Professional Documents
Culture Documents
Wound Assessment
Uploaded by
onlyabc123Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wound Assessment
Uploaded by
onlyabc123Copyright:
Available Formats
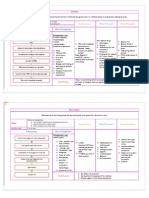
Wound Assessment & Documentation Terms WOUND LEVEL Pressure Ulcers: Stage I o An observable pressure-related alteration of intact skin
n with indicators, as compared to an adjacent or opposite area on the body, which may include changes in one or more of the following: Skin temperature (warmth or coolness) Tissue consistency (firm or boggy feel) &/or Sensation (pain, itching). o The ulcer appears as a defined area of persistent redness in lightly pigmented skin, whereas in darker skin tones, the ulcer may appear with persistent red, blue, or purple hues. Stage II-Partial thickness skin loss involving the epidermis &/or dermis. Stage III-Full thickness skin loss involving damage or necrosis of subcutaneous tissue that may extend down to, but not through, underlying fascia. Stage IV-Full thickness skin loss with extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures. Deep tissue injury o A pressure-related injury to subcutaneous tissues under intact skin. o Initially, these lesions have the appearance of a deep bruise & may herald the subsequent development of a Stage III-IV pressure ulcer even with optimal treatment. Other Wounds: Partial thickness-Tissue damage confined to the epidermis and/or dermis layers only. Full thickness-Tissue damage extending through the dermis & superficial fascia to involve subcutaneous tissue & possibly muscle/bone. WOUND TYPE Abscess-A cavity containing pus & surrounded by inflamed tissue. Ischemic/Arterial-A decreased supply of blood to a body part which typically leads to atrophy & in severe cases necrosis of the affected part. Neuropathic/diabetic foot ulcer o An ulcer typically occurring on the plantar aspect of the foot in areas prone to excessive pressure. o Generally presents as a symmetrically round, puncture-appearing wound cavity with a clean bed & heavily calloused periwound tissue. Pressure Ulcer-Localized injury to the skin &/or underlying tissue, usually over a bony prominence, & as a result of shear, friction, &/or pressure. Shearo The mechanical force that is parallel rather than perpendicular to an area. o It may play a role in triangularly shaped or tunneled sacral pressure ulcers. o This parameter is affected by pressure, the coefficient of friction between materials contacting each other, & how much the body interlocks with the support surface. Skin Tear-Traumatic peeling away of the epidermis from the dermis. Traumatic-Abrupt, acute tissue damage from physical or mechanical means external to the body. Venous insufficiency/stasis ulcer o A typically partial-thickness wound resulting from chronic venous insufficiency. o It is usually located between mid-calf & malleolus & has shaggy, irregular borders & often heavy exudate. Skin graft donor site-The area where the epidermis has been purposely removed so that free tissue can be moved to another part of the body where tissue coverage is needed. Page 1 of 4
Skin graft host site-The area where the skin graft is placed over a full-thickness wound. Surgical incision-A cut produced surgically that creates a partial thickness wound (if it does not penetrate the superficial fascia) or a full-thickness wound (if it penetrates to muscle tissue or deeper). Perineal Dermatitiso Moisture-associated skin damage resulting from prolonged exposure to urine &/or stool. o This exposure results in the release of inflammatory cytokines which causes redness, edema, blistering, skin erosion, weeping, itching, pain.
LOCATION Left or Right Bilateral-Occurring or appearing on two sides of the body Lateral-Away from the midline of the body Medial-Toward the midline of the body Anterior-Near to or at the front of the body Posterior-Near to or at the back of the body Dorsal-Pertaining to the back of an appendage, i.e. the back of the hand or top of the foot Plantar-The bottom of the foot Palmar-The palm of the hand Upper or Lower DIMENSIONS Length (cm)-Wound measurement along the vertical axis (head to toe is from 12:00 to 6:00) of the body. Width (cm)-Wound measurement along the horizontal axis (side to side is 3:00 to 9:00) of the body. Depth (cm)-Measurement from the top of the intact epidermis to the deepest part of a wound. Tunneling (cm) o A linear tract extending several times deeper than the wound opening. o Use clock positions to establish location within the wound. Undermining o Separation of the superficial or deep fascia from underlying tissues. o Separation of tissues creates a pocket that can collect wound exudate & prevents efficient removal. o Use clock positions to establish location around the wound. Clock positions-Use of the hour hands of a clock to denote locations of undermining; the head is 12:00, the foot is 6:00, & 9:00 & 3:00 are the lateral aspects. WOUND BED-The area of the wound contained within the borders of the viable epidermis. Granulation tissue (%) o Pink/red, moist tissue composed of new blood vessels, connective tissue, fibroblasts, & inflammatory cells, which fills an open, healing wound o Typically appears deep pink or red with an irregular, granular (bumpy) surface. Necrotic fibrous tissue/slough (%) o Soft, moist, devitalized, dead tissue; may be white, yellow, tan, brown, or green. o It may be loose or firmly adherent & has a stringy or fibrous texture & appearance. Eschar (%) o Black, brown, or gray necrotic, devitalized tissue. o It can be firmly adherent or separated from surrounding viable wound margins. o Eschar may be hard, soft or boggy. Hypertrophic o Excessive granulation tissue formation above the plane of surrounding healthy epidermis. Page 2 of 4
It prevents expedient reepithelialization of the wound bed.
WOUND MARGINS-The area immediately adjacent to the wound bed where epithelialization typically occurs. Wound length & width are measured from the margins. Epithelialized-complete-Total coverage of wound bed with epithelial cells. Epithelializing o The process of becoming covered with epithelial cells. o The new epithelial cells advance across the wound until they eventually meet epithelial cells moving in from the opposite direction. Rolled epithelium-Chronic, excessive epidermal growth along the wound border that does not extend into the wound bed. Callous-Typically painless thickening of the stratum corneum at locations of external pressure or friction. PERIWOUND-The tissues within 3 cm. of the wound Bruise (ecchymosis)-Black/blue/purple discoloration of skin caused by blood extravasation into subcutaneous tissues as a result of trauma to underlying vessels or fragility of vessel walls. Excoriation-Injury to epidermis or dermis caused by scratching, abrasion, or chemical/thermal burning. Induration-Hardening of tissue, especially the skin & superficial fascia, caused by edema, inflammation, &/or granulation. Inflammation o A protective response of the body to irritation or injury. o Cardinal signs of inflammation include redness, heat, swelling & pain. Intact-Epidermis & dermis without damage. Maceration-The softening or breaking down of skin resulting from prolonged exposure to moisture. Tape-skin tearing o Removal of epithelium caused by tape. o This is separate from epidermis removal related to shearing or pressure. EXUDATE-Fluid from a variety of sources that is discharged from the wound Type: Serous o Clear watery wound drainage. o Can be composed of blood plasma, intracellular or extracellular fluids, or a variety of other fluids. Sanguinous-Mostly bloody drainage with little, if any, serous fluid. Serosanguinous-A combination of serous & bloody drainage. Purulent (pus) o Creamy, viscous fluid primarily composed of polymorphonuclear leukocytes. o It is usually pale yellow to yellow green, sometimes whitish, bloody & is typically associated with infection. Amount: No drainage-Wound drainage that does not stain the dressing during routine dressing changes. Minimal-Wound drainage that mildly stains the dressing during routine dressing changes. Moderate-Wound drainage that has met the limit of the dressing's absorptive ability without saturating or leaking during routine & appropriate dressing change intervals. Heavy-Wound exudate that saturates a dressing during routine & appropriate dressing change intervals. IMPEDIMENTS TO HEALING Active tobacco use Page 3 of 4
PAIN
Blood glucose consistently above 200 mg/dL End of life Steroid use Limb ischemia Heavy disease burden-Multiple medical comorbidities that delay/stop wound healing. Infection-The invasion of body tissues by pathogenic organisms that reproduce & multiply, causing disease by local cellular injury, secretion of toxins, or antigen-antibody host reaction. Malnutrition-Nutritional status below what is needed for optimal wound healing. Noncompliance-Patient is unwilling or unable to make lifestyle changes that maximize wound healing.
Continuous-Pain at some level is always present. Episodic-Pain in response to some stimulus such as movement, dressing changes, or procedures. Level-Rating on a scale of 1 to 10.
DRESSING Dry-No strikethrough or leakage of wound exudate. Intact-Dressing is well-secured to the body. Leaking-Exudate is not contained within the dressing. Strikethrough-Exudate has penetrated the outermost level of the dressing but is not actively leaking. CURRENT GOAL OF THERAPY Compete resolution-Complete epithelialization of the wound with no drainage. Infection control-To prevent or lessen the damage of pathogenic organisms that invade the host tissues. Palliative care-Interventions designed to relieve/reduce the negative effects of a wound but not necessarily with the goal of complete healing. DEBRIDEMENT Autolytic-Removal of devitalized tissue accomplished by use of moisture-retentive dressings to accelerate the body's natural proteolytic debridement processes. Biologic-Removal of devitalized tissue by the external application of maggots. Enzymatic-Removal of devitalized tissue by the external application of proteolytic enzymes. Mechanical-Removal of devitalized tissue by physical forces (whirlpool, pulsatile lavage, wet/dry gauze). Sharp-Removal of devitalized tissue by a sharp instrument (scalpel, scissors). IMPRESSION Healed-Fully epithelialized wound or fully approximated incision with no discernible drainage. Improved-Overall wound characteristics have changed for the better. Initial assessment-First comprehensive assessment of the wound when a plan of care is formulated. Unchanged-No significant change in wound characteristics since the last comprehensive exam. Worsening-Deterioration of several wound aspects since the last comprehensive exam. Brown, G. (April 2006). Wound documentation: Managing risk. Advances in Skin & Wound Care, 159-162.
Page 4 of 4
You might also like
- Assessing Neurological FunctionDocument59 pagesAssessing Neurological FunctionSherlyn PedidaNo ratings yet
- Drug Classificati On Indications Action Route/Dos e Side Effects Patient Teaching Nursing ImplicationsDocument7 pagesDrug Classificati On Indications Action Route/Dos e Side Effects Patient Teaching Nursing ImplicationsJenny NguyenNo ratings yet
- Administering Vaccines To AdultsDocument1 pageAdministering Vaccines To AdultsPaul Anthony LoricaNo ratings yet
- Transport of Critically Ill Adults 2011Document1 pageTransport of Critically Ill Adults 2011velocity25No ratings yet
- VPD RashchrtDocument2 pagesVPD RashchrtMarco Ramos JacobNo ratings yet
- Drugclasses Pharmacologypart 1 PDFDocument25 pagesDrugclasses Pharmacologypart 1 PDFSutanya100% (2)
- 04 - Soft Tissue InjuriesDocument13 pages04 - Soft Tissue InjuriesCielo GriñoNo ratings yet
- Burn Stabilization ProtocolDocument2 pagesBurn Stabilization ProtocolAli AftabNo ratings yet
- Rashes in Children by Dr. Muhammad - RashidDocument43 pagesRashes in Children by Dr. Muhammad - RashidAli DkaliNo ratings yet
- Municable DiseasesDocument18 pagesMunicable DiseasesEdamarie ChuaNo ratings yet
- CL-078 Wound Assessment Guideline 2015Document35 pagesCL-078 Wound Assessment Guideline 2015JovialNo ratings yet
- Neonatal Assessmnt Tool PDFDocument2 pagesNeonatal Assessmnt Tool PDFYestin Reece Corpus ArcegaNo ratings yet
- Abnormal Menstruations AUB and Dysmenorrhea: Abebe C (MD)Document34 pagesAbnormal Menstruations AUB and Dysmenorrhea: Abebe C (MD)adam0% (1)
- Heat and Cold Applications: Physiological Response Therapeutic BenefitDocument2 pagesHeat and Cold Applications: Physiological Response Therapeutic BenefitKim Rose SabuclalaoNo ratings yet
- An Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFDocument6 pagesAn Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFkatherine dayagNo ratings yet
- Study Guide #10 With HEENT ChecklistDocument4 pagesStudy Guide #10 With HEENT ChecklistPrince DuNo ratings yet
- Combined Hormone Pill, Patch, Ring Progestin Only Mini Pill, Depo-Provera, IUDDocument1 pageCombined Hormone Pill, Patch, Ring Progestin Only Mini Pill, Depo-Provera, IUDnkuligowskiNo ratings yet
- Mastitis Teaching PlanDocument2 pagesMastitis Teaching Planapi-252910411No ratings yet
- A Child With WheezeDocument53 pagesA Child With WheezeCodillia CheongNo ratings yet
- Clinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants PDFDocument27 pagesClinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants PDFJonathan WelchNo ratings yet
- The Physiology of ShockDocument37 pagesThe Physiology of ShockGauxy AromboNo ratings yet
- Parenting Styles: - Dictatorial or AuthoritarianDocument45 pagesParenting Styles: - Dictatorial or AuthoritarianCourseTree LearningNo ratings yet
- A Premature NewbornDocument17 pagesA Premature NewbornMegatFitriAzizNo ratings yet
- Preventing Skin Damage and Pressure UlcersDocument29 pagesPreventing Skin Damage and Pressure UlcersJOSHUA DICHOSO100% (1)
- Homeostasis Temperature RegulationDocument22 pagesHomeostasis Temperature RegulationChris AllamNo ratings yet
- Blank Physical Assessment SheetDocument2 pagesBlank Physical Assessment SheetRenee Hickman RobinsonNo ratings yet
- Nephrotic Syndrome: Dinesh Kumar PDocument42 pagesNephrotic Syndrome: Dinesh Kumar PRiya Sweetsolitude100% (1)
- Muscle Strength TestingDocument3 pagesMuscle Strength TestingGiselle Chloe Baluya ico100% (1)
- Abdominal ExaminationDocument4 pagesAbdominal ExaminationdizhalfaNo ratings yet
- Nursing QuestionnairesDocument3 pagesNursing QuestionnairesDianne Marbella AlvaradoNo ratings yet
- Acute Renal FailureDocument30 pagesAcute Renal FailureJerinNo ratings yet
- The Heart's Chambers and ValvesDocument29 pagesThe Heart's Chambers and ValvesomarNo ratings yet
- Maternal and Child Heath: Jay Pee C. Malibiran Nurse 1 RNDocument36 pagesMaternal and Child Heath: Jay Pee C. Malibiran Nurse 1 RNRosebel Lagura100% (1)
- DVT Guide: Symptoms, Risks and TreatmentDocument9 pagesDVT Guide: Symptoms, Risks and TreatmentGladys YaresNo ratings yet
- Neurological AssessmentDocument23 pagesNeurological AssessmentNavjot BrarNo ratings yet
- Fall Risk Assess OsceDocument2 pagesFall Risk Assess OsceLamyaa Ali HasanNo ratings yet
- Function of G I System: The Primary Digestive Functions Are Break Down Food Particles "Document113 pagesFunction of G I System: The Primary Digestive Functions Are Break Down Food Particles "cherryann_12100% (1)
- Carpal Tunnel Syndrome Guide: Causes, Symptoms & TreatmentDocument12 pagesCarpal Tunnel Syndrome Guide: Causes, Symptoms & Treatmentyordin deontaNo ratings yet
- Seven steps to safer care: A route map for England & WalesDocument58 pagesSeven steps to safer care: A route map for England & WalesDanissa Fidia PuteriNo ratings yet
- ASSESSMENT FORM: Spring 2006 Client's Number: InstructionsDocument6 pagesASSESSMENT FORM: Spring 2006 Client's Number: Instructionsdenisemw88No ratings yet
- Nursing Assessment Form: A. Demographic DataDocument5 pagesNursing Assessment Form: A. Demographic Datacat_w0m4nNo ratings yet
- PT 3 Knee Special TestsDocument10 pagesPT 3 Knee Special TestsCristine RamosNo ratings yet
- Fluid Overload Student PagesDocument4 pagesFluid Overload Student PagesJess OswaldNo ratings yet
- Different Positions Assumed by A Patient During A Physical Examination ProcedureDocument14 pagesDifferent Positions Assumed by A Patient During A Physical Examination ProcedureAziil LiizaNo ratings yet
- Muscular System DisordersDocument36 pagesMuscular System DisordersShawn Henry CepedaNo ratings yet
- Concept Map 1Document2 pagesConcept Map 1yfortilus100% (1)
- Concepts and Prevention of Disease PDFDocument41 pagesConcepts and Prevention of Disease PDFAna Rika Javier Harder100% (1)
- Nasal Cavity. The Nasal Cavity, Also Known As TheDocument11 pagesNasal Cavity. The Nasal Cavity, Also Known As TheWilly Chandra HermawanNo ratings yet
- Anaphylaxis Shock: Bagian Anestesi FK UNISSULA SemarangDocument15 pagesAnaphylaxis Shock: Bagian Anestesi FK UNISSULA SemarangTeguh PambudiNo ratings yet
- BronchiolitisDocument12 pagesBronchiolitisEz BallNo ratings yet
- Rheumatic Fever Symptoms, Causes & TreatmentDocument15 pagesRheumatic Fever Symptoms, Causes & TreatmentEnas NeyazNo ratings yet
- Examination of The ThroatDocument10 pagesExamination of The Throatsejal3vijNo ratings yet
- Cranial NervesDocument2 pagesCranial NervesAbdallah Essam Al-ZireeniNo ratings yet
- What Is LeadershipDocument21 pagesWhat Is LeadershiptaapNo ratings yet
- Error of RefractionDocument3 pagesError of RefractionMargot SanchezNo ratings yet
- DiagnosticDocument5 pagesDiagnosticjustin_saneNo ratings yet
- Pressure Ulcer Prevention and TreatmentDocument51 pagesPressure Ulcer Prevention and TreatmentIosefina DudeanuNo ratings yet
- WOUND CARE and BANDAGINGDocument9 pagesWOUND CARE and BANDAGINGJane BelvisNo ratings yet
- Skin IntegrityDocument112 pagesSkin IntegrityHerlina NababanNo ratings yet
- Skin Care PowerpointDocument52 pagesSkin Care Powerpointisapatrick812667% (3)
- Apdchap5 Transferspositioningjan11Document23 pagesApdchap5 Transferspositioningjan11api-272722550No ratings yet
- Nursing Care Plan for Patient with Impaired Physical MobilityDocument4 pagesNursing Care Plan for Patient with Impaired Physical Mobilityssairej06100% (3)
- Caregiver's Handbook - Part 4 of 9 - Personal CareDocument4 pagesCaregiver's Handbook - Part 4 of 9 - Personal CareAlicja PNo ratings yet
- Impaired Physical MobilityDocument2 pagesImpaired Physical MobilityJayson OlileNo ratings yet
- Anatomy and Physiology Lesson 2Document9 pagesAnatomy and Physiology Lesson 2Kimberly Abellar LatoNo ratings yet
- Mobility Nursing Diagnosis GuideDocument3 pagesMobility Nursing Diagnosis GuideYan ReyesNo ratings yet
- 2012 AWMA Pan Pacific Guidelines PDFDocument124 pages2012 AWMA Pan Pacific Guidelines PDFMoenaIsmailNo ratings yet
- May 2018 Solutions 1Document154 pagesMay 2018 Solutions 1Anderson Alfred100% (2)
- Best Practice Recommendations For Holistic Strategies To Promote and Maintain Skin IntegrityDocument32 pagesBest Practice Recommendations For Holistic Strategies To Promote and Maintain Skin IntegrityisaNo ratings yet
- Bali Geriatric Symposium 2018 UpdateDocument40 pagesBali Geriatric Symposium 2018 UpdateMardikaNo ratings yet
- Acute and Chronic Wounds - Current Management Concepts (PDFDrive)Document1,872 pagesAcute and Chronic Wounds - Current Management Concepts (PDFDrive)Tasha FarahNo ratings yet
- MedicationsDocument23 pagesMedicationsYou know whoNo ratings yet
- Critical Care Nurse Skills ChecklistDocument4 pagesCritical Care Nurse Skills ChecklistmilanbojicNo ratings yet
- Piciorul Diabetic CursDocument59 pagesPiciorul Diabetic Cursmichelle misu100% (1)
- Patients Care and Comfort MeasuresDocument13 pagesPatients Care and Comfort Measurespedrofsr06No ratings yet
- Zimmer Traction HandbookDocument92 pagesZimmer Traction HandbookMohd Saufee0% (1)
- Jurnal Perawatan LukaDocument7 pagesJurnal Perawatan LukaBefrie Mahaztra SNo ratings yet
- 2011 Fall JCR International CatalogueDocument32 pages2011 Fall JCR International CatalogueJoao HeckerNo ratings yet
- NSE121 - Care PlanDocument7 pagesNSE121 - Care Planramyharoon2004No ratings yet
- Wound Care Test QuestionsDocument7 pagesWound Care Test QuestionsAngella sseruwagiNo ratings yet
- Pressure Ulcer Prevention Report 130528Document358 pagesPressure Ulcer Prevention Report 130528Agung GinanjarNo ratings yet
- NCPDocument3 pagesNCPTweenie DalumpinesNo ratings yet
- NURSING & HEALTH BREAKDOWN SPRING REVISIONDocument25 pagesNURSING & HEALTH BREAKDOWN SPRING REVISIONchantlex3No ratings yet
- Occt630 Occupational Profile InterventionDocument19 pagesOcct630 Occupational Profile Interventionapi-290880850No ratings yet
- The Dangers of Faecal Incontinence in The At-Risk PatientDocument6 pagesThe Dangers of Faecal Incontinence in The At-Risk PatientRicardo BalauNo ratings yet
- Structured Nursing Rounds (SNR) Training Module On The Level of Patient SatisfactionDocument5 pagesStructured Nursing Rounds (SNR) Training Module On The Level of Patient SatisfactionMalarvizhi SureshNo ratings yet
- Stacy - Neurology FinalDocument13 pagesStacy - Neurology Finalapi-242547654No ratings yet
- Scope of The Problem: DefinitionsDocument34 pagesScope of The Problem: DefinitionsDecky AndreaNo ratings yet
- 5867 19344 1 PBDocument10 pages5867 19344 1 PBjerayneNo ratings yet
- CV - Mahbub MishuDocument3 pagesCV - Mahbub MishuMahbub Chowdhury MishuNo ratings yet