Professional Documents
Culture Documents
Hypertension
Uploaded by
Jam TorresOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypertension
Uploaded by
Jam TorresCopyright:
Available Formats
HYPERTENSION Introduction Hypertension (HTN) or high blood pressure is a cardiac chronic medical condition in which the systemic arterial
blood pressure is elevated. It is the opposite of hypotension. Hypertension is classified as primary (essential) hypertension, secondary hypertension, and malignant hypertension. About 9095% of cases are categorized as primary hypertension, which means high blood pressure with no obvious medical cause. The remaining 510% of cases (Secondary hypertension) are caused by other conditions that affect the kidneys, arteries, heart or endocrine system. On the other hand, malignant hypertension is a complication of hypertension characterized by very elevated blood pressure, and organ damage in the eyes, brain, heart and/or kidneys. It is considered a hypertensive emergency. Persistent hypertension is one of the risk factors for stroke, myocardial infarction, heart failure and arterial aneurysm, and is a leading cause of chronic kidney failure. Moderate elevation of arterial blood pressure leads to shortened life expectancy. Dietary and lifestyle changes can improve blood pressure control and decrease the risk of associated health complications, although drug treatment may prove necessary in patients for whom lifestyle changes prove ineffective or insufficient. Anatomy & Physiology The Cardiovascular [Circulatory] System The cardiovascular system consists of the heart, which is a muscular pumping device, and a closed system of vessels called arteries, veins, and capillaries. The vital role of the cardiovascular system in maintaining homeostasis depends on the continuous and controlled movement of blood through the thousands of miles of capillaries that permeate every tissue and reach every cell in the body. The heart is a muscular pump that provides the force necessary to circulate the blood to all the tissues in the body. It is located in the mediastinum, 2/3 left of the midline, behind the sternum, between the lungs, in front of the trachea, esophagus, & thoracic vertebrae. It lies on its side on the diaphragm and its pointed apex is directed toward left hip. Its base is at the level of the 2nd rib sternum, while its apex lies at the level of the 5th intercostal space. Three layers of the heart are: the epicardium, the myocardium, and the endocardium. The four chambers of the heart are: the right atrium, the right ventricle, the left atrium, and the left ventricle. Two types of valves of the heart are the atrioventricular valves and semilunar valves. Blood flows from the right atrium to the right ventricle and then is pumped to the lungs to receive oxygen. From the lungs, the blood flows to the left atrium, then to the left ventricle. From there it is pumped to the systemic circulation. Specialized cardiac muscle cells that make up the conduction system of the heart coordinate contraction of the chambers. The pulmonary vessels transport blood from the right ventricle to the lungs and back to the left atrium. The systemic vessels carry blood from the left ventricle to the tissues in all parts of the body and then return the blood to the right atrium. Substances pass through the capillary wall by diffusion, filtration, and osmosis. Blood pressure is the pressure of the blood in the circulatory system, often measured for diagnosis since it is related to the force and rate of the heartbeat and the diameter and elasticity of the arterial walls. Blood pressure is classified as follows: Normal blood pressure: Prehypertension: Hypertension: Stage 1 Hypertension: Stage 2 Hypertension: Malignant Hypertension: less than 120/80 mmHg 120-139/80-89 mmHg greater than 140/90 mmHg 140-159/90-99 mmHg 160 or greater/ 100 or greater mmHg greater than 200/140mmHg
Pathophysiology of Hypertension Hypertension may be primary, which may develop as a result of environmental or genetic causes, or secondary, which has multiple etiologies, including renal, vascular, and endocrine causes. Hypertensive emergencies [Malignant hypertension] are most often precipitated by inadequate medication or poor compliance. Environmental and genetic causes: Hypertension develops secondary to environmental factors, as well as to multiple genes, whose inheritance appears to be complex. Very rare secondary causes are related to single genes and include Liddle syndrome, glucocorticoid-remediable hyperaldosteronism, 11 beta-hydroxylase and 17 alpha-hydroxylase deficiencies, the syndrome of apparent mineralocorticoid excess, and pseudohypoaldosteronism type II. Primary or essential hypertension accounts for 90-95% of adult cases and a small percentage of patients (510%) have a secondary cause. Causes of secondary hypertension: Renal causes (2.5-6%) include the renal parenchymal diseases and renal vascular diseases, as follows: Polycystic kidney disease Urinary tract obstruction Liddle syndrome Chronic kidney disease Renin-producing tumor
Renovascular hypertension (RVHT) causes 0.2-4% of cases. Since Goldblatts seminal experiment in 1934, RVHT has become increasingly recognized as an important cause of clinically atypical hypertension and chronic kidney disease, the latter by virtue of renal ischemia. The coexistence of renal arterial vascular (ie, renovascular) disease and hypertension roughly defines this type of nonessential hypertension. More specific diagnoses are made retrospectively when hypertension is improved after intravascular intervention. Vascular causes include the following: Endocrine causes account for 1-2% and include exogenous or endogenous hormonal imbalances. Exogenous causes include administration of steroids. The most common form of secondary hypertension is an endocrine cause: oral contraceptive use. Activation of the renin-angiotensin-aldosterone system is the likely mechanism because hepatic synthesis of angiotensinogen is induced by the estrogen component of oral contraceptives. Approximately 5% of women prescribed oral contraceptives may develop hypertension, which abates within 6 months of discontinuation. The risk factors for oral contraceptiveassociated hypertension include mild renal disease, familial history of essential hypertension, age older than 35 years, and obesity. Exogenous administration of the other steroids used for therapeutic purposes also increases blood pressure, especially in susceptible individuals, mainly by volume expansion. Nonsteroidal anti-inflammatory drugs (NSAIDs) may also have adverse effects on blood pressure. NSAIDs block both cyclooxygenase-1 (COX-1) and COX-2 enzymes. The inhibition of COX-2 can inhibit its natriuretic effect, which, in turn, increases sodium retention. NSAIDs also inhibit the vasodilating effects of prostaglandins and the production of vasoconstricting factors, namely endothelin-1. These effects can contribute to the induction of hypertension in a normotensive and/or controlled hypertensive patient Endogenous hormonal causes include the following: Neurogenic causes include the following: Drugs and toxins that cause hypertension include the following: Causes of Malignant Hypertension
The most common hypertensive emergency is a rapid unexplained rise in BP in a patient with chronic essential hypertension. Most patients who develop hypertensive emergencies have a history of inadequate hypertensive treatment or an abrupt discontinuation of their medications. Other causes of hypertensive emergencies include the use of recreational drugs, abrupt clonidine withdrawal, post pheochromocytoma removal, and systemic sclerosis. Risk Factors Although the exact cause of high blood pressure is unknown, there are several factors and conditions that may increase risk. The factors that cannot be controlled are: Age, Race, Gender, Family history of high blood pressure The factors that can be controlled are: Obesity, Smoking, Little or no exercise, Too much salt in the diet, Drinking too much alcohol & coffee, Stress, Certain chronic diseases, such as high cholesterol, diabetes, kidney disease, and sleep apnea. Diagnosis Hypertension is generally diagnosed on the basis of a persistently high blood pressure. Usually this requires three separate sphygmomanometer measurements at least one week apart. Often, this entails three separate visits to the physician's office. Initial assessment of the hypertensive patient should include a complete history and physical examination. Exceptionally, if the elevation is extreme, or if symptoms of organ damage are present then the diagnosis may be given and treatment started immediately. Once the diagnosis of hypertension has been made, physicians will attempt to identify the underlying cause based on risk factors and other symptoms, if present. Secondary hypertension is more common in preadolescent children, with most cases caused by renal disease. Primary or essential hypertension is more common in adolescents and has multiple risk factors, including obesity and a family history of hypertension. Laboratory tests can also be performed to identify possible causes of secondary hypertension, and determine if hypertension has caused damage to the heart, eyes, and kidneys. Additional tests for Diabetes and high cholesterol levels are also usually performed because they are additional risk factors for the development of heart disease require treatment. Tests typically performed are classified as follows: System Tests Renal - Microscopic urinalysis, proteinuria, serum BUN (blood urea nitrogen) and/or creatinine Endocrine - Serum sodium, potassium, calcium, TSH (thyroid-stimulating hormone). Metabolic - Fasting blood glucose, total cholesterol, HDL and LDL cholesterol, triglycerides Other - Hematocrit, electrocardiogram, and chest radiograph Creatinine (renal function) testing is done to determine if kidney disease is present, which can be either the cause or result of hypertension. In addition, it provides a baseline measurement of kidney function that can be used to monitor for side-effects of certain antihypertensive drugs on kidney function. Additionally, testing of urine samples for protein is used as a secondary indicator of kidney disease. Glucose testing is done to determine if diabetes mellitus is present. Electrocardiogram (EKG/ECG) testing is done to check for evidence of the heart being under strain from high blood pressure. It may also show if there is thickening of the heart muscle (left ventricular hypertrophy) or has experienced a prior minor heart disturbance such as a silent heart attack. A chest X-ray may be performed to look for signs of heart enlargement or damage to heart tissue. Signs and Symptoms The patient with hypertension tends to be older and the prevalence of the disease increases with age. However, 2 percent of children have hypertension while another 5 percent are borderline. Black adults have a
higher incidence of hypertension than Caucasian adults and typically a more severe form of the disease. Risk factors for the development of hypertension include a positive family history of hypertension or cardiovascular disease, diabetes, hypercholesterolemia, obesity, sedentary lifestyle, high sodium intake, high dietary fat intake, alcohol use, smoking, and a stressful lifestyle. Hypertension is defined as systolic blood pressure (BP) exceeding 140mmHg and/or diastolic BP exceeding 90mmHg measured at least twice on separate days. About 90 percent of cases are due to essential hypertension, while the remaining cases are secondary to another disease. Hypertension is manifested within the eye as both hypertensive retinopathy and hypertensive ocular complications. Hypertensive ocular complications include retinal vessel occlusion, ocular ischemic syndrome, non-arteritic anterior ischemic optic neuropathy, internuclear ophthalmoplegia, cranial nerve palsy, nystagmus and midbrain syndrome, and amaurosis fugax and transient ischemic attack.
Complications The excessive pressure on your artery walls caused by high blood pressure can damage your blood vessels, as well as organs in your body. The higher your blood pressure and the longer it goes uncontrolled, the greater the damage. Uncontrolled high blood pressure can lead to: Heart attack or stroke. High blood pressure can cause hardening and thickening of the arteries (atherosclerosis), which can lead to a heart attack, stroke or other complications. Aneurysm. Increased blood pressure can cause your blood vessels to weaken and bulge, forming an aneurysm. If an aneurysm ruptures, it can be life-threatening. Heart failure. To pump blood against the higher pressure in your vessels, your heart muscle thickens. Eventually, the thickened muscle may have a hard time pumping enough blood to meet your body's needs, which can lead to heart failure. Weakened and narrowed blood vessels in your kidneys. This can prevent these organs from functioning normally. Thickened, narrowed or torn blood vessels in the eyes. This can result in vision loss. Metabolic syndrome. This syndrome is a cluster of disorders of your body's metabolism including increased waist circumference, high triglycerides, low high-density lipoprotein (HDL), or "good," cholesterol, high blood pressure, and high insulin levels. If you have high blood pressure, you're more likely to have other components of metabolic syndrome. The more components you have, the greater your risk of developing diabetes, heart disease or stroke. Trouble with memory or understanding. Uncontrolled high blood pressure also may affect your ability to think, remember and learn. Trouble with memory or understanding concepts is more common in people who have high blood pressure.
Treatments and drugs Hypertension is dangerous because it can lead to strokes, heart attacks, heart failure, or kidney disease. The goal of hypertension treatment is to lower high blood pressure and protect important organs, like the brain, heart, and kidneys from damage. Treatment for hypertension has been associated with reductions in stroke, heart attack, and heart failure, according to research. All patients with blood pressure readings greater than 120/80 should be encouraged to make lifestyle modifications, such as eating a healthier diet, quitting tobacco and getting more exercise. Treatment with medication is recommended to lower blood pressure to less than 140/90 mmHg. For patients who have diabetes or chronic kidney disease the recommended blood pressure is less than 130/80 mmHg.
Treating high blood pressure involves lifestyle changes and possibly drug therapy. A critical step in preventing and treating high blood pressure is a healthy lifestyle. You can lower your blood pressure with the following lifestyle changes: Losing weight if you are overweight or obese. Quitting smoking. Eating a healthy diet, including the DASH diet (Dietary Approaches to Stop Hypertension -eating more fruits, vegetables, and low fat dairy products, less saturated and total fat). Reducing the amount of sodium in your diet to less than 1,500 milligrams a day. Getting regular aerobic exercise (such as brisk walking at least 30 minutes a day, several days a week). Limiting alcohol to two drinks a day for men, one drink a day for women.
In addition to lowering blood pressure, these measures enhance the effectiveness of high blood pressure drugs. There are several types of drugs used to treat high blood pressure, including: Angiotensin-converting enzyme (ACE) inhibitors Angiotensin II receptor blockers (ARBs) Diuretics Beta-blockers Calcium channel blockers Alpha-blockers Alpha-agonists Renin inhibitors Combination medications
Diuretics are often recommended as the first line of therapy for most people who have high blood pressure. However, your doctor may start a medicine other than a diuretic as the first line of therapy if you have certain medical problems. For example, ACE inhibitors are often a choice for a people with diabetes. If one drug doesn't work or is disagreeable, other types of drugs are available. After starting high blood pressure drug therapy, you should see your doctor at least once a month until the blood pressure goal is reached. Once or twice a year, your doctor will check the level of potassium in your blood (diuretics can lower this, and ACE inhibitors and ARBs may increase this) and other electrolytes and BUN/creatinine levels (to check the health of the kidneys). After the blood pressure goal is reached, you should continue to see your doctor every three to six months, depending on whether other diseases such as heart failure are present.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Nur2811c JournalDocument5 pagesNur2811c Journalapi-533991468No ratings yet
- Success Magazine (Liam Neeson)Document92 pagesSuccess Magazine (Liam Neeson)Nathan100% (5)
- 2005 Pleiotropic Effects of StatinsDocument9 pages2005 Pleiotropic Effects of StatinsK KNo ratings yet
- Cardiac Enzyme: Presented By: Group 5 .Document28 pagesCardiac Enzyme: Presented By: Group 5 .Zafieys Jehan100% (3)
- 2 5193183311375110881Document20 pages2 5193183311375110881Mohamed H ElboraeyNo ratings yet
- Ischaemic Heart Disease: DR Haider Baqai Assistant Professor of Medicine Rawalpindi Medical CollegeDocument104 pagesIschaemic Heart Disease: DR Haider Baqai Assistant Professor of Medicine Rawalpindi Medical CollegeputriluftiNo ratings yet
- Shock ExamDocument3 pagesShock ExamMilagros Fuertes Yosores100% (1)
- Ninja NerdDocument3 pagesNinja NerdSalsabila HMNo ratings yet
- Jaypee's Dental Dictionary (2009) (PDF) (UnitedVRG)Document619 pagesJaypee's Dental Dictionary (2009) (PDF) (UnitedVRG)baselrehawiNo ratings yet
- J of Clinical Hypertension - 2019 - Ishiyama - Constipation Induced Pressor Effects As Triggers For Cardiovascular EventsDocument5 pagesJ of Clinical Hypertension - 2019 - Ishiyama - Constipation Induced Pressor Effects As Triggers For Cardiovascular Eventskahar ahmadNo ratings yet
- CABG ArticleDocument9 pagesCABG ArticleDeepak PatelNo ratings yet
- IMPLANTS Diagnosis & Treatment PlanningDocument40 pagesIMPLANTS Diagnosis & Treatment Planningneethu67% (3)
- 11 Ways Women's Heart Attacks Are Different From Men'sDocument25 pages11 Ways Women's Heart Attacks Are Different From Men'sSri KondabattulaNo ratings yet
- TO HO W Preven T Lifestyle: DiseasesDocument18 pagesTO HO W Preven T Lifestyle: DiseasesJazyrin M. PullanNo ratings yet
- Sudden Cardiac Death in Anabolic Androgenic Steroids Abuse: Case Report and Literature ReviewDocument8 pagesSudden Cardiac Death in Anabolic Androgenic Steroids Abuse: Case Report and Literature ReviewmjkoNo ratings yet
- Journal Medicine: The New EnglandDocument9 pagesJournal Medicine: The New Englandrahma watiNo ratings yet
- Alteplase: Umair - M030 Farrakh - M036Document30 pagesAlteplase: Umair - M030 Farrakh - M036Farrakh AliNo ratings yet
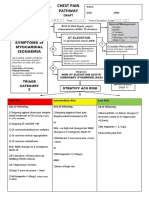
- Chest Pain Pathway GuideDocument4 pagesChest Pain Pathway GuidefauzanNo ratings yet
- Cardiovascular MCQs LJDocument11 pagesCardiovascular MCQs LJYanis Yan100% (1)
- CHRONIC HEART FAILURE SYMPTOMS AND DIAGNOSISDocument10 pagesCHRONIC HEART FAILURE SYMPTOMS AND DIAGNOSISYudha GanesaNo ratings yet
- Patient Profile and History of Acute Coronary SyndromeDocument32 pagesPatient Profile and History of Acute Coronary SyndromenidhiNo ratings yet
- Group 5 - Percutaneous Transluminal AngioplastyDocument15 pagesGroup 5 - Percutaneous Transluminal AngioplastyKimberly Abella CabreraNo ratings yet
- COVID-19 AstraZeneca Vaccine Analysis PrintDocument65 pagesCOVID-19 AstraZeneca Vaccine Analysis PrintcorreaNo ratings yet
- Mudra VigyanDocument4 pagesMudra VigyanMahesh MurugesanNo ratings yet
- Final Research PaperDocument16 pagesFinal Research Paperapi-593862121No ratings yet
- NCP Acute PainDocument5 pagesNCP Acute PainEzra TuanNo ratings yet
- MEDICAL SURGICAL NURSING Cardiovascular and Respiratory SystemDocument12 pagesMEDICAL SURGICAL NURSING Cardiovascular and Respiratory Systemvalentine95% (20)
- NPTE Sullivan EXAM CDocument134 pagesNPTE Sullivan EXAM CMarilia FarensenaNo ratings yet
- BibliographyDocument10 pagesBibliographySoumyaReddyNo ratings yet
- Coronary Artery Disease (Cad)Document4 pagesCoronary Artery Disease (Cad)Freddy PanjaitanNo ratings yet