Professional Documents
Culture Documents
Penetration of Anti Infective Agents Into.3
Uploaded by
Thawatchai NakkaratniyomCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Penetration of Anti Infective Agents Into.3
Uploaded by
Thawatchai NakkaratniyomCopyright:
Available Formats
REVIEW ARTICLE
Clin Pharmacokinet 2011; 50 (10): 637-664 0312-5963/11/0010-0637/$49.95/0
2011 Adis Data Information BV. All rights reserved.
Penetration of Anti-Infective Agents into Pulmonary Epithelial Lining Fluid
Focus on Antibacterial Agents
Keith A. Rodvold,1 Jomy M. George2 and Liz Yoo1
1 University of Illinois at Chicago, Chicago, IL, USA 2 Philadelphia College of Pharmacy, Philadelphia, PA, USA
Contents
Abstract. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 637 1. Epithelial Lining Fluid (ELF) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 638 1.1 Collection of ELF and Limitations of Methodology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 639 1.2 Factors Influencing Penetration of Antimicrobials into ELF and Comparison with Plasma Concentrations . . . . . . . . . . . . . . . . . 640 1.3 Pharmacokinetic-Pharmacodynamic Parameters of Efficacy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 640 2. b-Lactams . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 641 2.1 Oral Penicillins and Cephalosporins . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 641 2.2 Parenteral Penicillins and Cephalosporins . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 643 2.3 Carbapenems . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 643 3. Macrolides, Azalides and Ketolides . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 645 3.1 Erythromycin, Roxithromycin, Dirithromycin and Modithromycin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 645 3.2 Clarithromycin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 649 3.3 Azithromycin. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 649 3.4 Ketolides . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 650 4. Fluoroquinolones . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 650 4.1 Ciprofloxacin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 650 4.2 Moxifloxacin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 651 4.3 Levofloxacin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 652 5. Aminoglycosides . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 652 6. Glycopeptides and Lipoglycopeptides . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 654 6.1 Vancomycin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 654 6.2 Teicoplanin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 655 6.3 Telavancin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 655 6.4 Oritavancin . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 656 7. Miscellaneous Antibacterial Agents . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 656 7.1 Linezolid . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 657 7.2 Tigecycline . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 658 7.3 Iclaprim . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 658 8. Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 658
Abstract
The exposure-response relationship of anti-infective agents at the site of infection is currently being reexamined. Epithelial lining fluid (ELF) has been suggested as the site (compartment) of antimicrobial activity against lung infections caused by extracellular pathogens. There have been an extensive number of studies conducted during the past 20 years to determine drug penetration into ELF and to compare plasma
638
Rodvold et al.
and ELF concentrations of anti-infective agents. The majority of these studies estimated ELF drug concentrations by the method of urea dilution and involved either healthy adult subjects or patients undergoing diagnostic bronchoscopy. Antibacterial agents such as macrolides, ketolides, newer fluoroquinolones and oxazolidinones have ELF to plasma concentration ratios of >1. In comparison, b-lactams, aminoglycosides and glycopeptides have ELF to plasma concentration ratios of 1. Potential explanations (e.g. drug transporters, overestimation of the ELF volume, lysis of cells) for why these differences in ELF penetration occur among antibacterial classes need further investigation. The relationship between ELF concentrations and clinical outcomes has been under-studied. In vitro pharmacodynamic models, using simulated ELF and plasma concentrations, have been used to examine the eradication rates of resistant and susceptible pathogens and to explain why selected anti-infective agents (e.g. those with ELF to plasma concentration ratios of >1) are less likely to be associated with clinical treatment failures. Population pharmacokinetic modelling and Monte Carlo simulations have recently been used and permit ELF and plasma concentrations to be evaluated with regard to achievement of target attainment rates. These mathematical modelling techniques have also allowed further examination of drug doses and differences in the time courses of ELF and plasma concentrations as potential explanations for clinical and microbiological effects seen in clinical trials. Further studies are warranted in patients with lower respiratory tract infections to confirm and explore the relationships between ELF concentrations, clinical and microbiological outcomes, and pharmacodynamic parameters.
Plasma drug concentrations in relation to the minimum inhibitory concentration (MIC) for the bacterial pathogen of interest have traditionally been used as a predictive marker of the efficacy of antibacterial agents.[1] In vitro models and clinical trials during the past two decades have dramatically expanded our knowledge of exposure-effect relationships and have established pharmacokinetic-pharmacodynamic indices for many antibacterial agents.[2-4] Hence more attention has been placed on the importance of anti-infective concentrations, not only in plasma but also at the site of infection.[5-7] Pulmonary epithelial lining fluid (ELF) and alveolar macrophages (AMs) have been advocated as important sites of infection with common extracellular and intracellular respiratory pathogens, respectively. For community-acquired pneumonia, Streptococcus pneumoniae, Moraxella catarrhalis and Haemophilus influenzae are the predominant extracellular pathogens, and Mycoplasma pneumoniae, Chlamydophila (Chlamydia) pneumoniae and Legionella pneumophila are the primary intracellular pathogens. Thus knowledge of the location of the respective pathogens, drug penetration and drug concentrations in different compartments of the lung should assist in selection of appropriate antibacterial therapy and design of dosing regimens to effectively treat lower respiratory tract infections.[8-11] The aim of this review is to provide a comprehensive summary of the concentrations of antibacterial agents in ELF and the extent of their penetration. A brief overview has been included to describe the common methodologies that are used in collecting samples from ELF, the limitations associated with
2011 Adis Data Information BV. All rights reserved.
these methods and interpretation of the data that are obtained. Also discussed are the physicochemical and host-related factors that may influence penetration of anti-infective agents at the site of lung infections, comparison of ELF to plasma (or serum) concentration ratios, and correlation of pharmacokineticpharmacodynamic parameters that are specific for each class of antibacterial agents. 1. Epithelial Lining Fluid (ELF) A wide variety of different methodologies have been used for measuring concentrations of anti-infective agents and drug distribution patterns within the lungs. Commonly employed methods have included whole-tissue homogenates, sputum, respiratory secretions, bronchial mucosa, pleural fluid, bronchoalveolar lavage (BAL), ELF, microdialysis, positron emission tomography and magnetic resonance spectroscopy.[12] It remains unclear which of these techniques is the most appropriate.[11-15] Historically, anti-infective drug concentrations were measured by obtaining lung tissue during a surgical procedure. Although this is one of the oldest methods for measuring drug concentrations in the lung, whole-tissue concentrations are no longer recommended.[14] In addition, methods that include measurement of antibacterial concentrations in sputum or bronchial secretions have been considered less than optimal.[11,12,16] For example, the shortcomings of using sputum concentrations as an indicator of lung penetration include the possibility of falsely low saliva drug concentrations (indicating poor lung penetration) because of a dilutional effect caused by saliva, or
Clin Pharmacokinet 2011; 50 (10)
Penetration of Antibacterial Agents into Pulmonary ELF
639
falsely elevated saliva drug concentrations (suggesting high lung penetration) if the antibacterial is extensively distributed into saliva but not into other pulmonary fluids or tissues. The major drawback of drug concentrations reported from whole lung tissue, bronchial tissues and/or secretions is the assumption that anti-infective agents are uniformly distributed across all lung compartments (e.g. extracellular, intracellular). Thus the reported drug concentration represents a mixture from all compartments versus a value for a specific site of activity. Methods that measure concentrations of anti-infective agents in specific compartments of the lung (e.g. ELF, interstitial fluid, AMs) are currently preferred and are considered to provide further insight into the significance of drug concentrations at the site of pulmonary infections.[5,11-14,16] ELF has been considered the likely site of extracellular respiratory micro-organisms in bacterial pneumonia and acute bacterial exacerbation of chronic bronchitis. However, one must understand that no method or sampling site is perfect, and each has its advantages, potential limitations and methodological issues.[11-16]
1.1 Collection of ELF and Limitations of Methodology
ume of ELF.[17] Urea concentrations are normally the same in plasma and in ELF, since urea is non-polar and has a low molecular weight that allows it to rapidly diffuse and establish an equilibrium across the capillary-alveolar membrane. By measuring the urea in BAL aspirate and plasma, a ratio can be calculated and the dilution of the apparent volume of ELF can be estimated (equation 1): ELF volume Volume aspirated Urea BAL aspirate Urea plasma (Eq: 1
Using the calculated value of the ELF volume, the drug concentration in ELF (CELF) can be estimated as follows (equation 2): CELF Volume of BAL CBAL ELF volume (Eq. 2)
Currently, the combination of bronchoscopy and BAL has become a safe and effective method for obtaining samples from the bronchoalveolar surface of the lower respiratory tract. The procedure involves a fibre-optic bronchoscope being passed and wedged into a subsegment of the middle or lower lung lobe. BAL is performed by instillations of three or four aliquots of sterile 0.9% normal saline solution into the lung lobe, with the fluid being immediately aspirated and placed on ice after each aliquot. The aspirate from the first instillation is usually collected separately and discarded because of significant contamination with cells from the proximal airways. The aspirates recovered from the subsequent instillations are pooled, the volume is measured and recorded, and removal of a sample for other testing (e.g. a total cell count and a differential cell count) is sent to the laboratory. The remaining volume of BAL is immediately centrifuged, the supernatant and cell pellet are separated, and samples from the supernatant for determining urea and drug concentrations are collected and frozen until the assays can be performed. A blood sample to determine urea and drug concentrations is also obtained at the time of the scheduled bronchoscopy and BAL procedure. The recovered BAL fluid is a mixture of saline, ELF and cellular components of the ELF. In order to determine the antiinfective drug concentration, the apparent volume of ELF must be estimated. Urea (or albumin or creatinine) has been commonly used as an endogenous marker to estimate the vol 2011 Adis Data Information BV. All rights reserved.
where CBAL is the drug concentration measured in BAL. The techniques of bronchoscopy and BAL are associated with a low level of technical complexity.[12] However, our review of the literature indicates that the technique for performing BAL differs among investigators, with the main variations being the dwell time, the aspiration pressure, the volume of fluid injected and the number of BAL aspirates collected.[11,15,16,18] In addition, different assay methodologies and analytical kits are used to measure urea in BAL and plasma. Each of these variables may influence the correction for ELF dilution and the apparent volume of ELF. It has been suggested by some researchers that overestimation of the ELF volume (and thus underestimation of drug concentrations) can range from 100% to 300%.[9,11,13,16] It has also been suggested that lysis of cells (e.g. AMs) in the collected BAL fluid increases the measured concentrations of anti-infective agents in ELF.[12,13,15] Finally, alterations in the ELF volume, cell counts and protein concentrations in BAL have been associated with subjects who smoke and/or have interstitial lung disease.[19,20] Therefore it is recommended that a standardized BAL procedure be established and used consistently to ensure that technical errors are minimized and that distal ELF samples are obtained. The assays for urea in plasma and BAL need to be precise and reliable. Subject recruitment needs to be carefully considered in order to minimize unexpected variability. Accurate understanding of the methodology and strict adherence to the procedures are crucial to minimize known sources of error. Other shortcomings include the difficulty of obtaining multiple ELF samples from the same subject at several sampling timepoints, because of the nature of the BAL procedure.[12,13] As a result, clinical studies require a larger number of subjects who are randomized to a single BAL sampling time.
Clin Pharmacokinet 2011; 50 (10)
640
Rodvold et al.
Several studies from Japan have been able to overcome this issue by using bronchoscopy with bronchoscopic microsampling (BMS) probes.[21-25] This technique obtains samples of ELF from the bronchial space (whereas BAL samples are obtained from the alveolar space) and does not require measurement of urea concentrations. Differences in methodology and sampling sites explain, in part, why anti-infective drug concentrations have not always been similar when BMS and BAL were performed in the same subjects.
1.2 Factors Influencing Penetration of Antimicrobials into ELF and Comparison with Plasma Concentrations
sampled. Where ratios based on AUC estimates have been reported, we have incorporated them into the text of our review.
1.3 Pharmacokinetic-Pharmacodynamic Parameters of Efficacy
There are many factors that influence antimicrobial penetration into the pulmonary compartments.[8,9,11-13,15,16] Antiinfective agents must cross the blood-bronchus barrier to reach the alveolar ELF and the lung interstitium in order to achieve adequate concentrations. This barrier is composed of an alveolar-capillary membrane. The capillary endothelium is relatively permeable; however, the alveolar membrane is virtually impermeable because of the presence of tight junctions. The major mode of transport between membranes occurs through passive diffusion. Protein binding determines the amount of the unbound drug that is present to diffuse through membranes, explaining why antimicrobials with a high degree of protein binding do not penetrate well into lung tissue. The degree of lipophilicity, as well as administration of the drug in an unionized form, determine how well the antimicrobial will penetrate tissue.[8,9,11-13,15,16] Other factors that favour penetration include the pH at the site of infection and other dynamic processes such as bronchial inflammation at the site of infection.[5,8,11] Concentrations of anti-infective agents in ELF are considered to provide useful and accurate estimates for determining extracellular drug penetration in the lungs. Various methods have been suggested to compare plasma and ELF concentrations of anti-infective agents. Nearly all studies report comparisons of concentrations (e.g. ELF and plasma concentrations) that were simultaneously obtained at both sites. In fact, that is how the data are reported in our tables for the various classes of antibacterial agents. However, since the concentration-time profiles of drugs in plasma and ELF can increase and decrease at different paces from each other (known as system hysteresis), penetration ratios will vary in magnitude with the sampling time(s) chosen. To overcome this issue, it is recommended that research studies determine penetration ratios from estimates of the area under the concentration-time curve (AUC) values of plasma and ELF data.[26,27] Accurate estimates of the AUC can be obtained even when drug concentrations are only sparsely
2011 Adis Data Information BV. All rights reserved.
Our knowledge and understanding of the pharmacokineticpharmacodynamic parameters of anti-infective agents have grown substantially over the past 30 years.[2-4] Application of these parameters has had a major influence on the dose selection, the dosing interval and/or mode of administration, development of in vivo susceptibility breakpoint determinations, assessment of bacterial resistance and the clinical drug development process. This information has had an impact on how anti-infective agents are used at the bedside and developed in research. Pharmacokinetic-pharmacodynamic parameters that correlate with the efficacy of specific anti-infective agents include (i) the percentage of time during which unbound (free) drug concentrations remain above the MIC of an infecting microorganism (fT>MIC) [in the case of b-lactams (e.g. penicillins, cephalosporins, carbapenems, monobactams), linezolid or oritavancin];[2-4,7] (ii) the ratio of the maximum unbound concentration (fCmax) to the MIC of an infecting micro-organism (fCmax/MIC) [in the case of aminoglycosides, fluoroquinolones, daptomycin, oritavancin or metronidazole];[2-4,7] and (iii) the ratio of the unbound AUC during a 24-hour time period (fAUC24) to the MIC of an infecting micro-organism (fAUC24/MIC) [in the case of fluoroquinolones, aminoglycosides, azithromycin, clarithromycin, telithromycin, doxycycline, tigecycline, vancomycin, daptomycin, telavancin, linezolid, clindamycin or quinupristin/dalfopristin].[2-4,6,7] The concepts and categorization of the pharmacokineticpharmacodynamic parameters of anti-infective agents have been based on relationships established from plasma or serum concentrations.[2-4] We are unaware of any clinical studies that have evaluated and documented similar correlations with concentrations at the site of infection (e.g. ELF) for community- or hospital-acquired lower respiratory tract infections.[6,7] While many of the reports that are included in this review have described pharmacokinetic-pharmacodynamic parameters by using ELF concentration-time data, caution must be applied in presuming that the magnitude of exposure required in ELF and/or the relationship between parameters and outcomes are the same or even similar to those observed in plasma. Studies are needed in patients with lower respiratory tract infections to confirm and explore the relationships between ELF concentrations, clinical and microbiological outcomes, and pharmacodynamic parameters.
Clin Pharmacokinet 2011; 50 (10)
Penetration of Antibacterial Agents into Pulmonary ELF
641
2. b-Lactams Intrapulmonary penetration studies have been conducted with b-lactam agents since the early 1990s. Oral and intravenous cephalosporins have accounted for the majority of these studies (tables I and II).[28-41] b-lactamb-lactamase inhibitor combinations (e.g. amoxicillin/clavulanic acid, piperacillin/tazobactam) have been evaluated for the penicillin class. Several carbapenem agents (e.g. meropenem, ertapenem, biapenam) have been studied. No ELF data have been reported for the monobactam aztreonam.
2.1 Oral Penicillins and Cephalosporins
Intrapulmonary studies of oral penicillins and cephalosporins have usually been conducted after a single oral dose (table I). The concentrations of amoxicillin and clavulanic acid in ELF were found to be similar to each other (mean values 0.89 and 0.96 mg/mL, respectively); however, these values were less than 20% of the total plasma concentrations.[28] The concentrations of oral cephalosporins in ELF were commonly observed to be less than 1 mg/mL and were often reported as
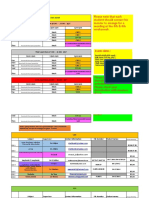
Table I. Plasma and epithelial lining fluid (ELF) concentrations of oral penicillins and cephalosporins Antibacterial agent Amoxicillin/ clavulanic acid (AMO/CLA) Cefuroxime axetil Dosage regimen Subjects (n) 500 mg AMO + 250 mg CLA 1 dose 500 mg 1 dose 500 mg 1 dose 15 Sampling time (h)a 12 Plasma concentration (mg/mL)b AMO: 6.90 [1.29.8]c CLA: 5.25 [0.79.95] 14 4 4 4 Cefpodoxime proxetil Ceftibuten 200 mg 1 dosef 6 6 400 mg 1 dose 7 4 3 Cefdinir 300 mg 1 dose 600 mg 1 dose Cefaclor 750 mg bid 7 dosesj 9 8 6 6 6 Cefditoren 400 mg 1 dose 8 8 8 a Sampling time after the last dose. b Values are expressed as mean SD unless specified otherwise. c Values are expressed as median [range]. d Fourteen ELF samples were measured in 15 patients. e Values are expressed as range. f Two tablets of cefpodoxime proxetil (130 mg per tablet; equivalent to 200 mg of cefpodoxime). 0.96.8e 6 12 24 3 6 1.9 [1.382.67]g 6.5 [4.088.08]
g c
ELF concentration (mg/mL)b CLA: 0.96 [08.36]c,d 0.7 0.2 <LLQ <LLQ <LLQ 0.22 0.13 0.12 0.14 1.6 [02.8]g 1.6 [0.762.1]
g
ELF/plasma Reference penetration ratiob 28
AMO: 0.89 [03.48]c,d NR NR 0.15 NA NA NA 0.108 0.044 0.0605 0.0479 0.13 0.12 0.38 0.15 [0.3.26]c,i 0.12 [0.0.14]c 0.88 3.2 2.6 0.381 0.501 0.232 0.181 0.318 0.192
3.9 0.5 1.1 0.3 0.06 0.12 <LLQ 1.85 0.82 1.40 1.25 15.2 [2.423.2]g 14.0 [7.817.6]
c g
29 30
31
32
13.3 [12.2515.0]g,h 4.1 [2.55.6]g,h 4 4 4 6 12 1.02.0
k
1.2 [0.42.2]g,h 0.29 [0.4.73]
c,i
2.0 [1.48.0]
33
4.2 [3.056.4]c 3.08 1.7 0.68 0.70 0.23 0.1 1.78 1.27 1.33 0.95 1.03 0.51
0.49 [0.0.59]c 2.71 0.87 2.16 1.70 0.6 0.3 0.39 0.21 0.34 0.25 0.30 0.18
34
35
2.013.0k 3.014.0k
g Values are expressed as mean [range]. h Samples at 20.25 h were not included because both plasma and ELF samples were <LLQ. i j Seven ELF samples were measured in nine patients. Modified-release formulation.
k Collection interval. bid = twice daily; LLQ = lower limit of quantification; NA = not applicable; NR = not reported; SD = standard deviation.
2011 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2011; 50 (10)
642
Rodvold et al.
Table II. Plasma and epithelial lining fluid (ELF) concentrations of parenteral penicillins and cephalosporins Antibacterial agent Piperacillin/ tazobactam (PIP/TAZ) Cefpirome Ceftazidime Dosage regimen 4 g PIP + 500 mg TAZ IV 0.5 h infusion q8h 1 g IV 0.5 h infusion 1 dose 1 g IM 1 dose Subjects (n) 10 Sampling time (h)a Steady statec Plasma concentration (mg/mL)b PIP: 24.0 13.8 TAZ: 2.4 1.2 37 5 5 5 5 5 2 g 0.5 h IV infusion 1 dose then continuous IV infusion of 4 g/d Cefepime 2 g IV 0.5 h infusion 1 dose then continuous IV infusion of 4 g/d 500 mg IV 2 h infusion q8h 4 doses 15 0.57d 1 2 4 8 12 8, 12, 18g 34.5 3.3e 39.89 10.42 36.04 9.21 13.34 4.12 6.08 1.71 1.07 0.45 39.6 15.2 ELF concentration (mg/mL)b PIP: 13.6 9.4 TAZ: 2.1 1.1 7.2 1.1e,f 2.71 0.88 2.66 0.64 1.32 0.64 0.66 0.36 0.12 0.15 8.2 4.8 ELF/plasma penetration ratiob PIP: 0.568 0.336 TAZ: 0.913 0.277 0.359 0.074e,f NR NR NR NR NR 0.206 0.089 39 37 38 Reference 36
7 7 6 6 6 6 6
8g 12
g
13.5 3.2h 13.7 3.5
h
13.7 3.0 13.5 3.3 14.9 2.3 2.55 0.99 2.00 1.07 4.58 5.82 1.51 0.39
1.01 0.99 1.12 0.255 0.366i
40
18g 2.5 4 6 8
13.3 3.6h 17.68 4.48 12.77 2.26 6.91 4.58 3.65 1.05
Ceftobiprole
41
a Sampling time after the start of the infusion unless specified otherwise. b Values are expressed as mean SD unless specified otherwise. c d e f Samples were collected at steady state after 2 d of therapy and at 5 h after a dose. Values are expressed as range. Values are expressed as mean SEM. Eight samples were available.
g Serum and ELF concentrations were sampled after 2 d of therapy at 8, 12 and 18 h during a continuous infusion. h i Twenty concentrations were available at each sampling time. The penetration ratio was calculated from AUC values for ELF and plasma.
AUC = area under the concentration-time curve; IM = intramuscularly; IV = intravenous; NR = not reported; q8h = every 8 h; SD = standard deviation; SEM = standard error of the mean.
undetectable.[29-35,42] The ratios of ELF concentrations to total plasma concentrations ranged from 0.1 to 0.38, suggesting low to moderate penetration into the ELF. The exception to this occurred following multiple doses of a modified-release formulation of cefaclor 750 mg.[34] The ELF concentrations of cefaclor were similar to the total plasma concentrations (mean values 2.71 and 3.08 mg/mL, respectively, at 4 hours) or exceeded the total plasma concentrations (mean values 2.16 and 0.68 mg/mL, respectively, at 6 hours; and 0.60 and 0.23 mg/mL, respectively, at 12 hours). Several methodological limitations of the intrapulmonary studies of oral penicillins and cephalosporins should be noted. Sampling times were often restricted in number and were often limited to the first few hours after antimicrobial administration,
2011 Adis Data Information BV. All rights reserved.
thus they did not include the entire dosing interval. The ratios of ELF concentrations to plasma concentrations were based on concentrations at these specific sampling times as opposed to a more accurate comparison being made by estimating AUCs for ELF and plasma. These issues probably contributed to the large difference between plasma and ELF concentrations, secondary to system hysteresis (e.g. concentrations in plasma and ELF often increase and decrease at different paces from each other). In addition, the ratios of ELF to plasma concentrations were based on total (versus unbound) plasma drug concentrations. Finally, the lower level of detection for measuring drug concentrations was limited, since two-thirds of the studies used microbiological assays. While a few recent studies
Clin Pharmacokinet 2011; 50 (10)
Penetration of Antibacterial Agents into Pulmonary ELF
643
have overcome most of these limitations, the ELF concentrations of cefuroxime were still undetectable throughout the entire dosing interval, and the percentages of penetration by ceftibuten and cefdinir into ELF were still less than 40%.[30,32,33]
2.2 Parenteral Penicillins and Cephalosporins
based on preclinical infection models, the pharmacokineticpharmacodynamic characteristics of the agent being studied and drug exposure information at the site of infection (e.g. the lung). In addition, this study allowed differences in ELF penetration in mice versus man (68.8% vs 25.5%) to be accounted for and dosage selection in humans to be evaluated.[41,44]
2.3 Carbapenems
Intrapulmonary studies of parenteral penicillins and cephalosporins have included a variety of subject types, modes of drug administration and differences in BAL collection techniques (table II). In critically ill patients with severe nosocomial pneumonia, three studies have been conducted using microlavage to determine ELF and plasma concentrations of piperacillin-tazobactam, ceftazidime and cefepime.[36,38,39] The mean ( standard deviation [SD]) concentrations of piperacillin and tazobactam following at least 2 days of therapy with an intravenous dosage regimen of 4 and 0.5 g every 8 hours were 13.6 9.4 and 2.1 1.1 mg/mL, respectively, which were approximately 57% and 91%, respectively, of the total plasma concentrations.[36] The same researchers used a similar study design and methods to evaluate the intrapulmonary penetration of ceftazidime and cefepime in critically ill patients receiving continuous intravenous infusions of 4 g/day.[38,39] The mean ( SD) concentrations of ceftazidime and cefepime were 8.2 4.8 and 14.1 2.8 mg/mL, respectively. However, the respective ratios of ELF to total plasma concentrations were 0.21 and 1.04. Unlike those of other parenteral cephalosporins whose ELF to total plasma concentration ratios range between 7% and 36%, the concentrations of cefepime in ELF were similar to or exceeded the total and unbound plasma concentrations (protein binding of cefepime is approximately 20%).[40,43] The discordance in penetration among the parenteral cephalosporins does not seem to be related to differences in structure or protein binding (range 1020%). A novel study design was used to evaluate drug exposure in ELF of ceftobiprole for the treatment of pneumonia caused by meticillin (methicllin)-resistant Staphylococcus aureus.[41] Population pharmacokinetic modelling of ELF and plasma concentrations from both animal and human data were used in Monte Carlo simulations to evaluate the probabilities of achieving a desired target attainment based on bacterial killing rates obtained from a preclinical pneumonia model in neutropenic mice.[44] For a dosage regimen of ceftobiprole 500 mg every 8 hours as a 2-hour intravenous infusion, the probabilities of achieving 1-log and 2-log cell kill rates were 85.6% and 79.7%, respectively, over the MIC distribution of 4958 isolates. This study provided a logical approach for evaluating dosage regimens for the treatment of lower respiratory tract infections,
2011 Adis Data Information BV. All rights reserved.
Single- and multiple-dose studies have evaluated the intrapulmonary penetration of meropenem and ertapenem (table III).[45-48] The mean concentrations of meropenem in ELF and the penetration ratios ranged from 7.07 to 0.59 mg/mL and from 0.51 to 1.04, respectively, in 30 subjects administered a single 1 g dose intravenously over 30 minutes.[45] A similar range of ELF and plasma concentrations was observed following multiple doses of 1 g every 8 hours in healthy adult subjects.[46] In both studies, concentrations of meropenem in ELF at 8 hours were undetectable or extremely low (mean 0.03 mg/mL). While plasma concentrations increased proportionally as doses of meropenem were increased, concentrations in ELF tended to decrease as meropenem doses increased. The ratios of ELF concentrations to total plasma concentrations ranged from 0.49 to 0.80 for the 500 mg dose, from 0.32 to 0.53 for the 1 g dose and from 0.048 to 0.219 for the 2 g dose.[46] It is unclear why this disproportionate percentage change in ELF concentrations occurred. In contrast to these findings, a mean penetration ratio (based on ratios of the AUC) of 0.72% was observed in critically ill patients with ventilator-associated pneumonia receiving 3-hour infusions of meropenem 2 g administered every 8 hours.[49] Subsequently, pharmacokinetic simulations based on the mean parameter vector of these data suggested that ELF concentrations of meropenem are maintained above MIC values of 1 mg/mL for nearly 30% of the dosing interval.[50] Similar median penetration ratios were observed with Bayesian parameter estimates of patients with ELF sampling (0.264) and a 9999-subject Monte Carlo simulation (0.254). Two studies have evaluated the penetration of ertapenem into ELF.[47,48] In 15 adult patients undergoing thoracotomy, the mean ELF concentrations of ertapenem ranged from 2.11 to 4.06 mg/mL during the first 5 hours after a single perioperative dose of 1 g.[47] The mean ratios of ELF concentrations to total plasma concentrations ranged from 0.062 to 0.094. In comparison, adult patients treated for early-onset ventilatorassociated pneumonia had median ELF concentrations of 9.4 and 0.3 mg/mL at 1 and 24 hours, respectively, after multiple doses of ertapenem 1 g once daily.[48] The ratios of ELF concentrations to total plasma concentrations ranged from 0.21 to
Clin Pharmacokinet 2011; 50 (10)
644
Rodvold et al.
Table III. Plasma and epithelial lining fluid (ELF) concentrations of carbapenems Antibacterial agent Meropenem Dosage regimen 1 g IV 0.5 h infusion 1 dose Subjects (n) 30c Sampling time (h)a 0.5 1 2 4 6 8 500 mg IV 0.5 h infusion q8h 4 doses 4 4 4 4 4 1 g IV 0.5 h infusion q8h 4 doses 4 4 4 4 4 2 g IV 0.5 h infusion q8h 4 doses 1 g IV 0.5 h infusion 1 dose 4 4 15e 1 2 3 5 8 1 2 3 5 8 1 3 1 3 5 1 g IV 1 h infusion q24h 15f 1g 12
g
Plasma concentration (mg/mL)b 25.96 22.16 14.98 5.30 12.01 3.48 2.51 0.68 0.57 0.27 0.29 0.24 10.9 1.3 5.2 1.6 2.4 0.9 0.3 0.4 0.0 0.0 19.0 7.6 7.5 1.3 5.3 1.5 2.0 1.3 0.0 0.0 60.9 8.0 12.8 2.7 63.1 16.9 39.7 15.2 27.2 15.5 30.3 [27.137.8]h,i 4.8 [3.96.4]
h,i
ELF concentration (mg/mL)b 5.04 3.33 7.07 2.87 3.86 2.74 2.20 2.29 0.59 1.09 NR 5.3 2.5 2.7 1.8 1.9 0.9 0.7 0.4 0.2 0.1 7.7 3.1 4.0 1.1 1.7 1.4 0.8 0.4 0.03 0.05 2.9 1.0 2.8 1.5 4.06 6.64 2.59 2.33 2.11 1.80 9.4 [8.010.7]j 2.0 [1.12.5]
j
ELF/plasma penetration ratiob 0.19 0.11 0.51 0.24 0.33 0.20 1.04 1.20 0.82 1.18 NA 0.490.80d
Reference 45
46
0.320.53d
0.048 0.219 0.0619 0.1100 0.0685 0.0645 0.0940 0.1070 0.32 [0.280.46]k 48 47
Ertapenem
24g Biapenem 300 mg IV 0.5 h infusion 1 dose 300 mg IV 3 h infusion 1 dose 6l 0.5 3
0.8 [0.51.2]h,i 18.1 2.8 6.8 1.2
0.3 [0.20.4]j 3.48 1.20 1.33 0.26 0.20 0.08 0.20 0.06 22
a Sampling time after the start of the infusion unless specified otherwise. b Values are expressed as mean SD unless specified otherwise. c Thirty subjects were assigned to one bronchoscopy sampling time (the number of subjects per sampling time was NR).
d Range for all sampling timepoints. e Fifteen subjects were enrolled, and samples were collected at each sampling time. f Fifteen subjects were assigned to one bronchoscopy sampling time.
g Samples were collected after 2 d of therapy. h Unbound serum concentration. i j k l Values are expressed as median [IQR] for 15 samples. Values are expressed as median [IQR] for five samples. Values are expressed as median [IQR] for 15 matching sample pairs. Each subject received both dosage regimens in a crossover study design.
IQR = interquartile range; IV = intravenous; NA = not applicable; NR = not reported; qxh = every x h; SD = standard deviation.
2011 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2011; 50 (10)
Penetration of Antibacterial Agents into Pulmonary ELF
645
0.64 (median 0.32). Since ertapenem is highly protein bound (e.g. 96% at 10 mg/mL and 84% at 300 mg/mL), the penetration ratios in both studies are closer to or greater than 1 if unbound plasma concentrations are considered. Kikuchi et al.[22] compared ELF concentrations in six healthy adult subjects administered a single dose of biapenem 300 mg as 0.5-hour and 3-hour intravenous infusions. The mean ( SD) ELF concentrations were 3.48 1.20 mg/mL at the end of the 0.5-hour infusion and 1.33 0.26 mg/mL at the end of the 3-hour infusion. The mean penetration ratios of ELF concentrations to total plasma concentrations were 0.20 for both infusion periods. These authors also evaluated a BMS technique, which used a polyester fibre rod probe to repeatedly obtain ELF concentrations at the surface of a bronchus (termed bronchial ELF). In contrast to the BAL sampling technique, bronchial ELF concentrations were higher with the 3-hour infusion (4.36 2.07 mg/mL) than with the 0.5-hour infusion (2.35 1.06 mg/mL). No explanations were provided for the discrepancies between the two techniques.
3. Macrolides, Azalides and Ketolides Intrapulmonary studies have been commonly conducted for agents from the antibacterial classes of macrolides, azalides and ketolides (tables IVVII).[23,24,30,51-68] The majority of reported studies have evaluated clarithromycin, azithromycin and telithromycin. Although the number of studies is small, data are available for older macrolide agents such as erythromycin, roxithromycin and dirithromycin, as well as the investigational ketolide cethromycin.
3.1 Erythromycin, Roxithromycin, Dirithromycin and Modithromycin
Intrapulmonary concentrations of erythromycin were first reported in 1995 from a multiple-dose study in 12 healthy adult subjects.[51] The mean ( SD) plasma concentrations and ELF concentrations at 4 hours after nine doses of oral erythromycin
Table IV. Plasma and epithelial lining fluid (ELF) concentrations of oral erythromycin, roxithromycin, dirithromycin and modithromycin Antibacterial agent Erythromycin Dosage regimen 250 mg q6h 9 doses Subjects (n) 4 4 4 Roxithromycin 300 mg q12h 10 doses 300 mg q12hd Dirithromycin 500 mg q24h 5 doses 8 7 5 5 5 5 5 Modithromycin 400 mg 1 dose 4 4 4 4 4 4 4 a Sampling time after the last dose. b Values are expressed as mean SD. c Two of eight subjects had ELF concentrations <LLQ (<0.2 mg/mL). d The duration of therapy was 3 mo. e Five of seven subjects had ELF concentrations <LLQ; a value of 0 was included to determine the mean ( SD). LLQ = lower limit of quantification; NR = not reported; qxh = every x h; SD = standard deviation.
2011 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2011; 50 (10)
Sampling time (h)a 4 8 12 2 NR 24 48 72 96 120 2 4 6 8 10 12 24
Plasma concentration (mg/mL)b 0.7 0.2 0.1 0.1 0.04 0.05 11.4 5.7 3.74 1.16 0.44 0.31 0.33 0.12 0.11 0.646 0.088 0.575 0.075 0.540 0.131 0.441 0.070 0.429 0.091 0.424 0.088 0.315 0.116
ELF concentration (mg/mL)b 0.8 0.1 <LLQ <LLQ 2.0 1.7c 0.90 0.68e 2.21 2.25 1.57 0.22 0.15 16.7 3.0 13.7 4.9 15.1 6.6 11.4 1.9 10.0 3.0 5.8 2.0 6.5 2.6
ELF/plasma penetration ratiob NR
Reference 51
0.17 NR 5.023 7.258 4.758 1.833 1.364 26.3 24.8 27.0 25.9 23.2 13.8 21.3
52 53 54
55
646
Rodvold et al.
Table V. Plasma and epithelial lining fluid (ELF) concentrations of oral clarithromycin Dosage regimen 200 mg 1 dose 500 mg 1 dose Subjects (n) 5 4 4 4 4 500 mg bid 7 doses 500 mg q12h 9 doses 10 3 4 4 3 4 500 mg q12h 9 doses 5 5 5 5 500 mg q12h 9 doses 5 5 5 5 1000 mg q24h 5 dosese 7 7 7 7 7 7 a Sampling time after the last dose. b Values are expressed as mean SD unless specified otherwise. c d e f Values are expressed as mean SEM. Three of five subjects had concentrations <LLQ. The clarithromycin formulation used in this study was an extended-release tablet. Five of seven subjects had concentrations <LLQ. Sampling time (h)a 3 6 12 24 48 4.25 0.27 4 8 12 24 48 4 8 12 24 4 8 12 24 3 6 9 12 24 48
c
Plasma concentration (mg/mL)b 0.36 0.07 1.0 0.6 0.25 0.21 0.07 0.05 <LLQ 3.96 1.19 2.2 0.9 2.6 0.5 0.8 0.3 0.5 0.07 0.01 0.03 3.29 0.94 1.58 0.50 0.91 0.59 0.19 0.09 2.00 0.60 1.55 0.42 1.22 0.35 0.23 0.11 1.54 0.60 1.43 0.42 2.22 0.60 1.04 0.42 0.75 0.35 0.156g
c
ELF concentration (mg/mL)b 4.84 3.39 39.6 41.1 <LLQ <LLQ <LLQ 20.46 6.7
c
ELF/plasma penetration ratiob 14 NR NR NR NR NR NR NR NR NR NR 11 14 28 31 NR NR NR NR NR NR NR NR NR NR
Reference 23 30
56 51
29.3 12.4 72.1 73.0 48.6 46.8 11.9 3.6 23.4 19.2 34.02 5.16 20.36 4.49 23.01 11.90 4.17 0.29d 34.5 29.3 26.1 7.2 15.1 11.1 4.6 3.7 6.38 3.92 6.89 4.19 11.50 6.65 7.14 7.29 6.80 3.39 6.08g
f
57
58
59
g Six of seven subjects had concentrations <LLQ. bid = twice daily; LLQ = lower limit of quantification; NR = not reported; qxh = every x h; SD = standard deviation; SEM = standard error of the mean.
250 mg every 6 hours were similar: 0.7 0.2 and 0.8 0.1 mg/mL, respectively. Unfortunately, the two other sampling times (8 and 12 hours) in this study were outside the dosing interval, and the concentrations of erythromycin were reported as undetectable (assay sensitivity = 0.05 mg/mL). Patients treated with oral erythromycin 250 mg every 6 hours for 28 days had measurable ELF concentrations at 2, 4 and 8 hours after the last dose administration.[69] The mean 2-hour ELF concentration of
2011 Adis Data Information BV. All rights reserved.
erythromycin was 0.97 mg/mL, and a similar 4-hour concentration was observed in the healthy subject study. In eight patients with mild chronic bronchitis treated with oral roxithromycin 300 mg every 12 hours for 5 days, the ELF concentration (mean SD 2.0 1.7 mg/mL) was only 17% of the simultaneously measured plasma concentration (mean SD 8.1 4.0 mg/mL).[52] In comparison, the concentration of roxithromycin in AMs was significantly higher (mean SD
Clin Pharmacokinet 2011; 50 (10)
Penetration of Antibacterial Agents into Pulmonary ELF
647
Table VI. Plasma and epithelial lining fluid (ELF) concentrations of azithromycin Dosage regimen 500 mg PO 1 dose Subjects (n) 4 4 4 6 4 500 mg PO 1 dose 4 4 4 4 4 4 500 mg PO first dose and then 250 mg PO q24h 4 doses 5 5 5 5 500 mg PO first dose and then 250 mg PO q24h 4 doses 6 5 5 5 6 6 6 5 500 mg PO first dose and then 250 mg PO q24h 4 doses 5 5 5 5 500 mg PO first dose and then 250 mg PO q24h 4 doses 4 4 4 4 500 mg IV 60 min infusion q24h 5 doses 4 4 4 Sampling time (h)a 12 24 48 72 96 6 12 24 48 120 240 4 8 12 24 4f 28
f
Plasma concentration (mg/mL)b 0.13 0.05c NR NR NR 0.01 0.13 0.07 <LLQ <LLQ <LLQ <LLQ <LLQ 0.09 0.05 0.06 0.05
d
ELF concentration (mg/mL)b NR NR 2.18 NR NR <LLQ <LLQ <LLQ <LLQ <LLQ <LLQ <LLQ 1.93
e
ELF/plasma penetration ratio NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR NR
Reference 60
30
57
0.04 0.02d 0.03 0.03
d
1.75e <LLQ 0.45 0.15 1.53 0.31 2.67 0.85 3.12 0.93 0.61 0.23 <LLQ <LLQ <LLQ 1.01 0.45g 2.18 0.25
d
0.178 0.05 0.122 0.055 0.093 0.036 0.054 0.008 0.031 0.055 0.015 0.005 <LLQ <LLQ 0.08 0.05 0.09 0.04 0.04 0.02 0.05 0.03 0.10 0.02 0.05 0.02 0.07 0.86 0.03 0.02 0.37 0.10 0.25 0.04 0.14 0.04
61
76f 124
f
172f 244
f
340f 508 4 8 12 24 4 8 12 24 4 12 24
f
58
0.95 0.40d 1.22 0.59 0.64 0.35 0.66 0.42 0.88 0.46 0.94 0.68 1.70 0.74 1.27 0.47h 2.86 1.75
g
62
63
a Sampling time after the last dose unless specified otherwise. b Values are expressed as mean SD unless specified otherwise. c Values are expressed as mean SEM.
d One of five subjects had concentrations <LLQ. e Four of five subjects had concentrations <LLQ. f Sampling time after the first dose (500 mg).
g Two of five subjects had concentrations <LLQ. h One of four subjects had concentrations <LLQ. IV = intravenous; LLQ = lower limit of quantification; NR = not reported; PO = orally; q24h = every 24 h; SD = standard deviation; SEM = standard error of the mean.
2011 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2011; 50 (10)
648
Rodvold et al.
Table VII. Plasma and epithelial lining fluid (ELF) concentrations of oral ketolides Antibacterial agent Telithromycin Dosage regimen 600 mg 1 dose 600 mg od 5 doses 600 mg od 5 doses Subjects (n) 5 5 6 6 800 mg od 5 doses 6 6 800 mg od 5 doses 7 6 7 800 mg od 5 doses 6 1 5 5 800 mg od 5 doses 5 6 6 6 Cethromycin 150 mg od 5 doses 5 5 5 5 5 300 mg od 5 doses 5 5 5 5 5 5 5 a Sampling time after the last dose. b Values are expressed as mean SD unless specified otherwise. c One of seven subjects had concentrations <LLQ. d One of six subjects had concentrations <LLQ. e Five of six subjects had plasma samples available. f Values are expressed as median. Sampling time (h)a 3 3 2 8 2 8 2 12 24 2 8 12 24 2 8 24 48 2 4 8 12 24 2 4 6 8 12 24 48 Plasma concentration (mg/mL)b 0.36 0.19 0.63 0.11 NR NR NR NR 1.86 0.31 0.23 0.05 0.08 0.03 1.97 1.64e 0.48 0.70 0.55 0.14 0.06 1.14f 0.63
f d
ELF concentration (mg/mL)b 2.94 2.64 7.51 4.54 4.91 4.00 2.26 1.17 4.24 3.14 4.31 1.87 14.89 11.35c 3.27 1.68 0.97 0.60
d c
ELF/plasma penetration ratiob NR 12 NR NR NR NR 8.57 13.58 16.77 3 2 5 7 NR 6.4 12.7 NA NR NR NR NR NR NR NR NR NR NR NR NR
Reference 24 24 64
64
65
5.22 2.79 1.09 3.47 3.88 0.84 0.54 5.5f 3.7
f
66
67
0.055f <0.03 0.12 0.08 0.09 0.06 0.04 0.02 0.02 0.01 0.01 0.11 0.25 0.15 0.38 0.21 0.18 0.07 0.09 0.03 0.10 0.06 0.01 0.01 0.00 0.00
0.82d,f 0.17
f,g
0.9 1.0 0.9 0.2 0.8 0.5 0.3 0.3 0.1 0.1 2.5 1.6 2.7 2.0 1.6 0.8 0.9 0.8 0.8 0.4 0.1 0.1 0.0 0.0
68
68
g Three of six subjects had concentrations <LLQ. LLQ = lower limit of quantification; NA = not applicable; NR = not reported; od = once daily; SD = standard deviation.
21.0 10.0 mg/mL). In a study evaluating the immunoregulatory effects of roxithromycin in patients with chronic respiratory tract infections, the ELF concentrations were measurable in only two of seven patients (1.56 and 4.77 mg/mL) who had received 3 months of oral roxithromycin 300 mg every 12 hours.[53]
2011 Adis Data Information BV. All rights reserved.
The plasma concentrations in these two patients were 2.55 and 8.78 mg/mL, respectively. Dirithromycin was one of the first macrolide agents for which ELF concentrations were reported to be significantly higher than concurrent plasma concentrations.[54] In 25 patients
Clin Pharmacokinet 2011; 50 (10)
Penetration of Antibacterial Agents into Pulmonary ELF
649
treated for acute exacerbation of chronic bronchitis, the mean ELF concentrations during the first 2472 hours after five oral doses of dirithromycin 500 mg once daily ranged from 1.57 to 2.25 mg/mL. Subsequent mean ELF concentrations were 0.22 mg/mL at 96 hours and 0.15 mg/mL at 120 hours. In comparison, the mean plasma concentrations ranged from 0.44 mg/mL at 24 hours to 0.11 mg/mL at 120 hours. A similar range of ELF concentrations was observed between 2 and 24 hours (approximately 2.37 mg/mL) after the last oral dose of dirithromycin 500 mg once daily in 20 patients treated for acute exacerbation of mild chronic obstructive pulmonary disease.[69] The investigational bridged bicyclic macrolide (bicyclolide) modithromycin (also known as S-013420 and EDP-420) has recently been studied in healthy Japanese subjects.[55] Following a single oral dose of 400 mg, the mean concentrations of modithromycin in ELF between 2 and 24 hours ranged from 5.8 to 16.7 mg/mL. The mean plasma concentrations during this same time period ranged from 0.315 to 0.646 mg/mL. As with other newer agents, the mean concentrations of modithromycin in AMs (range 61176 mg/mL) were well above those observed in plasma and ELF.
3.2 Clarithromycin
9 hours and 0.75 mg/mL at 24 hours. The concentrations of clarithromycin in AMs ranged between 43 and 1087 mg/mL (mean 303 mg/mL) and were comparable to values reported with the immediate-release formulation of clarithromycin. Maximum concentration (Cmax) values in plasma, ELF and AMs occurred at 9 hours with the extended-release formulation, which was later than with the immediate-release formulation. In vitro and in vivo murine pharmacodynamic models have made use of clinically observed plasma and ELF concentrations to evaluate the bactericidal activity and/or postantibacterial effect of clarithromycin against isolates of H. influenzae and/or S. pneumoniae.[70-73] In addition, Monte Carlo simulations have been used to assess the ability of pharmacodynamic parameters (e.g. an AUC/MIC ratio of 25) to determine susceptibility breakpoints and target attainment rates against penicillinsusceptible and -resistant strains of S. pneumoniae.[74,75] Overall, these studies support the concept that the higher concentrations of clarithromycin in ELF contribute to the potential efficacy of clarithromycin against S. pneumoniae strains with MIC values up to 8 mg/mL.
3.3 Azithromycin
Two single-dose studies of clarithromycin have suggested that ELF concentrations are measurable only within the first 6 hours after administration of oral doses of 200 and 500 mg (table V).[23,30] Four multiple-dose studies of the immediaterelease formulation of clarithromycin have reported plasma and intrapulmonary concentrations following the oral dosage regimen of 500 mg twice daily.[51,56-58] The mean concentrations of clarithromycin in ELF ranged between 20.46 and 32.4 mg/mL at 4 hours and between 15.1 and 48.6 mg/mL at 12 hours. Plasma concentrations were 10- to 60-fold lower and ranged between 2.0 and 3.96 mg/mL at 4 hours and between 0.8 and 1.22 mg/mL at 12 hours. The reported concentrations were fairly consistent between studies. Plasma and ELF concentrations of the active metabolite, 14-hydroxy-clarithromycin, were also reported in two studies. Concentrations of 14-hydroxy-clarithromycin in ELF (range 1.215.09 mg/mL) were greater than concurrent plasma concentrations (0.46.41 mg/mL), but the difference (1.1to 7.45-fold) was less than that observed with clarithromycin. One study evaluated the intrapulmonary disposition of the extended-release formulation of clarithromycin 1000 mg once daily.[59] Following five doses, the mean concentrations in ELF were 11.50 mg/mL at 9 hours and 6.80 mg/mL at 24 hours, and they remained constant throughout the 24-hour dosing interval. The mean plasma concentrations were 2.22 mg/mL at
2011 Adis Data Information BV. All rights reserved.
Six studies (two single-dose studies and four multiple-dose studies) have evaluated the intrapulmonary disposition of oral azithromycin (table VI). Interestingly, the single-dose studies provided minimal information, since most plasma and ELF samples had undetectable concentrations.[30,60] The multipledose studies indicated that the mean ELF concentrations ranged between 0.64 and 3.12 mg/mL during the first 24 hours after the last dose of the standard oral dosing regimen of azithromycin.[57,58,61,62] The concentrations of azithromycin in ELF were fairly stable and demonstrated minimal fluctuations throughout the 24-hour dosing interval. The mean plasma concentrations during this same time period ranged from 0.03 to 0.1 mg/mL. No study has reported ELF to plasma concentration ratios. However, the ELF concentrations were approximately 10- to 20-fold higher than the concurrent plasma concentrations. Single oral doses of azithromycin in the immediate-release and extended-release formulations were compared in 64 patients who had been diagnosed with lung cancer and required open-chest surgery for lung resection.[76] For the immediaterelease formulation, a single 500 mg dose resulted in AUC from 0 to 24 hours (AUC24) values in serum and ELF of 3.1 and 2.3 mg h/mL, respectively. Following a 2 g dose of the extendedrelease formulation, the AUC24 values in serum and ELF were 10.0 and 17.6 mg h/mL, respectively. Higher exposure was also
Clin Pharmacokinet 2011; 50 (10)
650
Rodvold et al.
observed in AMs and whole lung tissues with the extendedrelease formulation. Only one study has reported plasma and ELF concentrations following multiple intravenous doses of azithromycin 500 mg once daily.[63] The plasma concentrations at the time of bronchoscopy were comparable (range 0.090.49 mg/mL) to those associated with oral dosing once the differences in the dose and oral bioavailability were taken into account. Concentrations in ELF ranged from 0.79 to 5.86 mg/mL and were slightly higher than the values associated with oral dosing. The estimated AUC24 of azithromycin in ELF (45.8 mg h/mL) was approximately 5.6-fold higher than the AUC24 in plasma (8.2 mg h/mL) following intravenous dosing. The observed azithromycin concentrations in ELF and plasma have been used to investigate in vitro bactericidal activity and pharmacodynamic target attainment rates against clinical isolates of S. pneumoniae and H. influenzae. In ELF, azithromycin demonstrated greater potency, killing rates and postantibacterial effects than clarithromycin against H. influenzae and tended to be adequate for eradication of macrolidesusceptible S. pneumoniae (suggested susceptibility breakpoint 2 mg/mL).[73,74,77-80] The probability of achieving target attainment rates was lower with azithromycin than with clarithromycin.[74]
0.1 to 0.9 mg/mL after the 150 mg once-daily dosage regimen and from 0.1 to 2.7 mg/mL after the 300 mg once-daily dosage regimen (table VII).[68] In comparison, the plasma concentrations were approximately 10-fold lower than the ELF concentrations, whereas the AM concentrations were 10-fold higher than the ELF concentrations. Several pharmacodynamic studies have evaluated the in vitro activity and target attainment potential of telithromycin against pathogens commonly associated with community-acquired pneumonia (e.g. macrolide-susceptible and -resistant S. pneumoniae, and b-lactamase-positive and -negative H. influenzae).[73,82-85] Using simulated total and unbound serum and ELF concentrations of telithromycin, these studies have provided recommendations for potential pharmacokinetic-pharmacodynamic parameter values of the Cmax/MIC and AUC24/MIC ratios associated with bacteriostatic and bactericidal activity, as well as no regrowth of telithromycin-susceptible bacteria over 2448 hours.[73,82,83] 4. Fluoroquinolones Most fluoroquinolones that have been developed during the past 25 years have been studied to determine the degree of lung penetration. Ciprofloxacin, moxifloxacin and levofloxacin are currently the most commonly recommended fluoroquinolones for the treatment of lower respiratory tract infections. With that in mind, our review focuses on intrapulmonary penetration studies of those three fluoroquinolones only. However, a list of references has been provided for those readers who have an interest in similar studies of other fluoroquinolones.[86-100]
4.1 Ciprofloxacin
3.4 Ketolides
Several intrapulmonary studies have reported ELF concentrations for oral telithromycin dosage regimens of 600 and 800 mg once daily (table VII).[24,64-68] Like clarithromycin and azithromycin, telithromycin achieves higher and sustained extracellular concentrations (2- to 17-fold) in ELF than in plasma. The mean ELF concentrations following telithromycin 800 mg once daily for 5 days were approximately 5.0 and 0.9 mg/mL at 2 hours and 24 hours, respectively. The total plasma concentrations at these same sampling times averaged 1.9 and 0.1 mg/mL, respectively. The reported mean ratios for ELF to total plasma concentrations at individual sampling times ranged from 2 to 14.9. A mean penetration ratio of 7.95 (with AUC values of 83.73 and 10.53 mg h/mL for ELF and plasma, respectively) has been reported, based on a population pharmacokinetic analysis and a 10 000-subject Monte Carlo simulation.[81] These ratios would be greater if unbound plasma concentrations are considered (telithromycin plasma protein binding: 6070%). Intracellular concentrations of telithromycin are even higher in AMs than in ELF and can range from 50- to >500-fold greater than total plasma concentrations.[64-67] For the investigational ketolide antibacterial cethromycin, the ELF concentrations between 2 and 24 hours ranged from
Several single- and multiple-dose studies have evaluated intrapulmonary penetration of oral ciprofloxacin in healthy adult subjects and patients undergoing diagnostic bronchoscopy (table VIII).[96,98-101] The concentration-time profile following a single oral dose of 500 mg suggests that ciprofloxacin does not achieve adequate ELF concentrations throughout the dosing interval. Although the mean plasma and ELF concentrations were similar (2.33 and 2.13 mg/mL, respectively) at 2.5 hours, subsequent ELF concentrations (range 548 hours) were below the lower limit of quantification (LLQ).[99,100] When multiple oral doses of ciprofloxacin 500 mg were administered every 12 hours, the mean concentrations were slightly lower in ELF than in plasma throughout the dosing interval (2.11 vs 1.87 mg/mL at 4 hours and 0.55 vs 0.41 mg/mL at 12 hours).[101] Two studies that measured ELF concentrations of ciprofloxacin between
Clin Pharmacokinet 2011; 50 (10)
2011 Adis Data Information BV. All rights reserved.
Penetration of Antibacterial Agents into Pulmonary ELF
651
Table VIII. Plasma and epithelial lining fluid (ELF) concentrations of oral ciprofloxacin and moxifloxacin Antibacterial agent Ciprofloxacin Dosage regimen 250 mg bid 4 d 250 mg bid 4 d 500 mg 1 dose Subjects (n) 11 13 4 4 4 4 500 mg 1 dose 5 5 5 500 mg q12h 9 doses 4 4 4 Moxifloxacin 400 mg 1 dose 19
g
Sampling time (h)a 36c 36 6 12 24 48 2.5 5 12 4 12 24 2.2 11.8 24.1
c
Plasma concentration (mg/mL)b 1.1 0.2d 1.19 0.16 0.95 0.32 0.23 0.07 0.03 0.01 <LLQ 2.33e 1.13 0.43
e e d
ELF concentration (mg/mL)b 2.0 1.7d 3.0 1.05 <LLQ <LLQ <LLQ <LLQ 2.13e,f <LLQ <LLQ
f d
ELF/plasma penetration ratiob 1.85 0.47d 2.13 0.5 NA NA NA NA NR NA NA NR NR NA 6.78 2.29 5.19 1.90 6.95 1.43 NR NR NR NR
d
Reference 96 98 99
100
2.11 0.35 0.55 0.09 0.08 0.03 3.22 1.25 1.14 1.42 0.51 1.19 3.23 0.88 2.21 0.59 1.68 0.53 0.78 0.39
1.87 0.91 0.41 0.10 <LLQ 20.7 1.92 5.90 2.20 3.57 1.58 11.66 11.86 7.80 5.08 10.52 3.66 5.71 6.28
101
102
400 mg q24h 5 doses
4 4 4 4
4 8 12 24
62
a Sampling time after the last dose. b c d e f g Values are expressed as mean SD unless specified otherwise. Values are expressed as range. Values are expressed as mean SEM. Values are expressed as median. Values measured in four subjects. A total of 19 subjects were studied, but information on how many subjects were assigned to each sampling time was not provided in the study.
bid = twice daily; LLQ = lower limit of quantification; NA = not applicable; NR = not reported; qxh = every x h; SD = standard deviation; SEM = standard error of the mean.
3 and 6 hours after multiple doses of an oral regimen of 250 mg every 12 hours reported that ELF concentrations (2.0 and 3.0 mg/mL at 3 and 6 hours, respectively) were higher than concurrent plasma concentrations (1.1 and 1.19 mg/mL at 3 and 6 hours, respectively).[96,98]
4.2 Moxifloxacin
Concentrations of moxifloxacin in ELF have been reported in two studies involving oral administration (table VIII).[62,102] After a single oral dose of moxifloxacin 400 mg, the mean concentrations in ELF ranged from 20.7 mg/mL at 2.2 hours to 3.57 mg/mL at 24.1 hours.[102] The mean ratios of ELF concentrations to total plasma concentrations ranged from
2011 Adis Data Information BV. All rights reserved.
5.19 to 6.95. Similarly, after multiple oral doses of moxifloxacin 400 mg every 24 hours in older adult subjects (mean age 67 10 years), the mean plasma concentrations ranged from 3.23 mg/mL at 4 hours to 0.78 mg/mL at 24 hours and the mean ELF concentrations ranged from 11.66 mg/mL at 4 hours to 5.71 mg/mL at 24 hours.[62] Even if protein binding (approximately 50%) is taken into account, ELF concentrations remain 2.5- to 3.5-fold higher than unbound plasma concentrations throughout a 24-hour dosing interval. A recent study using a Calu-3 lung epithelial cell model suggested that P-glycoproteinmediated active transport mechanisms influence the secretion of moxifloxacin into the lung and may explain, in part, why higher concentrations are observed in ELF than in plasma.[103]
Clin Pharmacokinet 2011; 50 (10)
652
Rodvold et al.
The intrapulmonary data generated from these two studies have been used in numerous evaluations to compare the pharmacodynamic characteristics of moxifloxacin with those of other antibacterial agents that are commonly used in lower respiratory tract infections.[77,79,104-110] Most investigations have used simulated plasma and ELF concentrations in vivo to link in vitro bactericidal killing activity, eradication rates against various genotypes and/or resistant patterns of S. pneumoniae and S. aureus, prevention of selection or emergence of resistance, and achievement of AUC/MIC target attainment rates. These studies have provided further support for the concept that ELF concentrations contribute to the efficacy of moxifloxacin against pathogens associated with lower respiratory tract infections.
4.3 Levofloxacin
was 1.16. The mean and median ratios were 3.18 (SD 5.71) and 1.43 (95% confidence interval [CI] 0.143, 19.12), respectively, when calculations were based on 1000-subject Monte Carlo simulations. The penetration ratio was greater than 1 in 61% of simulations. Other investigators have also evaluated pharmacodynamic target attainment rates using estimates of ELF concentrations of levofloxacin in hospitalized patients with communityacquired pneumonia and in a murine pneumonia model of Pseudomonas aeruginosa infection.[117,118] 5. Aminoglycosides Aminoglycosides such as gentamicin, tobramycin and netilmicin are most often used intravenously or via inhalation for the treatment of serious respiratory infections involving Gramnegative organisms. Aminoglycosides are known for poor lung penetration and varied concentrations in the lung tissue depending on the anatomical site that is sampled. Intrapulmonary penetration and ELF concentrations of aminoglycosides in critically ill patients with lower respiratory tract infections have been evaluated following intravenous and intramuscular administration of single and multiple doses (table X).[119-124] Sampling of ELF concentrations in aminoglycoside studies has been limited to the first 8 hours after drug administration, and no estimation of exposure throughout the dosing interval has been provided. In general, concentrations of aminoglycosides in ELF are significantly lower than plasma concentrations during the first 1.5 hours after administration. Subsequently, the concentrations in ELF become similar to those in plasma at approximately 2 or 3 hours after administration. For example, the mean concentrations of tobramycin in ELF were 2.7 mg/mL (approximately 12% of the plasma concentration [22.4 mg/mL]) at 0.5 hours following a 30-minute intravenous infusion of 710 mg/kg.[122] Similar ELF concentrations (e.g. <3 mg/mL) were observed at 1 hour after a single dose of gentamicin 240 mg (mean SD 3.5 0.1 mg/kg) and during the first 2 hours of adjusted doses of tobramycin.[119,121] Although the mean concentrations of netilmicin in ELF were higher at 1 and 1.5 hours (7.5 and 9.6 mg/mL, respectively) after a single dose of 450 mg, these ELF concentrations were only 35% and 62% of the concurrent mean plasma concentrations (21.4 and 15.3 mg/mL, respectively).[124] Once the Cmax values of gentamicin and netilmicin in ELF occurred at 2 hours (4.24 and 14.7 mg/mL, respectively), the ELF to plasma concentration ratios were 0.85 and >1, respectively.[119,124] Subsequently, ELF and plasma concentrations of the aminoglycosides became similar to each other. Thus system hysteresis has greatly influenced the large
Clin Pharmacokinet 2011; 50 (10)
Concentrations of levofloxacin in ELF have been investigated extensively (table IX).[25,62,63,101,111-115] Studies have included single and multiple doses of levofloxacin administered both orally and intravenously at a wide range of dosages (e.g. 1001000 mg). The individuals who were studied included healthy adult subjects, patients undergoing diagnostic fibreoptic bronchoscopy, critically ill patients with severe communityacquired pneumonia and outpatients with a clinical diagnosis of mild to moderate chronic bronchitis, chronic obstructive pulmonary disease or lower respiratory tract infection. Eleven of 13 studies used plasma and ELF sampling over a 24-hour interval.[62,63,101,111-115] The mean ratios of ELF concentrations to total plasma concentrations at individual sampling times ranged from 1.0 to 4.9 when the samples were obtained between 4 and 24 hours after dosing. Several studies reported AUC24 values in plasma and in ELF. For the 500 mg dose, the mean AUC24 values ranged from 34.5 to 180 mg h/mL in ELF, compared with 50.186.7 mg h/mL in plasma.[62,63,112] For the 750 mg dose, the mean AUC24 values in ELF and in plasma were 151.4 and 95.4 mg h/mL, respectively.[63] A 1000 mg dose resulted in mean AUC24 values of 260279.1 mg h/mL in ELF and 103.6130 mg h/mL in plasma.[114,115] The ratios of ELF concentrations to plasma concentrations that were estimated from these AUC values ranged from 1.59 to 2.69. Drusano et al.[116] performed population pharmacokinetic modelling and Monte Carlo simulations based on steady-state concentrations in plasma and ELF after oral doses of levofloxacin 500 and 750 mg were administered to healthy adult subjects. The penetration ratio based on the AUC values in ELF and in plasma, derived from the mean parameter vector,
2011 Adis Data Information BV. All rights reserved.
Penetration of Antibacterial Agents into Pulmonary ELF
653
Table IX. Plasma and epithelial lining fluid (ELF) concentrations of levofloxacin Dosage regimen 100 mg PO 1 dose 500 mg PO 1 dose Subjects (n) 5 35c Sampling time (h)a 2 0.5 1 2 4 68d 1224d 500 mg PO 1 dose 8 8 8 8 8 500 mg PO q24h 5 doses 4 4 4 500 mg PO q24h 5 doses 4 3 4 4 500 mg IV 1 h infusion q24h 5 doses 4 4 4 500 mg IV 1 h infusion q24h 12
e
Plasma concentration (mg/mL)b NR 4.73 6.6 4.9 4.1 4.0 1.2 3.34 3.00 4.06 1.90 2.12 1.11 1.90 0.64 0.93 0.61 5.29 1.23 3.07 0.93 0.60 0.10 5.08 2.31 4.37 0.71 4.60 4.58 1.52 1.42 4.74 1.37 1.63 0.59 0.48 0.16 12.6 3.0
f,g
ELF concentration (mg/mL)b 1.41 0.32 4.74 10.8 9.0 10.9 10.1 NR 3.44 3.69 2.35 1.97 1.64 1.51 0.95 0.93 0.87 0.72 9.94 2.74 6.46 2.48 0.70 0.40 15.23 4.53 10.18 6,74 6.85 4.36 2.94 1.74 11.01 4.52 2.50 0.97 1.24 0.55 11.9 3.9
f,g
ELF/plasma penetration ratiob NA 1.0 1.7 0.8 3.0 2.7 NA 0.788 NR NR NR 1.043 NR NR NR NR NR NR NR NR NR NR 1.31 0.31 1.18 0.36 1.27 0.46 1.12 0.40 NR NR NR NR NR NR 4.9 NR NR NR 2.0 3.6
Reference 25 111
1 4 8 12 24 4 12 24 4 8 12 24 4 12 24 1 24
112
101
62
63
113
f,g f,g
f,g f,g
500 mg IV 1 h infusion q12h
12
1 12
19.7
17.8
113
7.7f,g 11.98 2.99 4.06 0.51 1.69 1.14 6.55 1.65 3.52 0.77 0.84 0.20 5.7 0.4 9.2 1.9 7.5 1.4 6.0 1.1 4.8 1.7 1.2 0.4
11.8f,g 22.12 14.92 9.17 5.34 1.45 0.75 12.94 0.74 6.04 0.47
h
750 mg PO q24h 5 doses
4 4 4
4 12 24 4 12 24 4 3 4 8 12 24
101
750 mg IV 1.5 h infusion q24h 5 doses
4 4 4
63
1.73 0.78 28.0 23.6 25.8 7.9 24.8 10.2 15.7 4.5 9.6 4.7 4.3 1.8
750 mg IV 2 h infusion q24h 3 doses 1000 mg IV 2 h infusion q24h 3 doses
4 4 4 4 4 4
114 114
Continued next page
2011 Adis Data Information BV. All rights reserved.
Clin Pharmacokinet 2011; 50 (10)
654
Rodvold et al.
Table IX. Contd Dosage regimen 1000 mg IV 2 h infusion q24h 3 doses Subjects (n) 4 4 4 4 Sampling time (h)a 4 8 12 24 Plasma concentration (mg/mL)b 9.2 2.7 8.1 1.6 4.1 0.8 2.0 0.4 ELF concentration (mg/mL)b 22.8 12.9 10.5 4.3 9.4 3.8 2.8 1.0 ELF/plasma penetration ratiob NR NR NR NR Reference 115
a Sampling time after the last dose or after the start of the last IV infusion, as applicable. b c d Values are expressed as mean SD unless specified otherwise. A total of 35 subjects were studied, but information on how many subjects were assigned to each sampling time was not provided in the study. Values are expressed as range.
e 12 subjects had two bronchoscopies after administration of the final dose (e.g. at 1 h and 12 h or at 1 h and 24 h). f g Samples were collected after 2 d of therapy. Values are expressed as median.
h One of four subjects had concentrations <LLQ. IV = intravenous; LLQ = lower limit of quantification; NA = not applicable; NR = not reported; PO = orally; qxh = every x h; SD = standard deviation.
variability associated with reported ELF to plasma penetration ratios that have been observed in the limited number of intrapulmonary studies. 6. Glycopeptides and Lipoglycopeptides
6.1 Vancomycin
Vancomycin has been used for over 50 years to treat serious Gram-positive infections, including meticllin-resistant S. aureus. A great deal of attention has recently been paid to appropriate dosing of vancomycin, particularly in lower respiratory tract infections.[125,126] However, only a limited number of studies have evaluated ELF concentrations of vancomycin and assessed its plasma and intrapulmonary disposition (table XI).[127-131] Lamer et al.[127] investigated plasma and ELF concentrations of vancomycin in 14 critically ill adult patients (mean SD Acute Physiology and Chronic Health Evaluation II [APACHE II] score 18.7 6) who were mechanically ventilated and had signs and symptoms of lower respiratory tract infection. The patients received an initial dose of intravenous vancomycin 15 mg/kg, and subsequent doses were adjusted to achieve a trough plasma concentration between 15 and 20 mg/mL. Blood and BAL samples were collected at an average of 6.6 days (range 511 days) after starting treatment with a cumulative dose of 9.4 g (range 317.5 g). Concentrations of vancomycin in ELF ranged from 0.4 to 8.1 mg/mL, and a significant linear correlation (r = 0.64; p < 0.02) was observed between plasma and ELF concentrations. Patients with lung inflammation (ELF albumin concentration 3.4 mg/mL; n = 7) had a sig 2011 Adis Data Information BV. All rights reserved.
nificantly higher (p < 0.02) vancomycin ELF to plasma concentration ratio (mean 0.246; range 0.1920.426) than patients without inflammation (mean 0.14; range 0.0230.285) and a normal ELF albumin concentration (<3.4 mg/mL; n = 7). Georges et al.[128] also evaluated vancomycin plasma and ELF concentrations in ten critically ill adult patients (mean SD age 65.5 8.4 years) with meticillin-resistant S. aureus pneumonia requiring mechanical ventilation. Plasma and ELF concentrations of vancomycin were measured 24 hours after starting intravenous vancomycin 7.5 mg/kg every 6 hours, infused over 1 hour. Four of ten patients had measurable concentrations of vancomycin in ELF (range 1.382.77 mg/mL), and the concomitant trough plasma concentrations ranged from 20.9 to 23.2 mg/mL. In the six patients with undetectable concentrations of vancomycin in ELF, the trough plasma concentrations ranged from 7.7 to 18.1 mg/mL. The authors of both studies[127,128] recommended that trough plasma concentrations of vancomycin should be approximately 20 mg/mL to ensure that adequate ELF concentrations are achieved. Plasma and intrapulmonary concentrations of vancomycin in ten healthy adult subjects were measured at 4 and 12 hours after the start of the ninth dose of intravenous vancomycin 1000 mg every 12 hours (table XI).[129] In addition, a population pharmacokinetic analysis and Monte Carlo simulations were conducted.[132] The ratio of ELF to total plasma concentrations was 0.5, based upon AUC values for each matrix. If protein binding of vancomycin in healthy adult subjects is assumed to be approximately 50%, ELF and unbound plasma vancomycin concentrations were essentially of the same magnitude. An in vitro model evaluated the effects of simulated ELF concentrations and penetration ratios on bacterial killing of
Clin Pharmacokinet 2011; 50 (10)
Penetration of Antibacterial Agents into Pulmonary ELF
655
meticillin-resistant S. aureus and development of resistance.[133] Bactericidal activity could not be demonstrated for dosage regimens that achieved an unbound AUC24/MIC ratio of 350 with a penetration ratio of 1.0. Development of resistance was suppressed when the unbound AUC24/MIC ratio was 280 with a penetration ratio of 0.8. These findings suggest that current dosage regimens, which recommend trough plasma vancomycin concentrations of 1520 mg/mL, are not adequate for bactericidal activity, even when the ELF penetration ratio is equal to 1.0. Development of resistance (e.g. heterogeneous) is likely to occur if MIC values are >1 mg/mL, the unbound AUC24/MIC ratio is <280 and/or the ELF penetration ratio is <0.8.
6.2 Teicoplanin
associated pneumonia who received 12 mg/kg twice daily for 2 days followed by 12 mg/kg once daily (table XI).[130] The total and unbound serum concentrations ranged from 8.8 to 29.9 mg/mL and from 2.0 to 5.4 mg/mL, respectively. The concentrations of teicoplanin in ELF ranged from 2.0 to 11.8 mg/mL, and the ratio of ELF to unbound serum concentrations ranged from 0.48 to 3.32 (median 1.46).
6.3 Telavancin
Teicoplanin is another glycopeptide that is commercially available in many countries other than the US. One study compared steady-state serum and ELF concentrations of intravenous teicoplanin in 13 critically ill patients with ventilator-
Telavancin is a lipoglycopeptide developed for the treatment of serious Gram-positive infections, including meticillinresistant S. aureus. Steady-state plasma and intrapulmonary concentrations of telavancin were evaluated in 20 healthy adult subjects who were administrated 10 mg/kg intravenously once daily for 3 days (table XI).[131] The mean concentrations of telavancin in ELF at 8 and 24 hours after the last dose were 3.73 and 0.89 mg/mL, respectively. The mean plasma concentrations at 12 and 24 hours were 22.9 and 7.28 mg/mL, respectively.
Table X. Plasma and epithelial lining fluid (ELF) concentrations of aminoglycosides Antibacterial agent Gentamicin Dosage regimen 240 mg IV 30 min infusion 1 dose Subjects (n) 6 6 6 6 Tobramycin 150 mg IM 1 or more doses 300 mg IM 1 or more doses IV doses adjusted to achieve serum Cmax ~8 mg/mL and Cmin <2 mg/mL while maintaining q8h dosing intervald 710 mg/kg IV 30 min infusion q24he 300 mg inhalation 1 dose Netilmicin 450 mg IV 30 min infusion 1 dose 5 5 4 4 4 4 12 12 5 5 5 5 Sampling time (h)a 1 2 4 6 6 6 0.5e 2e 4e 8 1 NA 1 1.5 2 3
e
Plasma concentration (mg/mL)b 8.79 0.64c 6.37 0.50
c
ELF concentration (mg/mL)b 2.95 0.37c 4.24 0.42
c
ELF/plasma penetration ratiob 0.30 0.05c 0.85 0.10c 1.14 0.26c 0.74 0.18c 1.4 0.8 1.6 0.6 0.30 0.03 0.42 0.16 0.64 0.37 1.53 0.76 0.119 0.019 NA NR NR NR NR
Reference 119
4.70 0.49c 4.70 0.57 4.1 1.5 4.3 2.4 6.90 1.44 4.08 1.30 2.14 0.85 0.79 0.38 22.4 5.9 NA 21.4 1.19c 15.3 0.85
c c c
3.10 0.39c 2.65 0.35 5.3 2.9 5.5 2.1 2.33 0.50 1.67 0.60 1.62 1.19 0.77 0.38 2.7 0.7 90 54 7.5 1.0c 9.6 0.3
c c
120 120 121
122 123 124
12.0 0.71c 8.3 0.64
14.7 2.2c 9.3 0.6
c
a Sampling time after the last dose or after the start of the last IV infusion, as applicable. b Values are expressed as mean SD unless specified otherwise. c Values are expressed as mean SEM. d The mean number of doses ( SD) administered before BAL fluid collection was 21.25 6.42. e Samples were collected at steady state after 2 d of therapy. BAL = bronchoalveolar lavage; Cmax = maximum concentration; Cmin = minimum concentration; IM = intramuscularly; IV = intravenous; NA = not applicable; NR = not reported; qxh = every x h; SD = standard deviation; SEM = standard error of the mean.
2011 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2011; 50 (10)
656
Rodvold et al.
Table XI. Plasma and epithelial lining fluid (ELF) concentrations of glycopeptides and lipoglycopeptides Antibacterial agent Vancomycin Dosage regimen 15 mg/kg IV 2 h infusion 5 for 11 dc,d 7.5 mg/kg IV 1 h infusion q6hf Subjects (n) 14 4 6 1000 mg IV 1 h infusion q12h 9 doses Teicoplanin 12 mg/kg IV 30 min infusion q12h 2 d, then 12 mg/kg IV 30 min infusion q24h 10 mg/kg IV 1 h infusion q24h 3 doses 5 5 13 Sampling time (h)a 18.4 11 6f 6f 4 12 1824h,i Plasma concentration (mg/mL)b 24 19 22.19 0.83 12.45 3.56 19.8 3.7 5.1 1.7 15.9 ELF concentration (mg/mL)b 4.5 2.3e 2.03 0.49 NDg 5.3 1.5 2.4 0.7 4.9 ELF/plasma penetration ratiob 0.18 NR NR NR NR 1.46j 130 129 Reference 127 128
Telavancin
5 5 5 5
4 8 12 24 4 12 24 168
NR NR 22.9 7.28 119.6 24.6 75.7 16.3 73.7 28.2 10.4 3.0
NR 3.73 1.28 NR 0.89 1.03 3.1 1.1 3.7 2.5 6.3 1.5 1.7 0.8
NR NR NR NR NR NR NR NR
131
Oritavancin
800 mg IV 12 h infusion q24h 5 doses
5 5 5 5
129
a Sampling time after the last dose unless specified otherwise. b c d Values are expressed as mean SD. Subsequent doses were adjusted in order to obtain a trough plasma concentration of 1520 mg/mL. The mean ( SD) duration of therapy was 6.6 1.75 d.
e No drug was detected in BAL fluid from one patient, therefore, the LLQ (10 ng/mL) was used in the analysis. f Sampling was performed 24 h after the start of vancomycin therapy.
g Concentrations in BAL fluid were undetectable (assay LLQ 0.5 mg/mL). h Samples were collected 4 to 6 d after the start of teicoplanin therapy. i j Values are expressed as range. The ratio represents the ELF to unbound serum concentration (median unbound fraction 22% [range 842%]).
BAL = bronchoalveolar lavage; IV = intravenous; LLQ = lower limit of quantification; ND = not detected; NR = not reported; qxh = every x h; SD = standard deviation.
The plasma protein binding of telavancin is approximately 90%. A subsequent population pharmacokinetic analysis and Monte Carlo simulation study reported mean and median values for the ratio between the ELF AUC and the unbound plasma AUC of 1.01 and 0.73, respectively.[134] The large variability (SD 0.96) of the ELF AUC from time zero to infinity (AUCp) skewed the mean value towards 1.
6.4 Oritavancin
lected in 20 healthy adult subjects for up to 168 hours after the fifth intravenous dose of 800 mg every 24 hours.[127] The mean concentrations of oritavancin in ELF (range 3.1 mg/mL at 4 hours to 1.7 mg/mL at 168 hours) were lower than the total plasma concentrations (range 119.610.4 mg/mL) [table XI]. If protein binding for oritavancin in healthy adult subjects is assumed to be approximately 90%, the ELF and unbound plasma oritavancin concentrations were similar. 7. Miscellaneous Antibacterial Agents Several studies have reported intrapulmonary concentrations of agents from other antibacterial classes (table XII).[135-139] Currently, linezolid and tigecycline are available for clinical
Clin Pharmacokinet 2011; 50 (10)
Oritavancin is an investigational lipoglycopeptide being developed for the treatment of serious Gram-positive infections, including meticillin-resistant S. aureus. Plasma and bronchopulmonary concentrations of oritavancin were col 2011 Adis Data Information BV. All rights reserved.
Penetration of Antibacterial Agents into Pulmonary ELF
657
use and have been approved for the treatment of lower respiratory tract infections. Iclaprim is an investigational agent that is undergoing clinical development.
7.1 Linezolid
Linezolid is an oral and parenteral antibacterial agent that is representative of the oxazolidinone class. Linezolid is used in the treatment of serious lower respiratory tract infections caused by Gram-positive pathogens such as meticillin-resistant S. aureus. The intrapulmonary disposition of linezolid has been investigated in healthy adult subjects, patients with chronic obstructive pulmonary disease and critically ill patients requiring mechanical ventilation. Plasma and bronchopulmonary concentrations of linezolid were measured in 25 healthy adult subjects for up to 48 hours after the fifth oral dose of 600 mg every 12 hours.[135] The mean concentrations and systemic exposure of linezolid in ELF (range 64.3 mg/mL at 4 hours to 0.7 mg/mL at 48 hours; AUC24 672 mg h/mL) exceeded those in plasma (range 15.50.2 mg/mL; AUC24 204.2 mg h/mL) and in AMs (range 2.2 mg/mL to below
the LLQ; AUC24 30.0 mg h/mL) [table XII]. For ELF, the AUC24/MIC ratio was 168 and the T>MIC was 100% for a 12-hour dosing interval at an MIC required to inhibit the growth of 90% of organisms (MIC90) of 4 mg/mL for S. aureus. Plasma and intrapulmonary concentrations of linezolid were measured between 2.9 and 7.5 hours following the sixth oral dose of 600 mg every 12 hours in ten subjects undergoing diagnostic bronchoscopy and BAL.[136] Concentrations of linezolid in ELF were detectable in nine subjects and ranged from 13.1 to 52.4 mg/mL (table XII). The concomitant plasma and AM concentrations ranged from 8.6 to 19.6 mg/mL and from 0.5 to 23.7 mg/mL, respectively. The mean SD ELF to plasma concentration ratio was 8.35 11.69 and quite variable over the ten sampling times. Plasma and ELF concentrations of linezolid were determined at steady state in 16 critically ill adult patients with ventilator-associated pneumonia.[137] Following 2 days of intravenous therapy with linezolid 600 mg every 12 hours, bronchoalveolar microlavage (with 40 mL of sterile 0.9% normal saline solution) was performed twice in each subject at 1 and 12 hours after the start of the last dose. Concentrations of
Table XII. Plasma and epithelial lining fluid (ELF) concentrations of linezolid, tigecycline and iclaprim Antibacterial agent Linezolid Dosage regimen 600 mg PO bid 5 doses Subjects (n) 5 5 5 5 5 600 mg PO bid 6 doses 600 mg IV 1 h infusion 2 d 10 16 16 Tigecycline 100 mg IV 30 min infusion 1 dose, then 50 mg IV 30 min infusion q12h 7 doses 5 5 5 5 5 5 Iclaprim 1.6 mg/kg IV 1 h infusion 1 dose 8 8 8 Sampling time (h)a 4 8 12 24 48 5.10 2.01 2c 12 2c 3
c c b
Plasma concentration (mg/mL)b 15.5 4.9 8.9 3.2 10.2 2.3 1.8 0.6 0.2 0.2 13.40 3.92 17.7 4.0 2.4 1.2 0.19 0.06 0.15 0.05 0.16 0.07 0.12 0.06
ELF concentration (mg/mL)b 64.3 33.1 31.4 33.0 24.3 13.3 7.6 6.0 0.7 0.8 25.09 14.59 14.4 5.6 2.6 1.7 0.19 0.15 0.12 0.21 0.06 0.13 0.37 0.36 0.10 0.17 0.00 0.00 12.61 7.33 6.38 5.17 2.66 2.08
ELF/plasma penetration ratiob 4.2 1.4 3.1 2.2 2.4 1.2 3.9 2.3 2.3 1.6 8.35 11.69 1.05 0.34 1.04 0.28 NR NR NR NR NR NR 21.29 11.18 24.93 16.53 20.57 17.31
Reference 135
136 137
138
4c 6
c c
12
0.10 0.09 0.05 0.01
b,c
24c 1.97 0.08 3.57 0.30b,c 6.50 0.29b,c
0.59 0.18 0.24 0.05 0.14 0.05
139
a Sampling time after the last dose unless specified otherwise. b Values are expressed as mean SD. c Sampling time after the start of the last IV infusion. bid = twice daily; IV = intravenous; NR = not reported; PO = orally; q12h = every 12 h; SD = standard deviation.
2011 Adis Data Information BV. All rights reserved. Clin Pharmacokinet 2011; 50 (10)
658
Rodvold et al.
linezolid in ELF ranged from 4.5 to 25.4 mg/mL (mean 14.4 mg/mL) at 1 hour and from 0.3 to 5.8 mg/mL (mean 2.6 mg/mL) at 12 hours (table XII). The ELF to plasma concentration ratio was approximately 1 at both sampling times, and the mean AUC24 in plasma was 154.6 mg h/mL.
7.2 Tigecycline
Tigecycline is a parenteral glycylcycline and belongs to the tetracycline class of anti-infective agents. Tigecycline has shown activity against a wide spectrum of pathogens, including Grampositive, Gram-negative, atypical and anaerobic pathogens. Steady-state plasma and intrapulmonary concentrations of tigecycline were measured in 30 healthy adult subjects following the last dose of an intravenous regimen, which included a loading dose of 100 mg followed by 50 mg every 12 hours for a total of seven doses.[138] The mean concentrations of tigecycline in serum and ELF were similar during the entire 12-hour dosing interval and ranged from 0.10 to 0.19 mg/mL and from 0.06 to 0.37 mg/mL, respectively (table XII). In contrast, the mean concentrations in AMs were significantly higher (p < 0.05) and ranged from 10.7 to 15.2 mg/mL. A population pharmacokinetic analysis and Monte Carlo simulations were subsequently conducted to determine systemic exposure (based on AUC24 values) and penetration ratios.[140] The median ELF to serum concentration ratio was 1.15 and was associated with wide variability (5th and 95th percentiles 0.561 and 5.23, respectively). It is worth noting that the protein binding of tigecycline in humans ranges from 71% to 89%, and the data reported above used total serum concentrations from uninfected subjects. Two recent studies in animal models have suggested that (i) a significantly higher penetration ratio is seen when protein binding is accounted for and unbound serum concentrations are used; (ii) ELF to unbound serum concentration ratios are significantly higher in mice with a pulmonary infection (12.9 and 23.3 at doses of 25 and 50 mg/kg, respectively) than in those without a pulmonary infection (6.2 and 8.1 at doses of 25 and 50 mg/kg, respectively); and (iii) the penetration ratio is dose dependent and tends to increase with larger doses.[141,142] Further studies are needed to confirm these observations in patients with lower respiratory tract infections.
7.3 Iclaprim
thogens, including meticillin-resistant S. aureus and Streptococcus species. Plasma and intrapulmonary concentrations of iclaprim were measured in 24 healthy male subjects from 1.8 to 7.08 hours after the start of a 1-hour intravenous infusion of 1.6 mg/kg of bodyweight.[139] The concentrations of iclaprim in ELF (range 0.525.3 mg/mL) exceeded the concomitant plasma concentrations at all sampling times with the ratios of ELF to total plasma concentrations ranging from 6 to 51.2 (table XII). The MIC90 values for Gram-positive pathogens such as penicillinsusceptible and -intermediate S. pneumoniae (0.06 and 2 mg/mL, respectively) and meticillin-resistant S. aureus (0.12 mg/mL) were exceeded by the concentrations of iclaprim in ELF for up to 7 hours. The concentrations of iclaprim in AMs were similar to or higher than those in ELF. 8. Conclusions The penetration of antibacterial agents into the ELF of the lung has been extensively evaluated during the past 20 years. This review includes more than 80 studies that have reported ELF concentrations and extracellular penetration ratios of antibacterial agents that are used to treat lower respiratory tract infections. More studies (e.g. >100) would have been included in the review if we had elected to include all reports on fluoroquinolones instead of just those on ciprofloxacin, moxifloxacin and levofloxacin.[25,62,63,86-102,111-115] In spite of this, fluoroquinolones still accounted for approximately 25% of the studies that we reviewed. A wide variety of penetration ratios and patterns of ELF disposition have been observed for agents from various antibacterial classes. Aminoglycosides, b-lactams and glycopeptides tend to have ELF to total plasma concentration ratios of 1. Aminoglycosides tend to have ELF concentrations that are fairly constant and significantly lower than plasma concentrations in the first few hours after drug administration, with subsequent ELF concentrations being similar to or slightly lower than plasma concentrations during the last half of the dosing interval. A wide range of penetration ratios has been reported for b-lactam agents. Even when protein binding and differences in the characteristics of the molecule are taken into account, the discordance in penetration could not be predicted for various agents from the b-lactam classes. Although the number of studies of glycopeptide or lipoglycopeptide agents (e.g. vancomycin, telavancin, oritavancin) is limited, once protein binding is accounted for, the pattern of disposition and the ratios of ELF to unbound plasma concentrations are similar and approach values closer to 1.
Clin Pharmacokinet 2011; 50 (10)
Iclaprim is a dihydrofolate reductase inhibitor and a member of the diaminopyrimidine class of anti-infective agents. Iclaprim has potent in vitro activity against Gram-positive pa 2011 Adis Data Information BV. All rights reserved.
Penetration of Antibacterial Agents into Pulmonary ELF
659
In comparison, antibacterial agents such as macrolides, ketolides, fluoroquinolones (e.g. levofloxacin and moxifloxacin) and linezolid have ELF to total plasma concentration ratios of >1. Why agents from these antibacterial classes tend to have higher concentrations in ELF than in plasma remains unknown. Recent studies have suggested that active transporter systems in epithelial cells may be involved and may influence the secretion of these agents in the lung.[103,143-145] On the other hand, technical issues associated with the collection of BAL samples and measurement of ELF concentrations have been raised as other potential explanations for these observations.[12,13,15] Some authors have provided rationales as to why these confounding variables may not explain the higher observed ELF concentrations. Obviously, more research is needed to understand the underlying mechanisms of drug transporters in the lung, and strict adherence to sample collection procedures is required in order to minimize known sources of error. The majority of studies have been conducted in adults who were healthy or outpatients undergoing an elective diagnostic fibre-optic bronchoscopy. The BAL procedure has usually consisted of 150200 mL of 0.9% normal saline solution being instilled as three or four aliquots. A few recent studies have targeted older outpatients or patients with a clinical diagnosis of mild to moderate chronic bronchitis, chronic obstructive pulmonary disease or lower respiratory tract infection.[53,54,62,69,112,115] The reported ELF concentrations were similar to or slightly higher than those observed in healthy subjects. An increasing number of studies have provided ELF data in critically ill patients who were in an intensive care unit, receiving mechanical ventilation and being treated for severe pneumonia.[36,39,40,49,113,118,119,121,122,124,126-128,130,137] In these patients, microlavage or minilavage (e.g. 20 mL of 0.9% normal saline solution instilled as one or two aliquots per sampling time) has commonly been used for the BAL procedure.[18] Despite differences in study procedures and patient populations, the data on the antibacterial agents that have been studied so far (e.g. piperacillin/tazobactam, ceftazidime, cefepime, meropenem, levofloxacin, aminoglycosides, vancomycin, teicoplanin, linezolid) have shown that ELF concentrations were similar to those observed in healthy subjects and outpatients. Thus antibacterial concentrations in ELF from noninfected subjects tend to serve as conservative estimates of the likely drug concentrations at extracellular sites of lung infection. However, further studies are still warranted in patients with pulmonary infections to explore the importance of intrapulmonary concentrations with respect to establishing relationships between pharmacokinetic-pharmacodynamic parameters and clinical or microbiological outcomes.
2011 Adis Data Information BV. All rights reserved.
The interpretation of antibacterial concentrations in ELF is greatly influenced by the study design, sample collection and timing, analytical methods and data analysis. Our review of the literature and our work as investigators in these types of studies have provided us with an appreciation of the following key issues that need to be considered when reviewing and/or designing intrapulmonary penetration studies: (i) multiple-dose studies are more likely to provide meaningful information and measurable ELF concentrations; (ii) serial sampling times should be spaced throughout a dosing interval in order to provide accurate estimates of AUCs in plasma and in ELF; (iii) procedures for collection, handling and storage of BAL samples are required, including careful separation of ELF and cell components; (iv) studies should involve experienced personnel using established bronchoscopy and BAL procedures that are individualized to the type of subjects being studied; (v) analytical methodologies must be sensitive and specific for measurement of urea and drug concentrations in plasma and in ELF; and (vi) pharmacokinetic-pharmacodynamic data analysis and mathematical modelling should take into account protein binding, systemic exposure, simulations of drug concentration profiles and evaluation of target attainment rates. Ideally, a logical approach for evaluating dosage regimens based on preclinical infection models, the pharmacokineticpharmacodynamic characteristics of the agent being studied and drug exposure information at the site of infection (e.g. ELF in the lung) should be incorporated into the study design.[41] All of these considerations are important to the understanding of ELF penetration and appropriate decision-making to guide dosage regimen designs for patients with lower respiratory tract infections.[7] This review has focused on human studies that have measured ELF concentrations of antibacterial agents. An increasing number of intrapulmonary penetration studies have been conducted in animals. Antibacterial agents that have and have not been studied in humans have been evaluated for applications in veterinary medicine for foals, horses and dogs.[146-155] In addition, animal studies evaluating different modes of administration or formulations of current and investigational antibacterial agents have been reported.[156-160] These studies are also providing further insights into the penetration of antibacterial agents into ELF.
Acknowledgements
No sources of funding were used in the preparation of this review. The authors have no conflicts of interest that are directly relevant to the content of this review.
Clin Pharmacokinet 2011; 50 (10)
660
Rodvold et al.
References
1. Siegel RE. The significance of serum versus tissue concentrations of antibiotics in the treatment of penicillin-resistant Streptococcus pneumoniae and community-acquired pneumonia: are we looking in the wrong place? Chest 1999; 116: 535-8 2. Craig WA. Pharmacokinetic-pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 1998; 26: 1-10 3. Rodvold KA. Pharmacodynamics of antiinfective therapy: taking what we know to the patients bedside. Pharmacotherapy 2001; 11 (Pt 2): 319S-330S 4. Ambrose PG, Bhavnani SM, Rubino CM, et al. Pharmacokineticspharmacodynamics of antimicrobial therapy: its not just for mice anymore. Clin Infect Dis 2007; 44: 78-86 5. Muller ML, dela Pen a A, Derendorf H. Issues in pharmacokinetics and pharmacodynamics of anti-infective agents: distribution in tissue. Antimicrob Agents Chemother 2004; 48: 1441-53 6. Drusano GL. Infection site concentrations: their therapeutic importance and the macrolide and macrolide-like class of antibiotics. Pharmacotherapy 2005; 25 (Pt 2): 150S-158S 7. Ambrose PG, Bhavnani SM, Ellis-Grosse EJ, et al. Pharmacokineticpharmacodynamic considerations in the design of hospital-acquired or ventilator-associated bacterial pneumonia studies: look before you leap! Clin Infect Dis 2010; 51 Suppl. 1: S103-10 8. Honeybourne D. Antibiotic penetration in the respiratory tract and implications for the selection of antimicrobial therapy. Curr Opin Pulm Med 1997; 3: 170-4 9. Nix DE. Intrapulmonary concentrations of antimicrobial agents. Infect Dis Clin North Am 1998; 12: 631-46 10. Fish DN. Bronchoscopic sampling of drug concentrations: penetration to tissue is the issue. Am J Respir Crit Care Med 2003; 168: 1263-5 11. Baldwin DR, Honeybourne D, Wise R. Pulmonary disposition of antimicrobial agents: in vivo observations and clinical relevance. Antimicrob Agents Chemother 1992; 36: 1176-80 12. Dhanani J, Roberts JA, Chew M, et al. Antimicrobial chemotherapy and lung microdialysis: a review. Int J Antimicrob Agents 2010; 36: 491-500 13. Zeitlinger M, Muller M, Joukhadar C. Lung microdialysis: a powerful tool for the determination of exogenous and endogenous compounds in the lower respiratory tract (mini-review). AAPS J 2005; 7: E600-8 14. Mouton JW, Theuretzbacher U, Craig WA, et al. Tissue concentrations: do we ever learn? J Antimicrob Chemother 2008; 61: 235-7 15. Kiem S, Schentag JJ. Interpretation of antibiotic concentration ratios measured in epithelial lining fluid. Antimicrob Agents Chemother 2008; 52: 24-36 16. Baldwin DR, Honeybourne D, Wise R. Pulmonary disposition of antimicrobial agents: methodological considerations. Antimicrob Agents Chemother 1992; 36: 1171-5 17. Rennard SI, Basset G, Lecossier D, et al. Estimation of volume of epithelial lining fluid recovered by lavage using urea as marker of dilution. J Appl Physiol 1986; 60: 532-8 18. Mimoz O, Dahyot-Fizelier C. Mini-broncho-alveolar lavage: a simple and promising method for assessment of antibiotic concentration in epithelial lining fluid. Intensive Care Med 2007; 33: 1495-7 19. Burke WMJ, Roberts CM, Bryant DH, et al. Smoking-induced changes in epithelial lining fluid volume, cell density and protein. Eur Respir J 1992; 5: 780-4 20. Roberts CM, Cairns D, Bryant DH, et al. Changes in epithelial lining fluid albumin associated with smoking and interstitial lung disease. Eur Respir J 1993; 6: 110-5 21. Hasegawa N, Nishimura T, Watabnabe M, et al. Concentrations of clarithromycin and active metabolite in the epithelial lining fluid of patients with Mycobacterium avium complex pulmonary disease. Pulm Pharmacol Ther 2009; 22: 190-3 22. Kikuchi E, Kikuchi J, Nasuhara Y, et al. Comparison of the pharmacodynamics of biapenem in bronchial epithelial lining fluid in healthy volun 2011 Adis Data Information BV. All rights reserved.
teers given half-hour and three-hour intravenous infusions. Antimicrob Agents Chemother 2009; 53: 2799-803 23. Kikuchi E, Yamazaki K, Kikuchi J, et al. Pharmacokinetics of clarithromycin in bronchial epithelial lining fluid. Respirology 2008; 13: 221-6 24. Kikuchi J, Yamazaki K, Kikuchi E, et al. Pharmacokinetics of telithromycin using bronchoscopic microsampling after single and multiple oral doses. Pulm Pharmacol Ther 2007; 20: 549-55 25. Yamazaki K, Ogura S, Ishizaka A, et al. Bronchoscopic microsampling method for measuring drug concentration in epithelial lining fluid. Am J Respir Crit Care Med 2003; 168: 1304-7 26. Bamberger DM, Foxworth JW, Bridwell DL, et al. Extravascular antimicrobial distribution and the respective blood and urine concentrations in humans. In: Lorain V, editor. Antibiotics in laboratory medicine. 5th ed. Philadelphia (PA): Lippincott Williams & Wilkins, 2005: 719-809 27. Chu H-M, Ette EI. Analysis of quantic pharmacokinetic study: robust estimation of tissue-to-plasma ratio. In: Ette EI, Williams PJ, editors. Pharmacometrics: the science of quantitative pharmacology. Hoboken (NJ): John Wiley & Sons, Inc., 2007: 1035-68 28. Cook PJ, Andrews JM, Woodcock J, et al. Concentration of amoxycillin and clavulanate in lung compartments in adults without pulmonary infection. Thorax 1994; 49: 1134-8 29. Baldwin DR, Andrews JM, Wise R, et al. Bronchoalveolar distribution of cefuroxime axetil and in-vitro efficacy of observed concentrations against respiratory pathogens. J Antimicrob Chemother 1992; 30: 377-85 30. Conte Jr JE, Golden J, Duncan S, et al. Single-dose intrapulmonary pharmacokinetics of azithromycin, clarithromycin, ciprofloxacin, and cefuroxime in volunteer subjects. Antimicrob Agents Chemother 1996; 40: 1617-22 31. Muller-Serieys C, Bancal C, Dombret MC, et al. Penetration of cefpodoxime proxetil in lung parenchyma and epithelial lining fluid of noninfected patients. Antimicrob Agents Chemother 1992; 36: 2099-103 32. Andrews JM, Wise R, Baldwin DR, et al. Concentrations of ceftibuten in plasma and the respiratory tract following a single 400 mg oral dose. Int J Antimicrob Agents 1995; 5: 141-4 33. Cook PJ, Andrews JM, Wise R, et al. Distribution of cefdinir, a third generation cephalosporin antibiotic, in serum and pulmonary compartment. J Antimicrob Chemother 1996; 37: 331-9 34. Mazzei T, Novelli A, Esposito S, et al. New insight into the clinical pharmacokinetics of cefaclor: tissue penetration. J Chemother 2000; 12: 53-62 35. Lodise TP, Kinzig-Schippers M, Drusano GL, et al. Use of population pharmacokinetic modeling and Monte Carlo simulation to describe the pharmacodynamic profile of cefditoren in plasma and epithelial lining fluid. Antimicrob Agents Chemother 2008; 52: 1945-51 36. Boselli E, Breilh D, Cannesson M, et al. Steady-state plasma and intrapulmonary concentrations of piperacillin/tazobactam 4 g/0.5 g administered to critically ill patients with severe nosocomial pneumonia. Intensive Care Med 2004; 30: 976-9 37. Baldwin DR, Maxwell SRJ, Honeybourne D, et al. The penetration of cefpirome into the potential sites of pulmonary infection. J Antimicrob Chemother 1991; 28: 79-86 38. Cazzola M, Matera MG, Polverino M, et al. Pulmonary penetration of ceftazidime. J Chemother 1995; 7: 50-4 39. Boselli E, Breilh D, Rimmele T, et al. Plasma and lung concentrations of ceftazidime administered in continuous infusion to critically ill patients with severe nosocomial pneumonia. Intensive Care Med 2004; 30: 989-91 40. Boselli E, Breilh D, Duflo F, et al. Steady-state plasma and intrapulmonary concentrations of cefepime administered in continuous infusion in critically ill patients with severe nosocomial pneumonia. Crit Care Med 2003; 31: 2102-6 41. Rodvold KA, Nicolau DP, Lodise TP, et al. Identifying exposure target for treatment of staphylococcal pneumonia with ceftopibrole. Antimicrob Agents Chemother 2009; 53: 3294-301
Clin Pharmacokinet 2011; 50 (10)
Penetration of Antibacterial Agents into Pulmonary ELF
661
42. Krumpe P, Lin C-C, Radwanski E, et al. The penetration of ceftibuten into the respiratory tract. Chest 1999; 116: 369-74 43. Bayat S, Louchahi K, Verdiere B, et al. Comparison of 99mTc-DTPA and urea for measuring cefepime concentrations in epithelial lining fluid. Eur Respir J 2004; 24: 150-6 44. Laohavaleeson S, Tessier PR, Nicolau DP. Pharmacodynamic characterization of ceftobiprole in experimental pneumonia caused by phenotypically diverse Staphylococcus aureus strains. Antimicrob Agents Chemother 2008; 52: 2389-94 45. Allegranzi B, Cazzadori A, Di Perri G, et al. Concentrations of single-dose meropenem (1 g iv) in bronchoalveolar lavage and epithelial lining fluid. J Antimicrob Chemother 2000; 46: 319-22 46. Conte Jr JE, Golden JA, Kelley MG, et al. Intrapulmonary pharmacokinetics and pharmacodynamics of meropenem. Int J Antimicrob Agents 2005; 26: 449-56 47. Burkhardt O, Majcher-Peszynska J, Borner K, et al. Penetration of ertapenem into different pulmonary compartments of patients undergoing lung surgery. J Clin Pharmacol 2005; 45: 659-65 48. Boselli E, Breilh D, Saux M-C, et al. Pharmacokinetics and lung concentrations of ertapenem in patients with ventilator-associated pneumonia. Intensive Care Med 2006; 32: 2059-62 49. Drusano GL, Sorgel F, Ma L, et al. Pharmacokinetics and penetration of meropenem into epithelial lining fluid in patients with ventilatorassociated pneumonia [abstract no. A-222]. 45th Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC); 2005 Dec 16-19; Washington, DC 50. Lodise TP, Sorgel F, Melnick D, et al. Penetration of meropenem into epithelial lining fluid of patients with ventilator-associated pneumonia. Antimicrob Agents Chemother 2011; 55: 1606-10 51. Conte Jr JE, Golden JA, Duncan S, et al. Intrapulmonary pharmacokinetics of clarithromycin and erythromycin. Antimicrob Agents Chemother 1995; 39: 334-8 52. Chastre J, Brun P, Fourtillan JB, et al. Pulmonary disposition of roxithromycin (RU 28965), a new macrolide antibiotic. Antimicrob Agents Chemother 1987; 31: 1312-6 53. Nakamura H, Fujishima S, Inoue T, et al. Clinical and immunoregulatory effects of roxithromycin therapy for chronic respiratory tract infection. Eur Resp J 1999; 13: 1371-9 54. Cazzola M, Matera MG, Tufano MA, et al. Pulmonary penetration of dirithromycin in patients suffering from acute exacerbations of chronic bronchitis. Pul Pharmacol 1994; 7: 377-81 55. Furuie H, Saisho Y, Yoshikawa T, et al. Intrapulmonary pharmacokinetics of S-013420, a novel bicyclolide antibacterial, in healthy Japanese subjects. Antimicrob Agents Chemother 2010; 54: 866-70 56. Honeybourne D, Kees F, Andrews JM, et al. The levels of clarithromycin and its 14-hydroxy metabolite in the lung. Eur Respir J 1994; 7: 1275-80 57. Patel KB, Xuan D, Tessier PR, et al. Comparison of bronchopulmonary pharmacokinetics of clarithromycin and azithromycin. Antimicrob Agents Chemother 1996; 40: 2375-9 58. Rodvold KA, Gotfried MH, Danziger LH, et al. Intrapulmonary steady-state concentrations of clarithromycin and azithromycin in healthy adult volunteers. Antimicrob Agents Chemother 1997; 41: 1399-402 59. Gotfried MH, Danziger LH, Rodvold KA. Steady-state plasma and bronchopulmonary characteristics of clarithromycin extended-release tablets in normal healthy adult subjects. J Antimicrob Chemother 2003; 52: 450-6 60. Baldwin DR, Wise R, Andrews JM, et al. Azithromycin concentrations at the sites of pulmonary infection. Eur Resp J 1990; 3: 886-90 61. Olsen KM, San Pedro GS, Gann LP, et al. Intrapulmonary pharmacokinetics of azithromycin in healthy volunteers given five oral doses. Antimicrob Agents Chemother 1996; 40: 2582-5
2011 Adis Data Information BV. All rights reserved.
62. Capitano B, Mattoes HM, Shore E, et al. Steady-state intrapulmonary concentrations of moxifloxacin, levofloxacin, and azithromycin in older adults. Chest 2004; 125: 965-73 63. Rodvold KA, Danziger LH, Gotfried MH. Steady-state plasma and bronchopulmonary concentrations of intravenous levofloxacin and azithromycin in healthy adults. Antimicrob Agents Chemother 2003; 47: 2450-7 64. Kadota J-I, Ishimatsu Y, Iwashita T, et al. Intrapulmonary pharmacokinetics of telithromycin, a new ketolide, in healthy Japanese volunteers. Antimicrob Agents Chemother 2002; 46: 917-21 65. Khair OA, Andrews JM, Honeybourne D, et al. Lung concentrations of telithromycin after oral dosing. J Antimicrob Chemother 2001; 47: 837-40 66. Ong CT, Dandekar PK, Sutherland C, et al. Intrapulmonary concentrations of telithromycin: clinical implications for respiratory tract infections due to Streptococcus pneumonia. Chemotherapy 2005; 51: 339-46 67. Muller-Serieys C, Soler P, Cantalloube C, et al. Bronchopulmonary disposition of the ketolide telithromycin (HMR 3647). Antimicrob Agents Chemother 2001; 45: 3104-8 68. Conte Jr JE, Golden JA, Kipps J, et al. Steady-state plasma and intrapulmonary pharmacokinetics and pharmacodynamics of cethromycin. Antimicrob Agents Chemother 2004; 48: 3508-15 69. Matera MG, Tufano MA, Polverino M, et al. Pulmonary concentrations of dirithromycin and erythromycin during acute exacerbation of mild chronic obstructive pulmonary disease. Eur Resp J 1997; 10: 98-103 70. Bergman KL, Olsen KM, Peddicord TE, et al. Antimicrobial activities and postantibiotic effects of clarithromycin, 14-hydroxy-clarithromycin, and azithromycin in epithelial cell lining fluid against clinical isolates of Haemophilus influenzae and Streptococcus pneumoniae. Antimicrob Agents Chemother 1999; 43: 1291-3 71. Noreddin AM, Roberts D, Nichol K, et al. Pharmacodynamic modeling of clarithromycin against macrolide-resistant [PCR-positive mef(A) or erm(B)] Streptococcus pneumoniae simulating clinically achievable serum and epithelial lining fluid free-drug concentrations. Antimicrob Agents Chemother 2002; 46: 4029-34 72. Maglio D, Capitano B, Banevicius MA, et al. Differential efficacy of clarithromycin in lung versus thigh infection models. Chemotherapy 2004; 50: 63-6 73. Noreddin AM, El-Khatib WF, Aolie J, et al. Pharmacodynamic target attainment potential of azithromycin, clarithromycin, and telithromycin in serum and epithelial lining fluid of community-acquired pneumonia patients with penicillin-susceptible, intermediate, and resistant Streptococcus pneumoniae. Int J Antimicrob Agents 2009; 13: 483-7 74. Kays MB, Denys GA. In vitro activity and pharmacodynamics of azithromycin and clarithromycin against Streptococcus pneumoniae based on serum and intrapulmonary pharmacokinetics. Clin Ther 2001; 23: 413-24 75. Ambrose PG. Antimicrobial susceptibility breakpoints: PK-PD and susceptibility breakpoints. Treat Respir Med 2005; 4 Suppl. 1: 5-11 76. Lucchi M, Damle B, Fang A, et al. Pharmacokinetics of azithromycin in serum, bronchial washings, alveolar macrophages and lung tissue following a single oral dose of extended or immediate release formulations of azithromycin. J Antimicrob Chemother 2008; 61: 884-91 77. Alou L, Gimenez M-J, Sevillano D, et al. A pharmacodynamic approach to antimicrobial activity in serum and epithelial lining fluid against in vivoselected Streptococcus pneumoniae mutants and association with clinical failure in pneumonia. J Antimicrob Chemother 2006; 58: 349-58 78. Sevillano D, Alou L, Aguilar L, et al. Azithromycin IV pharmacodynamic parameters predicting Streptococcus pneumoniae killing in epithelial lining fluid versus serum: an in vitro pharmacodynamic simulation. J Antimicrob Chemother 2006; 57: 1128-33 79. Cafini F, Alou L, Sevillano D, et al. Bactericidal activity of moxifloxacin against multidrug-resistant Streptococcus pneumoniae at clinically achievable serum and epithelial lining fluid concentrations compared with three other antimicrobials. Int J Antimicrob Agents 2004; 24: 334-8
Clin Pharmacokinet 2011; 50 (10)
662
Rodvold et al.
80. Zhanel GG, DeCorby M, Noreddin A, et al. Pharmacodynamic activity of azithromycin against macrolide-susceptible and -resistant Streptococcus pneumoniae simulating clinically achievable free serum, epithelial lining fluid and middle ear fluid concentrations. J Antimicrob Chemother 2003; 52: 83-8 81. Lodise TP, Preston S, Bhargava V, et al. Pharmacodynamics of an 800-mg dose of telithromycin in patients with community-acquired pneumonia caused by extracellular pathogens. Diagn Microbiol Infect Dis 2005; 52: 45-52 82. Zhanel GG, Johanson C, Laing N, et al. Pharmacodynamic activity of telithromycin at simulated clinically achievable free-drug concentrations in serum and epithelial lining fluid against efflux (mefE)-producing macrolideresistant Streptococcus pneumoniae for which telithromycin MICs vary. Antimicrob Agents Chemother 2005; 49: 1943-8 83. Zhanel GG, Johanson C, Hisanaga T, et al. Pharmacodynamic activity of telithromycin against macrolide-susceptible and macrolide-resistant Streptococcus pneumoniae simulating clinically achievable free serum and epithelial lining fluid concentrations. J Antimicrob Chemother 2004; 54: 1072-7 84. De Vecchi E, Nicola L, Larosa M, et al. In vitro activity of telithromycin against Haemophilus influenzae at epithelial lining fluid concentrations. BMC Microbiol 2008; 8: 23 85. Al-Lahham A, Reinert RR. Time-kill kinetics of Streptococcus pneumoniae with reduced susceptibility to telithromycin. Chemotherapy 2007; 53: 190-3 86. Chierakul N, Klomsawat D, Chulavatnatol S, et al. Intrapulmonary pharmacokinetics of ofloxacin in drug-resistant tuberculosis. Int J Tuberc Lung Dis 2001; 5: 278-82 87. Andrews JM, Honeybourne D, Brenwald NP, et al. Concentrations of trovafloxacin in bronchial mucosa, epithelial lining fluid, alveolar macrophages and serum after administration of single or multiple oral doses to patients undergoing fibre-optic bronchoscopy. J Antimicrob Chemother 1997; 39: 797-802 PR, et al. Trovafloxacin con88. Peleman RA, Van De Velde V, Germonpre centrations in airway of patients with severe community-acquired pneumonia. Antimicrob Agents Chemother 2000; 44: 178-80 89. Honeybourne D, Banerjee D, Andrews J, et al. Concentrations of gatifloxacin in plasma and pulmonary compartments following a single 400 mg oral dose in patients undergoing fibre-optic bronchoscopy. J Antimicrob Chemother 2001; 48: 63-6 90. Kikuchi J, Yamazaki K, Kikuchi E, et al. Pharmacokinetics of gatifloxacin after a single oral dose in healthy young adult subjects and adult patients with chronic bronchitis, with a comparison of drug concentrations obtained by bronchoscopic microsampling and bronchoalveolar lavage. Clin Ther 2007; 29: 123-30 91. Andrews J, Honeybourne D, Jevons G, et al. Concentrations of garenoxacin in plasma, bronchial mucosa, alveolar macrophages and epithelial lining fluid following a single oral 600 mg dose in healthy adult subjects. J Antimicrob Chemother 2003; 51: 727-30 92. Panteix G, Harf R, Desnottes JR, et al. Accumulation of pefloxacin in the lower respiratory tract demonstrated by bronchoalveolar lavage. J Antimicrob Chemother 1994; 33: 979-85 93. Wise R, Andrews J, Imbimbo BP, et al. The penetration of rufloxacin into sites of potential infection in the respiratory tract. J Antimicrob Chemother 1993; 32: 861-6 94. Honeybourne D, Andrews JM, Cunningham B, et al. The concentrations of clinafloxacin in alveolar macrophages, epithelial lining fluid, bronchial mucosa and serum after administration of single 200 mg oral doses to patients undergoing fibre-optic bronchoscopy. J Antimicrob Chemother 1999; 43: 153-5 95. Baldwin DR, Wise R, Andrews JM, et al. The distribution of temafloxacin in bronchial epithelial lining fluid, alveolar macrophages and bronchial mucosa. Eur Respir J 1992; 5: 471-6 96. Wise R, Baldwin DR, Andrews JM, et al. Comparative pharmacokinetic disposition of fluoroquinolones in the lung. J Antimicrob Chemother 1991; 28 Suppl. C: 65-71
2011 Adis Data Information BV. All rights reserved.
97. Cazzola M, Matera MG, Tufano MA, et al. Pulmonary disposition of lomefloxacin in patients with acute exacerbations of chronic obstructive pulmonary disease: a multiple-dose study. J Chemother 2001; 13: 407-12 98. Baldwin DR, Wise R, Andrews JM, et al. Comparative bronchoalveolar concentrations of ciprofloxacin and lomefloxacin following oral administration. Respir Med 1993; 87: 595-601 99. Schuller P, Zemper K, Borner K, et al. Penetration of sparfloxacin and ciprofloxacin into alveolar macrophages, epithelial lining fluid, and polymorphonuclear leucocytes. Eur Respir J 1997; 10: 1130-8 100. Honeybourne D, Greaves I, Baldwin DR, et al. The concentrations of sparfloxacin in lung tissues after single and multiple oral doses. Int J Antimicrob Agents 1994; 4: 151-5 101. Gotfried MH, Danziger LH, Rodvold KA. Steady-state plasma and intrapulmonary concentrations of levofloxacin and ciprofloxacin in healthy adult subjects. Chest 2001; 119: 1114-22 102. Soman A, Honeybourne D, Andrews J, et al. Concentrations of moxifloxacin in serum and pulmonary compartments following a single 400 mg oral dose in patients undergoing fibre-optic bronchoscopy. J Antimicrob Chemother 1999; 44: 835-8 103. Brillault J, De Castro WV, Harnois T, et al. P-glycoprotein-mediated transport of moxifloxacin in a Calu-3 lung epithelial cell model. Antimicrob Agents Chemother 2009; 53: 1457-62 104. Morrissey I, George JT. Measurement of the bactericidal activity of fluoroquinolones against Streptococcus pneumonia using the bactericidal index method. Int J Antimicrob Agents 2001; 17: 33-7 105. Florea NR, Tessier PR, Zhang C, et al. Pharmacodynamics of moxifloxacin and levofloxacin at simulated epithelial lining fluid drug concentrations against Streptococcus penumoniae. Antimicrob Agents Chemother 2004; 48: 1215-21 106. Schubert S, Dalhoff A, Stass H, et al. Pharmacodynamics of moxifloxacin and levofloxacin simulating human serum and lung concentrations. Infection 2005; 33 Suppl. 2: 15-21 107. Lee SY, Fan HW, Sutherland C, et al. Antibacterial effects of moxifloxacin and levofloxacin simulating epithelial lining fluid concentrations against community-acquired methicillin-resistant Staphylococcus aureus. Drugs R D 2007; 8: 69-77 108. Deryke CA, Du X, Nicolau DP. Evaluation of bacterial kill when modeling the bronchopulmonary pharmacokinetic profile of moxifloxacin and levofloxacin against parC-containing isolates of Streptococcus pneumoniae. J Antimicrob Chemother 2006; 58: 601-9 109. Noreddin AM, Reese AA, Ostroski M, et al. Comparative pharmacodynamics of garenoxacin, gemifloxacin, and moxifloxacin in communityacquired pneumonia caused by Streptococcus pneumoniae: a Monte Carlo simulation analysis. Clin Ther 2007; 29: 2685-9 110. De Vecchi E, Nicola L, Ossola F, et al. In vitro selection of resistance in Streptococcus pneumoniae at in vivo fluoroquinolone concentrations. J Antimicrob Chemother 2009; 63: 721-7 111. Andrews JM, Honeybourne D, Jevons G, et al. Concentrations of levofloxacin (HR 355) in the respiratory tract following a single oral dose in patients undergoing fibre-optic bronchoscopy. J Antimicrob Chemother 1997; 40: 573-7 112. Zhang J, Xie X, Zhou X, et al. Permeability and concentration of levofloxacin in epithelial lining fluid in patients with lower respiratory tract infections. J Clin Pharmacol 2010; 50: 922-8 113. Boselli E, Breilh D, Rimmele T, et al. Pharmacokinetics and intrapulmonary diffusion of levofloxacin in critically ill patients with severe communityacquired pneumonia. Crit Care Med 2005; 33: 104-9 114. Conte Jr JE, Golden JA, McIver M, et al. Intrapulmonary pharmacokinetics and pharmacodynamics of high-dose levofloxacin in healthy volunteer subjects. Int J Antimicrob Agents 2006; 28: 114-21 115. Conte Jr JE, Golden JA, McIver M, et al. Intrapulmonary pharmacodynamics of high-dose levofloxacin in subjects with chronic bronchitis or
Clin Pharmacokinet 2011; 50 (10)
Penetration of Antibacterial Agents into Pulmonary ELF
663
chronic obstructive pulmonary disease. Int J Antimicrob Agents 2007; 30: 422-7 116. Drusano GL, Preston SL, Gotfried MH, et al. Levofloxacin penetration into epithelial lining fluid as determined by population pharmacokinetic modeling and Monte Carlo simulation. Antimicrob Agents Chemother 2002; 46: 586-9 117. Noreddin AM, Marras TK, Sanders K, et al. Pharmacodynamic target attainment analysis against Streptococcus pneumoniae using levofloxacin 500 mg, 750 mg, and 1000 mg once daily in plasma (P) and epithelial lining fluid (ELF) of hospitalized patients with community acquired pneumonia. Int J Antimicrob Agents 2004; 24: 479-84 118. Louie A, Fregeau C, Liu W, et al. Pharmacodynamics of levofloxacin in a murine pneumonia model of Pseudomonas aeruginosa infection: determination of epithelial lining fluid targets. Antimicrob Agents Chemother 2009; 53: 3325-30 119. Panidis D, Markantonis SL, Boutzouka E, et al. Penetration of gentamicin into the alveolar lining fluid of critically ill patients with ventilatorassociated pneumonia. Chest 2005; 128: 545-52 120. Mazzei T, Novelli A, De Lalla F, et al. Tissue penetration and pulmonary disposition of tobramycin. J Chemother 1995; 7: 363-70 121. Carcas AJ, Garcia-Satue JL, Zapater P, et al. Tobramycin penetration into epithelial lining fluid of patients with pneumonia. Clin Pharmacol Ther 1999; 65: 245-50 122. Boselli E, Breilh D, Djabarouti S, et al. Reliability of mini-bronchoalveolar lavage for the measurement of epithelial lining fluid concentrations of tobramycin in critically ill patients. Intensive Care Med 2007; 33: 1519-23 123. Rosenfeld M, Gibson R, McNamara S, et al. Serum and lower respiratory tract drug concentrations after tobramycin inhalation in young children with cystic fibrosis. J Pediatr 2001; 139: 572-7 124. Valcke VJ, Vogelaers DP, Colardyn FA, et al. Penetration of netilmicin in the lower respiratory tract after once-daily dosing. Chest 1992; 101: 1028-32 125. Rybak M, Lomaestro B, Rotschafer JC, et al. Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm 2009; 66: 82-98 126. Scheetz MH, Wunderink RG, Postelnick MJ, et al. Potential impact of vancomycin pulmonary distribution on treatment outcomes in patients with methicillin-resistant Staphylococcus aureus pneumonia. Pharmacotherapy 2006; 26: 539-50 127. Lamer C, De Beco V, Soler P, et al. Analysis of vancomycin entry into pulmonary lining fluid by bronchoalveolar lavage in critically ill patients. Antimicrob Agents Chemother 1993; 37: 281-6 128. Georges H, Leroy O, Alfandari S, et al. Pulmonary disposition of vancomycin in critically ill patients. Eur J Clin Microbiol Infect Dis 1997; 16: 385-8 129. Rodvold KA, Gotfried MH, Loutit JS, et al. Plasma and intrapulmonary concentrations of oritavancin and vancomycin in normal healthy adults [abstract no. O-254]. Clin Microbiol Infect 2004; 10 Suppl. 3: 44 130. Mimoz O, Rolland D, Adoun M, et al. Steady-state trough serum and epithelial lining fluid concentrations of teicoplanin 12 mg/kg per day in patients with ventilator-associated pneumonia. Intensive Care Med 2006; 32: 775-9 131. Gotfried MH, Shaw J-P, Benton BM, et al. Intrapulmonary distribution of intravenous telavancin in healthy subjects and effects of pulmonary surfactant on in vitro activities of telavancin and other antibiotics. Antimicrob Agents Chemother 2008; 52: 92-7 132. Drusano GL, Rubino CM, Ambrose PG, et al. Penetration of vancomycin into epithelial lining fluid [abstract no. A-11]. 47th Interscience Conference for Antimicrobial Agents and Chemotherapy (ICAAC); 2007 Sep 17-20; Chicago (IL) 133. Harigaya Y, Bulitta JB, Forrest A, et al. Pharmacodynamics of vancomycin at simulated epithelial lining fluid concentrations against methicillin-resistant
2011 Adis Data Information BV. All rights reserved.
Staphylococcus aureus (MRSA): implications for dosing in MRSA pneumonia. Antimicrob Agents Chemother 2009; 53: 3894-901 134. Lodise TP, Gotfried M, Barriere S, et al. Telavancin penetration into human epithelial lining fluid determined by population pharmacokinetic modeling and Monte Carlo simulation. Antimicrob Agents Chemother 2008; 52: 2300-4 135. Conte Jr JE, Golden JA, Kipps J, et al. Intrapulmonary pharmacokinetics of linezolid. Antimicrob Agents Chemother 2002; 46: 1475-80 136. Honeybourne D, Tobin C, Jevons G, et al. Intrapulmonary penetration of linezolid. J Antimicrob Chemother 2003; 51: 1431-4 137. Boselli E, Breilh D, Rimmele T, et al. Pharmacokinetics and intrapulmonary concentrations of linezolid administered to critically ill patients with ventilator-associated pneumonia. Crit Care Med 2005; 33: 1529-33 138. Conte Jr JE, Golden JA, Kelly MG, et al. Steady-state serum and intrapulmonary pharmacokinetics and pharmacodynamics of tigecycline. Int J Antimicrob Agents 2005; 25: 523-9 139. Andrews J, Honeybourne D, Ashby J, et al. Concentrations in plasma, epithelial lining fluid, alveolar macrophages and bronchial mucosa after a single intravenous dose of 1.6 mg/kg of iclaprim (AR-100) in healthy men. J Antimicrob Chemother 2007; 60: 677-80 140. Rubino CM, Ma L, Bhavnani SM, et al. Evaluation of tigecycline penetration into the colon wall tissue and epithelial lining fluid using a population pharmacokinetic model and Monte Carlo simulation. Antimicrob Agents Chemother 2007; 51: 2085-9 141. Crandon JL, Kim A, Nicolau DP. Comparison of tigecycline penetration into the epithelial lining fluid of infected and uninfected murine lungs. J Antimicrob Chemother 2009; 64: 837-9 142. Koomanachai P, Crandon JL, Banevicius MA, et al. Pharmacodynamic profile of tigecycline against methicillin-resistant Staphylococcus aureus in an experimental pneumonia model. Antimicrob Agents Chemother 2009; 53: 5060-3 143. Deguchi Y, Sun J, Tauchi Y, et al. Distribution characteristics of grepafloxacin, a fluoroquinolone antibiotic, in lung epithelial lining fluid and alveolar macrophage. Drug Metab Pharmacokinet 2003; 18: 319-26 144. Sun J, Deguchi Y, Tauchi Y, et al. Distribution characteristics of orally administered olamufloxacin, a newly synthesized fluoroquinolone antibacterial, in lung epithelial lining fluid and alveolar macrophage in rats. Eur J Pharm Biopharm 2006; 64: 238-45 145. Aoki M, Iguchi M, Hayashi H, et al. Active uptake of ulifloxacin in plasma to lung that controls its concentrations in epithelial lining fluid. Biol Pharm Bull 2009; 32: 1095-100 146. Winther L, Guardabassi L, Baptiste KE, et al. Antimicrobial disposition in pulmonary epithelial lining fluid of horses: part I. Sulfadiazine and trimethoprim. J Vet Pharmacol Ther 2011; 34: 277-84 Hansen S, Baptiste KE, et al. Antimicrobial disposition in 147. Winther L, Honore pulmonary epithelial lining fluid of horses: part II. Doxycycline. J Vet Pharmacol Ther 2011; 34: 285-9 148. Winther L, Baptiste KE, Friis C. Antimicrobial disposition in pulmonary epithelial lining fluid of horses: part III. Cefquinome. J Vet Pharmacol Ther. Epub 2010 Nov 18 149. Winther L, Baptiste KE, Friss C. Pharmacokinetics in pulmonary epithelial lining fluid and plasma of ampicillin and pivampicillin administered to horses. Res Vet Sci. Epub 2010 Dec 6 150. Javsicas LH, Giguere S, Womble AY. Disposition of oral telithromycin in foals and in vitro activity of the drug against macrolide-susceptible and macrolide-resistant Rhodococcus equi isolates. J Vet Pharmacol Ther 2010; 33: 383-8 151. Womble A, Giguere S, Lee EA. Pharmacokinetics of oral doxycycline and concentrations of body fluids and bronchoalveolar cells of foals. J Vet Pharmacol Ther 2007; 30: 187-93
Clin Pharmacokinet 2011; 50 (10)
664
Rodvold et al.
152. Womble AY, Giguere S, Lee EA, et al. Pharmacokinetics of clarithromycin and concentrations in body fluids and bronchoalveolar cells of foals. Am J Vet Res 2006; 67: 1681-6 153. Jacks S, Giguere S, Gronwall RR, et al. Pharmacokinetics of azithromycin and concentrations in body fluids and bronchoalveolar cells of foals. Am J Vet Res 2001; 62: 1870-5 154. Suarez-Mier G, Giguere S, Lee EA. Pulmonary disposition of erythromycin, azithromycin, and clarithromycin in foals. J Vet Pharmacol Ther 2007; 30: 109-55 155. Hawkins EC, Boothe DM, Guinn A, et al. Concentrations of enrofloxacin and its active metabolite in alveolar macrophages and pulmonary epithelial lining fluid in dogs. J Vet Pharmacol Ther 1998; 21: 18-23 156. Togami K, Chono S, Seki T, et al. Aerosol-based efficient delivery of telithromycin, a ketolide antimicrobial agent, to lung epithelial lining fluid and alveolar macrophages for treatment of respiratory infections. Drug Dev Ind Pharm 2010; 36: 861-6 157. Togami K, Chono S, Seki T, et al. Distribution characteristics of telithromycin, a novel ketolide antimicrobial agent applied for treatment of
respiratory infection, in lung epithelial lining fluid and alveolar macrophages. Drug Metab Pharmacokinet 2009; 24: 411-7 158. Chono S, Tanino T, Seki T, et al. Efficient drug delivery to alveolar macrophages and lung epithelial lining fluid following pulmonary administration of liposomal ciprofloxacin in rats with pneumonia and estimation of its antibacterial effects. Drug Dev Ind Pharm 2008; 34: 1090-6 159. Chono S, Suzuki H, Togami K, et al. Efficient drug delivery to lung epithelial lining fluid by aerosolization of ciprofloxacin incorporated into PEGylated liposomes for treatment of respiratory infections. Drug Dev Ind Pharm 2011; 37: 367-72 160. Chono S, Tanino T, Seki T, et al. Pharmacokinetic and pharmacodynamic efficacy of intrapulmonary administration of ciprofloxacin for the treatment of respiratory infections. Drug Metab Pharmacokinet 2007; 22: 88-95
Correspondence: Professor Keith A. Rodvold, University of Illinois at Chicago, College of Pharmacy, m/c 886, 833 South Wood Street, Room # 164, Chicago, IL 60612, USA. E-mail: kar@uic.edu
2011 Adis Data Information BV. All rights reserved.
Clin Pharmacokinet 2011; 50 (10)
You might also like
- An Overview of Topical Antifungal Therapy in Dermatomycoses: A North American PerspectiveDocument30 pagesAn Overview of Topical Antifungal Therapy in Dermatomycoses: A North American PerspectivePseodostiintaNo ratings yet
- Similar But Not The Same Differential Diagnosis of HLH and SepsisDocument12 pagesSimilar But Not The Same Differential Diagnosis of HLH and SepsisJuan JoséNo ratings yet
- Meropenem: A Review of Its Use in Patients in Intensive CareDocument28 pagesMeropenem: A Review of Its Use in Patients in Intensive CareHAIDAR RACHMANNo ratings yet
- Review in Electrospinning 2Document25 pagesReview in Electrospinning 2Muaathe IbrahimNo ratings yet
- Risk factors associated with colic in horses: A review of epidemiological studiesDocument13 pagesRisk factors associated with colic in horses: A review of epidemiological studiesJuan Manuel HenaoNo ratings yet
- Guidelines For Sample Collection PostmortemDocument9 pagesGuidelines For Sample Collection PostmortemJhoŋ AcerosNo ratings yet
- 2023 Guidelines On AntthrombDocument63 pages2023 Guidelines On AntthrombjoannahalmanNo ratings yet
- Morfología Chlorella VulgarisDocument14 pagesMorfología Chlorella VulgarisFlor IV IrNo ratings yet
- Tuberculosis Vaccines and Prevention of InfectionDocument22 pagesTuberculosis Vaccines and Prevention of InfectionSorina ElenaNo ratings yet
- J Jchromb 2006 07 035Document29 pagesJ Jchromb 2006 07 035Hasna NoerNo ratings yet
- Journal of Oral and Maxillofacial Surgery, Medicine, and PathologyDocument9 pagesJournal of Oral and Maxillofacial Surgery, Medicine, and PathologyabdulrazaqNo ratings yet
- Lipids QPDocument14 pagesLipids QPJainam Mehta100% (1)
- Eusinofil Pneumonia PDFDocument12 pagesEusinofil Pneumonia PDFBrigita GalileoNo ratings yet
- Quaternary Protoberberine Alkaloids (Must Read)Document26 pagesQuaternary Protoberberine Alkaloids (Must Read)Akshay AgnihotriNo ratings yet
- The International Journal of Biochemistry & Cell BiologyDocument15 pagesThe International Journal of Biochemistry & Cell BiologyNathalia PietraniNo ratings yet
- A Review On Application of Flocculants in Wastewater TreatmentDocument20 pagesA Review On Application of Flocculants in Wastewater TreatmentHuy Nguyen100% (1)
- Seminars in Cell & Developmental Biology: Shan Liao, P.Y. Von Der WeidDocument7 pagesSeminars in Cell & Developmental Biology: Shan Liao, P.Y. Von Der WeidItzelArteagaNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument6 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive Biologydiego jNo ratings yet
- Antiseptics and Disinfectants: Activity, Action, and ResistanceDocument34 pagesAntiseptics and Disinfectants: Activity, Action, and ResistanceShare linkNo ratings yet
- Barreras en El Crebro en DesarrolloDocument19 pagesBarreras en El Crebro en DesarrolloAlvarez Flores GilmerNo ratings yet
- Advances in Biomedical and Pharmaceutical Applications of Functional Bacterial Cellulose-Based NanocompositesDocument23 pagesAdvances in Biomedical and Pharmaceutical Applications of Functional Bacterial Cellulose-Based NanocompositesFreddy Albaro Manayay LLaguentoNo ratings yet
- Properties of Cordyceps Sinensis A Review - 2013 - Journal of Functional FoodsDocument20 pagesProperties of Cordyceps Sinensis A Review - 2013 - Journal of Functional FoodsSara SanabriaNo ratings yet
- Test InterpretDocument243 pagesTest Interpretjogendra.singhNo ratings yet
- Fungal and Parasitic Infections of The E PDFDocument24 pagesFungal and Parasitic Infections of The E PDFScerbatiuc CristinaNo ratings yet
- West Nile VirusDocument14 pagesWest Nile VirusHawa MasfufahNo ratings yet
- Crossm: Current and Emerging Topical Antibacterials and Antiseptics: Agents, Action, and Resistance PatternsDocument34 pagesCrossm: Current and Emerging Topical Antibacterials and Antiseptics: Agents, Action, and Resistance PatternsVlady78No ratings yet
- Akhtar 2015Document6 pagesAkhtar 2015Rizwan TonoyNo ratings yet
- Coordination Chemistry Reviews: Luigi Messori, Antonello MerlinoDocument23 pagesCoordination Chemistry Reviews: Luigi Messori, Antonello MerlinoFelipe BrondaniNo ratings yet
- Tace Convencional 2013Document20 pagesTace Convencional 2013PeñaTaurina El ClarinNo ratings yet
- Antimicrobial Herb and Spice Compounds in FoodDocument20 pagesAntimicrobial Herb and Spice Compounds in FoodPrabowo SuryaningtyasNo ratings yet
- 先天免疫学糖生物学Document673 pages先天免疫学糖生物学Wenbo Yan100% (1)
- Laboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottDocument29 pagesLaboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottChangNo ratings yet
- Hormonal Signaling and Signal Pathway Crosstalk in The Control of Myometrial Calcium DynamicsDocument10 pagesHormonal Signaling and Signal Pathway Crosstalk in The Control of Myometrial Calcium DynamicsayluyNo ratings yet
- Laboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottDocument29 pagesLaboratory Diagnosis of Bacterial Gastroenteritis: Romney M. Humphries, Andrea J. LinscottFatah Jati PNo ratings yet
- Guillain-Barré Syndrome: Understanding Epidemiology, Pathophysiology and ManagementDocument15 pagesGuillain-Barré Syndrome: Understanding Epidemiology, Pathophysiology and ManagementindadzilarsyNo ratings yet
- M. N. Ghosh - Fundamentals of Experimental Pharmacology (2019)Document274 pagesM. N. Ghosh - Fundamentals of Experimental Pharmacology (2019)Achyut KanungoNo ratings yet
- Antiseptics and Disinfectants: Activity, Action, and ResistanceDocument33 pagesAntiseptics and Disinfectants: Activity, Action, and ResistanceDevalina JunaharNo ratings yet
- Interference of Antibacterial Agents With Phagocyte Functions: Immunomodulation or "Immuno-Fairy Tales"?Document3 pagesInterference of Antibacterial Agents With Phagocyte Functions: Immunomodulation or "Immuno-Fairy Tales"?greeenbeeNo ratings yet
- Per Halkjaer Nielsen, Holger Daims, Hilde Lemmer - FISH Handbook For Biological Wastewater Treatment - Identification and Quantification of Microorganisms in Activated Sludge and Biofilms by FISH-IntlDocument137 pagesPer Halkjaer Nielsen, Holger Daims, Hilde Lemmer - FISH Handbook For Biological Wastewater Treatment - Identification and Quantification of Microorganisms in Activated Sludge and Biofilms by FISH-IntlEbenezer CarvalhoNo ratings yet
- RodenticidasDocument11 pagesRodenticidasAny MartNo ratings yet
- Journal of Molecular Liquids: Mumtaz A. Quraishi, Dheeraj Singh Chauhan, Viswanathan S. SajiDocument40 pagesJournal of Molecular Liquids: Mumtaz A. Quraishi, Dheeraj Singh Chauhan, Viswanathan S. SajiRawan AbdullahNo ratings yet
- Metodos de Extraccion de CarrageninaDocument16 pagesMetodos de Extraccion de CarrageninaDeivi CcNo ratings yet
- Nikolai Vekshin - Biophysics of Mitochondria-Springer International Publishing - Springer (2019)Document205 pagesNikolai Vekshin - Biophysics of Mitochondria-Springer International Publishing - Springer (2019)Leandro Dellacqua100% (1)
- Mip As BiosensorDocument15 pagesMip As Biosensorhareesh13hNo ratings yet
- Literatura BrightenylDocument39 pagesLiteratura BrightenylMaiko CarlosNo ratings yet
- Mycobacterium Tuberculosis Pathogenesis and Molecular: Determinants of VirulenceDocument34 pagesMycobacterium Tuberculosis Pathogenesis and Molecular: Determinants of VirulenceGrafita DyahNo ratings yet
- 3058 Simpson Forensic MedicineDocument26 pages3058 Simpson Forensic MedicineHendro SihalohoNo ratings yet
- Bupropion 3Document37 pagesBupropion 3Robert MovileanuNo ratings yet
- Microbiology and ImmunologyDocument274 pagesMicrobiology and Immunologychiprios100% (5)
- Structure and Biological Activities of The Polysaccharides From The Leaves, Roots and Fruits of Panax Ginseng C.A. Meyer: An OverviewDocument10 pagesStructure and Biological Activities of The Polysaccharides From The Leaves, Roots and Fruits of Panax Ginseng C.A. Meyer: An OverviewAlfredo de la CruzNo ratings yet
- Treatment of Allergic Rhinitis in Infants and ChildrenDocument36 pagesTreatment of Allergic Rhinitis in Infants and ChildrenMuhammad Agung HidayatNo ratings yet
- Supercritical Fluid ChromatographyDocument33 pagesSupercritical Fluid ChromatographyNatalia GalloNo ratings yet
- Hidrólisis Asistida Por UltrasonidoDocument38 pagesHidrólisis Asistida Por UltrasonidoGabriel Hernandez MoralesNo ratings yet
- Epidemiology of and Diagnostic Strategies For ToxoplasmosisDocument34 pagesEpidemiology of and Diagnostic Strategies For ToxoplasmosisEduardo UlloaNo ratings yet
- phaRMACOCINETICA NICOTINA 2005Document37 pagesphaRMACOCINETICA NICOTINA 2005Alin DragosNo ratings yet
- Food Chemistry: Nidheesh Thadathil, Suresh Puthanveetil VelappanDocument8 pagesFood Chemistry: Nidheesh Thadathil, Suresh Puthanveetil VelappanAr Rahman ArifNo ratings yet
- Retention and Selectivity in Liquid Chromatography: Prediction, Standardisation and Phase ComparisonsFrom EverandRetention and Selectivity in Liquid Chromatography: Prediction, Standardisation and Phase ComparisonsNo ratings yet
- All About Albumin: Biochemistry, Genetics, and Medical ApplicationsFrom EverandAll About Albumin: Biochemistry, Genetics, and Medical ApplicationsNo ratings yet
- Laser Retinopexy PDFDocument4 pagesLaser Retinopexy PDFveerroxxNo ratings yet
- Updates in Management of Enterocutaneous FistulaDocument35 pagesUpdates in Management of Enterocutaneous FistulabashiruNo ratings yet
- Liver Function TestsDocument3 pagesLiver Function Testssamdaman001No ratings yet
- Kalten BornDocument34 pagesKalten BornjayadevanNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex 10 List of Alternative Documents For Record of Operative or Surgical TechniqueDocument14 pagesPhilHealth Circular No. 0035, s.2013 Annex 10 List of Alternative Documents For Record of Operative or Surgical TechniqueChrysanthus HerreraNo ratings yet
- Hepatomegali in Infant and Children - Pediatrics in Review-2000-Wolf-303-10Document10 pagesHepatomegali in Infant and Children - Pediatrics in Review-2000-Wolf-303-10Reddy LufyanNo ratings yet
- Malaysian vaccine certificate detailsDocument1 pageMalaysian vaccine certificate detailsNuh NuhaNo ratings yet
- Obsessive Compulsive DisorderDocument13 pagesObsessive Compulsive Disorderapi-296998780No ratings yet
- Atlas of Pain Management Injection TechniquesDocument3 pagesAtlas of Pain Management Injection TechniquesMudassar SattarNo ratings yet
- Health Survey and Development CommitteeDocument10 pagesHealth Survey and Development CommitteeNidhiNo ratings yet
- Atropine SulfateDocument2 pagesAtropine SulfateKureaa OhNo ratings yet
- Health Promotion and Aging - Chapter 1Document13 pagesHealth Promotion and Aging - Chapter 1Rong Zhuang100% (1)
- Prolonged pregnancy & abnormal uterine actionDocument110 pagesProlonged pregnancy & abnormal uterine actionAnnapurna DangetiNo ratings yet
- Thromboangiitis Obliterans (Buerger Disease)Document12 pagesThromboangiitis Obliterans (Buerger Disease)Sheila AzelyaNo ratings yet
- Clinical Case Reports - 2018 - Toh Yoon - A Novel Semi Solidifying Liquid Formula Via The Nasogastric Route To MaintainDocument5 pagesClinical Case Reports - 2018 - Toh Yoon - A Novel Semi Solidifying Liquid Formula Via The Nasogastric Route To MaintainValentina RusuNo ratings yet
- Technique of Blood CollectionDocument8 pagesTechnique of Blood CollectionVivek TiwariNo ratings yet
- StarHealthAssureInsurancePolicy BrochureDocument13 pagesStarHealthAssureInsurancePolicy Brochurepradosh002No ratings yet
- Balancing BTWN Efficiency and SatisfactionDocument4 pagesBalancing BTWN Efficiency and SatisfactionJessy WairiaNo ratings yet
- 60 Item Pediatric Nursing Exam by JeddahDocument10 pages60 Item Pediatric Nursing Exam by Jeddahchelljynxie100% (1)
- AgnikarmReferenceManual PDFDocument11 pagesAgnikarmReferenceManual PDFPrakash ChavanNo ratings yet
- Tracheomalacia home workDocument11 pagesTracheomalacia home workAgung BhaktiyarNo ratings yet
- Basic Life Support Protocol MatrixDocument1 pageBasic Life Support Protocol MatrixAleksandar PetrovicNo ratings yet
- Pathophysiology: AppendicitisDocument3 pagesPathophysiology: AppendicitisEqah TajuddinNo ratings yet
- Product MonographDocument15 pagesProduct MonographAryl LyraNo ratings yet
- List of Drugs: DRUGS Acting On ANS Respiratory DrugsDocument2 pagesList of Drugs: DRUGS Acting On ANS Respiratory DrugsShambhu AshokNo ratings yet
- Strategies For Dengue Control ProgramDocument22 pagesStrategies For Dengue Control ProgramNaseem QaziNo ratings yet
- Clinical Exam of The Psychiatric PX HX MSE Signs Symptoms Modified For Senior Clerks 2021Document139 pagesClinical Exam of The Psychiatric PX HX MSE Signs Symptoms Modified For Senior Clerks 2021Rakesh KumarNo ratings yet
- Righ Choise TrialDocument17 pagesRigh Choise TrialOscar FloresNo ratings yet
- 10 LeprosyDocument27 pages10 LeprosyMakWohWeiNo ratings yet
- Book1new Table B6Document12 pagesBook1new Table B6Maryam BajNo ratings yet