Professional Documents
Culture Documents
Samantha Ford: Description of Situation and Environment in Which Interaction Took Place
Uploaded by
Samantha FordOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Samantha Ford: Description of Situation and Environment in Which Interaction Took Place
Uploaded by
Samantha FordCopyright:
Available Formats
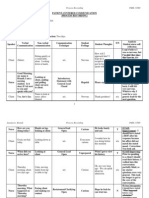
STUDENT NAME: Samantha Ford DATE: __3/23/2010____________________________________________________
DESCRIPTION OF SITUATION AND ENVIRONMENT IN WHICH INTERACTION TOOK PLACE: The
patient (MM) was lying in her bed in a normal supine position when I (SF) walked into the room. MM appeared to be asleep, but as I (SF) walked into the room she opened her eyes and seemed open to conversation, so I introduced myself. MM didnt look to be having any pain or discomfort and was receptive to my conversation and care. The room was quiet and peaceful when I walked in with no family members in attendance.
PROCESS RECORDING SN FACILITATIVE COMMUNICATION TECHNIQUES, BLOCKS TO COMMUNICATION, PREFERRED RESPONSES AND/OR ALTERNATE RESPONSES DEFENSE/COPING MECHANISMS EXHIBITED BY CLIENT PERCEIVED THOUGHTS (T), FEELINGS (F), BELIEFS (B) & VALUES(V) OF BOTH CLIENT AND STUDENT NURSE (WRITE OUT AND LABEL)
VERBAL INTERACTION
NON-VERBAL CUES/ACTIONS
SF: Hello, Mrs. Mrs. M , my name is S F . I am a nursing student from Kent State University and I am going to be taking care of you this morning.
I smiled and kept eye contact while speaking.
Giving information.
I was nervous because I wasnt sure if MM was going to be receptive to having a conversation with me (F).
MM: Hello.
She readjusted her position so she was sitting up. She smiled when speaking.
I think she felt a little at a disadvantage with me standing over her while she was confined to lying in bed so she readjusted her position (T).
SF: Tell me how you are feeling this morning?
I moved closer to the patient and pulled the room chair closer to the bed and sat down so I was at eye level with her Offering self.
Open-ended question.
I pulled the chair next to the bed because I felt that it would make her more comfortable and open to conversing with me. I felt that it was a way of showing respect (V). I had to stop myself from saying are you feeling better which would have been a closed-ended statement (T).
MM: I am feeling better. I am tired because I didnt sleep much last night.
MM spoke directly to me keeping eye contact. She shrugged while talking about how she didnt get much sleep. Focused question. Although its a focused question its also a closed-ended question. A preferred response might have been Youve had trouble sleeping?, which is an example of paraphrasing. Paraphrasing the question might have encouraged more elaboration. MM was coping with the lifestyle change of not being able to control her sleeping schedule by chalking it up to being a normal untreatable symptom of getting older. Reflecting feelings, focused question, encouraging elaboration.
It seemed to me that MM was unhappy about not getting much sleep, which is understandable, but that she was also used to having trouble sleeping (B).
SF: Have you had trouble sleeping before?
I made direct eye contact and kept my facial expression and posture attentive to encourage elaboration.
It felt very awkward for me to keep direct eye contact; its something Im not used to doing (F).
MM: Yes, I dont often sleep through the night anymore. I usually sleep a little and then wake up, and am not able to go back to sleep. Then I am tired throughout the day. SF: That must be very frustrating to you. MM: It is very frustrating. I am usually very active and being tired during the day limits me and makes me feel old. SF: Mmhm.
MM had a resigned look on her face and seemed a little bit agitated.
It seemed that MM was very frustrated with her sleeping schedule and was resigned to having to deal with it for the foreseeable future (B).
I touched MMs shoulder to convey sympathy- therapeutic touch. MM, again, seemed agitated and had a frustrated look on her face.
I felt awkward touching the patient and unsure of how MM would respond (F). MM was feeling very discouraged with her situation (F). Honestly, I wasnt sure how to respond in a way that would make her feel better (F).I almost said I understand how you feel, but realized that that was a stereotyped response. MM is distressed with her sleeping problem and because it is affecting her husband as well (B). She might also be a little resentful because he doesnt seem to be very sympathetic to her situation (T).
Silence/Active listening.
Instead of saying Mmhm I could have said something like Go on to convey that I am listening and to encourage MM to continue.
MM: Its frustrating for my husband too. He always tells me go back to bed like its my fault that Im awake in the middle of the night. I tell him that I cant help it, I just cant fall back asleep.
MM had a frown on her face and shifted in bed, seeming uncomfortable.
SF: Not being able to sleep through the night is very distressing to you because it makes you tired throughout the day and limits your everyday activities, and because it upsets your husband?
I spoke directly to MM keeping eye contact.
Summarizing.
I wanted to let her know that I was listening to her and cared about what she was saying even though having problems sleeping is a common in many people; I wanted to let her know that I care about her distress and would genuinely like to help her (V). MM was feeling hopeless about her situation and resigned to dealing with it (F).
MM: Yes, I just wish there was something I could do to make it easier fall asleep and stay asleep.
After saying this MM sighed.
MM wasnt really exhibiting a defense mechanism; she just seemed resigned to not being able to sleep. You could say that she was rationalizing the problem of not being able to sleep by reasoning that it was an unavoidable aspect of getting older. Focused question. Instead of saying maybe there is something we could do to help it might have been better to say why dont we see if there is anything we can do to help because my original response might be a little falsely reassuring.
SF: Maybe there is something we could do to help. Would it be okay if I let your nurse know how youre feeling about your sleeping situation, and see if she or the doctor might have any suggestions to help out? MM: Yes, I think that would be okay. SF: Okay, I will make sure to let your nurse know. I am going to go and do some more checking on your chart now and will be back to check your vitals shortly.
I kept direct eye contact and smiled as I was speaking to MM.
I wanted to make sure that I got permission before saying something to her nurse or doctor because I value her right to privacy (V).
MM seemed a little more relaxed and had a smile on her face.
Offering of self, giving information.
MM seemed to be feeling better about her situation and more relaxed. (B). I wanted to reassure her that I would make sure I said something to her nurse (V). Also, I wanted her to be aware that I would need to check her vitals soon so she knows ahead of time and is ok with that (V).
I again kept direct eye contact and kept a smile on my face.
1.
2.
Why did you select this interaction? I selected this interaction because I felt that it was a pretty good therapeutic conversation. Also, this was one of the first times that I was able to have time to have a decent therapeutic conversation without having to deal with family members being present, physical therapy interruptions ect., and phone conversations. I felt that MM was very receptive to my conversation and my care and seemed more relaxed after our conversation. What did you learn about IPR from this interaction? I learned that therapeutic communication is genuinely helpful to the patient, but that it is difficult to practice. Paying attention to someones non-verbal cues helps you to read between the lines and understand what is really being said. Also using open ended questions/statements and silence can really help with having a productive conversation instead of yes and no repetition. I do feel that using silence might be a little awkward and is something I will have to get used to, bu t I do see the benefits of this technique. Ive also realized the importance of using the communication technique of offering of self. If you dont offer something in return the patient wont connect with you and wont trust you. If your patient doesnt tr ust you, you have no relationship to build on. I was much more aware of myself and how I am speaking during this conversation. It seemed awkward to keep direct eye contact continually and to make sure I had a smile on my face. I feel that I had a decent conversation and that it was helpful to MM, but I do realize that there are areas in which I can improve to make my verbal and nonverbal communication more congruent and consistent. What kind of interaction was this? Overall, this interaction consisted of nonverbal and verbal therapeutic communication.
3.
You might also like
- Process Recording - SampleDocument3 pagesProcess Recording - SampleMara Magsanoc70% (10)
- MSE Sample PDFDocument5 pagesMSE Sample PDFSam Raven AndresNo ratings yet
- Psychosomatic MedicineDocument262 pagesPsychosomatic MedicineGonzalo Sepulveda Estay100% (1)
- 322 Clinical ReflectionDocument2 pages322 Clinical Reflectionapi-520874386No ratings yet
- Additional Nursing Care Plans - SchizophreniaDocument26 pagesAdditional Nursing Care Plans - SchizophreniaJasmin Jacob100% (5)
- Mental Health Nursing Case StudyDocument11 pagesMental Health Nursing Case Studyapi-499028250No ratings yet
- Jesse Bishop Process Recording FormDocument8 pagesJesse Bishop Process Recording FormVijaya Rani100% (1)
- Module On Life SkillsDocument36 pagesModule On Life SkillsJames De Los ReyesNo ratings yet
- Therapeutic TechniqueDocument3 pagesTherapeutic TechniqueJean Umbay MolinaNo ratings yet
- Running Head: Process Recording 1Document9 pagesRunning Head: Process Recording 1shawnee11No ratings yet
- Everyone Would Be Better Off Without Me" As Verbalized by The PatientDocument4 pagesEveryone Would Be Better Off Without Me" As Verbalized by The PatientDanica Kate GalleonNo ratings yet
- Systematic DesensitizationDocument8 pagesSystematic Desensitizationnosheen murtazaNo ratings yet
- Pyc2601 Assignments PDFDocument82 pagesPyc2601 Assignments PDFNomathemba Mgobhozi II0% (1)
- A Beautiful Mind Schziophrenia Case Study (Movie Review)Document4 pagesA Beautiful Mind Schziophrenia Case Study (Movie Review)Ermela Casillar EspinoNo ratings yet
- Process Recording Example1Document7 pagesProcess Recording Example1Carissa De Luzuriaga-BalariaNo ratings yet
- Paranoid SchizophreniaDocument26 pagesParanoid SchizophreniaCrisha Ann Billones BacutaNo ratings yet
- Paul Solomon Pdf1Document145 pagesPaul Solomon Pdf1John McDermottNo ratings yet
- Topic 10 PERFORMANCE APPRAISAL SEMINARDocument17 pagesTopic 10 PERFORMANCE APPRAISAL SEMINARSimran Josan100% (1)
- Process Recording #1Document2 pagesProcess Recording #1Catlyn Chatpman100% (1)
- Processing Recording 1 (1) .LGreenDocument24 pagesProcessing Recording 1 (1) .LGreenlmgreenNo ratings yet
- Process RecordingDocument5 pagesProcess Recordingkevnique11100% (1)
- IPR SampleDocument4 pagesIPR SampleOliver Leeper100% (4)
- Process RecordingDocument12 pagesProcess RecordingJan Jiv Sanchez MedalloNo ratings yet
- Communication 360 Process RecordingDocument10 pagesCommunication 360 Process Recordingapi-31617818650% (4)
- GRP1 Peurperal Mastitis CONCEPT MAPPINGDocument34 pagesGRP1 Peurperal Mastitis CONCEPT MAPPINGMada mada DaneNo ratings yet
- Psychiatric Nursing - Mental Status ExaminationDocument4 pagesPsychiatric Nursing - Mental Status ExaminationChien Lai R. BontuyanNo ratings yet
- RH Process RecordingDocument3 pagesRH Process Recordingals1974No ratings yet
- Outcome Based EducationDocument46 pagesOutcome Based Educationjohnhenryv100% (4)
- Quiz Process RecordingDocument7 pagesQuiz Process RecordingDewley Guevarra MontenegroNo ratings yet
- Final Reflective Journal 2019Document3 pagesFinal Reflective Journal 2019api-485315684No ratings yet
- Mental Health Nursing Case StudyDocument9 pagesMental Health Nursing Case Studyapi-454984300No ratings yet
- Nursing Management of AggressionDocument7 pagesNursing Management of AggressionMark Guerrero Jabonitalla100% (1)
- Therapeutic Communication Techniques 2Document3 pagesTherapeutic Communication Techniques 2Marc King MagsambolNo ratings yet
- Ipr Conversation Communication PDFDocument4 pagesIpr Conversation Communication PDFSantiago AbrahamNo ratings yet
- 360 Process Recording TemplateDocument13 pages360 Process Recording Templateapi-252910411100% (9)
- Process RecordingDocument12 pagesProcess Recordingapi-302732994100% (4)
- Role Case StudyDocument7 pagesRole Case StudyKomal KhanNo ratings yet
- Mind Tools - Leadership Skills PDFDocument342 pagesMind Tools - Leadership Skills PDFMadalinaBatalu100% (1)
- Process RecordingDocument8 pagesProcess Recordingapi-340063062No ratings yet
- 360 Process RecordingDocument11 pages360 Process Recordingapi-34006085780% (5)
- Process RecordingDocument12 pagesProcess Recordingchristian_cayle100% (1)
- Process RecordingDocument9 pagesProcess Recordingnailed_heartNo ratings yet
- Cues Nursing Diagnosis Outcome Nursingintervention Rationale Evaluation Discharge PlanningDocument5 pagesCues Nursing Diagnosis Outcome Nursingintervention Rationale Evaluation Discharge PlanningBSN 3B-Bulatao,Goergie Ann L. CPUSNNo ratings yet
- Process Recording 2016Document8 pagesProcess Recording 2016Anthony PaguyoNo ratings yet
- Process RecordingDocument10 pagesProcess Recordingmichaelsulivan616450% (2)
- Ipr Mr. CDocument3 pagesIpr Mr. CSamantha Hunter LowmanNo ratings yet
- Process Recording Doument 1Document2 pagesProcess Recording Doument 1Susan Bloomquist DavisNo ratings yet
- PMH Nursing Care Plan 01112017Document19 pagesPMH Nursing Care Plan 01112017api-371817203No ratings yet
- Giselle Riker Process Recording IDocument4 pagesGiselle Riker Process Recording Iapi-281551637No ratings yet
- Omar's Family AssessmentDocument10 pagesOmar's Family AssessmentfaizaNo ratings yet
- Interpersonal Communication Process Recording (Day 2)Document14 pagesInterpersonal Communication Process Recording (Day 2)Kiela Nicole Gatpandan Aguilar67% (3)
- Aa Na Observation Reflection TemplateDocument3 pagesAa Na Observation Reflection Templateapi-426049026No ratings yet
- Compare and Contrast The Insights Into Primary Health Care Provided by DRDocument2 pagesCompare and Contrast The Insights Into Primary Health Care Provided by DRKai GamiaoNo ratings yet
- Nursing DelegationDocument2 pagesNursing DelegationAndre FortunaNo ratings yet
- Psychiatric Nursing Diagnosis List Based On The Nanda-I Nursing Diagnoses (NDS)Document14 pagesPsychiatric Nursing Diagnosis List Based On The Nanda-I Nursing Diagnoses (NDS)Tania sharmaNo ratings yet
- Process RecordingDocument10 pagesProcess Recordingapi-318733585No ratings yet
- Nursing Care Plan 2Document30 pagesNursing Care Plan 2Shayla HudsonNo ratings yet
- Scizophrenia NCP1Document13 pagesScizophrenia NCP1Kholid Abu Mohammad AlfaizinNo ratings yet
- Psych NCPDocument4 pagesPsych NCPnoman-053No ratings yet
- Process Recording (PR) GuidelinesDocument2 pagesProcess Recording (PR) Guidelinesmrda9228No ratings yet
- NPI Reflects Spring 2013Document12 pagesNPI Reflects Spring 2013npinashvilleNo ratings yet
- CASE PRESENTATION PP - Anxiety. Tiffany GordonDocument6 pagesCASE PRESENTATION PP - Anxiety. Tiffany GordonTiffany GordonNo ratings yet
- Real PRDocument11 pagesReal PRapi-316378224No ratings yet
- Therapeutic Communication Assignment #1Document5 pagesTherapeutic Communication Assignment #1Jose R RomeroNo ratings yet
- Nur4140 Portfolio Final AnalysisDocument4 pagesNur4140 Portfolio Final Analysisapi-578141969No ratings yet
- Sample of Process Recording #2Document6 pagesSample of Process Recording #2David DueñasNo ratings yet
- Procedure of Insertion of A Intravenours CatheterDocument6 pagesProcedure of Insertion of A Intravenours CatheterSamantha FordNo ratings yet
- Peripheral IvsDocument17 pagesPeripheral IvsSamantha FordNo ratings yet
- NIDocument3 pagesNISamantha FordNo ratings yet
- PsychDocument6 pagesPsychSamantha FordNo ratings yet
- 2015 - Two Baselines Are Better Than One - Improving The Reliability of Computerized Testing in Sports NeuropsychologyDocument8 pages2015 - Two Baselines Are Better Than One - Improving The Reliability of Computerized Testing in Sports NeuropsychologyRaúl VerdugoNo ratings yet
- Body ShamingDocument1 pageBody ShamingAisen Denniel Neri100% (1)
- Interests Personal GrowthDocument2 pagesInterests Personal Growthapi-454337397No ratings yet
- Local Media6510953892956275898Document38 pagesLocal Media6510953892956275898danilo jr siquigNo ratings yet
- CISD ModelDocument27 pagesCISD Modelmary grace bana100% (1)
- Essay 1Document3 pagesEssay 1James SowNo ratings yet
- Principles of Management: Dr. A. Rashid KausarDocument30 pagesPrinciples of Management: Dr. A. Rashid KausarzrdNo ratings yet
- Shortcut To HeavenDocument14 pagesShortcut To HeavenAvneet SinghNo ratings yet
- Saving Our Planet - Criteria and RubricDocument3 pagesSaving Our Planet - Criteria and Rubricapi-284331957No ratings yet
- Social EntrepreneurshipDocument3 pagesSocial Entrepreneurshipjoan bonabonNo ratings yet
- Journal of Retailing and Consumer Services: Sheng-Fang Chou, Jeou-Shyan Horng, Chih-Hsing Sam Liu, Jun-You LinDocument11 pagesJournal of Retailing and Consumer Services: Sheng-Fang Chou, Jeou-Shyan Horng, Chih-Hsing Sam Liu, Jun-You Lindwi asriNo ratings yet
- AUNLP - All Course Competencies & SkillsDocument8 pagesAUNLP - All Course Competencies & SkillsSteve-39No ratings yet
- Study Habits of Students Acads PerfDocument14 pagesStudy Habits of Students Acads PerfNashNo ratings yet
- Lang - Acq Constructivism Autria-SumagueDocument10 pagesLang - Acq Constructivism Autria-SumagueLorielyn AustriaNo ratings yet
- G6138321 SopheakNichhaiTheng AssignmentDocument2 pagesG6138321 SopheakNichhaiTheng AssignmentSopheak Ni ChhaiNo ratings yet
- Emergence of CultureDocument7 pagesEmergence of CultureGarriy ShteynbergNo ratings yet
- Understanding The Self Prelims ReviewerDocument10 pagesUnderstanding The Self Prelims ReviewerJesrel Joy Cael CredoNo ratings yet
- THC6 - Module1Document7 pagesTHC6 - Module1Neil CutterNo ratings yet
- ESL 220 Alhaida Sarahan L1Document25 pagesESL 220 Alhaida Sarahan L1Rhoze Vhee ReddCapricorn SabillanoNo ratings yet
- Principles of HR ManagementDocument27 pagesPrinciples of HR ManagementtesfalemNo ratings yet
- Cardiac Depression Scale 26 Items - Hare 1993Document3 pagesCardiac Depression Scale 26 Items - Hare 1993TRIPTI RANINo ratings yet
- Makerere University Business School Bachelor of Entreprenuership and Small Business Management Human Behavior at Work Course Work 2Document10 pagesMakerere University Business School Bachelor of Entreprenuership and Small Business Management Human Behavior at Work Course Work 2asdddadaweeewerNo ratings yet
- Educ 38 Sir Acoriba ExercisesDocument17 pagesEduc 38 Sir Acoriba ExercisesRenalyn Samuya Jardio100% (1)