Professional Documents
Culture Documents
Pathophysiology of Pain
Uploaded by
Nickol BaylonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pathophysiology of Pain
Uploaded by
Nickol BaylonCopyright:
Available Formats
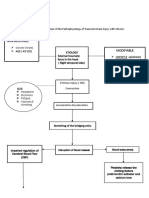
Pathophysiology of Pain
Pain Receptors
Pain receptors are found on free nerve endings located in many tissues throughout the body. This includes skin, muscles, joints, connective tissues, and internal organs. Pain receptors are activated in response to a painful stimulus, usually involving tissue damage. Once activated, pain receptors release chemicals called neurotransmitters that send information about the painful stimulus along nerves to the spinal cord and the brain. This entire process of pain transmission is called nociception, and the pain receptors found in tissues are called nociceptors. The substances that are released from damaged tissues and activate nociceptors are called second messengers. Important second messengers include bradykinin, prostaglandins,histamine, serotonin, leukotrienes, and potassium. Some of these second messengers are inhibited by pain medications. If a drug inhibits the release of second messengers, then the pain receptors will not be activated, the pain impulse will not reach the brain, and the person will not perceive pain from the damaged tissue. The peripheral nerve fibers that contain pain receptors are afferent nerves. This means that they send nerve impulses towards the brain and spinal cord. There are two main types of afferent nociceptors in the tissues: A-delta and C-sensory fibers. The A-delta fibers are myelinated nerves. Myelinated nerves transmit pain impulses very quickly. Pain receptors on A-delta fibers are activated in response to sharp, welllocalized pain that requires an immediate reaction. This type of painful stimulus is sometimes referred to as somatic pain, and it usually involves damage to skin or muscle.
Theories of Pain
Historical theories Before the relatively recent discovery of neurons and their role in pain, various different body functions were proposed to account for pain. There were several competing early theories of pain among the ancient Greeks: Aristotle believed that pain was due to evil spirits entering the body through injury, and Hippocrates believed that it was due to an imbalance in vital fluids. In the 11th century, Avicenna theorized that there were a number of feeling senses including touch, pain and titillation, but prior to the scientific Renaissance in Europe pain was not well-understood, and it was thought that pain originated outside the body, perhaps as a punishment from God. In 1644, Ren Descartes theorized that pain was a disturbance that passed down along nerve fibers until the disturbance reached the brain, a development that transformed the perception of pain from a spiritual, mystical experience to a physical, mechanical sensation. Descartes's work, along with Avicenna's, prefigured the 19th-century development of specificity theory. Specificity theory saw pain as "a specific sensation, with its own sensory apparatus independent of touch and other senses". Another theory that came to prominence in the 18th and 19th centuries was intensive theory, which conceived of pain not as a unique sensory modality, but an emotional state produced by
stronger than normal stimuli such as intense light, pressure or temperature. By the mid1890s, specificity was backed mostly by physiologists and physicians, and the intensive theory was mostly backed by psychologists. However, after a series of clinical observations by Henry Head and experiments by Max von Frey, the psychologists migrated to specificity almost en masse, and by century's end, most textbooks on physiology and psychology were presenting pain specificity as fact. In 1955, DC Sinclair and G Weddell developed "peripheral pattern theory", based on a 1934 suggestion by John Paul Nafe. They proposed that all skin fiber endings (with the exception of those innervating hair cells) are identical, and that pain is produced by intense stimulation of these fibers. Another 20th-century theory was "gate control" theory, introduced by Ronald Melzack and Patrick Wall in the 1965 Science article "Pain Mechanisms: A New Theory. The authors proposed that both thin (pain) and large diameter (touch, pressure, vibration) nerve fibers carry information from the site of injury to two destinations in the dorsal horn of the spinal cord, and that the more large fiber activity relative to thin fiber activity at the inhibitory cell, the less pain is felt. Both peripheral pattern theory and gate control theory have been superseded by more modern theories of pain.
Gate Control theory
According to this theory, nociceptive impulses are transmitted to the spinal cord through large A delta and small C- fibers These fibers create synapses in the SG The cells in this structure function as a gate, regulating transmission of impulses to CNS Stimulation of larger nerve fibers (A-alfa, A-beta) causes the cells in SG to close the gate". A closed gate decreases stimulation of T-cells (the 2nd afferent neuron), which decreases transmission of impulses, and diminishes pain perception. Stimulation of small fiber input inhibits cells in SG and "open the gate". An open gate increases the stimulation of T-cells transmission of impulses enhances pain perception In addition to gate control through large and small fibers stimulation, the central nervous system, through efferent pathways, may close, partially close, or open gate. Cognitive functioning may thus modulate pain perception.
Theory today Regions of the cerebral cortex associated with pain. "Intensive" theory, that a pain signal can be generated by intense enough stimulation of any sensory receptor, has been soundly disproved. In humans, the detection of peripheral pain begins at free nerve endings. It is here that the polymodal pain receptors TRPA1, TRPV1, TRPV2, ASICs, and high threshold mechanoreceptors detect noxious stimuli such as strong mechanical forces, H+, K+, chemicals, and temperature. Some nociceptors do not differentiate noxious from non-noxious stimuli, while others respond only to painfully intense stimuli. The sensation of pain then travels from the periphery to the spinal cord along A-delta and C fibers. Because the A-delta fiber is thicker than the C fiber and is thinly sheathed in an electrically insulating material (myelin), it carries its signal faster (530 m/s) than the unmyelinated C fiber (0.52 m/s). Pain evoked by the (faster) A-delta fibers is described as sharp and is felt first. This is followed by a duller pain, often described as burning, carried by the C fibers. These first order neurons enter the spinal cord via Lissauer's tract. A-delta and C fibers synapse on second order neurons in substantia gelatinosa(laminae II and III of the dorsal horns). These second order neurons (spinothalamic tract) then decussate, crossing via the anterior white commissurebefore ascending contra laterally. Before reaching the brain, the spinothalamic tract splits into the lateral neospinothalamic tract and the medial paleospinothalamic tract. Second order neospinothalamic tract neurons carry information from A-delta fibers and terminate at the ventral posterolateral nucleus of the thalamus, where they synapse on third order neurons (dendrites of the somatosensory cortex). Paleospinothalamic neurons carry information from C fibers and terminate throughout the brain stem, a tenth of them in the thalamus and the rest in the medulla, pons and periaqueductal grey matter. Spinal cord fibers dedicated to carrying A-delta fiber pain signals, and others that carry both A-delta and C fiber pain signals up the spinal cord to the thalamus in the brain have been identified. Other spinal cord fibers, known as wide dynamic range neurons, respond to A-delta and C fibers, but also to the large A-beta fibers that carry touch, pressure and vibration signals. Pain-related activity in the thalamus spreads to the insular cortex (thought to embody, among other things, the feeling that distinguishes pain from other homeostatic emotions such as itch and nausea) and anterior cingulate cortex (thought to embody, among other things, the motivational element of pain); and pain that is distinctly located also activates the primary and secondary somatosensory cortices. Melzack and Casey's 1968 picture of the dimensions of pain is as influential today as ever, firmly framing theory and guiding research in the functional neuroanatomy and psychology of pain. A. D. (Bud) Craig and Derek Denton include pain in a class of feelings they name, respectively, "homeostatic" or "primordial" emotions. These are feelings such as hunger,
thirst and fatigue, evoked by internal body states, communicated to the central nervous system by interoceptors, which motivate behavior aimed at maintaining the internal milieu at its ideal state. Craig and Denton distinguish these feelings from the "classical emotions" such as love, fear and anger, which are elicited by environmental stimuli sensed through the nose, eyes and ears.
Pain Pathway
Pain messages are two-way traffic. Inhibitory effects are achieved through the descending pathways, which reach from the conscious brain down to the gates in the subconscious brain and the spinal cord. The reason for this is that the gates are places where the flow of pain messages can be controlled or influenced By sending responses
back to the periphery, the brain can ordered the release of chemicals that have analgesic effects, which can reduces or inhibit pain sensation. Pain generally starts with a physical event; a cut, burn, tear, or bump. The sensation of pain usually depends on the activation of a set of neurons that includes primary afferent nociceptors, interneurons in the spinal cord, cells of the ascending tracts, thalamic neurons and neurons of the cerebral cortex. Hence, the pain system involves a set of ascending pathways that convey nociceptive information from peripheral nociceptors to higher levels of the central nervous system, as well as descending pathways that modulate that information. The term nociception refers to the process by which pain information is carried from the periphery sense receptors in the skin and in the viscera to the cerebral cortex through network of neuronal relays. Exteroceptors on the body surface and propioceptors within the body are specialized neurons that receive stimulation; mechanical (e.g. pressure), chemical, electrical, or thermal (i.e. hot-cold sensitive). The body is equipped with mechanical nociceptors at the periphery (so-called first-order neurons), which project to second-order neurons in the spinal cord and medulla, which then carries the sensory information (in the form of electrical impulse) to the thalamus, where it synapses with third-order neurons that transmit the impulse to the cortex. Second-order neurons send their sensory inputs to the thalamus via two ascending pathways: the dorsal column medial-lemniscal system and the anterolateral system (includes the spinothalamic, spinoreticular, and spinotectal fibers). The former transmits impulse involving position sense, touch, and pressure. The latter pathway is involved in pain transmission. The spinal cord is the central concourse along which all pain messages travels to and from the brain. For example, when you stub your toe and your peripheral nerves register alarm, this acute pain is immediately relayed along the nerve fibers of your foot and leg to the substantia gelatinosa located within the dorsal horn of the spinal cord. The cells in the substantia gelatinosa relay this "fast pain" message along the neospinothalamic and terminating it the thalamus and the cortex. The cortex is the region in which thoughts are processed. In contrast, chronic pain moves along a different and slower tract, called the paleospinothalamic tract. This "slow pain" is generally dull, aching, burning, and cramping. Slow pain follows the same path as the fast pain through the spinal cord, but once in the brain, it separates and terminates in the hypothalamus and the limbic structures. The hypothalamus is responsible for stimulating the release of stress hormones. The limbic structures are the places where emotions are processed. Just as there is an ascending pain pathway from the body to the brain, there is a descending pathway that allows the brain to modulate pain sensory. The brain uses this pathway to send chemical substances and nerve impulses back down to the cells in the
spinal cord to act against the pain message sent up by the pain receptors. Hence, the primarily role of the descending pathway is to send chemical messages from the brain to close the gates in the spinal cord to ascending messages. Descending inhibitory processes are of great interest in the research arena. Hence, it has been extensively studied by scientists. For instance, descending inhibitory processes have been investigated in anesthetized animals. It was found that the firing of dorsal horn neurons in response to noxious skin heating can be inhibited by stimulation in the periaqueductal gray (PAG) and the lateral reticular formation (LRF) in the midbrain. In addition, inhibition of the spinal cord neurons can also be achieved by electrical stimulation in other regions of the brain, such as the raphe nuclei, the locus coeruleus, and various regions of the medullary reticular formation, as well as sites in the hypothalamus, septum, orbital cortex, and sensorimotor cortex. Reaction: I have learned the pathophysiologys of pain where in it will start first as a stimulus, the example of stimulus are chemical, physical and thermal. This will stimulate the nocireceptors and pain receptors. Unmyelinated C Fibers will transmits the stimulation it wil pass thorough the dorsal root ganglia and through the spinal cord passing the dorsal horns then in the spinal cord synapses it will produce a reflex for the occurrence of pain. This response is called the motor or efferent response. Then it will go through the paleospinothalamic tract to the ascending tract. The tract is connected with the reticular formation, the pons and medulla. It will stimulate the awareness and the alertness. Ascend to the somatic sensory in cerebral cortex, this is the location and characteristic of pain perceived. Then the body response to the pain, there are two kind of response the emotional which include crying, moaning, and anger while the other one is the physical response the rigidity, guarding and behavior changes. In this research it also tackles about the theories related to pain, I have learn the gate control theory where in, nociceptive impulses are transmitted to the spinal cord through large A delta and small C- fibers These fibers create synapses in the SG The cells in this structure function as a gate, regulating transmission of impulses to CNS Stimulation of larger nerve fibers (Aalfa, A-beta) causes the cells in SG to close the gate". A closed gate decreases stimulation of T-cells (the 2nd afferent neuron), which decreases transmission of impulses, and diminishes pain perception. There are also two pathways of pain the ascending pathway and the descending pathway. Ive also learned that pain receptors are found on free nerve endings located in many tissues throughout the body. This includes skin, muscles, joints, connective tissues, and internal organs. Pain receptors are activated in response to a painful stimulus, usually involving tissue damage. Once activated, pain receptors release chemicals called neurotransmitters that send information about the painful stimulus along nerves to the spinal cord and the brain. This entire process of pain transmission is called nociception, and the pain receptors found in tissues are called nociceptors.
Pathophysiology of pain Pain receptors Pain theories Pain pathways
Submitted to: Prof. Dona Idang Submitted by: Baylon, Anne Nickol R. BSN406 Group 21A
You might also like
- Case Presentation On Scrub TyphusDocument31 pagesCase Presentation On Scrub TyphusManojNo ratings yet
- Feeding JejunostomyDocument4 pagesFeeding JejunostomyAbuNo ratings yet
- Pathophysiology of Myasthenia GravisDocument21 pagesPathophysiology of Myasthenia GravisNielArmstrong100% (2)
- Asthma Nanda Diagnoses Goals InterventionsDocument4 pagesAsthma Nanda Diagnoses Goals InterventionsZinya RobinsonNo ratings yet
- Pain ManagementDocument2 pagesPain ManagementprokunoNo ratings yet
- Acute Inflammatory Demyelinating PolyneuropathyDocument55 pagesAcute Inflammatory Demyelinating PolyneuropathyImmanuel100% (1)
- Pathophysiology of Brain Injury: Predisposing Factors: Precipitating FactorsDocument4 pagesPathophysiology of Brain Injury: Predisposing Factors: Precipitating FactorsHoney Lorie D. Simbajon100% (2)
- Appendicitis NCPDocument5 pagesAppendicitis NCPEarl Joseph DezaNo ratings yet
- Antiemetic Drug - PresentationDocument14 pagesAntiemetic Drug - PresentationYue Chen100% (1)
- Case Presentation About Spinal Shock SyndromeDocument56 pagesCase Presentation About Spinal Shock SyndromeAstral_edge010100% (1)
- Manage Bronchiectasis Nursing Care PlanDocument5 pagesManage Bronchiectasis Nursing Care PlanPaola Marie VenusNo ratings yet
- DX Infective Endocarditis PDFDocument7 pagesDX Infective Endocarditis PDFSherree HayesNo ratings yet
- Pre Post Operative Care of AppendicectomyDocument20 pagesPre Post Operative Care of AppendicectomyAngel DamoNo ratings yet
- Case Report - Deep Vein ThrombosisDocument12 pagesCase Report - Deep Vein ThrombosisAndi Meidin AnugerahNo ratings yet
- Assessment of The Peripheral Vascular SystemDocument17 pagesAssessment of The Peripheral Vascular SystemgrailbadNo ratings yet
- Tuberculosis Case StudyDocument43 pagesTuberculosis Case StudyAJIgama100% (1)
- Anatomy and Physiology PneumoniaDocument4 pagesAnatomy and Physiology PneumoniaJohnson MallibagoNo ratings yet
- 51 100Document18 pages51 100Jaessa Feliciano100% (1)
- Belles Palsy Case Study Group 1Document36 pagesBelles Palsy Case Study Group 1JOEY MEAD ARUGAY100% (1)
- Pathophysiology of Acute PancreatitisDocument1 pagePathophysiology of Acute PancreatitisHarvin FrancoNo ratings yet
- Discuss Nursing Interventions That Prevent Complications of ImmobilityDocument19 pagesDiscuss Nursing Interventions That Prevent Complications of ImmobilityLilly Ann Vaughan50% (2)
- Trixie - Anatomy and Physiology (Brain Tumor)Document4 pagesTrixie - Anatomy and Physiology (Brain Tumor)Trixie Marie Sabile AbdullaNo ratings yet
- Pathophysiology of Chemical BurnDocument3 pagesPathophysiology of Chemical Burnnursing concept maps100% (2)
- Small Bowel Obstruction Concept MapDocument1 pageSmall Bowel Obstruction Concept MapTessa Claire JaranowskiNo ratings yet
- Cerebral Palsy AnatomyDocument5 pagesCerebral Palsy AnatomyIoana irimiaNo ratings yet
- Scientific Explanation of Expected Outcomes and InterventionsDocument4 pagesScientific Explanation of Expected Outcomes and InterventionsGensen Cu RoxasNo ratings yet
- P 398Document1 pageP 398Arup Ratan PaulNo ratings yet
- Case Report-Hemorragic Stroke-Fitra RulianDocument29 pagesCase Report-Hemorragic Stroke-Fitra RuliannabiyaNo ratings yet
- Rheumatic Joint Disease Study GuideDocument18 pagesRheumatic Joint Disease Study Guidechalinsammy1No ratings yet
- NCPDocument9 pagesNCPKarell Eunice Estrellado Gutierrez100% (1)
- Asthma Patient ProfileDocument8 pagesAsthma Patient ProfileGlenn Asuncion PagaduanNo ratings yet
- Gerontologic Health Promotion ActivityDocument3 pagesGerontologic Health Promotion ActivityCorinne50% (2)
- BibliographyDocument10 pagesBibliographySourav Kumar PatraNo ratings yet
- Addison'sDocument4 pagesAddison'sKoRnflakesNo ratings yet
- DRUG STUDY MAGNESIUM SULFATEDocument7 pagesDRUG STUDY MAGNESIUM SULFATEminervanatividadNo ratings yet
- Cues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale EvaluationDocument4 pagesCues Nursing Diagnosis Scientific Reason Objective Nursing Intervention Rationale Evaluationjomsportg0% (1)
- Pathophysiology of HyperthyroidismDocument4 pagesPathophysiology of HyperthyroidismKitty YuffieNo ratings yet
- SyncopeDocument28 pagesSyncopeDurgesh PushkarNo ratings yet
- Pathophysiology (Myasthenia Gravis) ..Document20 pagesPathophysiology (Myasthenia Gravis) ..Suku ydvNo ratings yet
- Acute PainDocument1 pageAcute Painnursing concept mapsNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Goal Planning Rational Implementation Objective DataDocument8 pagesNursing Care Plan: Assessment Diagnosis Goal Planning Rational Implementation Objective DataMoonNo ratings yet
- Gentiourinary DisordersDocument14 pagesGentiourinary DisordersChona Jimenez67% (3)
- Rapid assessment vital for major burnsDocument8 pagesRapid assessment vital for major burnsHelena Meurial Hilkiah100% (1)
- Peripheral Arterial Occlusive DiseaseDocument4 pagesPeripheral Arterial Occlusive Diseasekrisfred14100% (1)
- Stroke Guide - Causes, Symptoms, RisksDocument12 pagesStroke Guide - Causes, Symptoms, RisksSuzette Rae TateNo ratings yet
- PPP TbiiiDocument3 pagesPPP TbiiiEricsonMitraNo ratings yet
- DP HyperthyroidismDocument6 pagesDP HyperthyroidismTracy May CandolitaNo ratings yet
- ChemotherapyDocument11 pagesChemotherapyRekha G.No ratings yet
- Review of Anatomy and PhysiologyDocument7 pagesReview of Anatomy and PhysiologyKyla CalzadoNo ratings yet
- NCP Total Hip ReplacementDocument11 pagesNCP Total Hip ReplacementDoneva Lyn MedinaNo ratings yet
- Subjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Document5 pagesSubjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Erle Gray CadangenNo ratings yet
- Physiology of PainDocument35 pagesPhysiology of PainJauhar Firdaus50% (2)
- Welcome To The Case Study Presentation:-: Prostate CancerDocument22 pagesWelcome To The Case Study Presentation:-: Prostate CancerDengo ChapatieeNo ratings yet
- HNP Case Scenario For Case StudyDocument2 pagesHNP Case Scenario For Case StudyDeinielle Magdangal RomeroNo ratings yet
- Sample Charting PDFDocument2 pagesSample Charting PDFjeffersonswallNo ratings yet
- MorphineDocument3 pagesMorphineAizat KamalNo ratings yet
- SEPTICARTHRITISDocument2 pagesSEPTICARTHRITISapi-3822433No ratings yet
- NCPDocument5 pagesNCPHuzzain PangcogaNo ratings yet
- Benign Prostatic HyperplasiaDocument9 pagesBenign Prostatic Hyperplasiaanju rachel joseNo ratings yet
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNo ratings yet
- HaloperidolDocument4 pagesHaloperidolNickol BaylonNo ratings yet
- Generic NameDocument2 pagesGeneric NameNickol BaylonNo ratings yet
- Nursing InformaticsDocument3 pagesNursing InformaticsNickol BaylonNo ratings yet
- NCMDocument3 pagesNCMNickol BaylonNo ratings yet
- CDX Group 5Document4 pagesCDX Group 5Nickol BaylonNo ratings yet
- 1st - Nickol & RJDocument21 pages1st - Nickol & RJNickol BaylonNo ratings yet
- Understanding the Four Aspects of EmotionsDocument13 pagesUnderstanding the Four Aspects of EmotionsRaymond FaeldoñaNo ratings yet
- 3 1Document4 pages3 1HakanNo ratings yet
- Planning Installation and Configuration Guide For Windows PDFDocument228 pagesPlanning Installation and Configuration Guide For Windows PDFmmilovanmNo ratings yet
- Engagement & Akad PDFDocument3 pagesEngagement & Akad PDFedputriNo ratings yet
- Chips Unlimited Blend LibraryDocument20 pagesChips Unlimited Blend Librarymizan sallehNo ratings yet
- IMG - 0092 PSME Code 2012 90Document1 pageIMG - 0092 PSME Code 2012 90Bugoy2023No ratings yet
- WK-3508F IPTV Gateway DatasheetDocument7 pagesWK-3508F IPTV Gateway DatasheetComunidad Tecnolibre.netNo ratings yet
- MA 102 Tutorial Sheet No. 2 on Limits and ContinuityDocument1 pageMA 102 Tutorial Sheet No. 2 on Limits and ContinuityKanan KumarNo ratings yet
- Sea Cucumber PDFDocument171 pagesSea Cucumber PDFRebeccaSulivanNo ratings yet
- Aqua Mon 4000 PH Red Ox AnalyserDocument4 pagesAqua Mon 4000 PH Red Ox Analyserarvindgupta_2005No ratings yet
- Sri Lanka's Mineral Resources Can Enrich Country's CoffersDocument139 pagesSri Lanka's Mineral Resources Can Enrich Country's CoffersPrashan Francis100% (3)
- Compression Molding of Gypsum Blocks Using Ecological Brick MachinesDocument11 pagesCompression Molding of Gypsum Blocks Using Ecological Brick Machinessami fanuaelNo ratings yet
- NPTEL Control Engineering Assignment 2 - SEO OptimizedDocument4 pagesNPTEL Control Engineering Assignment 2 - SEO OptimizedGanesh RadharamNo ratings yet
- AC Circuit 2 (Three-Phase)Document2 pagesAC Circuit 2 (Three-Phase)marlon desaculaNo ratings yet
- GMSARN Conf: Design Criteria on Substation ProtectionDocument6 pagesGMSARN Conf: Design Criteria on Substation Protectionbdaminda6701No ratings yet
- CH 2 Atoms, Ions, and MoleculesDocument64 pagesCH 2 Atoms, Ions, and MoleculesBritney SimmsNo ratings yet
- 13.phase Feeding and Feeding SystemsDocument21 pages13.phase Feeding and Feeding SystemsAsfand Ali SheikhNo ratings yet
- Carbozinc 859: Selection & Specification Data Substrates & Surface PreparationDocument2 pagesCarbozinc 859: Selection & Specification Data Substrates & Surface PreparationAmy JonesNo ratings yet
- PV Elite ResultDocument18 pagesPV Elite ResultVeny MartianiNo ratings yet
- Explore the Precambrian EraDocument3 pagesExplore the Precambrian EraArjay CarolinoNo ratings yet
- ADAMHAND8A4Document11 pagesADAMHAND8A4Elker José Camargo100% (1)
- Comparing characteristics and properties of various crude oilsDocument2 pagesComparing characteristics and properties of various crude oilsnishant bhushanNo ratings yet
- Science Technologyand International RelationsDocument20 pagesScience Technologyand International RelationsMuhammad HussainNo ratings yet
- Error Codes (DTC) : 15 Electrical TroubleshootingDocument13 pagesError Codes (DTC) : 15 Electrical TroubleshootingPoyraz PoyrazNo ratings yet
- Creative NonfictionDocument11 pagesCreative NonfictionRubelyn CagapeNo ratings yet
- Lab 7 Activities Sheet Winter 2020Document7 pagesLab 7 Activities Sheet Winter 2020Mareline MendietaNo ratings yet
- Fischer Carbene Complexes in Organic SynthesisDocument9 pagesFischer Carbene Complexes in Organic SynthesisNorah AltayyarNo ratings yet
- 28 2001 04 0007Document1 page28 2001 04 0007Fernando FanteNo ratings yet
- Outotec: Managing Talent Globally With Successfactors® SolutionsDocument3 pagesOutotec: Managing Talent Globally With Successfactors® SolutionsxandaniNo ratings yet
- Galaxy NanoporeDocument11 pagesGalaxy NanoporeDeborah ShirleenNo ratings yet