Professional Documents
Culture Documents
Rhu Day 1 Requirements
Uploaded by
Hanya Bint PotawanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rhu Day 1 Requirements
Uploaded by
Hanya Bint PotawanCopyright:
Available Formats
---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------ESTIMATED DATE OF DELIVERY It is impossible to predict the day an infant will be born with a high degree of accuracy.
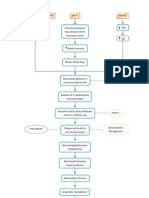
Traditionally, this date has been referred to as the estimated date of confinement (EDC). Because women are no longer confined after childbirth, the abbreviation EDB (estimated date of birth) or EDD (estimated date of delivery) is more commonly used today. Fewer than 5% of pregnancies end exactly 280 days from the last menstrual period; fewer than half end within 1 week of the 280th day. If fertilization occurred early in a menstrual cycle, the pregnancy will probably end early; if ovulation and fertilization occurred later in the cycle, the pregnancy will end late. Because of these normal variations, a pregnancy ending 2 weeks before or 2 weeks after the calculated EDB is considered well within the normal limit (38 to 42 weeks). Gestational age wheels or birth date calculators, which can be used to predict a birth date, are available. Nagele's rule is the standard method used to predict the length of a pregnancy. Nagele's Rule To calculate the date of birth by this rule, count backward 3 calendar months from the first day of the last menstrual period and add 7 days. For example, if the last menstrual period began May 15, you would count back 3 months (April 15, March 15, February 15) and add 7 days, to arrive at a date of birth of February 22. ---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------LEOPOLDS MANEUVER (ABDOMINAL EXAMINATION) - is a systematic method of observation and palpation to determine fetal position, presentation, lie and attitude. It is preferably performed after 24 weeks gestation when fetal outline can be palpated. Keen observation of abdomen should give data about: - longest diameter in appearance (longest diameter (axis) is the length of the fetus) - location of apparent fetal movement (the location of the activity most likely reflects the position of the feet) PREPARATION - Cardinal Rule: Instruct woman to empty bladder first. This will promotes comfort and allows for more productive palpation because fetal contour will not be obscured by a distended bladder - Place woman in dorsal recumbent position, supine with knee flexed to relax abdominal muscles. Place a small pillow under the head for comfort - Drape properly to maintain privacy - Explain procedures to gain patients cooperation - Warm hands first by rubbing them together before placing them over the womans abdomen to aid comfort. Cold hands may stimulate uterine contractions - Use the palm for palpation not fingers - During the first three maneuvers, stand facing the patients. For the last maneuver, stand facing patients feet THE FOUR MANEUVERS 1st Maneuver: Fundal Grip: What fetal pole or part occupies the fundus? - palpation of the fundal area to determine which fetal part is located in the uterine fundus - to determine the presenting part or presentation (part of the fetus lying over the inlet) Procedure 1. Nurse stands at the side of the bed, facing the client 2. Using both hands, feel for the fetal part lying in the fundus Findings The nurse-midwife should ascertain what is lying at the fundus by feeling the upper abdomen (fundus) with tips of both hands. Generally, she will find there is a mass, which will either be the head or the buttocks (breech) of he fetus. The nurse-midwife must decide which pole of the fetus; it is by observing three points: a. b. c. Relative consistency - the head is harder/ firmer than the breech Shape - if the head, it will be round and hard, and the transverse groove of the neck may be felt. The breech has no groove and usually feels more angular Mobility - the head will move independently of the trunk; but the breech moves only in conjunction with the body.
If the nurse-midwife feels the head, the fetus is in breech presentation; if the nurse-midwife feels the buttocks, it means the fetus is in vertex presentation 2nd Maneuver: Umbilical Grip: Which side is the fetal back? - to locate/identify the fetal back in relation to the right and left sides of the mother - to determine the fetal position (the relationship of the presenting part to one of the quadrants of the mothers pelvis Procedure 1. The nurse-midwife places the palmar surfaces of both hands on either side of the abdomen. 2. With left palm stationary on the left side of the abdomen to steady the uterus the right palpates the right side of the uterus on a circular motion from top to lower segment of the uterus applying gentle but deep pressure to palpate the fetal outline and small fetal parts 3. The nurse-midwife then reverses her hands. Findings - Small fetal parts (knees and elbows) feel nodular with numerous angular nodulations - Fetal back feels smooth, hard, like a resistant surface 3rd Maneuver: Pawliks Grip: What fetal part lies above the pelvic inlet? - determine if the presenting part has entered the pelvis (engagement of presenting part) - to find the head at the pelvis and to determine the mobility of the presenting part Procedure 1. Nurse-midwife stands at the side of the bed, facing the client 2. It should be conducted by gently grasping the lower portion of the abdomen, just above the symphysis pubis, between the thumb and the two fingers of one hand and then pressing together slightly and make gentle movements from side to side Findings - If the presenting part moves, round, balottable and easily displaced it is not yet engaged. If the presenting part is not movable felts as relatively fixed, knoblike part, it is engaged. - If it is firm, it must be the head. If soft, it could be breech 4th maneuver: Pelvic Grip: Which side is the cephalic prominence?
to determines the degree of fetal head flexion or extension to determine the attitude or habitus (degree of flexion of the fetal body, head and extremities, or the relationship of fetal parts to ach other) to determine the fetal descent should only be done if fetus is in cephalic presentation. Information about the infants anteioposterior position may also be gained from this final maneuver
Procedure 1. The nurse-midwife faces the feet of the client 2. Place one hand each on either side of the lower pole of the uterus 3. Palpate the fetal head by pressing downward about 2 inches above the inguinal ligament 4. Use both hands Findings - If descended deeply, only a small portion of the fetal head will be palpated. - If cephalic prominence or brow or the baby is on the same side of the small fetal parts, the head is flexed. - If the cephalic prominence is on the same side of the fetal back, the head is extended ---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------MEASUREMENT OF FUNDAL HEIGHT At about 12 to 14 weeks of pregnancy, the uterus is palpable over the symphysis pubis as a firm globular sphere. It reaches the umbilicus at 20 to 22 weeks and the xyphoid process at 36 weeks, and then often returns to about 4 cm below the yiphoid due to lightening at 40 weeks. If the woman is past 12 weeks of a pregnancy, palpate the fundus location, measure the fundal height (from the notch above the symphysis pubis to the superior aspect of the uterine fundus), and plot the height on a graph.. Plotting uterine growth at each visit can help detect any unusual variation in fetal growth. If an abnormality is detected, further investigation with ultrasound can be done to determine the cause of the unusual increase or decrease in growth. McDonald's rule, a symphysis-fundal height measurement, although not thoroughly documented to be reliable, is a common method of determining, during midpregnancy, that a fetus is growing in utero. Typically, the distance from the uterine fundus to the symphysis pubis in centimeters is equal to the week of gestation between the 20th and 31st weeks of pregnancy. McDonald's rule becomes inaccurate during the third trimester of pregnancy because the fetus is growing more in weight than in height during this time. Until then, a fundal height much greater than this standard suggests multiple pregnancy, a miscalculated due date, a large-for-gestational-age infant, hydramnios (increased amniotic fluid volume), or possibly even hydatidiform mole (see Chapter 15). A fundal measurement much less than this suggests that either the fetus is failing to thrive (intrauterine growth restriction), the pregnancy length was miscalculated, or an anomaly, such as anencephaly, has developed. Determining and recording that the fundus has reached typical milestone measurements, such as over the symphysis pubis at 12 weeks, at the umbilicus at 20 weeks, and at the xiphoid process at 36 weeks, is also helpful. ---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------FETAL HEART TONE (FHT) MONITORING Fetal hearts beat at 120 to 160 beats per minute throughout pregnancy. Fetal heart sounds can be heard and counted as early as the 10th to 11th week of pregnancy by the use of an ultrasonic Doppler technique. ASSESSMENT 1. Rhythm Strip Testing - is the assessment of the fetal heart rate for whether a good baseline rate and long- and short-term variability are present. The baseline reading refers to the average rate of the fetal heartbeat per minute. Short-term variability (also called beat-to-beat variability) denotes the small changes in rate that occur from second to second if the fetal parasympathetic nervous system is receiving adequate oxygen and nutrients. Long-term variability denotes the differences in heart rate that occur over the 20-minute time period. Thus, it reflects the state of the fetal sympathetic nervous system. 2. Nonstress Test - measures the response of the fetal heart rate to fetal movement. The woman is positioned and the fetal heart rate and uterine contraction monitors are attached as for obtaining a rhythm strip. The woman pushes a button attached to the monitor (similar to a call bell) whenever she feels the fetus move. When the fetus moves, the fetal heart rate should increase about 15 beats per minute and remain elevated for 15 seconds. It should decrease to its average rate again as the fetus quiets. If no increase in beats per minute is noticeable on fetal movement, poor oxygen perfusion of the fetus is suggested. 3. Contraction Stress Testing - analyzes the fetal heart rate in conjunction with contractions. Contractions are initiated by nipple stimulation. With external uterine contraction and fetal heart rate monitors in place, the baseline fetal heart rate is obtained. Next, the mother rolls a nipple between her finger and thumb until uterine contractions begin. Three contractions with a duration of 40 seconds or longer must be present in a 10-minute window before the test can be interpreted. The test is negative (normal) if no fetal heart rate decelerations are present with contractions. It is positive (abnormal) if 50% or more of contractions cause a late deceleration (a dip in fetal heart rate that occurs toward the end of a contraction and continues after the contraction). ---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------TETANUS TOXOID IMMUNIZATION GUIDE AND DOSAGE
---------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------HEALTH TEACHING PLAN General Health Teaching Specific Health Teaching
1. Self-Care Needs
Bathing Daily tub baths or showers are recommended. As pregnancy advances, a woman may have difficulty maintaining her balance when getting in and out of a bathtub. If so, she should change to showering or sponge bathing for her own safety. If membranes rupture or vaginal bleeding is present, tub baths are contraindicated because then there might be a danger of contamination of uterine contents. During the last month of pregnancy, when the cervix may begin to dilate, tub bathing is restricted. Breast Care A few precautions during pregnancy are helpful to prevent breast discomfort. A general rule is for a woman to wear a firm, supportive bra with wide straps to spread weight across the shoulders. A woman may need to buy a larger bra halfway through pregnancy to accommodate increased breast size. If she plans on breast-feeding her newborn, she might choose to buy bras suitable for breast-feeding so she can continue to use them after the baby's birth. At about the 16th week of pregnancy, colostrum secretion begins in the breasts. Instruct her to wash her breasts with clear tap water (no soap, because that could be drying) daily to remove the colostrum and reduce the risk of infection. Afterward, she should dry her nipples well by patting them. If colostrum secretion is profuse, a woman may need to place gauze squares or breast pads inside her bra, changing them frequently to maintain dryness. Dental Care Gingival tissue tends to hypertrophy during pregnancy. Unless a pregnant woman brushes well, pockets of plaque form readily between the enlarged gumline and teeth. In addition, encourage pregnant women to see their dentists regularly for routine examination and cleaning. Encourage the woman to snack on nutritious foods, such as fresh fruits and vegetables like apples and carrots to avoid sugar coming in contact with the teeth. If a client has trouble avoiding sweet snacks such as candy, suggest eating sweet snacks that dissolve easily (like a chocolate bar) rather than those that remain in the mouth a long time (like chewy candy). This helps to minimize the level of sugar in the mouth. Perineal Hygiene Although women have increased vaginal discharge during pregnancy, douching is contraindicated because the force of the irrigating fluid could cause it to enter the cervix and lead to infection. In addition, douching alters the pH of the vagina, leading to an increased risk of bacterial growth. Dressing A woman should avoid garters, extremely firm girdles with panty legs, and knee-high stockings because these may impede lower-extremity circulation. Suggest wearing shoes with a moderate to low heel to minimize pelvic tilt and possible backache.
2. Sexual Activity
Some women are embarrassed to ask questions about sexual relations during pregnancy. However, most women are concerned about whether sexual intercourse should be restricted. Many need information to refute some of the myths about sexual relations in pregnancy that still exist, such as: Coitus on the expected date of her period will initiate labor. Orgasm will initiate labor, but participating in sexual relations without orgasm will not. Coitus during the fertile days of a cycle will cause a second pregnancy or twins. Coitus might cause rupture of the membranes. None of these is true. Then you can help dispel these myths, allowing a woman to feel more comfortable and secure that coitus is not harming her child. Women with a history of spontaneous miscarriage may be advised to avoid coitus during the time of the pregnancy when a previous miscarriage occurred. Women whose membranes have ruptured or who have vaginal spotting should be advised against coitus until examined to prevent possible infection. Advise caution about male oralfemale genital contact, because accidental air embolism has been reported from this act during pregnancy. Otherwise, there are no sexual restrictions during pregnancy.
3. Exercise
Exercise during pregnancy is important to prevent circulatory stasis in the lower extremities. It also can offer a general feeling of well-being. Both pregnant and nonpregnant women should exercise at 70% to 85% of their maximum heart rate. Teach the client how to assess quickly if she is exercising too strenuously by evaluating her ability to continue talking while exercising. If she is too short of breath to do this, she is exercising beyond her target heart rate. A planned exercise program may have long-term benefits such as: Lowered cholesterol level Reduced risk of osteoporosis Increased energy level Maintenance of healthy body weight Decreased risk of heart disease Increased self-esteem and well-being
4. Sleep
The optimal condition for body growth occurs when growth hormone secretion is at its highest levelthat is, during sleep. If a woman has trouble falling asleep, drinking a glass of warm milk may help. Relaxation exercises (lying quietly, systematically relaxing neck muscles, shoulder muscles, arm muscles, and so on) also may be effective. She also may awaken with pyrosis or dyspnea if she has been lying flat. In this instance, sleeping on two pillows or on a couch with an armrest may be helpful. To obtain enough sleep and rest during pregnancy, most pregnant women need a rest period during the afternoon as well as a full night of sleep. A good resting or sleeping position is a modified Sims' position, with the top leg forward. Be certain the client knows to avoid resting in a supine position, as supine hypotension syndrome (faintness, diaphoresis, and hypotension from the pressure of the expanding uterus on the inferior vena cava) can develop in this position. Also be certain she knows not to rest with her knees sharply bent either when sitting or lying down, because of the increased risk of venous stasis this causes below the knee.
5. Employment
Remember, most women work to augment or supply the family income, not for fun. Counseling them to reserve periods during the day for rest and to eat a healthy diet is more effective than suggesting they resign from their jobs during pregnancy to get more rest
6. Travel
If a woman is susceptible to motion sickness, she should not take any medication for this unless it is specifically prescribed or approved by her physician or nurse-midwife. Caution her not to eat uncooked fruits, vegetables, and meat or drink unpurified water. If she is going to be away from home for an extended time, she needs to make arrangements to visit a health care provider in that area so she can keep the schedule of her regular prenatal visits. Encourage her to make these plans far enough in advance so that her records can be copied and sent with her or be forwarded to the interim health care provider. Be aware that you need her written permission to send records. Also, make sure she has enough of her prescribed vitamin supplement plus adequate prescriptions for refills as necessary. Advise a woman who is taking a long trip by automobile to plan for frequent rest or stretch periods. Pregnant women may drive as long as they fit comfortably behind the steering wheel. They should use seat belts like everyone else. Both shoulder harnesses and lap belts should be used. The lap belt should be worn as snugly as comfortable so that it fits under the abdominal bulge and across the pelvic bones. The shoulder harness should be snug but comfortable, worn across the shoulder, chest, and upper abdomen. A pad may be placed under the shoulder harness at the neck to avoid chafing.
7. Nutrition
Nurses can help the nation to achieve these goals by stressing the importance of a balanced diet for all people so women enter pregnancy with adequate nutritional stores. They can help pregnant women plan ways to ingest adequate iron daily and to remember to take their prenatal vitamin (which contains an iron and folic acid supplement) daily. During pregnancy, a woman must eat adequately to supply enough nutrients to the fetus, so it can grow, as well as to support her own nutrition. Adequate protein intake is vital because so much is needed by a fetus.
REFERENCES: Pillitteri, A. (2009) Maternal and Child Health Nursing, 6th ed. WHO (2004) Core Information for the Development of Immunization Policy.
You might also like
- Ineffective Cerebral Tissue PerfusionDocument3 pagesIneffective Cerebral Tissue PerfusionHanya Bint Potawan88% (25)
- Preparing for a Gentle Birth: The Pelvis in PregnancyFrom EverandPreparing for a Gentle Birth: The Pelvis in PregnancyRating: 4 out of 5 stars4/5 (8)
- Leopold' ManeuversDocument3 pagesLeopold' Maneuversjava_biscocho122995% (22)
- DocumentsDocument22 pagesDocumentsDivina D Galvez-BeronioNo ratings yet
- Schizophrenia UndifferentiatedDocument88 pagesSchizophrenia UndifferentiatedHanya Bint Potawan75% (4)
- Impaired Gas ExchangeDocument2 pagesImpaired Gas ExchangeHanya Bint PotawanNo ratings yet
- Impaired Skin IntegrityDocument1 pageImpaired Skin IntegrityHanya Bint PotawanNo ratings yet
- E-The Obstetric ExaminationDocument57 pagesE-The Obstetric ExaminationAbhilasha Solomon100% (3)
- Breech Presentation June 2023Document59 pagesBreech Presentation June 2023Imbodi TiliyeNo ratings yet
- Our Daily Bread - LEOPOLDDocument4 pagesOur Daily Bread - LEOPOLDJonas Marvin AnaqueNo ratings yet
- LEOPOLD's MANEUVER RATIONALEDocument3 pagesLEOPOLD's MANEUVER RATIONALEAngela AquisapNo ratings yet
- Care of Mother and Adolescent Well Client RLE Skills Lab ReviewerGonzalesDocument22 pagesCare of Mother and Adolescent Well Client RLE Skills Lab ReviewerGonzalesKarl LintanNo ratings yet
- Nursing Care of a Family During Labor and BirthDocument22 pagesNursing Care of a Family During Labor and BirthiMaibelle BelleNo ratings yet
- Maternal and Child NursingDocument23 pagesMaternal and Child Nursingdesh08No ratings yet
- Group II Makati Medical Center m8 1Document107 pagesGroup II Makati Medical Center m8 1CASSANDRAJUL VARINNo ratings yet
- Obs - GynaecDocument18 pagesObs - GynaecNathalie DeebNo ratings yet
- Dubowitz Ballard Score CHeRP 2007Document1 pageDubowitz Ballard Score CHeRP 2007istinengtiyasNo ratings yet
- Labor and Delivery CMCC NotesDocument12 pagesLabor and Delivery CMCC Notesrcestabillo6949100% (1)
- CH 15 Labor and Birth Part 1 HANDOUTDocument5 pagesCH 15 Labor and Birth Part 1 HANDOUTEula ReyesNo ratings yet
- Intrapartum Monitoring, Intrapartum Care and Normal Delivery 10Document77 pagesIntrapartum Monitoring, Intrapartum Care and Normal Delivery 10Austine OdhiamboNo ratings yet
- Leopolds-Maneuver StudentsDocument40 pagesLeopolds-Maneuver StudentsCarlo GacadNo ratings yet
- MCN Lab - M7 - INTRAPARTUM CARE 2020-2021Document28 pagesMCN Lab - M7 - INTRAPARTUM CARE 2020-2021Kristine Kim100% (1)
- Pregnancy: Signs and Symptoms Detection of Abnormalities Diagnosis, Physio Changes, CareDocument67 pagesPregnancy: Signs and Symptoms Detection of Abnormalities Diagnosis, Physio Changes, CareJovim Cervantes LanaNo ratings yet
- Intrapartum 2003Document76 pagesIntrapartum 2003Karla Jane100% (2)
- Braxton Hicks Contractions or False Labor: ST STDocument10 pagesBraxton Hicks Contractions or False Labor: ST STKristine Jade OdtujanNo ratings yet
- Finals 1. Maternal and Child Nursing - IntrapartumDocument11 pagesFinals 1. Maternal and Child Nursing - IntrapartumAlgen GayapNo ratings yet
- Caring for Women During ChildbirthDocument5 pagesCaring for Women During ChildbirthMarie PotayreNo ratings yet
- Intrapartum (Process of Labor Delivery)Document206 pagesIntrapartum (Process of Labor Delivery)coosa liquorsNo ratings yet
- Ballard ScoreDocument7 pagesBallard ScoreAndre OpaNo ratings yet
- Obstetrics & Gyn II PDF Abnormal PDFDocument305 pagesObstetrics & Gyn II PDF Abnormal PDFmaezu100% (3)
- INTRAPARTUMDocument27 pagesINTRAPARTUMLea Jane ArmeñaNo ratings yet
- LaborDocument22 pagesLaborHussain H. HussainNo ratings yet
- RLE MODULE - Gyne KarlDocument14 pagesRLE MODULE - Gyne KarlKristian Karl Bautista Kiw-isNo ratings yet
- Unit 4 Obg SubmissionDocument35 pagesUnit 4 Obg SubmissionSavita HanamsagarNo ratings yet
- How To Perform LeopoldDocument5 pagesHow To Perform LeopoldChared Lumba100% (3)
- LaborDocument45 pagesLaborDakayu Amin LugitNo ratings yet
- LaborDocument25 pagesLaborSameera DahamNo ratings yet
- Intra PartumDocument93 pagesIntra Partumjared gabuleNo ratings yet
- Breech PresentationDocument40 pagesBreech PresentationShuhada Wahab100% (3)
- Breech Presentation ManagementDocument16 pagesBreech Presentation Managementhussain AltaherNo ratings yet
- Intrapartum QuizletDocument15 pagesIntrapartum Quizletanon_616227840100% (3)
- Maternal&Fetal Assessment in LaborDocument49 pagesMaternal&Fetal Assessment in LaborAccounting PdfilesNo ratings yet
- zBREECH PRESENTATION AND DELIVERYDocument5 pageszBREECH PRESENTATION AND DELIVERYAlbert Francis BialaNo ratings yet
- Position of The Fetus's Head During Its Passage in Labor. These Are Described in Relation To A VertexDocument4 pagesPosition of The Fetus's Head During Its Passage in Labor. These Are Described in Relation To A VertexMadalina PitropNo ratings yet
- ManueversDocument97 pagesManueverscataleya mesaNo ratings yet
- Conduct of Normal Labor and DeliveryDocument141 pagesConduct of Normal Labor and DeliveryRea Dominique CabanillaNo ratings yet
- Breech PresentationDocument57 pagesBreech PresentationShailendra Yadav100% (2)
- INTRAPARTUM 1 (The Childbearing FamilyDocument7 pagesINTRAPARTUM 1 (The Childbearing FamilyBonbon TanNo ratings yet
- Obstetric Physical ExaminationDocument17 pagesObstetric Physical ExaminationYusnida Rahmawati100% (1)
- DR PretestDocument5 pagesDR PretestCrystal Ann TadiamonNo ratings yet
- LaborDocument69 pagesLaborzamurd76No ratings yet
- Leopods ManeuverDocument8 pagesLeopods ManeuverDaryl Adrian RecaidoNo ratings yet
- Thank you for the informative presentation on shoulder dystocia. Let me know if you have any other questionsDocument39 pagesThank you for the informative presentation on shoulder dystocia. Let me know if you have any other questionsDewina Dyani Rosari IINo ratings yet
- CS - Forceps - VacuumDocument3 pagesCS - Forceps - VacuumBench AvilaNo ratings yet
- Intrapartal Period: Theories of Labor Onset and Factors Affecting the Labor ProcessDocument80 pagesIntrapartal Period: Theories of Labor Onset and Factors Affecting the Labor ProcessEpilepsy ManNo ratings yet
- Intra PartumDocument138 pagesIntra Partumzhanniesy31No ratings yet
- Leopold's Maneuvers GuideDocument13 pagesLeopold's Maneuvers GuideFatima Diane S. MondejarNo ratings yet
- Routine Vaginal Delivery GuideDocument2 pagesRoutine Vaginal Delivery Guidetf2112100% (1)
- Holistic Childbirth Manual: Maternal Health Manuals, #2From EverandHolistic Childbirth Manual: Maternal Health Manuals, #2No ratings yet
- Scorpio Training: Kettlebell Exercises: The Way of the ScorpioFrom EverandScorpio Training: Kettlebell Exercises: The Way of the ScorpioNo ratings yet
- Newborn Baby: A Guide on how to Prepare for your Newborn Baby. Proper Feeding, Sleeping, and Care: A+ ParentingFrom EverandNewborn Baby: A Guide on how to Prepare for your Newborn Baby. Proper Feeding, Sleeping, and Care: A+ ParentingRating: 5 out of 5 stars5/5 (4)
- Impaired Physical MobilityDocument2 pagesImpaired Physical MobilityHanya Bint PotawanNo ratings yet
- Hanieyah Guro OR DR PRC FormatDocument4 pagesHanieyah Guro OR DR PRC FormatHanya Bint PotawanNo ratings yet
- Impaired Verbal and or Written CommunicationDocument2 pagesImpaired Verbal and or Written CommunicationHanya Bint Potawan100% (1)
- Pa Tho Physiology - Type 1 Diabetes (Hanieyah Guro)Document1 pagePa Tho Physiology - Type 1 Diabetes (Hanieyah Guro)Hanya Bint PotawanNo ratings yet
- Rhu Day 1 RequirementsDocument4 pagesRhu Day 1 RequirementsHanya Bint PotawanNo ratings yet
- Herbal MedicinesDocument6 pagesHerbal MedicinesHanya Bint PotawanNo ratings yet
- BSN - 4C: PresentorsDocument52 pagesBSN - 4C: PresentorsHanya Bint Potawan100% (1)
- Herbal MedicinesDocument6 pagesHerbal MedicinesHanya Bint PotawanNo ratings yet
- Psychotropic DrugsDocument49 pagesPsychotropic DrugsHanya Bint PotawanNo ratings yet
- Rhu Day 1 RequirementsDocument4 pagesRhu Day 1 RequirementsHanya Bint PotawanNo ratings yet
- MSHC Ordr PRC FormatDocument4 pagesMSHC Ordr PRC FormatHanya Bint PotawanNo ratings yet
- Impaired Breathing PatternDocument1 pageImpaired Breathing PatternHanya Bint PotawanNo ratings yet
- DOH Officials Directory Execom MembersDocument2 pagesDOH Officials Directory Execom MembersHanya Bint PotawanNo ratings yet
- Ineffective Airway ClearanceDocument2 pagesIneffective Airway ClearanceHanya Bint PotawanNo ratings yet
- Dopamine HydrochlorideDocument1 pageDopamine HydrochlorideJoannes SanchezNo ratings yet
- Angina PectorisDocument2 pagesAngina PectorisHanya Bint PotawanNo ratings yet
- Akiya - DiphtheriaDocument52 pagesAkiya - DiphtheriaHanya Bint PotawanNo ratings yet
- Jose Rizal: 'Those Who Cannot See Where They Came From Will Never Get To Where They Are Going.'Document55 pagesJose Rizal: 'Those Who Cannot See Where They Came From Will Never Get To Where They Are Going.'Anne Ginez BilledoNo ratings yet
- Mr. Bean's diagnostic blood test resultsDocument2 pagesMr. Bean's diagnostic blood test resultsHanya Bint PotawanNo ratings yet