Professional Documents
Culture Documents
Repots
Uploaded by
GLadys GegareOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Repots
Uploaded by
GLadys GegareCopyright:
Available Formats
Ventilation is the movement of air in and out of the lungs.
Inhalation or inspiration- movement of air into the lungs Exhalation or expiration- movement of air out of the lungs
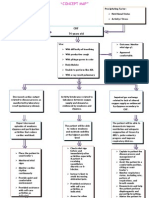
Perfusion is the exchange of oxygen and carbon dioxide at the alveolar- capillary level. Normal ventilation- perfusion (V/Q) ratio is 4:5 Normal Ventilation and Perfusion: When ventilation and perfusion is matched, unoxygenated blood from the venous system returns to the right side of the heart through the pulmonary arteries to the lungs, carrying carbon dioxide. The arteries branch into the alveolar capillaries where gas exchange takes place. Ventilation- Perfusion Dysfunction Two Types of Ventilation- Perfusion Mismatch: 1. Shunting- there is decreased ventilation related to perfusion This is the portion of the cardiac output that does not exchange with alveolar air. The PaO2 falls because less oxygen is delivered and the PaCO2 increases because less CO2 is expired. Clinical examples: Vascular lung tumors Congenital heart disease Intrapulmonary fistulas Pneumothorax Hemothorax Pleural effusion Obstruction of the bronchi or bronchioles
2. Dead Space- decreased perfusion related to ventilation also called wasted ventilation Anatomic dead space is that portion of ventilation that is within the upper airways, not in contact with a capillary. Alveolar dead space is the volume that is within the alveoli; theres no blood flow adjacent to it. PaCO2 falls because less CO2 is delivered and the PaO2 increases, because less oxygen enters the blood Clinical example: Pulmonary embolus
Hypoxemia versus Hypoxia Hypoxemia is a decreased level of oxygen in the arterial blood as measured by the PaO2.
Early signs: Late signs: Arrhythmias Hypotension Cyanosis Coma Restlessness Anxiety Disorientation, confusion, lassitude and listlessness Headaches
Hypoxia refers to the state of decreased perfusion of oxygen to the tissues and is measured by pulse oxymetry.
Signs: Change in mental status (earliest sign) Change in vital signs Headache Hypercapnia versus Hypocapnia Hypercapnia is defined as a PaCO2 above 45. Indicates that ventilation is inadequate.
Signs: flushed skin, full pulse, tachypnea, dyspnoea, extrasystoles, muscle twitches, hand flaps, reduced neural activity, and possibly a raised blood pressure
Hypocapnia is defined as a PaCO2 below 35. Indicates that there is too much ventilation
Signs: dizziness, visual disturbances anxiety muscle cramps
Oxygen Transport Two Ways: 1. Dissolved in the plasma Clinical measure of the dissolved oxygen is the PaO2 3% of O2 2. Attached to hemoglobin (oxyhemoglobin) 97% of O2 Clinical measure of this oxygen attached to hemoglobin is oxygen saturation (SaO2, SpO2 ) Fully saturated= SpO2 >92% Desaturated= SpO2 < 98% Oxygen- Hemoglobin Dissociation Curve Illustrates relationship between the PaO2 and the SaO2 Illustrates condition that change the affinity of oxygen for hemoglobin Factors that cause decreased affinity of oxygen for hemoglobin will shift the oxyhemoglobin dissociation curve to the RIGHT which causes Acidemia. Factors that cause increased affinity of oxygen for hemoglobin will shift the oxyhemoglobin dissociation curve to the LEFT which causes Alkalemia.
Left shift (high affinity for O2)
Right shift (low affinity for O2)
Temperature
hypothermia
hyperthermia
2,3-diphospoglycerate
increase
PaCO2
decrease
increase
pH
Increased arterial pH >7.45 (alkalosis)
Decreased arterial pH <7.35 (acidosis)
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Medibus For Dräger Intensive Care DevicesDocument52 pagesMedibus For Dräger Intensive Care DevicesMedsystem atNo ratings yet
- Nursing Care Plan Impaired Gas ExchangeDocument1 pageNursing Care Plan Impaired Gas Exchangecuicuita100% (3)
- ATI - Adult Medical Surgical NGN B (99 Questions and Answers 2023 - Guarantee A+Document28 pagesATI - Adult Medical Surgical NGN B (99 Questions and Answers 2023 - Guarantee A+denis100% (1)
- NEWS2 Chart 3 - NEWS Observation Chart - 0 PDFDocument1 pageNEWS2 Chart 3 - NEWS Observation Chart - 0 PDFKartini MedikalNo ratings yet
- Expanded Program On ImmunizationDocument7 pagesExpanded Program On ImmunizationGLadys Gegare100% (1)
- Health Assessment For Nursing Practice 5th Edition Wilson Test BankDocument16 pagesHealth Assessment For Nursing Practice 5th Edition Wilson Test BankJordanGibsonopaxj100% (13)
- ULAM, CHIN V. - NCM 118 PrelimDocument8 pagesULAM, CHIN V. - NCM 118 PrelimChin Villanueva Ulam100% (1)
- Fanem 1186 Infant Incubator - User ManualDocument78 pagesFanem 1186 Infant Incubator - User ManualrobinsongiraldoNo ratings yet
- Monitoring Intra OperatifDocument21 pagesMonitoring Intra OperatifAlaa Ulil HaqiyahNo ratings yet
- Burn Assessment ToolsDocument1 pageBurn Assessment ToolsGLadys GegareNo ratings yet
- External Eye Assessment and ManagementDocument18 pagesExternal Eye Assessment and ManagementGLadys GegareNo ratings yet
- Guillian-Barre Syndrome: Renalyn Galache Gladys Gegare BSN-3BDocument18 pagesGuillian-Barre Syndrome: Renalyn Galache Gladys Gegare BSN-3BGLadys GegareNo ratings yet
- Manual Oximetro Choicemed EspañolDocument2 pagesManual Oximetro Choicemed Españolgcamila.102No ratings yet
- Oxygen Saturation Targets in Critical Care - LITFL - CCCDocument30 pagesOxygen Saturation Targets in Critical Care - LITFL - CCCnonieshzNo ratings yet
- Impaired Gas ExchangeDocument3 pagesImpaired Gas ExchangePaul VincentNo ratings yet
- Domiciliary Oxygen Therapy - Summary of IndicationsDocument4 pagesDomiciliary Oxygen Therapy - Summary of IndicationsAdina BatajuNo ratings yet
- CP DP Man 01 Dolphin Cpap Manual 1.12enDocument44 pagesCP DP Man 01 Dolphin Cpap Manual 1.12enlidyamengistu12No ratings yet
- Ain ShamsJAnaesthesiol10184 2808197 074801 HYPOXAEMIADocument7 pagesAin ShamsJAnaesthesiol10184 2808197 074801 HYPOXAEMIAOYEBOLA ADEKOLANo ratings yet
- Electronic Design Services in Bangalore (HTTP://WWW - Dncltech.com)Document21 pagesElectronic Design Services in Bangalore (HTTP://WWW - Dncltech.com)AshokkumarKrishnanNo ratings yet
- B20 Specs Sheet - Mature MarketDocument4 pagesB20 Specs Sheet - Mature MarketShimon DoodkinNo ratings yet
- Sensores SPO2 G.EDocument4 pagesSensores SPO2 G.EEnmanuel DiazNo ratings yet
- Using Venous Blood Gas Analysis in The Assessment of COPD Exacerbations A Prospective Cohort StudyDocument7 pagesUsing Venous Blood Gas Analysis in The Assessment of COPD Exacerbations A Prospective Cohort Studynur amaliah idrusNo ratings yet
- VBG InterpretationDocument9 pagesVBG InterpretationLeo MartinNo ratings yet
- Communication Protocol of Contec Pulse Oximeter V7.0Document8 pagesCommunication Protocol of Contec Pulse Oximeter V7.0Mike KlopferNo ratings yet
- Modified Braden Q ScaleDocument1 pageModified Braden Q ScaleGrace Simarmata100% (1)
- Nanda Needs ListDocument24 pagesNanda Needs ListObrian ReidNo ratings yet
- Concept Map - Abby !Document2 pagesConcept Map - Abby !Abegail Abaygar100% (3)
- B20 Patient Monitor BrochureDocument6 pagesB20 Patient Monitor Brochurehphphp00No ratings yet
- HI English Kannada Final 1Document4 pagesHI English Kannada Final 1Sachinhonnatti SachinhonnattiNo ratings yet
- PALS Manual Changes January 2012Document1 pagePALS Manual Changes January 2012Danhil RamosNo ratings yet
- 1 - 爱度AD805规格及资质 高清 0611Document20 pages1 - 爱度AD805规格及资质 高清 0611Anupam JainNo ratings yet
- Omlor Et Al. - 2023 - Comparison of Serial and Parallel Connections of MDocument13 pagesOmlor Et Al. - 2023 - Comparison of Serial and Parallel Connections of Mgavain.ferronsNo ratings yet
- Critikon Dinamap Compact - Service Manual 2Document78 pagesCritikon Dinamap Compact - Service Manual 2Ayaovi JorlauNo ratings yet
- Moxy Strength Training EbookDocument22 pagesMoxy Strength Training EbookPippo PlutoNo ratings yet