Process Recording Day1Document10 pagesProcess Recording Day1Rhein ArcillaNo ratings yet
- Nursing Care Plan: Angeles University Foundation College of NursingDocument2 pagesNursing Care Plan: Angeles University Foundation College of NursingRey Ann PangilinanNo ratings yet
- Nursing Care Plan for Alcohol Withdrawal AnxietyDocument5 pagesNursing Care Plan for Alcohol Withdrawal Anxietykuro hanabusaNo ratings yet
- NCP FormatDocument3 pagesNCP FormatAl Bhert Timbal MagbalotNo ratings yet
- Nursing Care PlanDocument26 pagesNursing Care PlanDinda MaretaNo ratings yet
- ETIC211 Moral RelativismDocument1 pageETIC211 Moral RelativismNadineNo ratings yet
- Rle Module Rle Unit Week: Bachelor of Science in Nursing: Rle NCM 105 - Psychiatric NursingDocument5 pagesRle Module Rle Unit Week: Bachelor of Science in Nursing: Rle NCM 105 - Psychiatric NursingJordz PlaciNo ratings yet
- 6 Nursing Care Plan 1Document2 pages6 Nursing Care Plan 1Denise Louise PoNo ratings yet
- Assessment Nursing Diagnosis Scientific Explanation Planning Intervention Rationale Evaluation IndeoendentDocument3 pagesAssessment Nursing Diagnosis Scientific Explanation Planning Intervention Rationale Evaluation IndeoendentDiane Sarino CabonceNo ratings yet
- Termination PhaseDocument2 pagesTermination PhaseDarlene LaudeNo ratings yet
- I. Nursing Care Plan Assessment Diagnosis Planning Intervention EvaluationDocument4 pagesI. Nursing Care Plan Assessment Diagnosis Planning Intervention EvaluationCherubim Lei DC FloresNo ratings yet
- 2.D Ndera CaseDocument9 pages2.D Ndera CaseNsengimana Eric MaxigyNo ratings yet
- Depressive Disorders: Presented by Syed - Khaja.Aliuddin M.SC.DDocument14 pagesDepressive Disorders: Presented by Syed - Khaja.Aliuddin M.SC.DAli SyedNo ratings yet
- Posttraumatic Stress DisorderDocument9 pagesPosttraumatic Stress DisorderNsengimana Eric MaxigyNo ratings yet
- Stabilizing The Urinary CatheterDocument2 pagesStabilizing The Urinary CatheterJesse Israel TadenaNo ratings yet
- Marine Equipment and Supplies Table of ContentsDocument5 pagesMarine Equipment and Supplies Table of ContentsJesse Israel TadenaNo ratings yet
- Casepres FEDEL Oct. 5Document21 pagesCasepres FEDEL Oct. 5Jesse Israel TadenaNo ratings yet
- Far Eastern University Institute of Nursing SY: 2013-2014Document3 pagesFar Eastern University Institute of Nursing SY: 2013-2014Jesse Israel TadenaNo ratings yet
- Rabies, FiliarasisDocument4 pagesRabies, FiliarasisJesse Israel TadenaNo ratings yet
- Pa - Feu NRMFDocument9 pagesPa - Feu NRMFJesse Israel TadenaNo ratings yet
- A. Inspects Skull For: Head-to-Toe AssessmentDocument14 pagesA. Inspects Skull For: Head-to-Toe AssessmentJesse Israel TadenaNo ratings yet
- Significant difference in blood pressure based on BMIDocument5 pagesSignificant difference in blood pressure based on BMIJesse Israel TadenaNo ratings yet
- Ebn RMCDocument5 pagesEbn RMCJesse Israel TadenaNo ratings yet
- Statistical Analysis and Treatment of DataDocument3 pagesStatistical Analysis and Treatment of DataJesse Israel TadenaNo ratings yet
- Reflection - Bill of RightDocument1 pageReflection - Bill of RightJesse Israel TadenaNo ratings yet
- Full QXNR - 405Document7 pagesFull QXNR - 405Jesse Israel TadenaNo ratings yet
- Erik EriksonDocument1 pageErik EriksonJesse Israel TadenaNo ratings yet
- Accomplishment Report FinalDocument4 pagesAccomplishment Report FinalJesse Israel TadenaNo ratings yet
- NCP, Patho RugayDocument7 pagesNCP, Patho RugayJesse Israel TadenaNo ratings yet
- RRL - Weight, AgeDocument2 pagesRRL - Weight, AgeJesse Israel Tadena0% (1)
- Early Postoperative Treatment of Surgical Scars Using A Fractional Carbon Dioxide LaserDocument7 pagesEarly Postoperative Treatment of Surgical Scars Using A Fractional Carbon Dioxide LaserdoctorbanNo ratings yet
- Anaphy & SchematicDocument3 pagesAnaphy & SchematicJesse Israel TadenaNo ratings yet
- Cudia Et AlDocument2 pagesCudia Et AlJesse Israel TadenaNo ratings yet
- New RN seeks mental health positionDocument5 pagesNew RN seeks mental health positionJesse Israel TadenaNo ratings yet
- The StormDocument3 pagesThe StormJesse Israel TadenaNo ratings yet
- Ebn - FesDocument5 pagesEbn - FesJesse Israel TadenaNo ratings yet
- Perez Resignation Letter CompleteDocument1 pagePerez Resignation Letter CompleteJesse Israel TadenaNo ratings yet
- Anaphy & SchematicDocument3 pagesAnaphy & SchematicJesse Israel TadenaNo ratings yet
- Sensation and PerceptionDocument13 pagesSensation and PerceptionJesse Israel TadenaNo ratings yet
- PA - Fe DelmundoDocument9 pagesPA - Fe DelmundoJesse Israel TadenaNo ratings yet
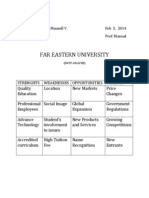
- FEU SWOT Analysis Report 2014Document1 pageFEU SWOT Analysis Report 2014Jesse Israel TadenaNo ratings yet
- Psychoanalytic Theory & Ideological Theories - For Review OnlyDocument28 pagesPsychoanalytic Theory & Ideological Theories - For Review OnlyJesse Israel TadenaNo ratings yet
- Ecologic Model AURIDocument3 pagesEcologic Model AURIJM AcNo ratings yet
- CeleryDocument2 pagesCeleryJesse Israel TadenaNo ratings yet
- History of Philippine Education under JapanDocument2 pagesHistory of Philippine Education under JapanMaeNo ratings yet
- Documentation - Lego HouseDocument2 pagesDocumentation - Lego Houseapi-582199472No ratings yet
- CSTP 5: Assessing Students For Learning: Emerging Exploring Applying Integrating InnovatingDocument10 pagesCSTP 5: Assessing Students For Learning: Emerging Exploring Applying Integrating InnovatingNancy CampNo ratings yet
- Marketing Plan Bachelor of Elementary Education (ETEEAP)Document6 pagesMarketing Plan Bachelor of Elementary Education (ETEEAP)Caila Chin DinoyNo ratings yet
- MODULE 1 - LearnDocument10 pagesMODULE 1 - LearnAsida Maronsing DelionNo ratings yet
- Wills & Succession 2021Document13 pagesWills & Succession 2021michelle zatarainNo ratings yet
- Grammatical Transformations-Synopsis+Tasks (копія)Document3 pagesGrammatical Transformations-Synopsis+Tasks (копія)Софія Жмут100% (1)
- Coaching Your Team As A Collective Makes It StrongerDocument7 pagesCoaching Your Team As A Collective Makes It StrongerRick LowNo ratings yet
- Effects of Absenteeism To The Academic Performances of Grade 12 Students in Ama Computer College Cebu Campus 1 SEMESTER 2018-2019Document7 pagesEffects of Absenteeism To The Academic Performances of Grade 12 Students in Ama Computer College Cebu Campus 1 SEMESTER 2018-2019Jdjarren panerNo ratings yet
- HRD Climate SurveyDocument3 pagesHRD Climate SurveySUKUMAR67% (3)
- Tiered Task From Pre-AssessmentDocument8 pagesTiered Task From Pre-Assessmentapi-313765228No ratings yet
- Management Science Group IDocument9 pagesManagement Science Group Illaneraerika14No ratings yet
- Sti TemplateDocument2 pagesSti TemplateIvy Ruth EscobarNo ratings yet
- DLL Math Grade2 Quarter1 Week1Document7 pagesDLL Math Grade2 Quarter1 Week1SRANo ratings yet
- Exploring The Association Between Interoceptive Awareness, Self-Compassion and Emotional Regulation - Erin BarkerDocument73 pagesExploring The Association Between Interoceptive Awareness, Self-Compassion and Emotional Regulation - Erin BarkerNoemi RozsaNo ratings yet
- Strong administrator seeks network roleDocument1 pageStrong administrator seeks network roleAbidullahNo ratings yet
- Levine Et Al. - 2005 - Identity and Emergency Intervention How Social Group Membership and Inclusiveness of Group Boundaries Shape HelpiDocument11 pagesLevine Et Al. - 2005 - Identity and Emergency Intervention How Social Group Membership and Inclusiveness of Group Boundaries Shape HelpiDeepesh MoolchandaniNo ratings yet
- WK 8 Conflict - Management - Skills LaptopDocument24 pagesWK 8 Conflict - Management - Skills LaptopAMEERA SHAFIQA MOHD RASHIDNo ratings yet
- Tip Course Book 2Document30 pagesTip Course Book 2Pearly AberaNo ratings yet
- Local Language Maintenance in Kolaka Through Mekongga FolkloreDocument10 pagesLocal Language Maintenance in Kolaka Through Mekongga Folklorewarda elfiantiNo ratings yet
- Guidelines For Fs 1Document7 pagesGuidelines For Fs 1Jason Dali-onNo ratings yet
- DLL Q4 All Subject Week 2Document71 pagesDLL Q4 All Subject Week 2Lorefe Delos SantosNo ratings yet
- ACCA f1 TrainingDocument10 pagesACCA f1 TrainingCarlene Mohammed-BalirajNo ratings yet
- HernándezGarcía Yuridia S4PIDocument3 pagesHernándezGarcía Yuridia S4PILuis Hernández100% (2)
- Winter Break Assignment for Class VIDocument1 pageWinter Break Assignment for Class VIibadaligNo ratings yet
- Innovation at WorkDocument267 pagesInnovation at WorkAdhiraj A. BhaduriNo ratings yet
- keys đề khảo sát lần 2 THPT Thanh Thuỷ- đề số 9Document3 pageskeys đề khảo sát lần 2 THPT Thanh Thuỷ- đề số 9Khanh ToanNo ratings yet
- Teaching and Learning With Technology Is A Reality in Many SchoolsDocument20 pagesTeaching and Learning With Technology Is A Reality in Many Schoolshymen11No ratings yet
- Final 2023 COT English Q3 Final1Document6 pagesFinal 2023 COT English Q3 Final1Alyssa JoyceNo ratings yet
- Ang Masipag at Ang InggitDocument2 pagesAng Masipag at Ang InggitEmon MijasNo ratings yet