Professional Documents
Culture Documents
Part3-B BLS
Uploaded by
Umar AhmatOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Part3-B BLS
Uploaded by
Umar AhmatCopyright:
Available Formats
1
TraumaticBrainInjuryModule forDSHS
GilesGifford,EMT MonicaS.Vavilala,MD
BLSprovidercourse
TBIEpidemiology:Nationally
Yearly1.7millionpeoplesustainTraumaticBrain Injury,(TBI) ~1.36millionaretreatedinEDanddischarged. 275,000arehospitalized 80,000to90,000aredisabled 52,000die Today,5.3millionAmericans(~2%)arelivingwithTBI relateddisabilityand~1%ofpeoplewithsevereTBIsurvive inapersistentvegetativestate In2000,theestimatedlifetimedirectmedicalcostsand indirectcosts(suchaslossoflifelongproductivity)fromTBI amountedto60billiondollars
TBIEpidemiology:WAState
Population; 6,664,195 - Jul 2009 Source: U.S. Census Bureau
TBI~10%ofallinjuryrelatedhospitalizations TBIdeathsareabout29%ofallinjuryrelatedfatalities Nearly123,750residentswithTBIrelateddisabilities ~26,000residentshadTBI(20052009) ~5,500hospitalizationsand1,300deaths/year(20022006)
YouwillseeTBIpatientsinyourcareer
WAEpidemiology:TBICauses
From20032007,falls,beingstruckbyanobject,andmotorvehiclerelatedTBIinjuries madeabout90%ofallTBIrelatedhospitalizationsandfalls,firearmsandmotorvehicle relatedinjuriesmadeabout91%ofTBIdeaths.
WAEpidemiology:TBIHospitalizationsbyCause
TBIHospitalizationsduetotransportinjuriesofvarioustypesfellintheearlyyears, andthenplateaued.Fallsincreasedsincethelate1990s,explainingtheoverallrise inTBIHospitalizations.TBIhospitalizationsbyfirearminjury remainslowdueto thelowsurvivalratefromtheinitialinjury.
WAEpidemiology:ElderlyFallRelatedTBI
TBIrelatedhospitalizationsanddeathswillsteadily increaseoverthenextfewdecadesasthebabyboom generation(thosebornfrom1946to1964)steadilyages 1 in3 adultsage65+fallseachyear 1 in2 adultsage80+fallseachyear 1 outof5 fallscausesaseriousinjurysuchasahead trauma(TBI)orfracture Only1in 5 peoplewhoarehospitalizedforfallsever returnhome
WAEpidemiology:TBIHospitalizationsbyAge
WhoisatRisk? Elderly Age1524years Malegender
TraumaticBrainInjury(TBI)
Injuriestothebraincausedbyphysicaltraumatothehead. Canbepenetratingorbluntforceinjury Twoformsofinjury Primary Directtraumatobrainandvascularstructures Examples:contusions,hemorrhages,andotherdirect mechanicalinjurytobraincontents(brain,CSF,blood). Secondary Ongoingpathophysiologicprocessescontinuetoinjure brainforweeksafterTBI PrimaryfocusinTBImanagementistoidentifyand limitorstopsecondaryinjurymechanisms
SecondaryInjury
AfterinitialTBI,prioritiesare: Identificationofsecondaryinsults Intracranialhypertension fromexpandingintracranial hematoma/brainswellingresultsinelevated intracranialpressure(ICP)and/orherniation Hypoxia fromventillatory/circulatoryfailure,airway obstruction,apnea,lunginjury,aspiration Hypotension associatedspinalcordinjury,bloodloss Inadequatecerebralbloodflowcancauseinadequate oxygenandglucosedelivery Hypercarbia frominadequateventilation,apnea Rapidtransporttoacapablehealthcarefacility
10
SignsandSymptoms
Signs
diminishedconsciousness convulsionsorseizures dilationofoneorbothpupils slurredspeech repeatedvomitingornausea increasingconfusion, restlessness,oragitation
Symptoms
headache blurredvision ringingintheear badtasteinthemouth weaknessornumbnessin extremities lossofcoordination dizziness/lightheadedness
11
SceneAwareness
Includethefollowinginthepatientcarereport: Kinematicsleadinguptotheinjury MVC speed,restraints,intrusion,helmet Assault headvs.object,repeatassault? Sportsrelated bodyposition,speedatimpact WitnessaccountofPatientBehaviorafterInjury LOC,slurredspeech,inappropriatebehavior,duration
12
Documentation
Completedocumentationcouldhaveapositiveimpact throughoutaTBIpatientslife DiagnosisandTreatmentaftertheinjurymaydependon thoroughnessofPCR Includeeventsoccurringpreandpostinjuryandbefore EMSarrival Ensureasuccessfulhandoffoftherunsheettothepatient careprovidersintheED. AfterobtainingsignatureensureacopyofthePCRis includedinthepatientchart
13
Documentation
Specificitemstodocumentinclude: MechanismofInjury/LOC? Primarysymptoms/associatedsymptoms Serialvitalsigns HR,BP,RR ComponentGCSandPupils Procedurespreformed Transportationdecisions
14
Assessment:Overview
Airway:
Priorities
Breathing:
Oxygenation Hypoxemia
Circulation:
Hypotension Shock Glasgow Coma Scale (GCS): Priorities Patient Interaction Components Motor Component Score Pupils: Value Pathophysiology Abnormalities Cerebral Herniation:
Indicators
15
Airway:Priorities
Determinethatairwayisopenandmaintainpatency Assessneedforartificialairway ForBLSproviders,isaMedicevaluationneeded? Reassessevery5minutesandasneeded Maintaincervicalspineprecautions Usecervicalcollarduringtransport
16
Breathing:Oxygenation
Assessrate,rhythm,depth,quality,andeffectivenessof ventilation(movementofairinandoutofthelungs)every5 minutesandasneeded IfpossibleusecontinuousSpO2 monitoring Avoidinadvertenthyperventilation IfnoSpO2 monitoringlookforapneaandslow/irregular breathingtoindicateadequatetissueoxygenationandcarbon dioxideremovallevels
17
Breathing:Hypoxemia
Assessandmonitorforhypoxemia(SpO2<90%) Occursin40%ofTBIcases Ifpulseoximetrynotavailable,observepatientforindirect signsofhypoxia PotentialSignsandSymptomsofHypoxia: Blueorduskymucusmembranes Impairedjudgment Confusion,delirium,agitation Decreasedlevelofconsciousness Tachycardiaheartrate>100beatsperminuteforadult Cyanosisoffingernailsandlips Tachypnea Atorabove20breathsperminuteforadult
18
Circulation:Hypotension
Monitorforhypotension inadequatecerebralbloodflowcan causeinadequateoxygenandglucosedelivery
Adulthypotension,systolicbloodpressure(SBP)<90mmHg
Monitorforhypertension mayindicateraisedICPwhen associatedwithbradycardiaandirregularrespiration Usecorrectcuffsizetomeasuresystolicanddiastolicblood pressure Cufftoosmall(falsehighornormal),toolarge(falselow) AssessSBPevery5minutes Continuousmonitoringifpossible
19
Circulation:Shock
Itisveryimportanttorecognizethesignsandsymptomsof shockanditissomethingthateveryEMSprovidercando SignsandSymptomsofShock:
Skincyanosis,pallor Restlessness,anxiety,changeinlevelofconsciousness Tachycardia rapidheartrate,greaterthan100beatsperminuet Tachypnea rapid,shallowrespiratoryrate Narrowedpulsepressure reductionintherangebetweenthe systolicanddiastolicbloodpressure Coolextremities Hypotension SBP<90mmHg
Ifspinalshockisassociatedpatientmaybehypotensive withbradycardia
20
GlasgowComaScale(GCS):Priorities
GCSpreferredmethodtodeterminelevelofconsciousness AVPU(Alert,Verbal,Pain,Unresponsive)istoosimpleto determineLOC¬quantifiable FollowABCsbeforemeasuringGCS Ifpossible,assessGCSpriortointubation MeasureGCSbeforeadministeringsedativeorparalytic agents,orafterthesedrugshavebeenmetabolized ReassessandrecordGCSevery5minutes
21
GCS:PatientInteraction
GCSobtainedbydirectpatientinteraction Prehospitalprovidermustaskdirectquestionsand performspecificactionsforaccurateGCSscore Donotsimplysaysqueezemyhands (reflexive) Insteadsayshowmetwofingers TheEMTneedstoillicitaresponsethatdemonstrates cognition,ortheabilityofthepatienttothink Ifeyeopeningdoesnotoccurtovoice,useaxillarypinch orfingernailbedpressure
22
GCS: Components
GCSshouldbemeasuredbyprehospitalproviderswho areappropriatelytrained
GCS 14-15: Mild TBI
GCS 9-13: Moderate TBI
GCS 3-8: Severe TBI
23
GCS:MotorComponent
ImportantpartofGCS Motorresponsewasdesignedtolooka thebestupperextremityresponse Spinalcordinjury,chemicalparalysis orexcessivepainmakesmotor assessmentimpossible Abnormalposturing(decerebration& decortication)looksimilarinthelower extremities Motor Response
6- Obeys 5- Localizes-(purposeful movements towards painful stimuli) 4-Withdraws from pain 3 Abnormal flexion - Image A 2-Abnormal extension - Image B 1-No response
A: Abnormal flexion (decorticate rigidity)
B: Extension posturing (decerebrate rigidity)
24
GCS:Value
GCSprovidesbasisfordeterminingthemethodof transportandthepreferredreceivingfacility Comparetopreviousscorestoidentifytrendovertime Asinglefieldmeasurementcannotpredictoutcome RepeatedGCSscorescanbevaluabletoEDstaff Deteriorationof> 2pointsisabadsign GCS<9indicatesapatientwithasevereTBIand requiretrachealintubation
25
Pupils:Value
Pupillarysizeandtheirreactiontolightshouldbeusedin thefieldasitcanbehelpfulindiagnosis,treatmentand prognosis Afixedanddilatedpupilisawarningsignandcan indicateandimpendingcerebralherniation Pupillarysizeshouldbemeasuredafterthepatienthas beenstabilized
26
Pupils:Pathophysiology
Whydopupilsdilate?
Thepresenceofintracranialhematoma cancausedownwarddisplacementof thebrain,untilitputspressureonthecranialnerveresponsibleforpupil dilation
Othercausesofabnormalpupils:
Hypoxia Hypotension Druguse(opiates) Hypothermia ToxicExposure Artificialeye Orbitaltrauma Congenitalabnormality Pharmacologicaltreatment,CataractSurgery (e.g.Atropine)
27
Pupils:Abnormalities
Unequalordilatedandunreactive suspectbrainherniation Unilateralorbilateralpupils
(asymmetricpupilsdiffer>1mm)
Dilatedpupils
(dilationmorethanorequalto4mm)
Fixedpupils
(fixedpupillessthan1mmchangein responsetobrightlight)
Evidenceoforbitaltraumashouldberecorded
28
CerebralHerniation:Indicators
Unresponsivepatient(noeyeopeningorverbalresponse) Unilaterallyorbilaterallydilatedorasymmetricpupils Abnormalextension(decerebrateposturing) Nomotorresponsetopainfulstimuli Deterioratingneurologicexamination,bradycardia(heart rate<60bpm),andhypertensionshouldbeviewedasa partofCushingsresponseandimpliesimpending herniation CushingsTriad(Reflex)isaLATEsignofherniation: ElevatedsystolicBP Bradycardia Irregularrespirations
29
AdditionalConsiderations
Patients with other illness/injury can have signs and symptoms similar to those of TBI ETOH / drug abuse Sports related injury / concussion Violence / domestic violence Has your partner hit or grabbed you are two questions EMT can ask to identify a possibly abusive situation Decreased mental status in the elderly
These patients can also have a TBI!
30
Treatment:Overview
Airway:
Priorities
Ventilation:
Priorities Hyperventilation
FluidResuscitation:
Priorities
CerebralHerniation:
SignsandSymptoms Hyperventilation AdditionalConsiderations
31
Airway:Priorities
ALS/Mediceval? Protectcervicalspinealignmentwithmanualinline stabilization,bewarefacialtrauma WhenairwaycannotbesecuredbyEndotrachealtube; consideralternateairwaydevices
Accordingtocountyprotocol
Providecombitubeorsupraglotticairwayifnotcertifiedto provideadvancedairwayadjuncts
Accordingtocountyprotocol
32
Ventilation:Priorities
Assessrate,rhythm,depth,andqualitytodeterminethe effectivenessofrespirations AssistventilationsasnecessarywithBagValveMaskand supplementalO2 ALS/Mediceval? Adult normalventilationrates:1012breathsperminute
33
Ventilation:Hyperventilation
Producesarapiddecreaseinarterial partialpressureofcarbondioxideandcauses cerebralvasoconstriction Decreasedcerebralbloodflow decreasedintracranialpressure(ICP) Hyperventilationisatemporarytreatmentusedonlyin patientsshowingsignsofherniationuntildefinitive diagnosticortherapeuticinterventionscanbeinitiated Hyperventilationratesage>9years:20BPM
34
FluidResuscitation:Priorities
ALS/Mediceval? Avoidhypotensionandinadequatevolumeresuscitation tomaintainnormotensionandadequatetissueperfusion Hypotension(SBP<90mmHg)doublesmortality
35
CerebralHerniation:Hyperventilation
Innormoventilated,normotensive,andwelloxygenated patientsstillshowingsignsofcerebralherniation, hyperventilationshouldbeusedasatemporizingmeasure andshouldbediscontinuedwhenclinicalsignsof herniationresolve
Rate 20BPMforadults(Every3seconds)
36
CerebralHerniation:Signs&Symptoms
SignsSymptoms
Dilatedorunreactivepupils Asymmetricpupils Amotorexamthatidentifieseither extensorposturingornoresponse Progressiveneurologicdeterioration, decreaseinGCSscoremorethan2 pointsfrompatientspriorbestscore in patientswithinitialGCS<9
OtherfactorsincreasingICP
Fearandanxiety Pain Vomiting Straining Environmentalstimuli Endotrachealintubation Airwaysuctioning
Frequently re-evaluate patient neurologic status
37
CerebralHerniation:AdditionalConsiderations
Ruleoutdecreasedlevelofconsciousnessdueto hypoglycemia Hypoglycemia bloodsugarbelow70mg/dL Performrapidbloodglucosedetermination Ifnecessary,giveIVglucose Followlocalprotocol
38
Transportdecisions: Priorities Priorities Receivingfacilities
39
TransportDecisions:Priorities
Minimizeprehospitaltimebyselectingappropriatemode oftransportation,rendezvouswithairmedicalserviceto decreaseenroutetimes Patientmayrequireemergentsurgeryforhematoma evacuation,earlytransportmustbetheprioritywhile resuscitationisongoing Ifnecessary,rendezvouswithairmedicalserviceto decreaseenroutetimes
40
TransportDecisions:Priorities
Allregionsshouldhaveanorganizedtraumacaresystem ProtocolsarerecommendedtodirectEMSregarding destinationdecisionsforpatientswithsevereTBI Improvedsuccessattributedtointegrationofprehospital andhospitalcareandaccesstoexpedioussurgery
41
TransportDecisions:Receivingfacilities
TransporttoappropriatereceivingfacilitybasedonGCS GCS14 15:HospitalEmergencyRoom GCS9 13:TraumaCenter GCS<9:TraumaCenterwithsevereTBIcapabilities PatientswithsevereTBIshouldbetransportedtoafacility withimmediatelyavailable: CTscanning Promptneurosurgicalcare TheabilitytomonitorICP Theabilitytotreatintracranialhypertension
42
References
[authorlastname,firstname],2007.GuidelinesforPrehospitalManagementof SevereTraumaticBrainInjury,secondedition,BrainTraumaFoundation,. NationalAssociationofEmergencyMedicalTechnicians(NAEMT),2011. PHTLS:PrehospitalTraumaLifeSupport,7thed.,ElsevierHealthSciences, Chap9. Shorter,Zeynep,2009.TraumaticBrainInjury:Prevalence,ExternalCauses, andAssociatedRiskFactors,WashingtonStateDepartmentofHealth, http://www.doh.wa.gov/hsqa/ocrh/har/TBIfact.pdf (April1,2011) U.S.CentersforDiseaseControlandPrevention,2011.InjuryPrevention& Control:TraumaticBrainInjury,http://www.cdc.gov/traumaticbraininjury/ (May1,2011)
43
Acknowledgements
MikeLopez,EMS/TraumaSupervisor;WashingtonStateDept.of Health MikeRoutley,EMSSpecialist/Liaison,WashingtonStateDept.of Health DeborahCrawley,ExecutiveDirectorandstaff, BrainInjuryAssociationofWashington WashingtonStateEMTsparticipatinginfocusgroupsandphone interviews. Peerreview:AndreasGrabinsky,MD,ArmaganDagal,MD,Deepak Sharma,MD,EricSmithEMTP,DaveSkolnickEMTB,RichardVisser EMTB
You might also like
- The Complete Hematopathology GuideDocument113 pagesThe Complete Hematopathology GuideJenny SNo ratings yet
- C Post Concussion ChecklistDocument1 pageC Post Concussion Checklistalston96No ratings yet
- Saving Lives Through Trauma CareDocument60 pagesSaving Lives Through Trauma CareSweetcharmed GoNo ratings yet
- Medical Emergencies in The Dental OfficeDocument100 pagesMedical Emergencies in The Dental OfficeSaleh Ahmed Saleh Ahmed100% (1)
- 16.00 DR Neil Baldwin, Management of StrokeDocument57 pages16.00 DR Neil Baldwin, Management of Strokeamir ahmadNo ratings yet
- Pathology Outlines - Papillary Carcinoma - GeneralDocument6 pagesPathology Outlines - Papillary Carcinoma - Generalpatka1rNo ratings yet
- Depression and Anxiety Among College StudentsDocument2 pagesDepression and Anxiety Among College StudentsAnonymous 5WUUQijWNo ratings yet
- Mnol Nihss CertificateDocument1 pageMnol Nihss Certificateapi-3647224180% (1)
- ALSBLS PPT FinalDocument64 pagesALSBLS PPT FinalIbnu Fadirul WahedNo ratings yet
- NeuroemDocument51 pagesNeuroemJameston BostreNo ratings yet
- Acute Lymphoblastic LeukemiaDocument20 pagesAcute Lymphoblastic LeukemiazahraaNo ratings yet
- Director &HOD Prof - Dr. K.PRAKASAM M.S.Ortho, D.Ortho, DSC (Hon)Document70 pagesDirector &HOD Prof - Dr. K.PRAKASAM M.S.Ortho, D.Ortho, DSC (Hon)vimalNo ratings yet
- Myocardial Infarction (Heart Attack) : by Rolly M. Policarpio RNDocument90 pagesMyocardial Infarction (Heart Attack) : by Rolly M. Policarpio RNThomas BenjaminNo ratings yet
- Pediatric Trauma AssessmentDocument36 pagesPediatric Trauma AssessmentAbdulrahman Y. SabbaghNo ratings yet
- Lake Country Medical Group ProjectDocument45 pagesLake Country Medical Group Projectapi-608668343No ratings yet
- Chronic Obstructive Pulmonary Disease: Martina S., Selda S., Sarah A.G., Dina H., Sonia C. UMFT Victor Babes'Document39 pagesChronic Obstructive Pulmonary Disease: Martina S., Selda S., Sarah A.G., Dina H., Sonia C. UMFT Victor Babes'Petcu FlorinaNo ratings yet
- The Golden Hour of Acute Ischemic StrokeDocument22 pagesThe Golden Hour of Acute Ischemic StrokeGiao MauNo ratings yet
- GRP 1 - Non Communicable DiseaseDocument121 pagesGRP 1 - Non Communicable Diseasepavitra pawan chandNo ratings yet
- Accupuncture On Stroke FK UNSDocument62 pagesAccupuncture On Stroke FK UNSdavidperdana100% (1)
- Heart Disease Causes, Symptoms & TreatmentDocument42 pagesHeart Disease Causes, Symptoms & TreatmentMuhammad ShahzadNo ratings yet
- Chronic Diseases 2. HaftaDocument42 pagesChronic Diseases 2. HaftaAHMAD SOAPNo ratings yet
- Management of Ischemic Stroke in Resource-Limited SettingsDocument34 pagesManagement of Ischemic Stroke in Resource-Limited SettingsericNo ratings yet
- Preoperative ManagmentDocument58 pagesPreoperative ManagmentYibeltalNo ratings yet
- Week 5 Respiratory EmergencyDocument61 pagesWeek 5 Respiratory EmergencyArmand Bong SantiagoNo ratings yet
- Sudden Unexpected Death in EpilepsyDocument22 pagesSudden Unexpected Death in EpilepsyYu Xiang LinNo ratings yet
- Ncd. StrokeDocument20 pagesNcd. StrokeM Zohaib Irshad AhmadNo ratings yet
- Coventry 06.2013Document12 pagesCoventry 06.2013karan270No ratings yet
- PERIOPERATIVE PRINCIPLES AND PRE-OP CAREDocument155 pagesPERIOPERATIVE PRINCIPLES AND PRE-OP CAREDaniel Lim100% (3)
- Ade AmiDocument48 pagesAde AmiignasachyntiaNo ratings yet
- Anaesthesia For Renal TransplantationDocument65 pagesAnaesthesia For Renal TransplantationSouvik MaitraNo ratings yet
- Nurses Need to Know About Stroke CareDocument68 pagesNurses Need to Know About Stroke CareSuci Aning TNo ratings yet
- Neurosurgical Emergencies: Craig Goldberg, MD Chief, Division of Neurosurgery Bassett HealthcareDocument44 pagesNeurosurgical Emergencies: Craig Goldberg, MD Chief, Division of Neurosurgery Bassett HealthcareTolaniNo ratings yet
- 2019 Enls For ApacvsnnnnnnDocument46 pages2019 Enls For ApacvsnnnnnnAhmed ElshewiNo ratings yet
- 5.TCC ZdrehusDocument61 pages5.TCC ZdrehusCristina TrofimovNo ratings yet
- Seminar ON Seizure: Presented To Presented byDocument35 pagesSeminar ON Seizure: Presented To Presented byShitaljit IromNo ratings yet
- Myocardial Infarction. BPTDocument62 pagesMyocardial Infarction. BPTAanchal GuptaNo ratings yet
- MOH Pocket Manual in Emergency MedicineDocument244 pagesMOH Pocket Manual in Emergency MedicineAli Al-Brahim (AlucardAli)No ratings yet
- Icu 2Document57 pagesIcu 2astewale tesfieNo ratings yet
- Case Presentation ETD (COPD)Document45 pagesCase Presentation ETD (COPD)Dzachary13No ratings yet
- Critical Thinking Exercise NCM 106Document5 pagesCritical Thinking Exercise NCM 106Julienne Sanchez-SalazarNo ratings yet
- Stroke Show Notes: Signs, Risks, ManagementDocument63 pagesStroke Show Notes: Signs, Risks, ManagementApriani MargastutieNo ratings yet
- Heartfailure 180328114636Document52 pagesHeartfailure 180328114636mira pNo ratings yet
- Case Study 2Document27 pagesCase Study 2Hal00mNo ratings yet
- StrokeDocument63 pagesStrokeBeny RiliantoNo ratings yet
- Azmi SyncopeDocument50 pagesAzmi Syncopezakiyyatul aflakhaNo ratings yet
- Diagnosing and Treating a Stroke PatientDocument10 pagesDiagnosing and Treating a Stroke PatientMary Therese Joy BaldozaNo ratings yet
- ACLS Review Guide for Cardiac Arrest Scenarios and TreatmentDocument29 pagesACLS Review Guide for Cardiac Arrest Scenarios and TreatmentJB Reyes100% (2)
- Virtual Clinical Prep For Cardiopulmonary ArrestDocument1 pageVirtual Clinical Prep For Cardiopulmonary ArrestBridgette RandolphNo ratings yet
- Basic Life Support PamphletDocument26 pagesBasic Life Support PamphletRex Loren de Leon0% (1)
- Initial Trauma MusculoskeletalDocument53 pagesInitial Trauma MusculoskeletalAnonymous wyBvCzkENo ratings yet
- Transient Ischemic Attack: A Case StudyDocument44 pagesTransient Ischemic Attack: A Case Studytinay100% (8)
- HypertensionDocument15 pagesHypertensionSusan GamalNo ratings yet
- Guillain Barre SyndromeDocument49 pagesGuillain Barre SyndromeDavid SugiartoNo ratings yet
- Farmakoterapi HD PDFDocument32 pagesFarmakoterapi HD PDFgampang lupaNo ratings yet
- MDH 2012 JLPascual Acute Stroke - Handout VersionDocument67 pagesMDH 2012 JLPascual Acute Stroke - Handout VersionJ Leonard PascualNo ratings yet
- 5D-Sepsis-3-CACCN-Dynamics-2018-FaganDocument43 pages5D-Sepsis-3-CACCN-Dynamics-2018-FaganBarry TraceyNo ratings yet
- Clinical Profile of Stroke Patients at CMCTHDocument31 pagesClinical Profile of Stroke Patients at CMCTHajNo ratings yet
- CBT Neurosurgery - TutorDocument24 pagesCBT Neurosurgery - Tutoramoody95No ratings yet
- BRAIN DEATH ROLE OF IntensivistDocument41 pagesBRAIN DEATH ROLE OF Intensivistharsha mummakaNo ratings yet
- Heart TransplationDocument20 pagesHeart Transplationbinojdaniel17No ratings yet
- Pediatric Trauma: Bagian Bedah FK-UA / RSUP DR. M. Djamil PadangDocument16 pagesPediatric Trauma: Bagian Bedah FK-UA / RSUP DR. M. Djamil PadangyeziNo ratings yet
- The Legend of Toba LakeDocument7 pagesThe Legend of Toba LakeUmar AhmatNo ratings yet
- NAMA PEMAIN POSISI HARGA UMUR KLUBDocument5 pagesNAMA PEMAIN POSISI HARGA UMUR KLUBUmar AhmatNo ratings yet
- Ch3 PULMONARY PHYSIOLOGIC TESTING PDFDocument20 pagesCh3 PULMONARY PHYSIOLOGIC TESTING PDFUmar AhmatNo ratings yet
- NAMA PEMAIN POSISI HARGA UMUR KLUBDocument5 pagesNAMA PEMAIN POSISI HARGA UMUR KLUBUmar AhmatNo ratings yet
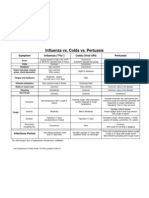
- Flu Colds PertussisDocument1 pageFlu Colds PertussisUmar AhmatNo ratings yet
- July - Newborn Anorectal MalformationsDocument14 pagesJuly - Newborn Anorectal Malformationsmiftahfarid21No ratings yet
- Flu Colds PertussisDocument1 pageFlu Colds PertussisUmar AhmatNo ratings yet
- Analysis GCT With Pulmonary MtasesetasDocument9 pagesAnalysis GCT With Pulmonary MtasesetasUmar AhmatNo ratings yet
- RBSK 160615192636 PDFDocument30 pagesRBSK 160615192636 PDFJerald BennyNo ratings yet
- Freelance Interactive Medical Advisor TestDocument2 pagesFreelance Interactive Medical Advisor TestNiki Erista AyudiaNo ratings yet
- Hemorrhagic Shock Signs, Assessment and ManagementDocument114 pagesHemorrhagic Shock Signs, Assessment and ManagementclaudiaNo ratings yet
- Tle 10Document49 pagesTle 10peepee poopooNo ratings yet
- Neonatal JaundiceDocument12 pagesNeonatal JaundiceGiska T PutriNo ratings yet
- Cholelithiasis: Group MembersDocument12 pagesCholelithiasis: Group MembersShiela GutierrezNo ratings yet
- The Natural Remedy HandbookDocument264 pagesThe Natural Remedy HandbookRoi Trawon100% (2)
- CefaclorDocument3 pagesCefaclorAyah PaasaNo ratings yet
- Head Injury and concussion-ENDocument5 pagesHead Injury and concussion-ENJasly SafeerNo ratings yet
- Apollo's ArrowDocument3 pagesApollo's ArrowMalik AssafNo ratings yet
- Disability Category ChartDocument4 pagesDisability Category Chartapi-325700981100% (1)
- 3 MBBS Part I Routine (Theory) Department of Pediatrics Total: 20 Duration: 1hrDocument12 pages3 MBBS Part I Routine (Theory) Department of Pediatrics Total: 20 Duration: 1hrGaurav BatniNo ratings yet
- NCP HeadDocument11 pagesNCP Headann-lisel-manahan-7670100% (2)
- Defining Treatment Response, Remission, Relapse, and RecoveryDocument21 pagesDefining Treatment Response, Remission, Relapse, and Recovery주병욱No ratings yet
- NitrofurantoinDocument3 pagesNitrofurantoinapi-3797941No ratings yet
- Marginal Zone Lymphomas: Subtypes: MALT (Extranodal), Nodal, SplenicDocument2 pagesMarginal Zone Lymphomas: Subtypes: MALT (Extranodal), Nodal, SplenicwwxxmmNo ratings yet
- Heart SoundDocument29 pagesHeart Sounddianpratiwirahim100% (1)
- Basinger Abraham - ConsultationDocument80 pagesBasinger Abraham - ConsultationVikas NairNo ratings yet
- Endometriosis & Adenomyosis Dr. Selly Septina, SpogDocument25 pagesEndometriosis & Adenomyosis Dr. Selly Septina, SpogRezkiRamadhanNo ratings yet
- Public Warned vs. Chickenpox (Article From ABSCBN News) : ReflectionDocument1 pagePublic Warned vs. Chickenpox (Article From ABSCBN News) : Reflectionkuu faalNo ratings yet
- Laporan Kasus - Dendy Dwi Ramadhani - PPDS Anestesi BrawijayaDocument1 pageLaporan Kasus - Dendy Dwi Ramadhani - PPDS Anestesi BrawijayaDendyNo ratings yet
- Soft Tissue InjuryDocument72 pagesSoft Tissue InjuryCucu Ne Eyang Kakung75% (8)
- Noninvasive Ventilation in Acute Respiratory FailureDocument6 pagesNoninvasive Ventilation in Acute Respiratory FailureCesar C SNo ratings yet
- Psycho Physiological Disorders 1Document8 pagesPsycho Physiological Disorders 1Cedric Jay Villegas TasicoNo ratings yet
- COVID-19 Isolation Effects on Mental Health and EconomyDocument10 pagesCOVID-19 Isolation Effects on Mental Health and EconomyRimsHa ShAbbirNo ratings yet