Professional Documents
Culture Documents
5 8
Uploaded by
nandaciaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
5 8
Uploaded by
nandaciaCopyright:
Available Formats
medication on at least one occasion during the seven days of observation .
The corresponding numbers for the previous four-hour interval (from 16 to 20 hours after morning dose) were eight patients in the ADPREM group and 11 patients in the CRM group . Exploratory sensitivity analyses , excluding subjects with no rescue use , showed similar results for rescue medication and BTP endpoints (n 30) . The average pain intensity scores for the two treatments were comparable , and all differences between the treatments were small and statistically nonsignificant (Table 3) . The current pain intensity at the morning evaluation , 24 hours after the most recent exposure to ADPREM and 12 hours after the most recent exposure to CRM , showed similar low mean values , indicating that both ADPREM and CRM provided effective pain control at the end of their respective dosing intervals . Exploratory correlation analyses for rescue use and pain intensity ratings demonstrated a very high within-patient correlation between treatment periods (Fig . 2) . The median
value for assessment of the drugs by patients was 3 (good) for both treatments . The ranges were 1 (poor) to 4 (very good) for the ADPREM treatment and 1 (poor) to 5 (excellent) for the CRM treatment , with an estimated difference of 0.00 (95% CI 0.50 , 0 .50 , P=1.0) . Thirteen (37.1%) patients expressed a preference for ADPREM , 14 (40.0%) patients expressed a preference for CRM , eight (22 .9%) patients had no preference , and one value was missing . No difference between the two treatments was found (P= 1.0) . There were no differences between the treatments in plasma concentrations of morphine , M-3-G , or M-6-G at trough level 24 hours after the last dose of ADPREM and 12 hours after the last dose of CRM (Table 4) . Safety The pattern of the overall and treatment-related AEs did not differ between treatments , and this was what a clinician would reasonably expect in a population with advanced malignancy and chronic use of opioids . Treatment-related AEs occurred in five (12.8%) patients during treatment with ADPREM and six
(15.0%) patients during treatment with CRM . The most common treatment-related AEs were constipation (one [2 .6%] patient during ADPREM treatment and three [7.5%] patients during CRM treatment) followed by somnolence (one [2 .6%] patient during ADPREM treatment and two [5.0%] patients during CRM treatment) . All other treatment-related AEs were single episodes . Discussion When treating patients with chronic pain , the goal is to provide adequate 24-hour pain relief . In this study , a low incidence of BTP and a limited requirement for rescue medication was observed in both treatment arms , demonstrating that both ADPREM dosed once daily and CRM dosed twice daily provide effective pain control around the clock . A number of endpoints were included in this study to assess if the analgesic effect of ADPREM lasted for the entire 24-hour dosing interval . No differences between treatments were observed in use of rescue medication , number of BTP episodes
, or pain intensity in the hours preceding the morning dose , indicating a similar 24-hour pain control with both treatments . In addition , the small number of patients experiencing BTP even once during the final four hours of the dosing interval and the absence of a trend for increasing numbers of patients with BTP episodes at the end of the dosing interval suggest that , in these patients , episodes of BTP were not attributable to the analgesic effect wearing off . Overall , the results , therefore , indicate that ADPREM provides effective pain control for the entire 24-hour dosing interval . In support of the similarities between the treatments for the pharmacodynamic endpoints , the trough plasma levels of morphine and its metabolites , 24 hours after the last dose of ADPREM and 12 hours after the last dose of CRM , were similar . A 90% CI within the 0 .80e1 .25 bioequivalence limits was nearly met in this small exploratory study (Table 4); retrospective calculations show that 80% power to achieve these equivalence margins in a future study would require 91 subjects . Patient ratings of satisfaction and preference provide important information about the overall perception of
treatment
effect
for
the
individual
patient
and
are
recommended to support repeated measurements of pain intensity .15 In this study , the assessment of the drugs was similar for the two treatments , and neither treatment was clearly preferred , supporting the similarity of ADPREM and CRM in the integrated treatment effect on pain , physical functioning , emotional state , and AEs . This study had some limitations . The trough concentrations measured were not exactly at 12 and 24 hours after the previous doses of CRM and ADPREM , respectively; the samples were collected between 11 hours and 20 minutes and 11 hours and 55 minutes after the last dose of CRM and between 23 hours and 30 minutes and 24 hours after the last dose of ADPREM . However , the steadystate plasma concentration vs . time profiles are almost horizontal from 11 to 12 hours after last dose of CRM16 and from 12 to 24 hours after last dose of ADPREM (Egalet a/s , unpublished data) . Hence , collecting the samples within the allowed one-hour window before the next dose would not lead to any significant differences in the estimated end-of-dose concentrations .
Few subjects took IR rescue morphine during the early morning hours before the phar-macokinetic sampling . To assess the potential influence of IR rescue use on the trough levels of morphine and its metabolites , the analysis of end-of-dose concentration was performed for the FAS and for the subset of subjects who had not taken rescue medication during the fourhour interval before sampling . The results were similar . This study was the first one with ADPREM in a patient population . It was designed as an exploratory study in a relatively small population to provide proof of concept for the analgesic efficacy of ADPREM morphine dosed once daily and provide a basis for sample size estimation for a future full-scale proof of efficacy . Hence , no prospective sample size calculation was performed and no preplanned equivalence margin was defined . A retrospective power calculation showed that the present study had greater than 99% power to show noninferiority in the number of rescue doses with a margin of less than one rescue dose/ day . Requiring or not requiring a dose of rescue medication is a valid indicator of the patients perception of pain and has been considered a clinically
appropriate outcome measurement to study the efficacy of the basal therapy .17 The high intrapatient correlation for rescue use and pain ratings was expected , considering that pain is a highly subjective experience ,18 and supports the rationale for a crossover design in early analgesic studies . A risk when performing crossover studies in a population of patients with a progressive disease , such as cancer , is that pain intensity and , hence , doses of morphine are often increased over time; however , no effect of period was detected in any of the analyses of the present study . Contrary to the narrow CIs for the endpoints related to the experience of pain , the CIs for the trough concentrations were relatively wide . This may be because patient characteristics only predict minor parts of the variability in plasma concentration of morphine and metabolites ,19 and the variability of PK parameters has been reported to be higher in patients than in healthy volunteers .20 The polymer-based erodible matrix has proven to be a simple way to provide a stable steady-state morphine concentration through once-daily oral dosing . As an additional advantage , a
recent noninterventional interview study in recreational drug users has confirmed that the physical and chemical properties of ADPREM may give rise to low abuse and tampering attractiveness compared with seven well-known marketed opioids .21 In conclusion , the results of this exploratory first-in-patients study show that ADPREM dosed once daily provides similar trough plasma levels of morphine and analgesic efficacy as CRM , another commonly used CR morphine product , dosed twice daily in cancer patients with chronic pain . No end-ofdose failure was detected at the end of the 24-hour dosing interval for ADPREM , confirming the intended once-daily dosage regimen for the formulation . With a once-daily dosage regimen and low tampering potential , ADPREM is considered a highly relevant new oral formulation of morphine sulfate .
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Mitsubishi Evo Vii Workshop ManualDocument1,471 pagesMitsubishi Evo Vii Workshop ManuallimaynardNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Baroque MusicDocument15 pagesBaroque Musicthot777100% (2)
- Instruction Manual for Capacitor Voltage TransformersDocument22 pagesInstruction Manual for Capacitor Voltage Transformerst.o.i.n.gNo ratings yet
- Models of Collaboration Between Education and ServicesDocument17 pagesModels of Collaboration Between Education and ServicesSimran Josan100% (3)
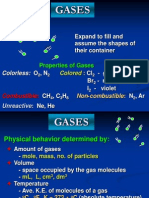
- Properties and Behavior of GasesDocument34 pagesProperties and Behavior of GasesPaul Jeremiah Serrano NarvaezNo ratings yet
- Unitized Curtain Wall SystemDocument38 pagesUnitized Curtain Wall Systems.senthil nathan100% (1)
- D5092 - Design and Installation of Ground Water Monitoring Wells in AquifersDocument14 pagesD5092 - Design and Installation of Ground Water Monitoring Wells in Aquifersmaxuelbestete100% (1)
- Vertebrates and InvertebratesDocument4 pagesVertebrates and InvertebratesJane Aubrey Saligan100% (2)
- VFTO DocumentationDocument119 pagesVFTO DocumentationSheri Abhishek ReddyNo ratings yet
- Fine Reader CMDDocument5 pagesFine Reader CMDferrousweiNo ratings yet
- EULA0Document14 pagesEULA0MRNNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Vancouver Reference SystemDocument11 pagesVancouver Reference SystemnandaciaNo ratings yet
- Service Agreement - Zeroid PDFDocument2 pagesService Agreement - Zeroid PDFYushau Muhammad LawalNo ratings yet
- Space Oddity Chords (Ver 2) by David Bowie Tabs at Ultimate Guitar ArchiveDocument3 pagesSpace Oddity Chords (Ver 2) by David Bowie Tabs at Ultimate Guitar ArchiveEMMANUEL ARNOULDNo ratings yet
- EM2P70CLP (LBP) - DatasheetDocument4 pagesEM2P70CLP (LBP) - DatasheetMarquesNo ratings yet
- IT Department - JdsDocument2 pagesIT Department - JdsShahid NadeemNo ratings yet
- Sujet Dissertation Sciences PolitiquesDocument7 pagesSujet Dissertation Sciences PolitiquesDoMyPaperSingapore100% (1)
- ADJECTIVES ENDING IN Ing and EdDocument1 pageADJECTIVES ENDING IN Ing and EdRafael FloresNo ratings yet
- Special Functions of Signal ProcessingDocument7 pagesSpecial Functions of Signal ProcessingSaddat ShamsuddinNo ratings yet
- Handout 4-6 StratDocument6 pagesHandout 4-6 StratTrixie JordanNo ratings yet
- Cronbach AlphaDocument15 pagesCronbach AlphaRendy EdistiNo ratings yet
- Rebecca A. Endaya Beed-Iii Art Education: ExploreDocument5 pagesRebecca A. Endaya Beed-Iii Art Education: ExploreBhecca Endaya0% (1)
- Investors' Perceptions of StocksDocument95 pagesInvestors' Perceptions of StocksPriya Ramanathan67% (3)
- The 5th Edition of The World Health Organization Classification - of Haematolymphoid Tumours Myeloid and Histiocytic - Dendritic NeoplasmsDocument17 pagesThe 5th Edition of The World Health Organization Classification - of Haematolymphoid Tumours Myeloid and Histiocytic - Dendritic NeoplasmsADMINISTRACION LABORATORIO INTERMEDICANo ratings yet
- Lipofectamine3000 ProtocolDocument2 pagesLipofectamine3000 ProtocolSamer AshrafNo ratings yet
- WEEK 1 Materi-EM101-M01-The Foundation of Business 2Document48 pagesWEEK 1 Materi-EM101-M01-The Foundation of Business 2ddhani299No ratings yet
- HavellsDocument4 pagesHavellsanurag_iiitmNo ratings yet
- FDocument109 pagesFssissaaNo ratings yet
- Tie Technology DK SKDocument32 pagesTie Technology DK SKVladimir PleșcaNo ratings yet
- Che 430 Fa21 - HW#5Document2 pagesChe 430 Fa21 - HW#5Charity QuinnNo ratings yet
- SYKES Home Equipment Agreement UpdatedDocument3 pagesSYKES Home Equipment Agreement UpdatedFritz PrejeanNo ratings yet
- Urea CycleDocument2 pagesUrea CycleyoungdandareNo ratings yet
- Literature Review BUS 507 PDFDocument18 pagesLiterature Review BUS 507 PDFtanmoy8554No ratings yet