Professional Documents
Culture Documents
Tetralogy of Fallot Patient Case
Uploaded by
Benjamin LeonzonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tetralogy of Fallot Patient Case
Uploaded by
Benjamin LeonzonCopyright:
Available Formats
I.
PATIENTS PERSONAL DATA Name: Mark Andrei Malapitan Quijano Age: 2 years and 6 months Birthday : October 1, 2008 Gender: Male Civil Status: Child Address: 2016-116 San Roque St. Sangandaan Quezon City Religion: Roman Catholic Chief Complaint: Difficulty of Breathing Tentative Diagnosis: TGA, VSD, PS Final Diagnosis: Tetralogy of Fallot Attending Physician: Dr. Paolo Becina II. Patients Health History Past Health History According to the patients mother, she thought that her child was born normally. But when the child undergone a follow up check up one week after the childs birth the doctor wondered why is it that when the child cries the childs skin color changes (violet ). Thats when they decided to follow the doctors suggestion which is to submit the child for further evaluation or diagnostic exams. The result is, the child has aTETRALOGY OF FALLOT. Present Health History The child is admitted in NCH since March 31, 2011. According to his mother they decided to brought the child in the hospital because he suffers from excessive gasping of breath , and the child complaint of chest pain. The child is now discharge (April 26, 2011) . His scheduled for follow up check up is on May 9, 2011.
III. Developmental Task Will: Autonomy vs. Shame & Doubt (Toddlers, 2 to 4 years) Psychosocial Crisis: Autonomy vs. Shame & Doubt Main Question: "Can I do things myself or must I always rely on others?" Virtue: Will
As the child gains control over eliminative functions and motor abilities, they begin to explore their surroundings. The parents still provide a strong base of security from which the child can venture out to assert their will. The parents' patience and encouragement helps foster autonomy in the child. Children at this age like to explore their world around them and they are constantly learning about their environment. Caution must be taken at this age while children may explore things that are dangerous to their health and safety. At this age, children develop their first interests. For example, a child that enjoys music may like to play with the radio. Children that enjoy the outdoors may be interested in animals and plants. Highly restrictive parents, however, are more likely to instill the child with a sense of doubt and reluctance to attempt new challenges. As they gain increased muscular coordination and mobility, toddlers become capable of satisfying some of their own needs. They begin to feed themselves, wash and dress themselves, and use the bathroom. If caregivers encourage self-sufficient behavior, toddlers develop a sense of autonomy- a sense of being able to handle many problems on their own. But if caregivers demand too much too soon, refuse to let children perform tasks of which they are capable, or ridicule early attempts at self-sufficiency, children may instead develop shame and doubt about their ability to handle problems.
IV. ANATOMY AND PHYSIOLOGY The Heart The heart itself is made up of 4 chambers, 2 atria and 2 ventricles. De-oxygenated blood returns to the right side of the heart via the venous circulation. It is pumped into the right ventricle and then to the lungs where carbon dioxide is released and oxygen is absorbed. The oxygenated blood then travels back to the left side of the heart into the left atria, then into the left ventricle from where it is pumped into the aorta and arterial circulation. Image: The passage of blood through the heart
The pressure created in the arteries by the contraction of the left ventricle is the systolic blood pressure. Once the left ventricle has fully contracted it begins to relax and refill with blood from the left atria. The pressure in the arteries falls whilst the ventricle refills. This is the diastolic blood pressure. The atrio-ventricular septum completely separates the 2 sides of the heart. Unless there is a septal defect, the 2 sides of the heart never directly communicate. Blood travels from right side to left side via the lungs only. However the chambers themselves work together . The 2 atria contract simultaneously, and the 2 ventricles contract simultaneously. Cardiac Conduction System Going back to the analogy of the central heating system, the pump, pipes and radiators are of no use unless connected to a power supply. The pump needs electricity to work. The human heart has a similar need for a power source and also uses electricity. Thankfully we don't need to plug ourselves in to the mains, the heart is able to create it's own electrical impulses and control the route the impulses take via a specialised conduction pathway. This pathway is made up of 5 elements: 1. 2. 3. 4. 5. The The The The The sino-atrial (SA) node atrio-ventricular (AV) node bundle of His left and right bundle branches Purkinje fibres
Image: The cardiac conduction system
The SA node is the natural pacemaker of the heart. You may have heard of permanent pacemakers (PPMs) and temporary pacing wires (TPWs) which are used when the SA node has ceased to function properly.
The SA node releases electrical stimuli at a regular rate, the rate is dictated by the needs of the body. Each stimulus passes through the myocardial cells of the atria creating a wave of contraction which spreads rapidly through both atria. As an analogy, imagine a picture made up of dominoes. One domino is pushed over causing a wave of collapsing dominoes spreading out across the picture until all dominoes are down. The heart is made up of around half a billion cells, In the picture above you can see the difference in muscle mass of the various chambers. The majority of the cells make up the ventricular walls. The rapidity of atrial contraction is such that around 100 million myocardial cells contract in less than one third of a second. So fast that it appears instantaneous. The electrical stimulus from the SA node eventually reaches the AV node and is delayed briefly so that the contracting atria have enough time to pump all the blood into the ventricles. Once the atria are empty of blood the valves between the atria and ventricles close. At this point the atria begin to refill and the electrical stimulus passes through the AV node and Bundle of His into the Bundle branches and Purkinje fibres. Imagine the bundle branches as motorways, if you like, with the Purkinje fibres as A and B roads that spread widely across the ventricles . In this way all the cells in the ventricles receive an electrical stimulus causing them to contract. Using the same domino analogy, around 400 million myocardial cells that make up the ventricles contract in less than one third of a second. As the ventricles contract, the right ventricle pumps blood to the lungs where carbon dioxide is released and oxygen is absorbed, whilst the left ventricle pumps blood into the aorta from where it passes into the coronary and arterial circulation. At this point the ventricles are empty, the atria are full and the valves between them are closed. The SA node is about to release another electrical stimulus and the process is about to repeat itself. However, there is a 3rd section to this process. The SA node and AV node contain only one stimulus. Therefore every time the nodes release a stimulus they must recharge before they can do it again. Imagine you are washing your car and have a bucket of water to rinse off the soap. You throw the bucket of water over the car but find you need another one. The bucket does not magically refill. You have to pause to fill it. In the case of the heart, the SA node recharges whilst the atria are refilling, and the AV node recharges when the ventricles are refilling. In this way there is no need for a pause in heart function. Again, this process takes less than one third of a second. The times given for the 3 different stages are based on a heart rate of 60 bpm , or 1 beat per second. The term used for the release (discharge) of an electrical stimulus is "depolarisation", and the term for recharging is "repolarisation". So, the 3 stages of a single heart beat are: 1. Atrial depolarisation 2. Ventricular depolarisation
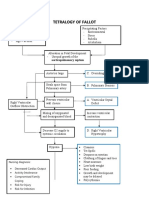
3. Atrial and ventricular repolarisation. As the atria repolarise during ventricular contraction, there is no wave representing atrial repolarisation as it is buried in the QRS. V. PATHOPHYSIOLOGY Primary four malformations "Tetralogy" denotes a four-part phenomenon in various fields, including literature, and the four parts the syndrome's name implies are its four signs. This is not to be confused with the similarly named teratology, a field of medicine concerned with abnormal development and congenital malformations, which thereby includes tetralogy of Fallot as part of its subject matter. As such, by definition, tetralogy of Fallot involves exactly four heart malformations which present together:
Tetralogy of Fallot Condition A: Pulmonary stenosis
Normal Heart Condition Description
A narrowing of the right ventricular outflow tract and can occur at the pulmonary valve (valvular stenosis) or just below the pulmonary valve (infundibular stenosis). Infundibular pulmonic stenosis is mostly caused by overgrowth of the heart muscle wall (hypertrophy of the septoparietal trabeculae), however the events leading to the formation of the overriding aorta are also believed to be a cause. The pulmonic stenosis is the major
cause of the malformations, with the other associated malformations acting as compensatory mechanisms to the pulmonic stenosis. The degree of stenosis varies between individuals with TOF, and is the primary determinant of symptoms and severity. This malformation is infrequently described as sub-pulmonary stenosis or subpulmonary obstruction. B: Overriding aorta C: ventricular septal defect (VSD) D: Right ventricular hypertrophy An aortic valve with biventricular connection, that is, it is situated above the ventricular septal defect and connected to both the right and the left ventricle. The degree to which the aorta is attached to the right ventricle is referred to as its degree of "override." The aortic root can be displaced toward the front (anteriorly) or directly above the septal defect, but it is always abnormally located to the right of the root of the pulmonary artery. The degree of override is quite variable, with 5-95% of the valve being connected to the right ventricle. A hole between the two bottom chambers (ventricles) of the heart. The defect is centered around the most superior aspect of the ventricular septum (the outlet septum), and in the majority of cases is single and large. In some cases thickening of the septum (septal hypertrophy) can narrow the margins of the defect. The right ventricle is more muscular than normal, causing a characteristic boot-shaped (coeur-en-sabot) appearance as seen by chest X-ray. Due to the misarrangement of the external ventricular septum, the right ventricular wall increases in size to deal with the increased obstruction to the right outflow tract. This feature is now generally agreed to be a secondary anomaly, as the level of hypertrophy generally increases with age.
There is anatomic variation between the hearts of individuals with tetralogy of Fallot. Primarily, the degree of right ventricular outflow tract obstruction varies between patients and generally determines clinical symptoms and disease progression.
VI. Laboratory Test After your baby is born, your baby's doctor may suspect tetralogy of Fallot if the baby has blue-tinged skin or if a heart murmur an abnormal whooshing sound caused by turbulent blood flow is heard in your child's chest. By using several tests, your doctor can confirm the diagnosis. Chest X-ray. A typical sign of tetralogy of Fallot on an X-ray is a "boot-shaped" heart, because the right ventricle is enlarged. Blood test. Your child will need a test that measures the number of each type of cell in the blood, called a complete blood count. In tetralogy of Fallot, the number of red blood cells may be abnormally high (erythrocytosis) as the body attempts to increase the oxygen level in the blood. Oxygen level measurement (pulse oximetry). This test uses a small sensor that can be placed on a finger or toe to measure the amount of oxygen in the blood. Echocardiography. Echocardiograms use high-pitched sound waves, inaudible to the human ear, to produce an image of the heart. Sound waves bounce off your baby's heart and produce moving images that can be viewed on a video screen. This test helps diagnose tetralogy of Fallot because it allows the doctor to see whether there is a ventricular septal defect, if the structure of the pulmonary valve is normal, if the right ventricle is functioning properly, and if the aorta is positioned properly.
Electrocardiogram. An electrocardiogram records the electrical activity in the heart each time it contracts. During this procedure, patches with wires (electrodes) are placed on your baby's chest, wrists and ankles. The electrodes measure electrical activity, which is recorded on paper. This test helps determine if your baby's right ventricle is enlarged (ventricular hypertrophy) and if the heart rhythm is regular. Cardiac catheterization. During this procedure, your doctor inserts a thin flexible tube (catheter) into an artery or vein in your baby's groin and threads it up to his or her heart. A dye is injected through the catheter to make your baby's heart structures visible on X-ray pictures. The catheter also measures pressure and oxygen levels in the chambers of the heart and in the blood vessels.
VII. DRUG STUDY Medicine Dosage, frequency & route of administratio n OD Indication Contraindication Adverse Reaction Nursing Implication
Multivitamin s
Use to treat vitamin deficiencies caused by illness, pregnancy, poor nutrition, digestive disorders, and many other conditions
Stomach upset, headache, unpleasant taste in mouth Contraindicated in those persons who have shown hypersensitivity to any component of this preparation.
1. Assess patient for signs of nutritional deficiency prior to & throughout therapy. 2. Interact to notify side effect of medication to physician 3. Encourace to comply on medications 4. Advise parents to refer to chewable multivitamins for children as candy.
OD Ascorbic acid
Vit C deficiency. Common colds, wound healing, prevents fragility of small blood vessels & gums, normocytic or macrocytic anemia, cartilage & bone. Increased resistance to stress & infections.
Contraindicated in those persons who have shown hypersensitivity to any component of this preparation.
Diarrhea, GI disturbances, renal Ca oxalate calculi.
Assessment & drug effects Lab tests: periodic hct & hgb, serum electrolytes. Monitor for S&S of acute hemolytic anemia, sickle cell crisis.
ORS
Prevention of dehydration & maintenance of normal fluid electrolyte balance in mild to moderate diarrhea secondary to acute diarrhea in infants & children.
Intractable vomiting, adynamic ileus, intestinal obstruction, bowel perforation.
Give rise to further complications including radiosensitization effct on thorx, skin inflammation, esophageal inflammation. Life- threatening effects include bone marrow suppression, neutropenic fever, anaphylactic reactions.
1. Give exact amount of oresol according to patients age. 2. If child vomits, wait for 10 mins then give the oresol again. 3. Give child alternately other fluids such as breast milk or juices.
Zinc Sulfate
OD to complete 14 days
helps stimulate the activities of many enzymes, promoting normal biochemical reactions in the body. Adequate daily zinc supplementation helps strengthen the immune system. Supports normal growth & development. Also helps in the management of acute diarrhea in infants & children.
Administration of emetics or gastric lavage in case of acute overdosage.
GI disturbances eg abdominal pain, dyspepsia, nausea, vomiting, diarrhea, gastric irritation, & gastritis ( on an empty stomach).
Patients receiving long-term TPN. Prolonged administration of high doses may lead to copper deficiency with associated anemia and neutropenia. .
VIII. DISCHARGE PLAN
Advised to follow treatment regimen
Encouraged to provide a well ventilated area.
Reminded to have follow up check up @ OPD on May 9, 2011.
Encouraged to minimize activity to decrease cardiac worklosd. Advised how to do deep breathing and coughing exercises.
O D S
Advised to seek physicians help if the following signs and symptoms of TOF are observed such as cyanosis. DOB and chest pain. Diet for age. Advised to seek Spiritual Guidance always.
IX. Nursing Care Plan Cues/supporting data Nursing diagnosis Inference of the nursing diagnosis Planning Intervention Rationale Evaluation
Subjective: Sabi ng Doctor niya kulang yung O2 na dumadaloy sa dugo nya as verbalized by mother. Objective: Cyanosis Clubbing of nail beds Weak looking Clammy skin With abnormal heart sounds ( S3 noted) Difficulty of breathing Bradycardia (33 bpm) Cool extremities Bradycardia (77bpm)
Ineffective Tissue perfusion r/t heart defect.
Heart Defect After 8 hours of nursing intervention the patients O2 demand will be minimized.
Independent: Monitor quality of all pulses. Assessment is needed for ongoing comparisons; loss of peripheral pulses must be treated immediately. To decrease cardiac workload. The patients O2 demand lessen and the mother expresses understanding about her childs condition.
Pulmonary VSD Stenosis
Minimize Activity. Decreased distribution of oxygen. Place in Knee-chest position.
Ineffective Tissue Perfusion
Maintain Proper Ventilation. Collaborative: O2 therapy per doctors order.
For Wellness and Comfort.
To follow the treatment plan for adequate ventilation; sufficient O2 supply ; increasing arterial O2 saturation delivers more O2 to the myocardium. EEG, X-ray may be required for accurate diagnosis.
Assist with diagnostic testing as ordered.
Involve SO in planning of activities. Provide emotional support.
To plan and provide rest periods. The parents and the child will be able to express their fears; to diminished anxiety.
Subjective: Minsan nahihirapan siyang huminga, nag 50/50 na nga siya eh as verbalizedv by mother. Objective: Difficulty of Breathing Restlessness Cyanosis Irritable Hypoxia Bradypnea Cough Nasal flaring Use of accessory muscle Bradypnea (33 rpm) Ineffective Breathing Pattern.
Heart Defect After 8 hours of Nursing Intervention , mother will report minimal complaint of dyspnea.
Independent Asses RR, Rhythm and depth. RR, Rhythm changes are early warning signs of impending respiratory difficulties. Indicative of increase Respiratory effort. Signify increase in respiratory effort. Three-point position or orthopnea is associated with breathing difficulty. The mother report minimal complaint of dyspnea.
Pulmonary VSD Stenosis
Observe for excessive use of accessory muscles. Decreased distribution of oxygen. Note retractions of flaring of nostrils. Asses the position that the patient assumes for breathing.
Ineffective Breathing Pattern
X. Nursing Implication A. Nursing Practice Nursing education is the basic foundation for the nursing students to become good health provider through comprehension and internalization of the nursing concepts and practices. Through this case study, the students will gain additional information regarding the Pathophysiology, developmental task, proper medication and good nursing interventions of the case presented. B. Nursing Education Nursing practice is based from the nursing theories and principles that serve as a medium or basis for the nursing students in rendering services. This case study allows them to acquire sufficient knowledge regarding the case presented and for them to identify the accurate nursing interventions and proper judgments on the disease/ illness they encountered. This also allows the nursing students to distinguish the therapeutic approach including physical, psychological, emotional and moral needs of the client to restore the clients optimum level of functioning. C. Nursing Research
This case study is some sort of a research that is significant for the students who are studying this and for those persons suffering from this illness to be able to understand well this kind of phenomenon. This case study provides further explanations and elaborations of the etiology and Pathophysiology of the case presented. This also serves as reliable source or reference for those who are studying this kind of illness.
Catanduanes State Colleges COLLEGE OF HEALTH SCIENCES Virac, Catanduanes
CASE STUDY
( TETRALOGY OF FALLOT)
NATIONAL CHILDRENS HOSPITAL Nephro CARDIO HEMA WARD
Submmited by: RACHEL E. ALDEA
CLARISSA TRIJO DAVE SECORATA CESAR TAULE MARIANNE E. GONZALES BSN 3A/Grp 4 Submitted to:
MARY ELAINE TAPEL C.I
You might also like
- Tetralogy of Fallot Nursing CaseDocument32 pagesTetralogy of Fallot Nursing CaseUday Kumar50% (2)
- Tof Care PlanDocument4 pagesTof Care Plankayal67% (12)
- Tetralogy of Fallot OverviewDocument12 pagesTetralogy of Fallot OverviewMaricel Agcaoili GallatoNo ratings yet
- Case PresentationDocument43 pagesCase Presentationkayal100% (1)
- New Born NCPDocument8 pagesNew Born NCPCarl Vincent Marrion Rejuso100% (1)
- Tetralogy of FallotDocument5 pagesTetralogy of FallotCharity OaniaNo ratings yet
- pg1-33 of Pneumothorax Case StudyDocument36 pagespg1-33 of Pneumothorax Case StudyikemasNo ratings yet
- Tetralogy of FallotDocument22 pagesTetralogy of FallotHusna Aje100% (1)
- 1.case Presentation CHDDocument23 pages1.case Presentation CHDDHARM MEENA0% (1)
- Baby fever nursing careDocument6 pagesBaby fever nursing caregopscharanNo ratings yet
- Case Presentation HydrocephalusDocument48 pagesCase Presentation HydrocephalusSu Osman50% (2)
- Case Presentation On TOFDocument19 pagesCase Presentation On TOFJay PaulNo ratings yet
- NCP FORM For TetralogyDocument3 pagesNCP FORM For TetralogyGraceMelendres100% (3)
- Fully Met If: The InfantDocument4 pagesFully Met If: The InfantSheila Mae Alcaide DagdagNo ratings yet
- Tetralogy of Fallot Case DiscussionDocument46 pagesTetralogy of Fallot Case DiscussionJoe Ha50% (2)
- Acute Glomerulonephritis Case StudyDocument12 pagesAcute Glomerulonephritis Case StudyPrincess Tindugan100% (1)
- Tetralogy of Fallot Pathophysiology & Risk FactorsDocument1 pageTetralogy of Fallot Pathophysiology & Risk FactorsEiztirfNo ratings yet
- Section P - Group 1 E.C.S. - Pediatric Ward Mr. Ralph P. Pilapil, R.N. Clinical InstructorDocument62 pagesSection P - Group 1 E.C.S. - Pediatric Ward Mr. Ralph P. Pilapil, R.N. Clinical InstructorClaudine N SantillanNo ratings yet
- Uterine ProlapseDocument44 pagesUterine ProlapseMoi Mendoza83% (6)
- Case Studies - Tetralogy of FallotDocument16 pagesCase Studies - Tetralogy of FallotKunwar Sidharth SaurabhNo ratings yet
- CP Intestinal Obstruction Nursing Care PlanDocument7 pagesCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaNo ratings yet
- Anemia Unspecified FinalDocument47 pagesAnemia Unspecified FinalMaria Paula BungayNo ratings yet
- Prioritized Nursing Interventions for AtelectasisDocument7 pagesPrioritized Nursing Interventions for AtelectasisJinaan MahmudNo ratings yet
- Tetralogy of Fallot Lesson PlanDocument25 pagesTetralogy of Fallot Lesson PlanUday Kumar100% (1)
- Fluorosis Diagnosis, Patient Management, Monitoring and RecoveryDocument24 pagesFluorosis Diagnosis, Patient Management, Monitoring and RecoverydrjriNo ratings yet
- Care of Patients With Mechanical VentilatorDocument4 pagesCare of Patients With Mechanical VentilatorIman Bee Sanayon0% (1)
- Anatomy &physiology JaundiceDocument2 pagesAnatomy &physiology JaundiceHCX dghhqNo ratings yet
- Gastroenteritis: Causes, Symptoms, and Treatment of Stomach FluDocument49 pagesGastroenteritis: Causes, Symptoms, and Treatment of Stomach Flukinasal21No ratings yet
- NCP PPHDocument2 pagesNCP PPHMark Joseph Christian100% (1)
- Tracheo-Oesophageal FistulaDocument19 pagesTracheo-Oesophageal Fistularajan kumar100% (3)
- Case Studybleeding Biliary AtresiaDocument13 pagesCase Studybleeding Biliary Atresialawrence tayamNo ratings yet
- ConjunctivitisDocument16 pagesConjunctivitisClark LopezNo ratings yet
- Incompetent NCPDocument1 pageIncompetent NCPMina RacadioNo ratings yet
- Fetal CirculationDocument2 pagesFetal CirculationEric Gato100% (3)
- Tetralogy of FallotDocument10 pagesTetralogy of FallotanggiehardiyantiNo ratings yet
- Pneumonia Case StudyDocument33 pagesPneumonia Case StudyArceo AbiGail100% (3)
- Nursing Diagnosis For AsthmaDocument6 pagesNursing Diagnosis For AsthmaTINAIDA33% (3)
- SuctionDocument15 pagesSuctionMissy Shona100% (1)
- NCP - Poststreptococcal GlomerulonephritisDocument12 pagesNCP - Poststreptococcal GlomerulonephritisAya BolinasNo ratings yet
- Abruptio Placentae Case StudyDocument4 pagesAbruptio Placentae Case StudyMonchee YusonNo ratings yet
- Case Study Pleural EffusionDocument4 pagesCase Study Pleural EffusionKhristine Anne FabayNo ratings yet
- Severe Nausea and Vomiting in PregnancyDocument14 pagesSevere Nausea and Vomiting in Pregnancyamelina0% (1)
- NCP Proper 1Document6 pagesNCP Proper 1Noreen PinedaNo ratings yet
- HELLP Syndrome: A Variant of Severe PreeclampsiaDocument29 pagesHELLP Syndrome: A Variant of Severe PreeclampsiaNona Saudale100% (1)
- Tetralogy of FallotDocument31 pagesTetralogy of FallotAnditha Namira RS100% (1)
- Tetralogy of FallotDocument3 pagesTetralogy of FallotJohn Mark PocsidioNo ratings yet
- Tetralogy of Fallot Nursing Diagnosis and ManagementDocument2 pagesTetralogy of Fallot Nursing Diagnosis and ManagementKarl KiwisNo ratings yet
- Cardiac Case Study NDDocument11 pagesCardiac Case Study NDapi-313165458No ratings yet
- Cord ProlapseDocument4 pagesCord ProlapseCleta Escabarte Dehlin100% (1)
- CP Hydatidiform MoleDocument13 pagesCP Hydatidiform Molesweetheart_joannieNo ratings yet
- Case Presentation About Hypertension Stage 2-BeluanDocument36 pagesCase Presentation About Hypertension Stage 2-BeluanKeepItSecretNo ratings yet
- Managing Diabetes and RisksDocument8 pagesManaging Diabetes and RisksChristopher LontocNo ratings yet
- Case Study: Acute BronchitisDocument34 pagesCase Study: Acute BronchitisJeffany Anne Rabaya Retirado0% (1)
- Partograph Case StudiesDocument3 pagesPartograph Case StudiesAfra Minong100% (1)
- Case StudyDocument25 pagesCase StudybomcorNo ratings yet
- Exam For Self-GradingDocument11 pagesExam For Self-Gradingtayma 123No ratings yet
- Cardiology Teaching PackageDocument9 pagesCardiology Teaching PackageRicy SaiteNo ratings yet
- Heart PathophysiologyDocument20 pagesHeart PathophysiologyDoctorDrapion100% (2)
- LP-2 The HeartDocument6 pagesLP-2 The HeartDavidNo ratings yet
- EKG Study Guide RevisedDocument29 pagesEKG Study Guide Revisedflashyboy506No ratings yet
- RARBGDocument1 pageRARBGBenjamin LeonzonNo ratings yet
- Pharmacist Job DutiesDocument1 pagePharmacist Job DutiesBenjamin LeonzonNo ratings yet
- Nursing Care Plan Cesarian DeliveryDocument2 pagesNursing Care Plan Cesarian Deliveryderic97% (39)
- HEENTDocument1 pageHEENTBenjamin LeonzonNo ratings yet
- Acute Gastro Enteritis AssignmentDocument3 pagesAcute Gastro Enteritis AssignmentBenjamin LeonzonNo ratings yet
- Drug Name and Classification First Page Catapress MissionDocument1 pageDrug Name and Classification First Page Catapress MissionBenjamin LeonzonNo ratings yet
- Drug Name and Classification First Page Catapress MissionDocument1 pageDrug Name and Classification First Page Catapress MissionBenjamin LeonzonNo ratings yet
- Drug Name and Classification First Page Catapress MissionDocument1 pageDrug Name and Classification First Page Catapress MissionBenjamin LeonzonNo ratings yet
- ErecoveryDocument5 pagesErecoveryBenjamin LeonzonNo ratings yet
- Read MEDocument1 pageRead MEBenjamin LeonzonNo ratings yet
- Rice Noodles and South Beach Diet RecipesDocument8 pagesRice Noodles and South Beach Diet RecipesBenjamin LeonzonNo ratings yet
- RabiesDocument9 pagesRabiesBenjamin LeonzonNo ratings yet
- RabiesDocument9 pagesRabiesBenjamin LeonzonNo ratings yet
- Fading Rainbow - Abm Sycipgroup 1 1Document14 pagesFading Rainbow - Abm Sycipgroup 1 1Kate ParanaNo ratings yet
- CHAPTER 57 Anatomy and Surgical Access of The MediastinumDocument6 pagesCHAPTER 57 Anatomy and Surgical Access of The MediastinumAbeNo ratings yet
- Treating A Bartholins Cyst or Abscess Patient InformationDocument6 pagesTreating A Bartholins Cyst or Abscess Patient InformationRezaFArthaNo ratings yet
- Thesis List of EquationsDocument8 pagesThesis List of Equationsfc5g0qm1100% (2)
- Health 10: (Consumer Rights and Laws)Document14 pagesHealth 10: (Consumer Rights and Laws)Clint Harvey C. BicoNo ratings yet
- LRD DIV SPE FM 001a RITM Lab Test Request Form - Clinical Lab 1Document1 pageLRD DIV SPE FM 001a RITM Lab Test Request Form - Clinical Lab 1Megen PLCNo ratings yet
- Occupational Health and Safety Issues of Traffic EnforcersDocument16 pagesOccupational Health and Safety Issues of Traffic EnforcersRhobin Mhark GabitoNo ratings yet
- File 7165Document111 pagesFile 7165Riley ScherrNo ratings yet
- Lecture Notes For Introduction To Safety and Health PDFDocument216 pagesLecture Notes For Introduction To Safety and Health PDFTeshome Dengiso100% (1)
- Collaborative Drug Therapy ManagementDocument10 pagesCollaborative Drug Therapy ManagementAyu Dina UnifahNo ratings yet
- PPK PTL Copper Silver Ionization Mk2-Ptl Copsil Rev-20110503Document2 pagesPPK PTL Copper Silver Ionization Mk2-Ptl Copsil Rev-20110503Katty TsaiNo ratings yet
- 660d2SessionPlans A54967112265 Therapeutic Direct Current PDFDocument10 pages660d2SessionPlans A54967112265 Therapeutic Direct Current PDFmilananandNo ratings yet
- Traumatic Brain Injury Final 2013.5.29Document59 pagesTraumatic Brain Injury Final 2013.5.29asylum1968No ratings yet
- IELTS SpeakingDocument18 pagesIELTS SpeakingJohnNo ratings yet
- CUI Texto Examen Multimedia Nivel 6 Curso BasicoDocument2 pagesCUI Texto Examen Multimedia Nivel 6 Curso BasicobertoniramiroNo ratings yet
- Benign Paroxysmal Positional VertigoDocument12 pagesBenign Paroxysmal Positional VertigoErnesto Trinidad Jr RNNo ratings yet
- Digestive System Lab ReportDocument9 pagesDigestive System Lab Reportapi-296603931No ratings yet
- Formulation Science & Bioavailability: Pharmacological Parameters Study On Loop Diuretic Drug - FurosemideDocument3 pagesFormulation Science & Bioavailability: Pharmacological Parameters Study On Loop Diuretic Drug - FurosemidevivianNo ratings yet
- Fermented BiocharDocument81 pagesFermented Biocharstar662100% (1)
- 2010 SPN BL Rez MALDI TOFDocument12 pages2010 SPN BL Rez MALDI TOFSergey SidorenkoNo ratings yet
- Curcuma Longa Extract.: ActionDocument2 pagesCurcuma Longa Extract.: ActionDrShiva PrasadNo ratings yet
- AAP Developmental and Behavioral Pediatrics 2nd EditionDocument693 pagesAAP Developmental and Behavioral Pediatrics 2nd Editionrina100% (13)
- Sirshasana: Sirsasana 001 Sirsasana 002 Sirsasana 003 Sirsasana 004Document2 pagesSirshasana: Sirsasana 001 Sirsasana 002 Sirsasana 003 Sirsasana 004Karisma SenapatiNo ratings yet
- TrajectoryDocument29 pagesTrajectoryDithaALkunaNo ratings yet
- Obesity Is A Progressive Problem Among Primary School ChildrenDocument15 pagesObesity Is A Progressive Problem Among Primary School ChildrenHimatul MuhimahNo ratings yet
- Gestational Hypertension and Preeclampsia ACOG Practice Bulletin, Number 222 1605448006Document24 pagesGestational Hypertension and Preeclampsia ACOG Practice Bulletin, Number 222 1605448006xibalba.edNo ratings yet
- NCP Con ConstipationDocument2 pagesNCP Con ConstipationChristine Marie Bucio OraizNo ratings yet
- Another 365 Things That People Believe That Aren't TrueDocument85 pagesAnother 365 Things That People Believe That Aren't TrueMohaideen SubaireNo ratings yet
- 001 210197064 Ci2 117 1Document1 page001 210197064 Ci2 117 1tooba arshadNo ratings yet
- Older AdultsDocument21 pagesOlder AdultsGildred Rada BerjaNo ratings yet