Professional Documents
Culture Documents
Functional Diarrhea - Some Answers To Often Asked Questions
Uploaded by
Dewi Puji AstutikOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Functional Diarrhea - Some Answers To Often Asked Questions
Uploaded by
Dewi Puji AstutikCopyright:
Available Formats
International Foundation for Functional Gastrointestinal Disorders
IFFGD 700 W. Virginia St., #201 Milwaukee, WI 53204 Phone: 414-964-1799 Toll-Free (In the U.S.): 888-964-2001 Fax: 414-964-7176 Internet: www.iffgd.org
Diarrhea (105)
Copyright 1994-2012 by the International Foundation for Functional Gastrointestinal Disorders Revised and Updated by Author, 2009
Functional Diarrhea - Some Answers to Often Asked Questions
By: Arnold Wald, M.D., M.A.C.G., A.G.A.F., University of Wisconsin School of Medicine and Public Health, Madison, WI
What is Diarrhea? For clinical purposes, diarrhea is defined as an abnormal looseness of stools and/or increase in frequency of bowel movements. On the basis of surveys of normal populations, more than three bowel movements per day exceeds normal frequency but is not sufficient. A better definition is the frequent passage of unformed stool that takes the form of the container that it is collected in. If diarrhea lasts longer than three weeks, it is classified as chronic. If no specific cause is found after a thorough investigation and certain criteria are met, a diagnosis of functional diarrhea may be considered. What are Functional Bowel Disorders? Patients with functional bowel disorders do not demonstrate physical or laboratory abnormalities to explain their GI symptoms. One example of a functional bowel disorder is Irritable Bowel Syndrome (IBS), which is estimated to affect approximately 1520% of all adults. Is Functional Diarrhea the Same as Irritable Bowel Syndrome? Patients with functional diarrhea may represent a subgroup of patients with IBS. Patients with IBS often complain of altered bowel habits, including diarrhea and/or constipation, associated with abdominal pain, bloating, rectal urgency, straining, or a sense of incomplete evacuation. Many of these symptoms occur in patients with functional diarrhea but the absence of abdominal pain distinguishes these patients from those with IBS.
What is the Evaluation for Patients with Functional Diarrhea? The most important aspect of the workup is a thorough medical history, including use of medicines and dietary habits, and a careful physical examination. Additional studies such as blood tests and stool analysis may be ordered. Diagnostic procedures such as colonoscopy or endoscopy may be indicated, allowing the physician to examine the inner surface of the colon and small intestine to exclude other causes of chronic diarrhea, such as infections or inflammation of the colon or small intestinal diseases. Why is the Medical and Dietary History so Important? A diagnosis of functional diarrhea is made only after other possible causes, such as medications and diet induced diarrhea, are excluded. The list of medications which cause diarrhea is extensive and includes certain antibiotics, magnesium containing antacids, blood pressure lowering agents (including beta-blockers, ACE inhibitors), and drugs to control irregular heart beat (quinidine). All medications, whether prescription or over the counter, should be brought to the attention of the physician. Although some patients are sensitive to wheat and other related grains (Celiac disease, gluten enteropathy), true food allergies are rare. However, inability to completely absorb certain food groups can, if they are eaten in sufficient quantities, lead to diarrhea in susceptible subjects. Milk (lactose) intolerance is one of the more common examples of this. Patients with lactose intolerance have low levels of intestinal lactase, the enzyme required to
digest the milk sugar, lactose. The unabsorbed sugar then passes to the colon where it is broken down by bacteria to produce abdominal gas (bloating) and diarrhea. Whether a person develops symptoms depends on many factors including the amount of lactose ingested and the levels of lactase enzyme in the small intestine. Treatment involves reducing or eliminating lactose in the diet or using commercial products that contain the lactase enzyme. Other persons are intolerant of fructose (found in fruit and fruit juices), sorbitol (plums, pears and sugarless gum), and caffeine (coffee, tea, many sodas). Dietary elimination of possible offending agents may resolve symptoms in sensitive persons. What Other Factors May Worsen Functional Diarrhea? Some patients develop diarrhea after undergoing stomach or gallbladder surgery. The exact mechanisms are unclear, but are thought to involve increased transport of food through the GI tract or an increase in bile salts delivered to the colon. A condition called runners diarrhea has been described. As the name suggests, these individuals experience diarrhea during long distance marathons. The cause is uncertain but may involve alterations of GI motor activity. What is the Cause of Functional Diarrhea? Although there is no consensus, one proposed mechanism relates to alterations in gastrointestinal motility. Contractions of the smooth muscle of the gastrointestinal tract regulate movement of food through the small intestine and colon. Patients with functional diarrhea may have different motility patterns than do patients without diarrhea. However, the causes of the motility dysfunction and changes in intestinal fluid absorption leading to firmer stools or to diarrhea are incompletely understood.
What Treatments are Available for Functional Diarrhea? As the cause(s) of functional diarrhea is (are) unknown, treatment is symptomatic. Dietary modifications include elimination of various substances known to cause diarrhea. In addition to lactose, fructose, sorbitol, and caffeine some patients develop symptoms because they do not completely digest complex carbohydrates (pasta, beans). These too may be reduced in the diet to see if there is any improvement. Some patients with IBS and diarrhea may benefit from an increase in dietary fiber. In contrast, other patients benefit from carbohydrate restriction, as was shown in a recent study by investigators at the University of North Carolina, Chapel Hill. For patients who do not improve with dietary modifications, antidiarrheal agents such as loperamide (Imodium), diphenoxylate (Lomotil), and codeine are often effective. All work by similar mechanisms. In general, these drugs are used under the supervision of a physician; all but loperamide require a doctors prescription. As future research uncovers the mechanisms which underlie functional diarrhea, more specific therapies will be developed. As with many functional disorders, a trusting physician-patient relationship should enhance the treatment of this complex problem and promote a better understanding of the dynamics of GI symptoms.
Opinions expressed are an authors own and not necessarily those of the International Foundation for Functional Gastrointestinal Disorders (IFFGD). IFFGD does not guarantee or endorse any product in this publication nor any claim made by an author and disclaims all liability relating thereto. This article is in no way intended to replace the knowledge or diagnosis of your doctor. We advise seeing a physician whenever a health problem arises requiring an expert's care. IFFGD is a nonprofit education and research organization. Our mission is to inform, assist, and support people affected by gastrointestinal disorders. For more information, or permission to reprint this article, write to IFFGD, 700 W. Virginia St., #201, Milwaukee, WI 53204. Call toll-free (in the U.S.) 888-964-2001 or 414-964-1799. Visit our websites at: www.iffgd.org or www.aboutibs.org.
You might also like
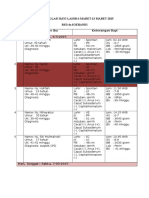
- Jadwal Jaga Malam Periode 23 Maret 2015 - 31 Mei 2015Document6 pagesJadwal Jaga Malam Periode 23 Maret 2015 - 31 Mei 2015Dewi Puji AstutikNo ratings yet
- List Judul RefegfratDocument1 pageList Judul RefegfratDewi Puji AstutikNo ratings yet
- Rekapitulasi Bayi Lahir 6 Maret-13 Maret 2015 RSD DR - SoebandiDocument8 pagesRekapitulasi Bayi Lahir 6 Maret-13 Maret 2015 RSD DR - SoebandiDewi Puji AstutikNo ratings yet
- Kesling 2 1 04Document15 pagesKesling 2 1 04kuatsudrajatNo ratings yet
- Evaluation and Treatment of Women With HirsutismDocument8 pagesEvaluation and Treatment of Women With HirsutismDewi Puji AstutikNo ratings yet
- GFJGV KufDocument1 pageGFJGV KufDewi Puji AstutikNo ratings yet
- 3Document1 page3Dewi Puji AstutikNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- BLUE-Protocol and FALLS-Protocol: Two Applications of Lung Ultrasound in The Critically IllDocument12 pagesBLUE-Protocol and FALLS-Protocol: Two Applications of Lung Ultrasound in The Critically IllChristiaan CordovaNo ratings yet
- Medical Training: - Ventilation Options - For Internal Use OnlyDocument43 pagesMedical Training: - Ventilation Options - For Internal Use OnlyKamel HadyNo ratings yet
- 2009-2010 Boards ReviewDocument108 pages2009-2010 Boards Reviewanuj sharmaNo ratings yet
- Mariam Burchuladze: Group 7 / Reflection EssayDocument1 pageMariam Burchuladze: Group 7 / Reflection EssayMariam BurchuladzeNo ratings yet
- Chapter 50: Nursing Management: Endocrine Problems Test BankDocument16 pagesChapter 50: Nursing Management: Endocrine Problems Test BankPrince K. TaileyNo ratings yet
- Blurred VisionDocument7 pagesBlurred VisionRichi CiriacoNo ratings yet
- Rogers 2017Document29 pagesRogers 2017UmerNo ratings yet
- Low Back Pain SyndromeDocument244 pagesLow Back Pain Syndromebrunettebomshell100% (4)
- Oet 2.0 ReadingDocument7 pagesOet 2.0 ReadingSibi JohnyNo ratings yet
- Physical Assessment:: Area Technique Norms Findings Analysis and Interpretation A. SkullDocument15 pagesPhysical Assessment:: Area Technique Norms Findings Analysis and Interpretation A. SkullRoseben SomidoNo ratings yet
- Book 44 - Non VerbalDocument103 pagesBook 44 - Non VerbalcamcromanceNo ratings yet
- 11 Core Competencies in NursingDocument4 pages11 Core Competencies in NursingMikhael Jay IglesiasNo ratings yet
- FibromyalgiaDocument85 pagesFibromyalgiamariuscornel100% (1)
- Cohort 1Document25 pagesCohort 1jaish8904No ratings yet
- Nurs Fpx 4010 Assessment 3 Interdisciplinary Plan ProposalDocument5 pagesNurs Fpx 4010 Assessment 3 Interdisciplinary Plan Proposalfarwaamjad771No ratings yet
- Types of Stomas and Loop Ostomy CareDocument8 pagesTypes of Stomas and Loop Ostomy CareRadhiyatul Ashiqeen Binti MoktarNo ratings yet
- Eob2 Drug PDFDocument2 pagesEob2 Drug PDFBayu PrabowoNo ratings yet
- MLN CatalogDocument24 pagesMLN CatalogLhingboi100% (1)
- Bab I.First Aid: PPSDM MigasDocument31 pagesBab I.First Aid: PPSDM MigasacidafdolaNo ratings yet
- Postpartum BluesDocument17 pagesPostpartum BluesVeliani Putri anggrainiNo ratings yet
- Trauma Reactions in ChildrenDocument2 pagesTrauma Reactions in ChildrenAlesha Rose100% (2)
- Dry Needling Doc. Jan 18,13Document1 pageDry Needling Doc. Jan 18,13Rebecca SchirberNo ratings yet
- Basic Life SupportDocument33 pagesBasic Life SupportayudewintasariNo ratings yet
- The Growing Hospital's Journey To A Good Governance: OCTOBER 9, 2019Document17 pagesThe Growing Hospital's Journey To A Good Governance: OCTOBER 9, 2019Solo ReyesNo ratings yet
- Mycetoma Grading ScoringDocument5 pagesMycetoma Grading ScoringSahana R100% (1)
- Acute Bioligic CrisisDocument141 pagesAcute Bioligic CrisisJanelle MatamorosaNo ratings yet
- Chapter 33 Theory of Mind 3Document12 pagesChapter 33 Theory of Mind 3Costrut Laur100% (3)
- Patho Respiratory - KatherineDocument9 pagesPatho Respiratory - KatherineKayla MayerNo ratings yet
- Bruxism (Tooth Grinding) in Adults: SymptomsDocument3 pagesBruxism (Tooth Grinding) in Adults: SymptomsalgaipNo ratings yet
- Essay - What Does Love MeanDocument8 pagesEssay - What Does Love MeanHasan HusejnovicNo ratings yet