Professional Documents
Culture Documents
Kanker FIBROKISTIK
Uploaded by
Sitti RahmadaniOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Kanker FIBROKISTIK
Uploaded by
Sitti RahmadaniCopyright:
Available Formats
What are fibrocystic breasts? Fibrocystic breasts are characterized by lumpiness and usually discomfort in one or both breasts.
The condition is very common and benign, meaning that fibrocystic breasts are not malignant (cancerous). Fibrocystic breast disease (FBD), now referred to as fibrocystic changes or fibrocystic breast condition, is the most common cause of "lumpy breasts" in women and affects more than 60% of women. The condition primarily affects women between the ages of 30 and 50 and tends to become less of a problem after menopause. The diagnosis of fibrocystic breasts is complicated by the fact that the condition can vary widely in its severity. In some women, the symptoms of fibrocystic breast condition can be very mild with minimal breast tenderness or pain. The symptoms can also be limited in time, usually occurring only premenstrually. It may not even be possible to feel any lumps when the breasts are examined by the woman herself or by her doctor. In other women with fibrocystic breasts, the pain and tenderness are constant, and many lumpy or nodular areas can be felt throughout both breasts. Is there a difference between fibrocystic breast condition and fibrocystic breast disease? No. In the past, fibrocystic breast condition was often called fibrocystic breast disease. However, it is not a disease, but a condition. Most women tend to have some lumpiness in their breasts. Therefore, it is now being more appropriately termed fibrocystic breast condition. The abbreviation is FCC (an acronym derived from FibroCystic breast Condition). Other names that have been applied to fibrocystic breast condition include mammary dysplasia, chronic cystic mastitis, diffuse cystic mastopathy, and benign breast disease (a term that includes other benign breast disorders, including infections). What causes fibrocystic breasts? Fibrocystic breast condition involves the glandular breast tissue. The sole known biologic function of these glands is the production, or secretion, of milk. Occupying a major portion of the breast, the glandular tissue is surrounded by fatty tissue and support elements. The glandular tissue is composed of different types of cells: (1) clusters of secretory cells (cells that produce milk) that are connected to the milk ducts (tiny tubes); and (2) the cells that line the surfaces of the secretory cells, called the epithelial cells. The most significant contributing factor to fibrocystic breast condition is a woman's normal hormonal variation during her monthly cycle. Many hormonal changes occur as a woman's body prepares each month for a possible pregnancy. The most important of these hormones are estrogen and progesterone. These two hormones directly affect the breast tissues by causing cells to grow and multiply. Many hormones aside from estrogen and progesterone also play an important role in causing fibrocystic breasts. Prolactin, growth factor, insulin, and thyroid hormone are some of the other major hormones that are produced outside of the breast tissue, yet act in important ways on the breast. In addition, the breast itself produces hormonal products from its glandular and fat cells. Signals that are released from these hormonal products are sent to neighboring breast cells. The signals from these hormone-like factors may, in fact, be the key contributors to the symptoms of fibrocystic breast condition. These substances may also enhance the effects of estrogen and progesterone and vice versa. The same cyclical hormones that prepare the glandular tissue in the breast for the possibility of milk production (lactation) are also responsible for a woman's menstrual period. However, there is a major difference between what happens in the breast and uterus. In the uterus (the womb), these hormones promote the growth and multiplication of the cells lining the
uterus. If pregnancy does not occur, this uterine lining is sloughed off and discharged from a woman's body during menstruation. In the breast, these same hormones stimulate the growth of breast glandular tissue and increase the activity of blood vessels, cell metabolism, and supporting tissue. All this activity may contribute to the feeling of breast fullness and fluid retention that women commonly experience before their menstrual period. When the monthly cycle is over, however, these stimulated breast cells cannot simply slough away and pass out of the body like the lining of the uterus. Instead, many of these breast cells undergo a process of programmed cell death, called apoptosis. During apoptosis, enzymes are activated that start digesting cells from within. These cells break down and the resulting cellular fragments are then further broken down by scavenger cells (inflammatory cells) and nearby glandular cells. During this process, the fragments of broken cells and the inflammation may lead to scarring (fibrosis) that damages the ducts and the clusters (lobules) of glandular tissue within the breast. The inflammatory cells and some of the breakdown fragments may release hormone-like substances that in turn act on the nearby glandular, ductal, and structural support cells. The amount of cellular breakdown products, the degree of inflammation, and the efficiency of the cellular cleanup process in the breast vary from woman to woman. These factors may also fluctuate from month to month in an individual woman. They may even vary in different areas of the same breast in a woman. Which women are more likely to develop fibrocystic breast condition? Fibrocystic breast condition is said to primarily affect women age 30 and older. The reason for this is that the condition likely results from a cumulative process of repeated monthly hormonal cycles and the accumulation of fluid, cells, and cellular debris within the breast. The process starts with puberty and continues through menopause. After menopause, fibrocystic breast condition becomes less of a problem. Can fibrositic breast condition affect just one breast? Not usually. As a rule, fibrocystic breast condition tends to be symmetrical (bilateral) and affects both breasts. A woman can have more fibrocystic involvement in one breast than in the other. The less affected breast, however, often "catches up" over the years, and eventually both breasts become almost equally fibrocystic. Why is it important to diagnosis fibrocystic breasts? The basic problem with fibrocystic breast condition is the threat of breast cancer. Fibrocystic breast condition is itself benign (non-cancerous) and exceedingly common. Additionally, breast cancer is a common malignancy in women. Both conditions, one benign and the other a leading cause of cancer deaths in women, involve the same organ the breast. Fibrocystic lumps in the breast can closely mimic those found in breast cancer. They can also sometimes make breast cancer difficult to detect. Therefore, fibrocystic breast condition often makes both the patient and her physician quite concerned about the possibility of breast cancer. If a woman's breasts are fibrocystic, additional diagnostic tests may be necessary in order to rule out an underlying breast cancer. How is fibrocystic breast condition diagnosed? A common indicator of fibrocystic breast condition is breast pain or discomfort, but women with fibrocystic breasts may also not have any symptoms. If discomfort is present, the discomfort may
include a dull, heavy pain in the breasts, breast tenderness, nipple itching, and/or a feeling of fullness in the breasts. These symptoms may be persistent or intermittent (coming and going), especially appearing at the onset of each menstrual period and going away immediately afterwards. The primary method of diagnosing fibrocystic breast condition is physically touching and feeling (palpation) the lumpy areas in the breast(s). These lumps may be detected by a woman on selfexamination or by her physician. This lumpiness is most commonly found in the upper outer quadrant of the breast. (The breast is conventionally divided into quadrants or quarters. The upper outer quadrant is the one closest to the armpit.) The lumps in fibrocystic breast condition are typically mobile (they are not anchored to overlying or underlying tissue). They usually feel rounded, have smooth borders, and may feel rubbery or somewhat changeable in shape. Sometimes, the fibrocystic areas may feel irregular, ridge-like, or like tiny beads. These characteristics all vary from one woman to another. Breasts that are extremely fibrocystic can be very difficult to examine by palpation (touching and feeling). Even mammograms of such extremely fibrocystic breasts may be difficult to interpret. In these cases, specialized breast ultrasound exams and other tests can be very helpful. It may sometimes be necessary to obtain a sample (biopsy) of breast tissue with a needle or by surgery in order to make an accurate diagnosis and differentiate between fibrocystic breast condition and breast cancer. s there more than one type of fibrocystic breast condition? Yes. When biopsies (samples) of breast tissue are studied under the microscope, it is possible to identify different types of fibrocystic breast condition. Some cases of fibrocystic breast condition show little disturbance of the breast tissue. Other cases involve a large number of cysts, along with fibrous (scar) tissue, in the breast tissue. Additionally, in some cases of fibrocystic breast condition, the breast cells do not have a normal appearance. Cysts and fibrosis: Usually, even when the breast is not stimulated to produce milk, some secretions are produced by the secretory glandular cells. These secretions are normally reabsorbed "downstream" in the ducts. However, when there has been tissue damage and scarring (fibrosis) in the breast, these secretions may be trapped in the glandular portions of the breasts, thereby leading to the formation of fluid-filled sacs called cysts. In some areas of the breasts, there may be excessive fluid secretions due to stimulation by hormone-like substances. The resulting cysts may remain microscopic or enlarge until they contain several teaspoons or even tablespoons of fluid. These larger cysts may be felt as palpable (capable of being detected by touching) breast lumps. Even microscopic cysts may sometimes be felt as palpable lumps if many cysts are clustered together and there is a buildup of fibrous (scar) tissue around the cysts. Hyperplasia and atypical hyperplasia of breast cells: With repeated stimulation from normal hormones, and possibly the effects of many of the hormone-like substances produced in the breast, a few of the epithelial cells (cells that line the ducts in the breast) may eventually lose some of their genetic controls, which normally limit their multiplication (cell division). When this happens, cells may proliferate, leading to an abnormal architectural pattern of the epithelial cells. This over-proliferation of cells is termed hyperplasia. Sometimes these proliferating cells begin to appear abnormal and to look different from one another. They are now described as "atypical." As other more normal cells continue to cycle, die and break down, these atypical cells can move in, spread out, and accumulate. This extensive overgrowth and accumulation of atypical cells is called atypical hyperplasia. Why can fibrocystic breast condition be associated with an increased risk of breast cancer? Fibrocystic breast condition that involves hyperplasia is associated with a slightly elevated risk of breast cancer, and atypical hyperplasia is associated with a moderately increased risk of breast cancer when compared to women without fibrocystic changes. This is because genetic errors (mutations) have
begun to accumulate in cells that no longer respond normally to the signals that usually control cell growth and division. These cells may also have an impaired ability to repair any genetic damage. As the atypical cells increase in number, they accumulate additional genetic errors. Environmental, dietary, and metabolic toxins may also interact with a woman's complex hormonal system to increase the risk of mutations and thus increase the risk of breast cancer. It has been demonstrated that individuals differ significantly in their ability to break down and remove toxins from the body. Some of this varied response to toxins may be due to inherited differences. The potential for DNA damage (leading to genetic errors or mutations), which can be caused by a variety of damaging agents combined with the stimulation of cell division, is what ultimately leads to the risk of breast cancer that is associated with some cases of fibrocystic breast condition; the ability to recognize and repair DNA damage, a process that cells must continuously perform, varies from person to person. Why don't all women with fibrocystic breast condition have breast biopsies? One reason to undergo a breast biopsy is to diagnose breast cancer. Another reason is to identify those women with fibrocystic breast condition who are at an increased risk of developing breast cancer in the future. However, the severity of a woman's symptoms and clinical signs of fibrocystic breast condition (pain and lumpiness) do not necessarily correlate with the cellular findings under the microscope. Therefore, it is difficult to single out every woman with fibrocystic breast condition for whom a breast biopsy would be useful. Additional reasons why breast biopsies are not done on every woman with fibrocystic breast condition include: (1) the invasive nature of the biopsy procedure; (2) the necessity of anesthesia; and (3) costbenefit considerations. Instead, most women with fibrocystic breast condition are followed over time as if they all are at an increased risk for developing breast cancer. The woman herself must ensure that her clinician is appropriately monitoring her on a regular basis. What are the treatments for fibrocystic breast condition? The treatments for fibrocystic breast condition are directed at the individual components of the condition, including the relief of symptoms (such as breast pain and tenderness) and the correction of hormonal irregularities: 1. Relief of symptoms: Some simple measures, such as adequate support of the breasts and perhaps wearing a bra at night, may provide relief from many of the symptoms of fibrocystic breast condition. Antiinflammatory medications, including acetaminophen and nonsteroidal antiinflammatory medications (NSAIDs), often reduce the breast pain significantly. There are reports suggesting that a variety of vitamins may be of benefit in relieving the symptoms of fibrocystic breast condition. These have included vitamin C, vitamin E, vitamin B6 and vitamin A, among others. In general, the rationale for using these vitamins is unclear and is not based on duplicated, controlled clinical studies. The exception may be vitamin E where, at least in some studies, there appears to be a measurable benefit for some patients. Another food supplement that has been claimed to be of some benefit in clinical studies is Oil of Primrose. This substance contains certain essential fatty acids that allegedly benefit some fibrocystic breast condition patients by reducing their breast pain. There is no scientific evidence showing any correction (resolution) of the microscopic cellular abnormalities with use of this substance. 2. Hormonal irregularities: Some women with very irregular menstrual cycles seem to
progressively suffer more severe fibrocystic breast condition. This tendency is most likely due to the prolonged and irregular hormonal stimulation of the breasts. In these patients, it is sometimes helpful to establish menstrual cycle regularity with oral contraceptives. Regular cycles seem to allow the breast tissue to recover more completely at the end of each menstrual cycle. In patients who have had a hysterectomy and who are on hormone therapy, it may be helpful to be "off estrogen" for five days during each monthly cycle rather than remain on continuous estrogen. Again, this schedule is designed to avoid the continuous stimulation of the breast tissues by estrogen. It is important that any such hormone regulation be under the direct supervision of a physician. Certain common hormonal (endocrine) abnormalities, such as diabetes or thyroid dysfunction, may contribute to fibrocystic breast condition. Since these conditions may aggravate the symptoms of fibrocystic breast condition, they should be diagnosed and treated. 3. Studies have shown some benefit from the short term use of the antiestrogenic drug Tamoxifen in relieving breast pain. However, tamoxifen use may be associated with a number of adverse effects, especially in postmenopausal women, and its use should be limited to the short term. Likewise, the androgenic steroid drug danazol (Danocrine) has also been shown to reduce breast pain and nodule size in women with fibrocystic breast condition. Danazol is also associated with a number of side effects. Both of these medications may be considered for use in women with severe cyclical breast pain due to fibrocystic condition. Are there any dietary or life style factors associated with fibrocystic breast condition? Caffeine has been implicated as contributing to both the symptoms and scarring (fibrocystic) changes in fibrocystic breast condition. However, when the scientific evidence is reviewed, the results are conflicting, and no firm benefit of caffeine restriction can be scientifically established. Additionally, there appears to be no evidence that caffeine increases the risk of breast cancer. However, in women with fibrocystic breast condition, it might still be worth a trial of caffeine restriction. (Note that coffee is not the only source of caffeine. Tea, chocolate, and certain soft drinks also contain caffeine.) There is no harm in trying caffeine avoidance, and there may be a few fibrocystic breast condition patients for whom it is beneficial. At this time, there is a great deal of circumstantial evidence that dietary and hormonal factors can affect fibrocystic breast condition and its associated risk of breast cancer. Still, a firm association between dietary factors and fibrocystic breast condition has not been establishe
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Anesthesiology MnemonicsDocument1 pageAnesthesiology MnemonicsMartin Susanto, MD100% (3)
- Daftar PustakaDocument1 pageDaftar PustakaSitti RahmadaniNo ratings yet
- Daftar Pustaka P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document1 pageDaftar Pustaka P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Sitti RahmadaniNo ratings yet
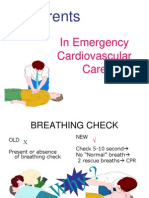
- Currents: in Emergency Cardiovascular CareDocument16 pagesCurrents: in Emergency Cardiovascular CareSitti RahmadaniNo ratings yet
- Renal Tissue Oxygenation in Essential HypertensionDocument8 pagesRenal Tissue Oxygenation in Essential HypertensionSitti RahmadaniNo ratings yet
- Special SenseDocument85 pagesSpecial SenseSitti RahmadaniNo ratings yet
- Dasar Biolistrik Ekg: Ilhamjaya PatellongiDocument25 pagesDasar Biolistrik Ekg: Ilhamjaya PatellongiSitti RahmadaniNo ratings yet
- Brain Neuroscience and LearningDocument42 pagesBrain Neuroscience and LearningSitti Rahmadani100% (3)
- Esophageal AhalasiaDocument6 pagesEsophageal AhalasiaSitti RahmadaniNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale Evaluation SubjectiveDocument1 pageAssessment Diagnosis Planning Implementation Rationale Evaluation SubjectiveKryza CastilloNo ratings yet
- Finalrationale CAGABCABDocument9 pagesFinalrationale CAGABCABCagabcab Canibel MelanyNo ratings yet
- English DialogueDocument3 pagesEnglish DialogueAnonymous ZL7WvYNo ratings yet
- Quality Form BDocument10 pagesQuality Form BFranz ToledoNo ratings yet
- Post Partum HemorrhageDocument18 pagesPost Partum Hemorrhageeric100% (1)
- Week 10Document2 pagesWeek 10mandok25No ratings yet
- High Risk Newborn Conditions Present at BirthDocument47 pagesHigh Risk Newborn Conditions Present at BirthChinchu ChinchuNo ratings yet
- mySinusitisCoach - Patient Empowerment in Chronic Rhinosinusitis Using Mobile TechnologyDocument7 pagesmySinusitisCoach - Patient Empowerment in Chronic Rhinosinusitis Using Mobile TechnologyMRMISSYNo ratings yet
- Ulkus VarricosumDocument26 pagesUlkus VarricosumNurul FadilahNo ratings yet
- Needle Stick InjuriesDocument1 pageNeedle Stick InjuriesAgnes BNo ratings yet
- Biological Properties of Lemongrass An OverviewDocument1 pageBiological Properties of Lemongrass An OverviewLilia RotariNo ratings yet
- Somatoform Disorders - Nursing AssessmentDocument15 pagesSomatoform Disorders - Nursing AssessmentPinkRose BrownSpiceNo ratings yet
- A Study On FNHW Interventions - K. ChaitanyaDocument63 pagesA Study On FNHW Interventions - K. ChaitanyaChaitanya KNo ratings yet
- Christian Rupal's ResumeDocument2 pagesChristian Rupal's ResumesaumiljoshilondonNo ratings yet
- 7 Doh Approved Herbal Medicine: Pictures Indicataion Contraindication Nursing ResponsibilityDocument5 pages7 Doh Approved Herbal Medicine: Pictures Indicataion Contraindication Nursing ResponsibilityShaira Ann CalambaNo ratings yet
- Psychosocial Rehabilitation 1Document2 pagesPsychosocial Rehabilitation 1Prakriti Kohli0% (1)
- Diabetes Advisor - A Medical Expert System For Diabetes ManagementDocument5 pagesDiabetes Advisor - A Medical Expert System For Diabetes ManagementPrincess LunieNo ratings yet
- Makalah HypertensionDocument6 pagesMakalah HypertensionFatin ZafirahNo ratings yet
- OB GyneDocument2 pagesOB GyneDragonviewerNo ratings yet
- Dental Traumatic InjuriesDocument152 pagesDental Traumatic InjuriesnishthaNo ratings yet
- Application of Upshur's Ethical Principles in Public Health Activities During The PandemicDocument4 pagesApplication of Upshur's Ethical Principles in Public Health Activities During The PandemicBinu KumarNo ratings yet
- AlexionDocument2 pagesAlexionLiz HartNo ratings yet
- Substance UseDocument3 pagesSubstance UseAlbert SamanteNo ratings yet
- Somatization DisorderDocument3 pagesSomatization DisorderVinceNo ratings yet
- Emily Morgan - ResumeDocument2 pagesEmily Morgan - Resumeapi-283578734No ratings yet
- Implant ArticleDocument20 pagesImplant ArticleArun PrasadNo ratings yet
- Fhap Family Summary: Group MembersDocument5 pagesFhap Family Summary: Group MembersJacob JrNo ratings yet
- Good Personal Hygiene Is Key To The Prevention of Foodborne Illness. Good Personal Hygiene IncludesDocument3 pagesGood Personal Hygiene Is Key To The Prevention of Foodborne Illness. Good Personal Hygiene IncludesKatrina BaluyutNo ratings yet
- Nebulizer Therapy PitfallsDocument8 pagesNebulizer Therapy PitfallskemalahmadNo ratings yet