Professional Documents
Culture Documents
Immunoprophylaxis Against Infectious Diseases
Uploaded by
Examville.comCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Immunoprophylaxis Against Infectious Diseases
Uploaded by
Examville.comCopyright:
Available Formats
APPLIED MICROBIOLOGY
Immunoprophylaxis against Infectious Diseases
Prevention of infections depends upon three concepts:
• Elimination of source of infection
• Prevention of transmission of infective agents
• Protection of susceptible persons by active or passive immunization
Vaccine is an immunobiological substance designed to confer specific protection against a disease. It
stimulates the immune system (either humoral or cell mediated or both) to generate specific protection
against an infectious agent. Vaccines may be prepared from live modified organisms, inactivated or killed
organisms, toxoids or combination of these.
Live Versus Killed Vaccines
Live attenuated as well as inactivated vaccines for different diseases are available. The former are also
called as replicating and the latter as non-replicating vaccines. The live vaccines are prepared from live
and generally attenuated organisms which have lost their ability to induce disease but retain their
immunogenicity. In general, live vaccines are more potent immunizing agents because of following
reasons:
a. Can multiply in the host thus increasing the antigen dose manifold.
b. Possess all major and minor antigenic components.
c. Occupy natural niches for the pathogen in the body thus blocking colonization by the pathogen.
d. May persist for longer time in the body in latent stages.
The killed vaccines are prepared by subjecting the organism to the action of physical or chemical agents.
These are usually safe but generally less efficacious than the live vaccines.
Differences between Attenuated and Inactivated vaccines
Feature Attenuated Inactivated
Preparation Attenuation Inactivation
Administration
Route Usually natural route Parenteral
Dose May be single Usually multiple
Adjuvant Not required Usually required
Safety May revert to virulence Safe
Cold chain requirement ++++ ++
Cost Low High
Duration of immunity Usually long May long or short
Immune response
Humoral IgG, IgA Mainly IgG
CMI + Little or no
Adverse reactions to vaccines
Normal toxicity
Faulty production Abnormal inherent toxicity
Presence of foreign toxin
Bacterial contamination
Wrong culture used
Viral contamination
Faulty administration Use of nonsterile apparatus
Contamination from operator
Allergy Local
Serum sickness
Neurological illness
General anaphylaxis
Other causes Abnormal sensitivity of vaccine
Indirect effects
Damage to fetus
Provocation of disease
Contraindications to Vaccinations
WHO has recommended a limited number of contraindications to vaccinations as summarized below:
a. Immunization should be delayed in case of severe illness with fever, so that any sign of illness will
not be attributed to the vaccination.
Malnutrition, moderate fever, respiratory infections, common diarrhoea and any other benign
ailment do not constitute contraindication for vaccination.
Hospitalized children may receive necessary vaccinations before their discharge, and, in some
cases, immediately following admission, particularly in the presence of nosocomial measles risk.
b. Discontinuation of DPT immunization is recommended in case of occurrence of a severe
postvaccinal reaction as collapse, shock, fever above 40.5°C, convulsions and other neurological
symptoms.
Diarrhoea is not considered a contraindication for oral poliomyelitis vaccination. Extra doses cor-
responding to those administered during the bout of diarrhoea should be given.
c. No live vaccine is to be given to a person with an immunodeficiency or undergoing
immunosuppressive treatment, corticosteroids therapy, radiotherapy, antimetabolite therapy, etc.
d. Measles, mumps or rubella immunization should be delayed for at least six weeks when a recent
injection of polyvalent immunoglobulin has been given.
IMMUNOGLOBULINS AND ANTISERA Immunoglobulins (Ig)
Two types of immunoglobulins are available: normal human Ig and specific human Ig. Normal human Ig
is an antibody rich fraction obtained from a pool of at least 1000 people. The preparation is rich in IgG,
almost whole of which is in free form (and not in aggregates). It contains very little of IgA. Normal
human Ig is administered to prevent measles in highly susceptible individuals and to provide temporary
protection (up to 12 weeks) against hepatitis A infection for travelers to endemic area and to contacts of
case of hepatitis A in an outbreak. There should be a gap of 3 months between the administration of
normal Ig and any live vaccine.
Specific human immunoglobulins are prepared from the plasma of patients who have recently recovered
from infection or who have been immunized against a specific infection. The plasma of donor should
contain at least five times the amount of specific antibody as is present in standard reference serum.
The immunoglobulins are usually given intramuscularly. Peak blood levels are reached in two days after
intramuscular injection. The average half-life is 20-35 days. Generally immunoglobulins should not be
given just before or after active immunization.
National Immunization Schedule
Every country has devised a schedule for immunizing children against common infectious diseases (which
have been included in EPI of WHO) to obtain optimal results with the available resources. As per WHO
recommendations one dose of BCG, three doses of combined OPT vaccine, three (if possible additional
zero dose at birth) doses of oral poliovaccine and one dose of measles vaccine is to be given to the child in
his first year of life to protect him against these six diseases. Of these BCG is given as soon after the birth
as is possible along with a dose of OPV. OPT is injected from the age of 6 weeks onwards with a gap of
four weeks each between three doses. Each injection of OPT is accompanied by a dose of OPV to reduce
the contact of child with health functionary. Vaccine against measles is given on the completion of 9
months of age. Upto the age of 9 months, a child is protected against measles by the antibodies passively
transferred to child from the mother.
You might also like
- The American Jobs Act (Full Text From The White House)Document199 pagesThe American Jobs Act (Full Text From The White House)Examville.comNo ratings yet
- Algebra Cheat SheetDocument2 pagesAlgebra Cheat SheetDino97% (72)
- Amazing Math TricksDocument22 pagesAmazing Math TricksExamville.comNo ratings yet
- Chemical BondingDocument33 pagesChemical BondingExamville.comNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument22 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreYoAmoNYCNo ratings yet
- Basic Math and Pre-Algebra Cheat SheetDocument34 pagesBasic Math and Pre-Algebra Cheat SheetExamville.com100% (1)
- Periodic TableDocument1 pagePeriodic TableRoy Cartagena CorderoNo ratings yet
- Chemical Bonding - Important Concepts in Inorganic ChemistryDocument34 pagesChemical Bonding - Important Concepts in Inorganic ChemistryExamville.comNo ratings yet
- Concentration Cheat SheetDocument2 pagesConcentration Cheat Sheetcontact2web50% (2)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- What Are Enzymes - Examville Study GuidesDocument13 pagesWhat Are Enzymes - Examville Study GuidesExamville.comNo ratings yet
- Building Successful Business GrowthDocument16 pagesBuilding Successful Business GrowthExamville.comNo ratings yet
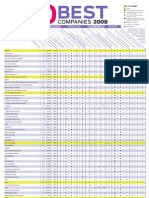
- 100 Best Women Friendly CompaniesDocument1 page100 Best Women Friendly CompaniesExamville.com100% (1)
- Global Education Digest UNESCODocument154 pagesGlobal Education Digest UNESCOExamville.com100% (1)
- Organic Chemistry Introduction Examville - Com Study Guides SectionDocument19 pagesOrganic Chemistry Introduction Examville - Com Study Guides SectionExamville.comNo ratings yet
- Online Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreDocument27 pagesOnline Practice Tests, Live Classes, Tutoring, Study Guides Q&A, Premium Content and MoreExamville.comNo ratings yet
- Start Up Customer Development ProcessDocument28 pagesStart Up Customer Development ProcessExamville.comNo ratings yet
- Quick Introduction To Organic Chemistry Examville - Com Study GuidesDocument27 pagesQuick Introduction To Organic Chemistry Examville - Com Study GuidesExamville.comNo ratings yet
- Business ModelsDocument42 pagesBusiness ModelsExamville.comNo ratings yet
- Top Universities in The WorldDocument6 pagesTop Universities in The WorldExamville.com75% (4)
- Free To Paid UsersDocument169 pagesFree To Paid UsersExamville.comNo ratings yet
- Kinematic Equations - Examville - Com Study Guides SectionDocument10 pagesKinematic Equations - Examville - Com Study Guides SectionExamville.comNo ratings yet
- Organic Chemistry Review Examville - Com Study AidsDocument25 pagesOrganic Chemistry Review Examville - Com Study AidsExamville.comNo ratings yet
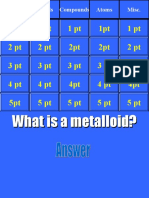
- Chemistry Jeopardy - Examville - Com Study Guides SectionDocument52 pagesChemistry Jeopardy - Examville - Com Study Guides SectionExamville.comNo ratings yet
- Total Synthesis - Organic Chemistry Notes atDocument40 pagesTotal Synthesis - Organic Chemistry Notes atExamville.comNo ratings yet
- Chemistry - Elements, Terminologies and More - Examville - Com Study Guides SectionDocument47 pagesChemistry - Elements, Terminologies and More - Examville - Com Study Guides SectionExamville.comNo ratings yet
- Synthesis - Organic Chemistry Notes atDocument76 pagesSynthesis - Organic Chemistry Notes atExamville.comNo ratings yet
- Triglycerides - Organic Chemistry Notes atDocument56 pagesTriglycerides - Organic Chemistry Notes atExamville.comNo ratings yet
- Substrate Control - Organic Chemistry Notes atDocument39 pagesSubstrate Control - Organic Chemistry Notes atExamville.comNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Postpartum Discharge PlanDocument3 pagesPostpartum Discharge PlanCassey CamamaNo ratings yet
- Estimated Time of Death:: Cooling of The BodyDocument2 pagesEstimated Time of Death:: Cooling of The BodynoramalinaabdmanafNo ratings yet
- Sanaani Nur Hathi M. Nso Jugular Venous Oximetry Staff Nurse 1Document7 pagesSanaani Nur Hathi M. Nso Jugular Venous Oximetry Staff Nurse 1Nur SanaaniNo ratings yet
- Abdominal NodesDocument8 pagesAbdominal NodesatihsaNo ratings yet
- Refeeding SyndromeDocument10 pagesRefeeding SyndromeEstefany GonzalezNo ratings yet
- Approach To The Adult With Unspecified Knee Pain - UpToDateDocument55 pagesApproach To The Adult With Unspecified Knee Pain - UpToDateCamila Gomes Santos MoraesNo ratings yet
- NCMB 312 Rle MS Final Exam ReviewerDocument50 pagesNCMB 312 Rle MS Final Exam Reviewer2-YA-4 ABEGAEL FERNANDEZNo ratings yet
- Agaches Measuring The Skin Non-Invasive Investigations, Physiology, Normal Constants (Philippe Humbert, Ferial Fanian Etc.) (Z-Library)Document1,622 pagesAgaches Measuring The Skin Non-Invasive Investigations, Physiology, Normal Constants (Philippe Humbert, Ferial Fanian Etc.) (Z-Library)irina obrejaNo ratings yet
- Ano RectalDocument57 pagesAno Rectaldrhemantt1279100% (1)
- Study Guide FCM 1 Part BDocument6 pagesStudy Guide FCM 1 Part Bpranaji100% (3)
- Cancer Protocol for Spooky2 CoilDocument9 pagesCancer Protocol for Spooky2 CoilFlavio Galib100% (2)
- Workplace First-Aid Program GuideDocument28 pagesWorkplace First-Aid Program Guidehpss77100% (1)
- AssignmentDocument9 pagesAssignmentTenzin Norzom NegiNo ratings yet
- Principle Principle PrincipleDocument12 pagesPrinciple Principle PrincipleDarshana JuvekarNo ratings yet
- Itrack Advance BrochureDocument2 pagesItrack Advance BrochureHaag-Streit UK (HS-UK)No ratings yet
- 2022 Mechanical Ventilation From Pathophysiology To Clinical EvidenceDocument422 pages2022 Mechanical Ventilation From Pathophysiology To Clinical EvidenceJose Castellon67% (3)
- Revised Children's Anxiety and Depression Scale (And Subscales) (Rcads)Document6 pagesRevised Children's Anxiety and Depression Scale (And Subscales) (Rcads)e_nov78No ratings yet
- Essential Oils For BronchitisDocument26 pagesEssential Oils For BronchitissanjaigNo ratings yet
- Question Preparation Exam2023-1Document350 pagesQuestion Preparation Exam2023-1alicNo ratings yet
- What Is The Female Reproductive System?: External PartsDocument3 pagesWhat Is The Female Reproductive System?: External PartsKeneth Dave AglibutNo ratings yet
- Aminoglycoside Dosing Guide 2019-05-20 PDFDocument10 pagesAminoglycoside Dosing Guide 2019-05-20 PDFAbu Hammoud AlyazeediNo ratings yet
- MBF90324234Document407 pagesMBF90324234Emad Mergan100% (1)
- Warfarin LeafletDocument2 pagesWarfarin LeafletchampbeeNo ratings yet
- London Core Review Course - (Thurs 18 May - Sun 21 May 2017) - TimetableDocument5 pagesLondon Core Review Course - (Thurs 18 May - Sun 21 May 2017) - Timetablelondon_core_reviewNo ratings yet
- Pregnancy Regulation and Fertility TestingDocument17 pagesPregnancy Regulation and Fertility TestingSanti Deliani RahmawatiNo ratings yet
- Please Fill This Story Below Into The Partogram CompletelyDocument1 pagePlease Fill This Story Below Into The Partogram CompletelydwindoksmNo ratings yet
- Continuum - Key Points (All Topics)Document379 pagesContinuum - Key Points (All Topics)vigneshkumar.r3850No ratings yet
- Chest Pain ProtocolDocument7 pagesChest Pain Protocolomar kmr97No ratings yet
- Research in Autism Spectrum Disorders: Johnny L. Matson, Jennifer Beighley, Nicole TuryginDocument6 pagesResearch in Autism Spectrum Disorders: Johnny L. Matson, Jennifer Beighley, Nicole Turyginjhernandez8394No ratings yet
- Sandra M. Nettina MSN ANP BC Lippincott Manual of Nursing Practice Handbook 2005 LWWDocument1,109 pagesSandra M. Nettina MSN ANP BC Lippincott Manual of Nursing Practice Handbook 2005 LWWJoan Ano CaneteNo ratings yet