Professional Documents
Culture Documents
Robbins Pathology Chapter 14 - RBCs
Uploaded by
scorpiosphinx79Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Robbins Pathology Chapter 14 - RBCs
Uploaded by
scorpiosphinx79Copyright:
Available Formats
Path Chapter 14 Red Blood Cells
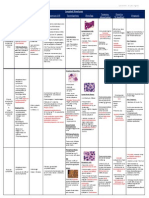
Anemia Clinical manifestations of anemia -pallor, weakness, fatigue, malaise, dyspnea -fatty change in liver, myocardium, kidney -cardiac failure (angina), oliguria/anuria (kidney hypoperfusion), CNS sx (headache, vision loss, faintness) Acute Blood Loss Anemia -normochromic, normocytic -lowered Hct: hemodilution from fluid shift from interstitial to intravascular compartment -increased erythropoietin: stimulates erythroid progenitors, 5-7 days later increased reticulocytes -leukocytosis: compensatory release of adrenergic hormones mobilizes granulocytes -thrombocytosis - increased platelets Chronic Blood Loss Anemia -only occurs when rate of loss > regenerative capacity of marrow or when iron reserves are depleted and iron deficiency anemia appears General Characteristics of Hemolytic Anemias Premature destruction of RBCs (<120days) in phagocytes -> splenomegaly Elevated erythropoietin levels Accumulation of hemoglobin degradation products Increased number of reticulocytes Extravascular Hemolysis -reduced deformability of RBCs -Sx: anemia, splenomegaly, jaundice; decreased plasma haptoglobin (from binding extra hemoglobin) -Tx: splenectomy Intravascular Hemolysis -caused by mechanical injury, complement fixation, intracellular parasites (malaria), exogenous toxic factors (clostridial sepsis) -Sx: anemia, hemoglobinemia, hemoglobinuria, hemosiderinuria, jaundice (or pigment gallstones); decreased serum haptoglobin (complexes are phagocytosed) -increased erythropoietin -> normoblasts -> reticulocytes Hereditary Spherocytosis (HS) -autosomal dominant disorder with defect in RBC cell membrane skeleton proteins ankyrin, band 3, spectrin, or band 4.2 -> sphere-shaped, non-deformable, easily sequestered RBCs -RBC lifespan 10-20 days, hyperchromic, increased MCHC -sx: splenomegaly, anemia, jaundice, aplastic crises, pigment gallstones -Tx: splenectomy (corrects anemia but not RBC shape) Glucose-6-Phosphate Dehydrogenase Deficiency -X-linked recessive; abnormality in glutathione metabolism -> RBCs not protected against oxidative injury (reduced NADPH)-> hemolysis -mutation may be protectant against malaria -older RBCs hemolyse > younger RBCs -Sx worse with exposures to oxidative stress (infections, drugs, foods) -oxidants cause intravascular and extravascular hemolysis -> Heinz bodies, bite cells, spherocytes -Sx: increased reticulocytes, hemolysis is self-limited Sickle Cell Disease -point mutation in -globulin causes replacement of glutamate with valine (HbS) -Trait: heterozygous for HbS -protects against malaria -HbS molecules polymerize when deoxygenated, cytosol gels and HbS aggregates form -chronic hemolysis, microvascular occlusion, tissue damage -Variables: Hb interactions, MCHC, intracellular pH, RBC transit time
Pathogenesis of Sickle Cell Disease -Deoxygenation -> influx of Ca2+ outflux of K+ and H2O -> sickling -if reoxygenated: sickle cells -> become bi-concave but with dehydration and membrane damage, if redeoxygenated -> sickling and microvascular occlusion -if membrane-damaged: sickle cells hemolyse -vicious cycle - deoxygenation ->sickling -> hypoxia -> more sickling Sickle Cell Clinical Manifestations -Howell-Jolly bodies; "crew-cut" Xray -vaso-occlusive "pain" crises: fever, cough, chest pain, pulmonary infiltrates -anemia, reticulocytosis, hyperbilirubinemia, sickled cells on blood smear -children: hand-foot syndrome/dactylitis -Sequestration crisis: splenomegaly, hypovolemia, shock; Aplastic crisis: parvovirus -Altered kidney function -> hyposthenuria -susceptibility to infxn (pneumonia, H. flu, meningitis) -Tx: hydroxyurea (DNA synthesis inhibitor)
Thalassemia -0 mutation -> no -globulin; + mutation -> reduced -globulin -mutations -> deficit in HbA synthesis -> hypochromic, microcytic RBCs, reduced O2 capacity, decreased RBC lifespan; membrane damage -> ineffective erythropoiesis (erythroid hyperplasia and extramedullary hemotopoiesis and extravascular hemolysis -> cachexia), iron overload (from decreased hepcidin) Pathogenesis of -Thalassemia -hallmark = aggregates of unpaired -globulin chains (not seen on blood smears) -Thalassemia syndromes -Thalassemia Major (0-0,+-0,+-+) - elevated HbF, severe transfusion-dependent anemia 6-9 months after birth; anisocytosis, poikilocytosis, microcytosis, hypochromia, reticulocytosis, "crew cut" xray, iron overload -Thalassemia Minor (trait) (0-, +-) - mild asymptomatic microcytic anemia -Thalassemia Intermedia - severe non-transfusion dependent anemia Clinical Features of -Thalassemia -growth retardation and early death in untreated children -cardiac disease from iron overload and secondary hemochromatosis (from transfusions) -tx with iron chelators -Tx: bone marrow transplant -Thalassemia -inherited deletions that result in reduced or absent synthesis of -globulin chains -anema from lack of adequate hemoglobin and excess unpaired non--chains (,,)-> Hemoglobin Barts and HbH -Thalassemia Syndromes severity depends on number of defective genes (there are 4 -globulin genes) carrier=1: asymptomatic, no RBC abnormality trait=2: asymptomatic, microcytic anemia HbH disease=3: severe, non-transfusion-dependent anemia hydrops fetalis=4: lethal in utero w/o transfusions; b/c hemoglobin Barts doesn't release O2 Paroxysmal Nocturnal Hemoglobinuria -acquired (X-linked lyonized) mutation in PIGA gene (enzyme for cell surface protein synthesis) -blood cells are deficient in GPI-linked proteins that regulate complement activity: CD55, CD59 (C3 convertase inhibitor that prevents spontaneous complement activation), CD8 -intravascular hemolysis at night when blood pH is lower -> hemosiderinuria -> iron deficiency -thrombosis is leading cause of death (dysfunctional platelets) -dx: flow cytometry tx: bone marrow transplant Immunohemolytic anemia -caused by antibodies against RBCs -> premature destruction -sometimes caused by a drug -dx: direct and indirect Coombs test -Warm antibody type, cold agglutinin type, cold hemolysin type Warm antibody type (immunohemolytic anemia) -most common - 50% idiopathic, rest is autoimmune, drug-induced (penicillins, cephalosporins, -methyldopa), or lymphomas -IgG antibodies against Rh antigens coat RBCs which bind to Fc receptors on phagocytes -> partial phagocytosis -> spherocytosis -> splenomegaly and extravascular hemolysis Cold agglutinin type (immunohemolytic anemia) -IgM antibodies bind to RBCs at low temperatures -antibodies appear after infxns (mycoplasma pneumoniae, EBV, CMV influenza, HIV) -agglutination occurs in "cold skin" areas (fingers, toes, nose, ears) -> pallor, cyanosis, Raynaud Cold hemolysin type (immunohemolytic anemia) -"paroxysmal cold hemoglobinuria" -> intravascular hemolysis and hemoglobinuria (sometimes fatal) -autoantibodies (IgG) bind to P group RBC antigens in cool areas of body -> complement-mediated lysis occurs when RBCs move to warm areas of body -most cases follow viral infections and are transient -treatment involves removing offending factors (drugs), or treating with immunosuppression and splenectomy Hemolytic anemia resulting from mechanical trauma mechanical trauma from cardiac valve prostheses -hemolysis occurs from shear forces from turbulent flow and pressure gradients across mechanical valves microangiopathic disorders (DIC, TTP, HUS, malignant hypertension, SLE, disseminated cancer) -luminal narrowing (deposition of fibrin and platelets) dx: RBC fragments (schistocytes), burr cells, helmet cells, triangle cells Megaloblastic Anemias -impairment of DNA synthesis that leads to morphologic changes -pernicious anemia (vit B12 and folate deficiency) -RBCs are macrocytic and oval, MCHC is not elevated, reticulocyte count is low, neutrophils are macropolymorphonuclear Pernicious anemia: Vitamin B12 deficiency
-caused by autoimmune gastritis and attendant failure of intrinsic factor production which leads to vit B12 deficiency -Sx: atrophic glossitis, CNS lesions from demyelination of lateral and dorsal tracts (->parathesia, ataxia, paraperesis) -Dx: megaloblastic anemia, leukopenia, low vitB12, high homocysteine and methylmalonic acid -may have inc risk for gastric carcinoma and vascular disease Normal Vitamin B12 Metabolism -cobalamin complex; humans can't synthesize it (comes from microorganisms), usually from animal food products -bound B12 is released by pancreatic proteases then associated with intrinsic factor (secreted by parietal cells in stomach), transported to ileum and endocytosed, then associated with transcobalamin II and secreted into plasma -high bioavailability of vitamin B12 supplements Biochemical Functions of Vitamin B12 -1)methylcobalamin is a cofactor for conversion of homocysteine to methionine by methionine syntheses via FH 4 -folic acid is needed for this rxn, and if deficient causes the anemia -supplement cures anemia -2)isomerization of methylmalonyl CoA to succinyl CoA -> demyelination ->-neurologic complications (not cured with folate supp.) Other disorders of Vitamin B12 deficiency -achlorhydria and loss of pepsin secretion -gastrectomy (no intrinsic factor) -loss of exocrine pancreas function -ileal resection (reduced absorption) -tapeworms (competes for host vitB12) -hyperthyroidism, pregnancy, disseminated cancer, chronic infection (increased vitB12 demand) Anemia of folate deficiency -causes megaloblastic anemia similar to vitamin B12 deficiency (through reduced DNA synthesis) -via FH4 participates in 1)purine synthesis, 2)homocysteine->methionine 3)deoxythymidylate monophosphate synthesis Etiology of Anemia of folate deficiency 1. decreased intake (cannot be synthesized, sensitive to heat, not stored) -usually in general malnutrition setting, certain drugs impair absorption 2. increased requirements (pregnancy, infancy, hemolytic anemias, etc) 3. impaired utilization (folic acid antagonists-methotrexate-inhibit dihydrofolate reductase) Clinical manifestations of Folate deficiency anemia -decreased levels of folate in serum and RBCs -no neurological effects -folate administration may exacerbate neuro sx in vit B12 deficiency anemia (so check levels first) Iron deficiency anemia -most common nutritional disorder in the world -20% of heme iron from diet is absorbed -80% of functional iron is in hemoglobin (myoglobin and iron-containing enzymes (catalase and cytochromes) contain the rest) -storage pool (hemosiderin and ferritin) = 15-20% of total body iron -iron is recycled extensively, it is transferred by iron-binding glycoprotein transferrin (synthesized in liver) -major function of plasma transferrin is to deliver iron to cells -free iron is highly toxic so storage iron must be sequestered (by binding to ferritin or hemosiderin) -plasma ferritin is derived from the storage pool of body iron, its levels correlate with body iron store levels -iron balance is maintained by regulating GI absorption there is no regulated pathway for excretion -luminal non-heme iron is Fe3+ and must be reduced to Fe2+ (ferrous) by ferrireductases (b cytochromes and STEAP3) -iron that enters duodenal cells enters via transport to the blood or storage as mucosal iron -Iron absorption is regulated by hepcidin inhibits iron transfer from the erythrocyte to plasma by binding to ferriportin and causing it to be endocytose and degraded; it also suppresses iron release from macrophages -alterations in hepcidin have a central role in diseases involving disturbances of iron metabolism Rare form of microcytic anemia caused by mutations that disable TMPRSS6 (hepatic transmembrane serine protease) that normally suppresses hepcidin production when iron stores are low affects pts have high hepcidin levels, reduced iron absorption and failure to respond to iron therapy Hepcidin is low in hemachromatosis (systemic iron overload) primary is associated with inherited mutations in hepcidin gene or genes that regulate hepcidin expression Secondary hemachromatosis can occur in diseases associated with ineffective erythropoiesis ( -thalassemia major and myelodysplastic syndromes) Etiology of Iron Deficiency Anemia 1. Results from dietary lack of iron men need 7-10mg, women 7-20mg (avg intake is 15-20mg) a. Heme iron is more absorbable than inorganic iron absorption of inorganic iron is enhanced by ascorbic acid, citric acid, amino acids and sugars it is inhibited by tannates, carbonates, oxalates, and phosphates b. Dietary iron deficiency usually occurs in infants, elderly, impoverished, teenagers 2. Impaired absorption due to sprue, other causes of steatorrhea, chronic diarrhea, gastrectomy, achlorhydria 3. Increased requirement infancy and childhood and pregnancy (esp if pregnancies are close together) 4. Chronic blood loss **most important and most common a. External hemorrhage or internal bleeding into GI, urinary or genital tracts depletes iron reserves b. Iron deficiency in adult men or postmenopausal women MUST be attributed to GI bleed until proven otherwise Pathogenesis -iron deficiency causes microcytic, hypochromic anemia -anemia only appears when iron stores are completely depleted and is accompanied by low serum iron, ferritin and transferrin levels Clinical Features -features of general anemia -iron depletion in cells causes: koilonychia (spoon nails), alopecia, atrophic changes to tongue (glossitis) and gastric mucosa, and intestinal malabsorption, depletion of iron from CNS may cause pica -Plummer-Vinson Syndrome triad: esophageal webs, microcytic hypochromic anemia, atrophic glossitis -Dx: decreased H&H, microcytosis, hypochromia, poikolocytosis, serum iron and ferritin are low, total plasma iron-binding capacity (increased trasferrin levels) is high, hepcidin levels are low
-in uncomplicated iron-deficiency anemia tx is iron supplements, reticulocytes appear in 5-7 days Anemia of chronic disease -impaired red cell production associated with chronic diseases is most common anemia in hospitalized pts -Illnesses associated: 1. Chronic microbial infections (osteomyelitis, bacterial endocarditis, lung abscess) 2. Chronic immune disorders (RA, regional enteritis) 3. Neoplasms (carcinomas of lung and breast, Hodgkin lymphoma) -occurs in setting of chronic inflammation -associated with low serum iron, reduced total-binding capacity, abundant iron in tissue macrophages -Inflammatory mediators (esp IL-6) stimulate increase in hepatic production of hepcidin (inhibits ferriportin function in macrophages and reduces transfer of iron from the storage pool to developing erythroid precursors in the bone marrow (as a result erythroid precursors are starved for iron) -erythropoietin is low (maybe b/c hepcidin suppresses production) -iron may be sequestered to prevent access to microbes -hepcidin is structurally related to defensins (antibacterial) -anemia is usually mild, RBCs are normochromic and normochromic OR microcytic and hypochromic -increased storage of iron in marrow macrophages, high serum ferritin level, reduced total iron-binding capacity rules out iron-deficiency anemia -Tx: treat underlying disease, sometimes (with cancer) erythropoietin Aplastic anemia -syndrome of chronic primary hematopoietic failure and attendant pancytopenia (anemia, neutropenia, thrombocytopenia) -Idiopathic: usually autoimmune, can be acquired or inherited defects of hematopoietic stem cells -Etiology most cases follow exposure to chemicals and drugs (chemotherapy, benzene) that cause marrow suppression, sometimes drugs not related to marrow suppression (chloramphenicol, gold salts) -persistant marrow aplasia can appear after viral infections (hepatitis - non-A,B,C,E,G; CMV, EBV, HZV) -whole body irradiation (dose-dependent) -inherited defects (Fanconi anemia rare AR disorder with defects in multiprotein complex that is required for DNA repair); inherited defects in telomerase -Pathogenesis 1. Extrinsic, immune-mediated suppression of marrow progenitors, 2. Intrinsic abnormality of stem cells -Clinical Features -pancytopenia: Anemia: weakness, pallor, dyspnea; Thrombocytopenia (petechiae, ecchymosis), Neutropenia (minor infections, chills, fever, prostration); splenomegaly is ABSENT, RBCs are normochromic and slightly macrocytic; RETICULOCYTOPENIA is the RULE; Dx: bone marrow aspirate (distinguish from other causes of aplastic anemia that have same presentation); Tx: bone marrow transplant Pure Red Cell Aplasia -primary marrow disorder in which only erythroid progenitors are suppressed (or absent in severe cases) -associated with neoplasms (thymoma, leukemia), drug exposures, *autoimmune disorders, parvovirus (B19 infects and destroyed red cell progenitors specifically) -Tx: if thymoma, removal; sometimes plasmaphoresis helps (esp with autoimmune); parvovirus is usually self-limited and anemia is transient, can cause major problems in pts with hemolytic anemia or who are immunosuppressed Other Causes of Marrow failure Myelophthisic anemia -marrow failure associated with space-occupying lesions that replace normal bone marrow elements (most often metastastases from breast, lung and prostate); can be infiltrative granulomatous process; also a feature of spent phase of myeloproliferative disorders; all cause marrow distortion and fibrosis, release of granulocytes from marrow causes abnormal leukoerythroblasts on smears and tear-drop-shaped cells Chronic Renal Failure multifactorial but mostly from decreased erythropoietin synthesis; tx: recombinant erythropoietin and iron Hepaticellular liver disease whether toxic, infectious or cirrhotic; anemia is due to decreased marrow function and exacerbated by folate and iron deficiency (from poor nutrition and bleeding), erythroid progenitors are mostly affected, slightly macrocytic anemia (due to lipid abnormalities) Endocrine disorders esp hypothyroidism (mild, normochromic, normocytic anemia) Polycythemia -abnormally high red cell count usually with increased hemoglobin -relative polycythemia (increase in red cell when there is hemoconcentration due to reduced plasma volume) caused by dehydration -stress polycythemia (Gaisbck syndrome) pts are usually obese, hypertensive and stressed unknown mechanism -absolute polycythemia (increase in total red cell mass) -primary intrinsic abnormality in hematopoietic precursors -polycythemia vera (most common cause) myeloproliferative disorder due to mutations that lead to erythropoietin-independent growth of red cell progenitors (less common is familial mutations in erythropoietin receptor that induces activationnatural blood doping) -secondary red cell progenitors respond to compensatory or pathologic increased levels of erythropoietin; erythropoietin-secreting tumors and rare inherited defects that lead to stabilization of HIF-1 (hypoxia-induced factor that stimulates transcription of erythropoietin gene) Intro to Bleeding Disorders (Hemorrhagic diatheses) -bleeding can result from 1) increased fragility of vessels 2) platelet deficiency/function 3) derangement of coagulation 4) combination -LAB test: Prothrobin time (PT): tests extrinsic and common coagulation pathways; prolonged PT from deficiency/dysfunction of factor V, factor VII, factor X, prothrombin, fibrinogen Partial thromboplastin time (PTT): tests intrinsic and common pathways; prolonged PTT from deficiency/dysfunction of factors V, VIII, IX, X, XI, XII, prothrombin, fibrinogen, or antibodies to phospholipid Platelet counts: reference range 150-300 x10^3 platelets/L; clumping of platelets can cause thrombocytopenia during automated coun ting; high counts may indicate myeloproliferative disorder (essential thrombocytopenia) Tests of platelet function: bleeding time (not accurate), tests of platelet aggregation, quantitative/qualitative tests of vWF Specialized tests: levels of specific clotting factors, fibrinogen, fibrin split products, presence of circulating anticoagulants Bleeding disorders caused by vessel wall abnormalities nonthrombocytopenic purpuras; most often induce small hemorrhages (petichiae and purpura) on skin and mucous membranes (esp gingiva), more significant bleeds can occur in joints, muscles, subperiosteal locations, menorrhagia, epistaxis, GI bleeds, hematuria; platelet count, bleeding time, PT/PTT are usually normal Infections: cause petichiae/purpura; menignococcemia, septicemia, infective endocarditis, rickettsioses; mechanism: microbial damage to the microvasculature (vasculitis) and DIC
Drug Reactions: cause cutaneous petichiae/purpura w/o thrombocytopenia; deposition of drug-induced immune complexes in vessel walls which leads to hypersensitivity (leukocytoclastic) vasculitis Scurvy, Ehlers-Danlos Syndrome, Cushing syndrome: microvascular bleeding; defects in collagen weakens vessel walls Henoch-Schnlein Purpura: characterized by purpuric rash, colicky abdominal pain, polyarthralgia, acute glomerulonephritis; caused by deposition of circulating antibody-antigen complexes within vessels and glomerular mesangial regions Hereditary hemorrhagic telangiectasia (Weber-Osler-Rendu): AD disorder characterized by dilated, tortuous vessels with thin walls that bleed easily (oral cavity, GI tract); serious bleeding is possible Perivascular amyloidosis: weakens blood vessel walls and causes bleeding; mucocutaneous petichiae
Thrombocytopenia - <100,000 platelets/L; NORMAL PT/PTT; spontaneous bleeding usually associated with small vessels; bleeding in skin, mucous membranes, GI and GU tracts, serious intracranial bleeds -Causes of thrombocytopenia: Decreased platelet production: conditions that depress marrow output generally or affect megakaryocytes selectively o Drugs, infections (HIV), B12/folate deficiency, aplastic anemia, leukemia, disseminated cancer, granulomatous disease, myelodysplastic syndromes Decreased platelet survival: immune thrombocytopenia platelet destruction is caused by antibodies to platelets or immune complexes that deposit on platelets; IgG antibodies from mother can cause thrombocytopenia in the fetus o Autoimmune (primary and secondary), alloimmune (posttransfusion/neonatal), drugs, infections (HIV, EBV), DIC, thrombotic microangiopathies, giant hemangiomas, mechanical injury (prosthetic heart valves) Sequestration: in spleen, normally sequesters 30-35% of platelets, can be as high as 80-90% with splenomegaly (hypersplenism) Dilution: massive transfusions; platelets decrease in stored blood Chronic Immune Thrombocytopenic Purpura (ITP) Pathogenesis: caused by autoantibodies to platelets; may be secondary (SLE, HIV, CLL) or primary (only after secondary dx excluded); autoantibodies against platelet membrane glycoproteins IIb-IIIa or Ib-IX, usually IgG; antiplatelet antibodies act as opsonins and are recognized by IgG Fc receptors on phagocytes leading to increased platelet destruction; autoantibodies may also bind to and damage megakaryocytes Morphology: spleen is normal size, congestion of sinusoids and enlargement of follicles, scattered megakaryocytes in sinuses; marrow has increased number of megakaryocytes; peripheral blood shows abnormally large platelets (megathrombocytes) (sign of accelerated thrombopoiesis) Clinical features: adult women <40YOA; bleeding into skin and mucosal surfaces (petichiae, can become confluent and develop into ecchymoses); hx of easy bruising, epistaxis, gingival bleeding, hemorrhages into soft tissue with minor trauma; may manifest as melena, hematuria, excessive menstrual flow; subarachnoid hemorrhage and intracerebral hemorrhage are fatal complications; splenomegaly and lymphadenopathy uncommon in primary disease; Lab: low platelet count, normal/increased megakaryocytes in bone marrow; large platelets in peripheral blood, normal PT/PTT; Tx: glucocoricoids (inhibit phagocyte function), splenectomy normalizes platelet count (increases risk of bacterial sepsis); IV Ig or anti-CD20 antibody (ritucimab) effective in pts who relapse after splenectomy Acute Immune Thrombocytopenic Purpura Pathogenesis: Caused by autoantibodies to platelets Clincal features: children; usually follows viral illness (2 weeks prior); self-limited (6 months); glucocorticoids given if severe Drug-induced Thrombocytopenia - direct effect of drug on platelets or immunologically-mediated platelet destruction; drugs: gold salts (unknown mech) vancomycin, quinidine, quinine (bind to platelet glycoproteins or create antigenic determinants that are recognized by autoantibodies), common consequence of platelet inhibitory drugs that bind to glycoprotein IIb-IIIa (conformational changes -> antigenic epitope) Heparin-induced thrombocytopenia: 5% of pts receiving heparin, most develop type I thrombocytopenia (little clinical importance, most likely from platelet aggregation), type II occurs 5-14 days after therapy begins, leads to life-threatening venous and arterial thrombosis (caused by antibodies that recognized factor V-heparin complexes, binding of antibody to these complexes activates platelets and promotes thrombosis (even in thrombocytopenia), unless therapy is stopped clots in large arteries can lead to vascular insufficiency and limb loss, and emboli from DVTs can cause PE; risk of severe HIT is lower in low-molecular weight heparin HIV-associated Thrombocytopenia - One of the most common hematologic complications of HIV; both impaired production and increased destruction contribute (CD4 and CXCR4 are on megakaryocytes and allow them to be infected with HIV); HIV-infected megakaryocytes are prone to apoptosis and their ability to produce platelets is impaired; HIV also causes B-cell hyperplasia and dysregulation (predisposes to development of autoantibodies sometimes against Gp IIb-IIIa complexes), autoantibodies opsoninize platelets (they are destroyed by mononuclear phagocytes in the spleen and elsewhere Thrombotic Thrombocytopenic Purpura (TTP) thrombotic microangiopathy; PENTAD: fever, thrombocytopenia, microangiopathic hemolytic anemia, transient neurological deficits, renal failure; caused by increased activation of platelets which deposit as thrombi in microcirculatory beds; usually associated with deficiency (acquired or inherited) of plasma enzyme ADAMTS13 (vWF metalloprotease) which causes multimers of vWF to accumulate in the plasma and promote platelet activation and aggregation; delay in diagnosis can be fatal; tx with plasmapheresis (removes autoantibodies and provides functional ADAMTS13); PT/PTT normal Hemolytic Uremic Syndrome (HUS) - thrombotic microangiopathy; Characterized by: microangiopathic hemolytic anemia, thrombocytopenia, no neurological symptoms, acute renal failure; usually seen in children; caused by increased activation of platelets which deposit as thrombi in microcirculatory beds; strongly associated with E. coli O157:H7 (Shiga toxin); results in platelet activation and aggregation; children and elderly at highest risk; presentation is bloody diarrhea followed by HUS; irreversible renal damage and death can occur Non-endemic atypical HUS: associated with inherited defects or acquired autoantibodies to complement factor H, membrane cofactor protein (CD46) or factor I (three proteins normally act to prevent excessive activation of alternative complement pathway); relapsing and remitting course; mechanism unclear; PT/PTT normal Defective Platelet syndromes inherited disorders of platelet function Defects of adhesion: autosomal recessive Bernard-Soulier syndrome (inherited deficiency of platelet membrane gp Ib-IX (receptor for vWF)) Defects of aggregation: autosomal recessive Glanzmann thrombasthenia (deficiency in gp IIb-IIIa) Disorders of platelet secretion (release reaction): defective release of certain mediators of platelet activation (thromboxanes, granule-bound ADP); storage pool disorders Acquired defects: aspirin (irreversible inhibitor of COX) and other NSAIDs; uremia (complex mechanism) Hematologic diatheses related to abnormalities in clotting factors: isolated coagulation factor deficiencies; usually manifest as large post-traumatic ecchymoses or hematomas, or prolonged bleeding after surgery or laceration; bleeding in the GI and urinary tracts and weight bearing joints (hemarthroses) is common; hereditary disorders usually affect one factor, acquired deficiencies affect multiple factors and can be based on decreased protein synthesis or shortened half-life (vit K deficiency causes impaired synthesis of factors II, VII, IX, X and protein C); DIC
Factor VII-vWF Complex: once factor VIII reaches circulation it binds to vWF (which stabilizes it), most important function of vWF is to promote platelet adhesion to subendothelial matrix; factor VIII function is assessed by coagulation assays with mixtures of patient plasma and factor VIII-deficient plasma; vWF is assessed using ristocetin agglutination test Von Willebrand Disease: most common inherited bleeding disorder (1% of US); most common symptoms: spontaneous bleeding from mucous membranes (epistaxis), excessive bleeding from wounds, menorrhagia, prolonged bleeding time with normal platelet count, secondary decrease in gp IIb-IIIa reflected as prolonged PTT (in types 1 and 3), hemarthroses not seen; treat patients facing hemostatic challenges (dental work, surgery) with desmopressin (stimulates vWF release) or infusions of plasma concentrates containing factor VIII and vWF Type 1: associated with reduced quantity of circulating vWF; type 1 is autosomal dominant, mild deficiency, 70% of cases Type 3: associated with reduced quantity of circulating vWF; autosomal recessive, extremely low levels of functional vWF and corresponding severe symptoms (bleeding resembles hemophilia because vWF stabilizes gp IIb-IIIa) Type 2: qualitative defects in vWF; 25% of cases; many subtypes: 2A (most common, autosomal dominant, normal amounts of vWF but missense mutations cause defective multimer assembly, mild-moderate bleeding) Hemophilia A (Factor VIII deficiency): most common hereditary disease associated with life-threatening bleeding; caused by mutations in factor VIII; X-linked (males and homozygous females); inadequate coagulation (fibrinogenesis) and inappropriate clot removal (fibrinolysis) contribute to bleeding; wide range of clinical severity that correlates with level of factor VIII activity (not levels, protein may be created, but inactive); symptoms: easy bruising and massive hemorrhage after trauma or surgery, hemarthroses (if recurrent may lead to crippling deformities), petichiae are absent; LAB: prolonged PTT, normal PT (abnormality of intrinsic pathway), factor VIII assays required for dx; Tx: infusions of recombinant factor VIII, about 15% of pts develop antibodies to factor VIII (therapeutic challenge); many hemophiliacs contracted AIDS from concentrates Hemophilia B (Christmas Disease, Factor IX deficiency): severe factor IX deficiency; clinically indistinguishable from hemophilia A; X-linked; variable clinical severity; 15% of pts have present but non-functioning factor IX; LAB: PTT is prolonged, PT is normal (intrinsic pathway abnormality); Dx: assay of factor IX; Tx: infusions of recombinant factor IX Disseminated Intravascular Coagulation (DIC): acute, subacute, or chronic thrombohemorrhagic disorder characterized by excessive activation of coagulation, which leads to formation of thrombi in microvasculature in the body, secondary complication to many disorders; consumption of platelets, fibrin, coagulation factors, secondary activation of fibrinolysis; presents with signs and symptoms of hypoxia and infarction from thrombi and hemorrhage due to depletion of factors required for hemostasis and activation of fibrinolysis, or both. Pathogenesis: pathologic activation of extrinsic and/or intrinsic pathways of coagulation (more common) or the impairment of clot-inhibiting mechanisms (less common) o Mechanisms: Release of tissue factor or thromboplastic substances into circulation a from variety of sources: Obstetric complications: thromboplastins derived from placenta, dead retained fetus, or amniotic fluid that enters circulation Cancers o Cytoplasmic granules of acute promyelocytic leukemia cells o Mucus from certain adenocarcinomas (lung, colon, pancreas, stomach): can directly activate factor X independent of factor VII Widespread injury to endothelial cells: Endothelial cell injury and necrosis causes exposure of the subendothelial matrix leading to activation of platelets and both arms of the coagulation pathway; TNF (implicated in DIC in sepsis) induces endothelial cells to express tissue factor on their surfaces and decreases expression of thrombomodulin (shifting hemostasis towards coagulation), TNF also regulates expression of adhesion molecules on endothelial cells (promoting adhesion of leukocytes which can cause further damage by ROS) Deposition of antigen-antibody complexes (SLE) Temperature extremes (heat stroke, burns) Sepsis: Microorganisms (meningococci, rickettsiae); injury to endothelial cells from endotoxins Major trauma/surgery/burns: major trigger is release of thromboplastins Hypoxia/acidosis/shock: can cause endothelial injury, further complicated by supervening infections o Possible consequences Widespread deposition of fibrin in microcirculation, leads to ischemia and microangiopathic hemolytic anemia Consumption of platelets and coagulation factors and the activation of plasminogen leads to hemorrhagic diatheses Morphology: thrombi are most often seen in brain, heart, lungs, kidneys, adrenals, spleen and liver (decreasing frequency), any tissue can be affected o Waterhouse-Friedrichsen syndrome: massive adrenal hemorrhages probably caused by fibrin thrombi in microcirculation of adrenal cortex, associated with menigococcemia o Sheehan syndrome: pituitary post-partum necrosis, form of DIC o Toxemia of pregnancy: placenta has widspread microthrombi causing premature atrophy of the cytotrophoblast and syncytiotrophoblast o Giant hemangiomas: thrombi form within the neoplasm because of stasis and recurrent trauma to blood vessels Clinical features: onset can be fulminant (as in endotoxic shoc or amniotic fluid embolism), or insidious and chronic (carcinomatosis or retention of dead fetus); 50% are obstetric patients (tends to reverse with delivery); 33% have carcinomatosis; clinical presentations vary o Common patterns: microangiopathic hemolytic anemia; dyspnea, cyanosis and respiratory failure; convulsions and coma; oliguria and acute renal failure; sudden or progressive circulatory failure and shock Acute DIC (associated with obstetric complications and trauma) is dominated by bleeding diatheses Chronic DIC (cancer patients) tends to present as thrombotic complications o Diagnosis: clinical observation, lab studies (fibrinogen levels, PT/PTT, fibrin degradation products) o Prognosis: highly variable, depends on underlying disorder o Treatment: remove and treat inciting cause, management requires balance between hemorrhage and thrombosis (sometimes administration of anticoagulants or procoagulants is indicated)
You might also like
- Chapter 11 Blood Vessels 8th Ed NotesDocument7 pagesChapter 11 Blood Vessels 8th Ed NotesKyle Christopher SiaNo ratings yet
- Chapter 14 Red Blood CellsDocument37 pagesChapter 14 Red Blood CellsCatherine LiuNo ratings yet
- Quiz PathologyDocument28 pagesQuiz PathologyMedShare86% (35)
- Endocrine Pathology p17-32Document16 pagesEndocrine Pathology p17-32zeroun24No ratings yet
- WBC Neoplasms Review - PathologyDocument6 pagesWBC Neoplasms Review - Pathologylas100% (6)
- Robbin's SummariesDocument98 pagesRobbin's SummariesnopedontsuemepleaseNo ratings yet
- Patho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Document12 pagesPatho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Grant GarcesNo ratings yet
- (Mebooksfree Com) Rev&Pat&Gen&Gar&Gup&8thDocument633 pages(Mebooksfree Com) Rev&Pat&Gen&Gar&Gup&8thcharlie100% (7)
- Hematology & OncologyDocument94 pagesHematology & OncologyDaNy Chiriac100% (1)
- Pathology Board Questions PDFDocument92 pagesPathology Board Questions PDFJulius Matthew Luzana100% (2)
- IVMS-Hematology-Oncology Terminology Summary TableDocument16 pagesIVMS-Hematology-Oncology Terminology Summary TableMarc Imhotep Cray, M.D.No ratings yet
- Ch.1 Baby Robbins OutlineDocument11 pagesCh.1 Baby Robbins OutlinePA2014100% (3)
- Robbins Basic Pathology 9th Edition QBankDocument4 pagesRobbins Basic Pathology 9th Edition QBankVarshini Tamil SelvanNo ratings yet
- Cellular responses to stress and toxic insultsDocument29 pagesCellular responses to stress and toxic insultsMK100% (1)
- Endocrine PathologyDocument13 pagesEndocrine Pathologysarguss14100% (1)
- General PATHOLOGYDocument72 pagesGeneral PATHOLOGYlimpek100% (2)
- Acute Inflammation - Robbins Basic Pathology - Inflammation & RepairDocument24 pagesAcute Inflammation - Robbins Basic Pathology - Inflammation & RepairLuis Adrian De Jesús100% (9)
- Robbins Pathology NotesDocument48 pagesRobbins Pathology NotesRajesh Kumar Asunala91% (93)
- Heart - PathologyDocument22 pagesHeart - Pathologyjmosser100% (1)
- Patho ReviewDocument40 pagesPatho ReviewCoy Nuñez100% (2)
- The Rubik's Cube Approach To Clinical MedicineDocument2 pagesThe Rubik's Cube Approach To Clinical Medicinehenrygoldstein100% (1)
- Chapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of DiseaseDocument9 pagesChapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of DiseaseArun Nayak100% (11)
- General & Systemic Pathology Concepts - A Global OverviewDocument315 pagesGeneral & Systemic Pathology Concepts - A Global OverviewMarc Imhotep Cray, M.D.90% (10)
- Pediatric Anesthesiology PDFDocument309 pagesPediatric Anesthesiology PDFAviv Pasa100% (1)
- GI PathologyDocument22 pagesGI Pathologyzeroun24100% (5)
- Hemodynamic Disorders, Thromboembolic Disease and ShockDocument13 pagesHemodynamic Disorders, Thromboembolic Disease and Shockpjcanero100% (5)
- Patho4-6 - Liver (Dr. Dy)Document13 pagesPatho4-6 - Liver (Dr. Dy)miguel cuevas100% (1)
- NBME Answer With Explanation in DepthDocument10 pagesNBME Answer With Explanation in DepthDejan Zolak100% (3)
- Microcytic Hypochromic Macrocytic Normochromic Normocytic: Anemia HematocritDocument7 pagesMicrocytic Hypochromic Macrocytic Normochromic Normocytic: Anemia Hematocritjjjj31No ratings yet
- 480 MCQs With Answers of Goljan PathologyDocument382 pages480 MCQs With Answers of Goljan PathologySana Sheikh96% (28)
- Chapter 6 - Immune Diseases (Part I) (Robbins and Cotran Pathologic Basis of Disease)Document6 pagesChapter 6 - Immune Diseases (Part I) (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD90% (21)
- Robbins Questions Chp1-10Document28 pagesRobbins Questions Chp1-10verbatimmt100% (1)
- RObbinsDocument37 pagesRObbinsapi-374646950% (4)
- AnemiasDocument2 pagesAnemiasdoktorcoop100% (2)
- Robbins Pathology - Chapter 4 TransDocument9 pagesRobbins Pathology - Chapter 4 Transnath nathNo ratings yet
- Robbins and Cotran's Pathologic Basis of Disease Chapter 1Document14 pagesRobbins and Cotran's Pathologic Basis of Disease Chapter 1Mon Dominguez100% (2)
- Top 100 Pathology Secrets List W/ NotesDocument6 pagesTop 100 Pathology Secrets List W/ NotesPA2014100% (4)
- Pathology Qbank ChecklistDocument12 pagesPathology Qbank Checklistdr_sadiq100% (1)
- Robbins Ch. 20 The Kidney Review QuestionsDocument10 pagesRobbins Ch. 20 The Kidney Review QuestionsPA2014100% (4)
- General Pathology Bimonthly Exam Compilation Updated 2Document197 pagesGeneral Pathology Bimonthly Exam Compilation Updated 2Cherry Rahima100% (1)
- Endocrine System - Part 1 (Robbins)Document28 pagesEndocrine System - Part 1 (Robbins)sarguss14100% (2)
- Chapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Document3 pagesChapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD100% (5)
- Case report of 3-year old boy with asthmaDocument6 pagesCase report of 3-year old boy with asthmaJiaYee GoNo ratings yet
- Chapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of DiseaseDocument12 pagesChapter 8 Infectious Diseases Robbins and Cotran Pathologic Basis of DiseaseArun Nayak86% (7)
- Chapter 1 - Cellular Injury, Cell Adaptation & Cell Death (Robbins and Cotran Pathologic Basis of Disease)Document3 pagesChapter 1 - Cellular Injury, Cell Adaptation & Cell Death (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD91% (34)
- Lung - PathologyDocument34 pagesLung - Pathologyjmosser100% (3)
- IVMS Hematology-Oncology Summary Table-Notes For USMLE Step 1 Prep.Document16 pagesIVMS Hematology-Oncology Summary Table-Notes For USMLE Step 1 Prep.Marc Imhotep Cray, M.D.100% (1)
- Robbins Pathology - Chapter 5 TransDocument20 pagesRobbins Pathology - Chapter 5 Transnath nath100% (1)
- Robbins Pathology Chapter 13 - White Blood CellsDocument7 pagesRobbins Pathology Chapter 13 - White Blood Cellsscorpiosphinx7980% (5)
- Pathology A - The Cell As A Unit of Health and DiseaseDocument13 pagesPathology A - The Cell As A Unit of Health and DiseaseYui VainNo ratings yet
- Antiarrhythmic Drugs 1Document32 pagesAntiarrhythmic Drugs 1AliImadAlKhasakiNo ratings yet
- Cell Adaptation and Injury ReviewDocument137 pagesCell Adaptation and Injury ReviewBabak Barghy100% (1)
- Test Bank for Robbins and Cotran Pathologic Basis of Disease 9th EditionDocument6 pagesTest Bank for Robbins and Cotran Pathologic Basis of Disease 9th Editionahsan shahNo ratings yet
- Atherosclerosis-Thrombosis QuestionsDocument42 pagesAtherosclerosis-Thrombosis QuestionsJim Jose Antony100% (17)
- Preboard Exam Np3 Medical Surgical NursingDocument19 pagesPreboard Exam Np3 Medical Surgical NursingDavid LopezNo ratings yet
- Patho - Inflammation SummaryDocument28 pagesPatho - Inflammation SummaryTep Gonzales71% (7)
- FNCPDocument3 pagesFNCPLander VirayNo ratings yet
- Chapter 2 (Questions 2008-2009 Compiled)Document89 pagesChapter 2 (Questions 2008-2009 Compiled)vetpathforum100% (1)
- Pathology of Liver, Biliary, and PancreasDocument52 pagesPathology of Liver, Biliary, and PancreasHassan.shehri100% (11)
- Asynchronous Activity#2Document10 pagesAsynchronous Activity#2Nur Sanaani100% (1)
- GASTROINSTINAL TRACT Robbins 8th EditionDocument4 pagesGASTROINSTINAL TRACT Robbins 8th EditionLim EricNo ratings yet
- Liver - RobbinsDocument25 pagesLiver - Robbinssarguss14100% (2)
- HP Pathologies SummaryDocument10 pagesHP Pathologies SummaryMiki AberaNo ratings yet
- Red Blood Cells PathologyDocument47 pagesRed Blood Cells PathologyRodriguez Vivanco Kevin DanielNo ratings yet
- AnaemiaDocument83 pagesAnaemiaMohammad_Islam87100% (2)
- Disease Chart I3-1 (Emmeline)Document20 pagesDisease Chart I3-1 (Emmeline)ivankcurryNo ratings yet
- SGL 2 (Hemolytic Anemia & Hemoglobinopathies)Document53 pagesSGL 2 (Hemolytic Anemia & Hemoglobinopathies)raman mahmudNo ratings yet
- Coverage Midterm Examination 2021 Drug and Vice ControlDocument4 pagesCoverage Midterm Examination 2021 Drug and Vice ControlTaga Phase 7No ratings yet
- Diagnosis and Treatment of Limb Fractures Associated With Acute Peripheral IschemiaDocument6 pagesDiagnosis and Treatment of Limb Fractures Associated With Acute Peripheral IschemiaramadhaniandaNo ratings yet
- Using Magnets To Increase Retention of Lower DentureDocument4 pagesUsing Magnets To Increase Retention of Lower DentureFirma Nurdinia DewiNo ratings yet
- ImmerciDocument14 pagesImmercitextilessathishNo ratings yet
- Prevention of Surgical Site Infections: Surgical Patient Care SeriesDocument11 pagesPrevention of Surgical Site Infections: Surgical Patient Care Seriestien duongNo ratings yet
- Newborn PQDocument6 pagesNewborn PQNurseNancy93No ratings yet
- MapehasdasdDocument2 pagesMapehasdasdAmiel Angelo BaliosNo ratings yet
- Care of A Bedridden Patient: Prepared by Jannet Reena PuraniDocument25 pagesCare of A Bedridden Patient: Prepared by Jannet Reena PuraniAnn Merlin Jobin100% (1)
- Power of The Pinch Pinch Lower Lid BlepharoplastyDocument6 pagesPower of The Pinch Pinch Lower Lid BlepharoplastyBFF BotoxNo ratings yet
- Systemic in Ammatory Response Syndrome (SIRS) : Where Did It Come From and Is It Still Relevant Today?Document8 pagesSystemic in Ammatory Response Syndrome (SIRS) : Where Did It Come From and Is It Still Relevant Today?Jhanu JaguarNo ratings yet
- Ejsr 72 3 04Document9 pagesEjsr 72 3 04Khalifa BakkarNo ratings yet
- "HIV Depletes T-Helper17, We Simply Stimulate It": by Prof. DR - Pichaet Wiriyachitra PH.D., F.R.A.C.IDocument37 pages"HIV Depletes T-Helper17, We Simply Stimulate It": by Prof. DR - Pichaet Wiriyachitra PH.D., F.R.A.C.IfroggyzzNo ratings yet
- Anatomi Dan Fisiologi PerkemihanDocument89 pagesAnatomi Dan Fisiologi Perkemihannia djNo ratings yet
- OSCE Subcutaneous Injection SkillsDocument2 pagesOSCE Subcutaneous Injection SkillsvishnuNo ratings yet
- Becozyme AmpDocument1 pageBecozyme AmpMohammed IbrahimNo ratings yet
- 2016 - Byk FotoDocument7 pages2016 - Byk FotoSyifa IKNo ratings yet
- NBEMS announces DNB/DrNB practical exam datesDocument2 pagesNBEMS announces DNB/DrNB practical exam datesShivaraj S ANo ratings yet
- Jazel Ibon Galon PDFDocument2 pagesJazel Ibon Galon PDFJazel GalonNo ratings yet
- Secretin Hormone Activates Satiation by Triggering Brown FatDocument1 pageSecretin Hormone Activates Satiation by Triggering Brown FatTalal ZariNo ratings yet
- Addiction CaseDocument4 pagesAddiction CasePooja VarmaNo ratings yet
- Fora 6 Brochure PDFDocument8 pagesFora 6 Brochure PDFFatma IsmawatiNo ratings yet
- OtrivinDocument12 pagesOtrivinkanika sengarNo ratings yet