Professional Documents
Culture Documents
Bone Morphogenetic
Uploaded by
ssaikalyanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bone Morphogenetic
Uploaded by
ssaikalyanCopyright:
Available Formats
Int. J. Odontostomat., 1(1):53-58, 2007.
Bone Morphogenetic Proteins: Its Application in the Process of Repairing the Dentin Pulp Complex
Protenas seas Morfogenticas: Su Aplicacin en el Processo de Reparacin del Complejo Dentina Pulpa.
Joo Paulo Mardegan Issa*; Cssio do Nascimento*; Rodrigo Tiossi*; Dimitrius Leonardo Pitol**; Mamie Mizusaki Iyomasa*
ISSA, M. J. P. ; NASCIMENTO, C., TIOSSI; PITOL, D. L. & IYOMASA, M. M. Bone morphogenetic proteins: Its application in the process of reparing the dentin pulp complex. Int. J. Odontostomat., 1(1):53-58, 2007. ABSTRACT: Evolution of knowledge related to molecular Biology has been applied in different areas of clinical Biology, Dentistry among them, allowing the use of these new advances in the treatment of offenses to the pulpal organ. The use of bone morphogenetic proteins (BMPs) represents another possibility in the treatment of exposed pulps with no contact with aggressive agents and free from undesirable effects to maintain pulp vitality. KEY WORDS: bone Morphogenetic proteins, reparative dentin, pulp capping.
INTRODUCTION
Evolution of knowledge related to molecular Biology has been applied in different areas of clinical Biology, Dentistry among them, allowing the use of these new advances in the treatment of offenses to the pulpal organ. The use of bone morphogenetic proteins (BMPs) represents another possibility in the treatment of exposed pulps with no contact with aggressive agents and free from undesirable effects to maintain pulp vitality. Within this context, the authors aim to review the literature on the subject. Dentin-pulp complex. Pulpal tissue has a great reparative capacity, proved by clinical studies and histological cuts (Weinreb et al. 1967). This reparatory capability of the pulp represents the main source for dentin neoformation (Goldberg et al. 2003). Pulp healing and repair through dentin tissue deposition, happens as consequence of a complex cellular process, sequential and inter-related, including chemotaxis, proliferation, neovascularization, extracellular matrix remodelation and cellular differentiation, leading to the formation of reparative dentin (Melin et al., 2000).
* **
Direct pulp capping consists in the direct application of a protective agent on the exposed pulp, aiming to help pulp tissue reparation, maintain its vitality and protect it from additional injuries, through stimulation and development of a new dentin layer (Mondelli, 1998). The ideal protective agent should be the one that is completely reabsorbed, not affecting pulpal tissue vitality in the healing process and not unleashing any adverse effects when used. Calcium hydrate. Calcium hydrate based compounds, the paste specifically [Ca(OH)2], are the agents most commonly used for direct pulp capping. By showing a highly alkaline pH, around 12, bactericide activity and promoting tissue repair by producing dentin bridge (Foreman & Barnes, 1990). These compounds neutralize the acid pH from the inflammatory tissue (Murray et al., 2002) however, by being too alkaline, they create obliteration zones and superficial necrosis by coagulation of deeper areas, where reparative dentin is beginning to be formed (Stanley, 1989). Structural flaws present in the dentin bridge, formed after calcium hydrate use, shows the presence of numerous
Faculty of Dentistry, University of So Paulo, Ribeiro Preto, So Paulo, Brazil. Biosciences Institute- Molecular and Cellular Biology (UNESP), Rio Claro, So Paulo, Brazil.
53
ISSA, M. J. P. ; NASCIMENTO, C., TIOSSI; PITOL, D. L. & IYOMASA, M. M. Bone morphogenetic proteins: Its application in the process of reparing the dentin pulp complex. Int. J. Odontostomat., 1(1):53-58, 2007.
porosities, called tunnel defects, which allows for bacterial micro-infiltration and its toxins into pulp interior (Ulmansky et al., 1972 and Cox et al., 1996). These flaws make dentin bridge an inefficient and discontinuous barrier, incapable of stopping a new pulp infection and bacterial contamination causing irreversible damage to pulp vitality (Goldberg et al., 2003). These materials have unstable physical properties, which allow migration of their particles inside pulpal tissue, eventually producing an inflammatory process that leads to necrosis (Walton & Langeland, 1978). Continuous cell stimulation in the dentin bridge formation by using calcium hydrate compounds is another factor that leads to excessive mineralized tissue, with occasional closure of the pulp chamber and its consequent obliteration. This particularity makes internal circulation difficult, also affecting radicular canals, causing atresia and toughening a later endodontic treatment, if needed (Stanley, 1989). Undesirable effects, inherent to Calcium Hydrate paste action, caused improvements in the conventional Calcium Hydrate cements composition, with more acceptable biocompatibility characteristics (Costa et al., 2000), a better defined pH, determinant factor in the mild initial pulp inflammation (Negm et al., 1981) and less chances of necrosis (Turner et al., 1987). Because of the adverse effects caused by the use of calcium hydrate base compounds directly over the exposed pulp, other capping agents have been studied and indicated by literature. MTA (Mineral Trioxide Aggregate): MTA consists in a material composed by hydrophilic particles, in which the components are tricalcium silicate, tricalcium aluminate, tricalcium oxide, silicate oxide and bismuth oxide. MTA is used in Endodontics to repair pulp chamber floor or furcation perforations, effectively stimulating reparatory dentin formation and pulpal healing after pulpotomy, without showing any adverse effects (Ford et al., 1996; Faraco & Holland, 2001; Tziafas et al., 2002; Dominguez et al., 2003; Aeinehchi et al., 2003). BMP (Bone Morphogenetic Proteins). Dentin and pulp tissue formation has been made both in vitro and in vivo using strategies applied in tissue engineering. The great potential in applying this technique is treating teeth with pulpal injury. Grafting enamel matrix derivate has also been evaluated for direct pulp capping suggesting that its use increases the formation of reparatory dentin and effectively producing the dentin bridge (Igarashi et al., 2003;
Matsumoto & Lyngstadaas, 2002). This technique was evaluated by Ishizaki et al. 2003 where, after 4 and 8 weeks observation, through microscopic exam, an increase in tertiary dentin was found, suggesting that the material used influenced odontoblasts and endothelial capillary cells to perform the role of neoformed calcification tissue. Urist and Strates (1971) designated the term osteoinduction to a fundamental principle of osseous regeneration unleashed by action of the BMPs, which are indicated nowadays to repair exposed pulps and belong to a super-family of growth transformation factors (TGFb_). TGFb_ is a potent modulator of tissue repair in different situations (Six et al., 2002; Goldberg et al., 2003). Melin et al., (2000) saw the action of this factor in human teeth for direct pulp capping, stating that this material is capable to induce type I collagen formation by pulp cells, suggesting that the same is directly involved in regulating cell proliferation and migration, and also in the production of extracellular matrix in human dental pulp and consequently influencing tooth repair process. Since the BMPs belong to the growth factor super-family (TGFb), Nakashima (1990) reports that these proteins can be used, with great success, directly on exposed pulps, without any adverse effect to the pulpal organ. There are evidences suggesting that, if the odontoblasts are lost due cavities, the formation of new pulp cells can be stimulated by the presence of BMPs (Kaigler et al., 2001). These proteins exist in odontoblasts, ameloblasts and in the dentin matrix, being capable to induce undifferentiated pulp cells into odontoblast-like cells. The molecules that belong to the BMPs group act as important signaling molecules, both in dental development as in reparatory processes stimuli in mature tooth tissue, being originally isolated from the osseous cell matrix and having the capability to induce ectopically osseous formation (Helder et al., 1998; Lianjia et al., 1993). Actuation of BMPs originated from several animals was compared by verifying if, no matter the animal specie which was extracted from, it promoted osteoinduction (Bessho et al., 1992). On first studies, human BMPs were extracted and purified from corpses bones or dentinary matrix, with the risk of transmitting infections (Cala et al., 1999). In the present day, with advances in tissue engineering, these molecules can be synthesized, making them available for therapeutic application in dental practice (Cohen et al., 1975). BMPs production available for professionals nowadays
54
ISSA, M. J. P. ; NASCIMENTO, C., TIOSSI; PITOL, D. L. & IYOMASA, M. M. Bone morphogenetic proteins: Its application in the process of reparing the dentin pulp complex. Int. J. Odontostomat., 1(1):53-58, 2007.
offers a uniform and standardized product, of high quality and with capability of reproduction which allows for the production of large amounts (Cala et al., 1999). For clinical application, it is essential the efficiency of the carrying material (transmitter), which should promote bioaccessibility to the host tissues of the BMP and assure its uniform and gradual distribution. Also, this carrier must be reabsorbed as tissue formation occurs, be biodegradable and biocompatible (Toriumi and Robertson, 1993). Among the tested biomaterials as carriers include various extracellular matrix components, combined or isolated (collagen, fibronectin, glucosaminoglycans), calcium hydrate and calcium phosphate (Rutherford et al., 1994). The physical structure or the molecular organization of the carrier can contribute to cell guidance and facilitate the reparatory and regenerating process in the newly formed tissues (Goldberg et al., 2003). Clarkson et al. (2001) reported that, of all studies conducted on animals, with BMPs extracted from purified and recombining BMP-7, these proteins presented as capable of regenerating tubular and intratubular dentin, when used on vital exposed pulp. Lianjia et al. (1993), reported that a week after pulp protection with BMP, a small sign of inflammation was found; however, at the end of the second week, these signs were gone and a substantial amount of dentin and osteodentin was observed, being well distinguished in two regions, in the osteodentin and in the regular dentin surrounded by osteodentin areas. In the last region, there was the presence of many dentin tubes with well defined odontoblastic processes. In the beginning of the third week, dentin formation was inducted and the dentin bridge was completely formed, and calcification process had started. For the control group, capped with calcium hydrate, only a small formation of osteodentin was present in the fourth week after the treatment and without formation of the dentin bridge, which shows the main advantages of using BMPs as capping material rather than calcium hydrate.
BMPs play an important role in cell differentiation and consist in one of the most important agents in odontoblasts induction when used as direct pulp protectors (Lianjia et al., 1993), indicating the possibility of its use as a substitute for materials commonly used for direct pulp capping, such as calcium hydrate that despite satisfying results, have effects of risking pulp vitality (Rutherford et al., 1995; Stanley, 1989; Walton & Langeland, 1978; Ulmansky et al., 1972; Cox et al., 1996; Goldberg et al., 2003). Lianjia et al. (1993) found that BMPs are also responsible for dentinogenesis, inducing non differentiated mesenchymal cells from the pulp to form odontoblast-like cells, obtaining osteodentin and tubular dentin deposition, when used as direct protectors. This result was also shown by Nakashima (1990); Rutherford et al. (1993). Rutherford et al. (1993) saw that osteogenic protein (OP-1) when applied directly on dentin, in monkey teeth, stimulates the formation of reparatory dentin significantly more than the calcium hydrate paste, also presenting the carrier characteristic, collagen in such case, completely reabsorbed and substituted by a fibrous mineralized connective tissue, which is different from calcium hydrate, that stays in the tooth under the dentin bridge. This author also found that the extension of tissue mineralization evaluated in another work (Rutherford et al., 1994), followed in periods of 1, 2, 4 and 6 weeks of healing time of the exposed area, and covered with osteogenic protein-1 (hOP-1, BMP-7), ended with the formation of reparatory dentin and its mineralization happened in a proportion of 75% at the end of the first month and 95% after four months. Among studies found in Literature, they all unanimously attested, according to each experiment condition, that the pattern of formed dentin with the use of calcium hydrate as a direct pulp protector was different from the pattern achieved with the use of BMPs, which provided higher quantity and more homogeneous reparatory dentin with the presence of many tubes with defined odontoblastic processes (Nakashima, 1990; Lianjia et al., 1993; Rutherford et al., 1995) which, according to Rutherford et al. (1994), there is also a correlation between the amount of the formed dentin and the quantity of BMP used; in this last study, authors reported better results, obtaining a larger amount of neo-formed dentin when 1-2mg of the protein were used, which did not occur when calcium hydrate was used.
DISCUSSION
Advances in tissue engineering and studies with bioactive molecules has provided new methods and resources to preserve pulp vitality, which represents the main source to produce reparatory dentin, without compromising the lifetime of the tooth element and not causing any dystrophic calcifications.
55
ISSA, M. J. P. ; NASCIMENTO, C., TIOSSI; PITOL, D. L. & IYOMASA, M. M. Bone morphogenetic proteins: Its application in the process of reparing the dentin pulp complex. Int. J. Odontostomat., 1(1):53-58, 2007.
Lianjia et al., (1993) reported that, one week after pulp capping with BMP, a small sign of inflammation was found; however, at the end of the second week, a small formation of osteodentin was present, without the formation of the dentin bridge, thus showing one of the main advantages of BMP use, as capping material. Tissue engineering is a complex and multidisciplinary field that uses knowledge from biological and biochemical sciences, aiming to promote induction, conduction and cell transplant with different approaches and objectives (Kaigler et al., 2001). Within this context, first questionings about processes that lead to osseous neo-formation on sites not provided with osseous tissues, are attributed to Urist & Strates (1971) and, to them, a main factor would be responsible for this effect. This factor was reported as a substance inductor of osseous formation present in the collagen osseous matrix. The authors also state that the inducing cells and the inducted cells are from the host and that
these same inductive cells are descendent from mobile histiocytes and cells from the perivascular conjunctive tissue.
CONCLUSIONS
As found in Literature, the use of morphogenetic proteins, especially BMP-7 or OP-1, are well indicated to be used for direct pulp capping in vital teeth that suffered from pulp exposure. As studies showed, the capacity of stimulating pulp cells to produce high quality of reparatory dentin, reporting better and more promising results, when compared to results found with the use of calcium hydrate compounds. However, more clinical studies should be made and to prove with more samples, their indication and to know the effects and mechanisms by which BMPs stimulate pulp repair and regeneration, with clarity and security.
ISSA, M. J. P. ; NASCIMENTO, C., TIOSSI; PITOL, D. L. & IYOMASA, M. M. Protenas seas morfogenticas: Su aplicacin en el Processo de reparacin del complejo dentina pulpa. Int. J. Odontostomat., 1(1):53-58, 2007. RESUMEN: La evolucin del conocimiento relacionado a la Biologa Molecular ha sido aplicado en diferentes reas de la Biologa Clnica, entre ellas la Odontologa, permitiendo el uso de esos nuevos adelantos en el tratamiento de agresiones al rgano pulpar. El uso de protenas seas morfogenticas (BMPs), representa otra posibilidad en el tratamiento de pulas expuestas sin la presencia de agentes agresores, libre principalmente de los efectos indeseables a la mantencin de la vitalidad pulpar. PALABRAS CLAVE: protena sea morfogentica, dentina reparadora, capeamento pulpar.
REFERENCES
Aeinehchi, M.; Eslami, B.; Ghanbarilha, M. & Saffar, A S. Mineral Trioxide Aggregate (MTA) and calcium hidroxide as pulp-capping agents in human teeth: a preliminary report. Int. Endod. J., 33(3):225-31, 2003. Bessho, K.; Tagawa, T. & Murata, M. Comparison of bone matrix-derived bone morphogenetic proteins from various animals. J. Oral Maxillofac. Surg., 50:496501, 1992. Cala, A. L. et al. O potencial da protena ssea morfogentica humana recombinante-2 (RH BMP2) na regenerao ssea. Rev. Bras. Odontol., 56(4):185-91, 1999. Clarkson, B. H.; Rafter, M. E. & Dent, B. Emerging methods used in the prevention and repair of carious
tissues. J. Dent. Educ., 65(10):1114-9, 2001. Cohen, S. et al. Similarities of T cell function in cell mediated immunity and antibody production. Cell Imunol., 12:150-9, 1975. Costa, C. A.; Mesas, A. N. & Hebling, J. Pulp response to direct capping whit an adhesive system. Am. J. Dent., 13(2):81-7, April. 2000. Cox, C.F.; Sbay, R. K. Ostro, E. & Suzuki, S. Tunnel defects in dentin bridges: Their formation following direct pulp capping. Oper. Dent., 21:4-11, 1996. Domnguez, M. S.; Whiterspoon, D. E.; Gutmann, J. L. & Opperman, L. A. Histological e scanning electron microscopy assessment of various vital pulp therapy materials. J. Endod, 29(5):324-33, 2003.
56
ISSA, M. J. P. ; NASCIMENTO, C., TIOSSI; PITOL, D. L. & IYOMASA, M. M. Bone morphogenetic proteins: Its application in the process of reparing the dentin pulp complex. Int. J. Odontostomat., 1(1):53-58, 2007.
Faraco, I. M. & Holland, R. Response of the pulp of dogs to capping with mineral trioxide aggregate or a calcium hydroxide cement. Dent. Traumatol., 17(4):163-6, 2001. Ford, T. R.; Torabinejad, M.; Abedi, H.R.; Bakland, L.K. 6 Kariyavasam, S. P. Using mineral trioxide aggregate as a pulp-capping material. J. Am. Dent. Assoc., 127(10):1491-4, 1996. Foreman, P. C. & Barnes, I. E. Review of calcium hydroxide. Int. Endod. J., 23:283-7, 1990. Goldberg, M.; Six, N.; Lasfargues, J. J.; Salih, E.; Tompkins, K. & Veis A. Bioactive molecules and the future of pulp therapy. Am. J. Dent., 16(1):6676, 2003. Helder, M. N.; Karg, H.; Bervoets, T. J. M.; Vukicevic, S.; Burger, E. H.; Douza, R. N.; Wltgens, J. H. M.; Karsenty, G. & Bronckers, A. L. Bone morphogenetic protein-7 (osteogenic protein-1, OP-1) and tooth development. J. Dent. Res., 77(4):545-53, 1998. Igarashi, R; Sahara, T; Shimizu-Ishiura, M. & Sasaki, T. Porcine enamel matrix derivative enhances the formation of reparative dentine and dentine bridges during wound healing of amputed rat molars. J. Electron. Microsc., 52(2):227-36, 2003. Ishizaki, N.T; Matsumoto, K; Kimura, Y.; Wang, X. & Yamashita, A. Histopathological study of dental pulp tissue capped with enamel matrix derivative. J. Endod. 29(3):176-9, 2003. Kaigler, D. & Mooney, D. Tissue engineerings impact on dentistry. J. Dent. Educ., 65(5):456-62, 2001. Lianjia, Y.; Yuhao, G. & White, F.H. Bovine bone morphogenetic protein-induced dentinogenesis. Clin. Orthop. Rel. Res., 295:305-12, 1993. Matsumoto, K. & Lyngstadaas, S.P. The induction of reparative dentin by enamel proteins. Int. Endod. J., 35(5):407, 2002. Melin, M.; Joffreromeas, A.; Farges, J.C.; Couble, M. L.; Magloire, H. & Bleicher, F. Effects of TGFb 1 on dental pulp cells in cultured human tooth slices. J. Dent. Res., 79(9):1689-95, 2000. Mondelli, J. Proteo do Complexo Dentino-pulpar. Artes Mdicas, EAP, APCD, 1998. pp.125-301.
Murray, P. E.; Kitasako,Y.; Tagami, J.; Windsor, L. J. & Smith, A. J. Hierarchy of variables correlated to odontoblast-like cell numbers followung pulp capping. J. Dent., 30:297-304, 2002. Nakashima, M. The induction of reparative dentine in the amputated dental pulp of the dog by bone morphogenetic protein. Archs. Oral Biol., 35(7):4937, 1990. Negm, M. M.; Combe, E. C. & Grant, A. A. Reaction of the exposed pulps to new cementes containing calcium hydroxide. Oral Surg. Oral Med. Oral Pathol., 51(2):190-204, 1981. Rutherford, R. B.; Wahle, J.; Tucker, M.; Rueger, D. & Charette, M. Induction of reparative dentine formation in monkeys by recombinant human osteogenic protein-1. Archs. Oral Biol., 38(7):5716, 1993. Rutherford, R. B.; Spangberg, L.; Tucker, M.; Rueger, D.; Charette, M. The time-course of the induction of reparative dentine formation in monkeys by recombinant human osteogenic protein-1. Archs. Oral Biol., 39(10):833-8, 1994. Rutherford, R. B.; Charette, M. & Rueger, D. Role of osteogenic(bone morphogenetic) protein and platelet-derived growth factor in periodontal wound healing. In Genco, R. et al. Molecular basis of periodontal disease, 1994. pp.427-37 Rutherford, R. B.; Spangberg, L.; Tucker, M. & Charette, M. Transdentinal stimulation of reparative dentine formation by osteogenic protein-1 in monkeys. Arch. Oral Biol., 40(7):681-3, 1995. Six, N.; Lasfargues, J. J. & Goldberg, M. Differential repair responses in the coronal and radicular areas of the exposed rat molar pulp induced by recombinant human bone morphogenetic protein 7 (osteogenic protein 1). Arch. Oral Biol., 47(3):17787, 2002. Stanley, H .R. Pulp capping: conserving the dental pulpcan it be done? Is it worth it? Oral Surg. Oral Med. Oral Pathol., 68:628-39, 1989. Toriumi, D. M. & Robertson, K. Bone inductive biomaterials in facial plastic and reconstructive surgery. Facial Plastic Surgery, 9(1):29-36, 1993.
57
ISSA, M. J. P. ; NASCIMENTO, C., TIOSSI; PITOL, D. L. & IYOMASA, M. M. Bone morphogenetic proteins: Its application in the process of reparing the dentin pulp complex. Int. J. Odontostomat., 1(1):53-58, 2007.
Turner, C.T.; Courts, F. J. & Stanley, H.R. A histological comparison of direct pulp, capping agents in primary canines. ASDC J. Dent. Child., 54(6):423-8, 1987. Tziafas, D.; Pantelidou, O; Alvanou, A.; Belibasakis, G. & Papadimitriou, S. The dentinogenic effect of mineral trioxide aggregate (MTA) in short-term capping experiments. Int. End. J. 35(3):245-54, 2002. Ulmansky, M.; Sela, J. & Sela, M. Scanning electron microscopy of calcium hydroxide induced bridges. J. Oral Pathol.,1:244-8, 1972. Urist, M. R. & Strates, B. S. Bone morphogenetic protein. J. Dent. Res., 50(6):1392-406, 1971. Walton, R. E. & Langeland, K. Migration of materials in the dental pulp of monkeys. J. End., 4:167-77, 1978. Weinreb, M. M.; Sharav, Y. & Ickowicz, M. The recuperative capacity of the pulp. Arch. Oral Biology, 17(2):393-404, 1967.
Correspondence to: Joo Paulo Mardegan Issa Depto. de Morfologia, Estomatologia e Fisiologia Faculdade de Odontologia de Ribeiro Preto Av. Caf S/N, CEP: 14040-904 Ribeiro Preto-SP - BRAZIL. Phone: +55 16 9717-0509 or 3602-4095 E-mail: jpmissa@forp.usp.br Received: 04-03-2007 Accepted: 16-04-2007
58
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- SSNDocument1,377 pagesSSNBrymo Suarez100% (9)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- PH Miracle Complete Whole Body Alkalizing Program-1201724Document20 pagesPH Miracle Complete Whole Body Alkalizing Program-1201724joao carlos100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- SWOT AnalysisDocument6 pagesSWOT Analysishananshahid96No ratings yet
- Solidwork Flow Simulation TutorialDocument298 pagesSolidwork Flow Simulation TutorialMilad Ah100% (8)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- UFO Midwest Magazine April2011Document16 pagesUFO Midwest Magazine April2011Jimi HughesNo ratings yet
- Checklist For Mold RemediationDocument2 pagesChecklist For Mold Remediation631052No ratings yet
- Finishing of Posterior CompositeDocument3 pagesFinishing of Posterior CompositessaikalyanNo ratings yet
- Finishing of Posterior CompositeDocument3 pagesFinishing of Posterior CompositessaikalyanNo ratings yet
- Publications FireSafetyDesign SDocument369 pagesPublications FireSafetyDesign SJayachandra Reddy AnnavaramNo ratings yet
- 14 - Hydraulic Design of Urban Drainage Systems PDFDocument45 pages14 - Hydraulic Design of Urban Drainage Systems PDFDeprizon SyamsunurNo ratings yet
- Solution of Introduction To Many-Body Quantum Theory in Condensed Matter Physics (H.Bruus & K. Flensberg)Document54 pagesSolution of Introduction To Many-Body Quantum Theory in Condensed Matter Physics (H.Bruus & K. Flensberg)Calamanciuc Mihai MadalinNo ratings yet
- Fabm2 q2 Module 4 TaxationDocument17 pagesFabm2 q2 Module 4 TaxationLady HaraNo ratings yet
- ASCP User GuideDocument1,566 pagesASCP User GuideThillai GaneshNo ratings yet
- Gas Chromatography - COLIN F. POOLE 2012 PDFDocument743 pagesGas Chromatography - COLIN F. POOLE 2012 PDFVo Manh Tien100% (1)
- SRS documentation of Virtual Classroom System , SRS documentation of Personal Identity Management ,SRS documentation of EMentoring for women system , SRS Documentation of Employee Performance Management SRS Documentation of Online TicketingDocument79 pagesSRS documentation of Virtual Classroom System , SRS documentation of Personal Identity Management ,SRS documentation of EMentoring for women system , SRS Documentation of Employee Performance Management SRS Documentation of Online Ticketingsaravanakumar1896% (26)
- NRSPDocument27 pagesNRSPMuhammad Farhan67% (3)
- 541Document12 pages541ssaikalyanNo ratings yet
- Clearing ReveiwDocument2 pagesClearing ReveiwssaikalyanNo ratings yet
- Nano Technology in Civil EngineeringDocument8 pagesNano Technology in Civil EngineeringNArendra REddyNo ratings yet
- Perio and Endo RegenerationDocument8 pagesPerio and Endo RegenerationNoor SolikhahNo ratings yet
- Pes PlanusDocument36 pagesPes PlanusssaikalyanNo ratings yet
- Photography in DentistryDocument8 pagesPhotography in DentistryssaikalyanNo ratings yet
- Teach-Introducing A SpeakerDocument8 pagesTeach-Introducing A SpeakerssaikalyanNo ratings yet
- Observations and Results: Table No.1: Distribution of Samples and Groups Under StudyDocument9 pagesObservations and Results: Table No.1: Distribution of Samples and Groups Under StudyssaikalyanNo ratings yet
- Mineral Trioxide AggregateDocument1 pageMineral Trioxide AggregatessaikalyanNo ratings yet
- Mta and External ResorptionDocument9 pagesMta and External ResorptionssaikalyanNo ratings yet
- Primary Homework Help Food ChainsDocument7 pagesPrimary Homework Help Food Chainsafnaxdxtloexll100% (1)
- Modification Adjustment During Upgrade - Software Logistics - SCN WikiDocument4 pagesModification Adjustment During Upgrade - Software Logistics - SCN Wikipal singhNo ratings yet
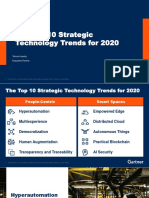
- The Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerDocument31 pagesThe Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerCarlos Stuars Echeandia CastilloNo ratings yet
- Lignan & NeolignanDocument12 pagesLignan & NeolignanUle UleNo ratings yet
- Case Study On Vivekananda Flyover BridgeDocument8 pagesCase Study On Vivekananda Flyover BridgeHeta PanchalNo ratings yet
- UntitledDocument4 pagesUntitledMOHD JEFRI BIN TAJARINo ratings yet
- ABRAMS M H The Fourth Dimension of A PoemDocument17 pagesABRAMS M H The Fourth Dimension of A PoemFrancyne FrançaNo ratings yet
- Monitoring Tool in ScienceDocument10 pagesMonitoring Tool in ScienceCatherine RenanteNo ratings yet
- Chapter One: Business Studies Class XI Anmol Ratna TuladharDocument39 pagesChapter One: Business Studies Class XI Anmol Ratna TuladharAahana AahanaNo ratings yet
- The Quantum Gravity LagrangianDocument3 pagesThe Quantum Gravity LagrangianNige Cook100% (2)
- Plumbing Arithmetic RefresherDocument80 pagesPlumbing Arithmetic RefresherGigi AguasNo ratings yet
- O - 6 Series Mill Operation Manual-ENDocument119 pagesO - 6 Series Mill Operation Manual-ENLeonardo OlivaresNo ratings yet
- Offshore Wind Turbine 6mw Robust Simple EfficientDocument4 pagesOffshore Wind Turbine 6mw Robust Simple EfficientCristian Jhair PerezNo ratings yet
- Microwave: Microwaves Are A Form ofDocument9 pagesMicrowave: Microwaves Are A Form ofDhanmeet KaurNo ratings yet
- Amo Plan 2014Document4 pagesAmo Plan 2014kaps2385No ratings yet
- KS4 Higher Book 1 ContentsDocument2 pagesKS4 Higher Book 1 ContentsSonam KhuranaNo ratings yet