Professional Documents
Culture Documents
NCP - Impaired Skin Integrity
Uploaded by
Flauros Ryu Jabien90%(29)90% found this document useful (29 votes)
82K views3 pagesOriginal Title
Ncp- Impaired Skin Integrity
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
90%(29)90% found this document useful (29 votes)
82K views3 pagesNCP - Impaired Skin Integrity
Uploaded by
Flauros Ryu JabienCopyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
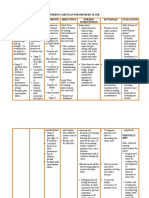
Javier, Jomar A.
BSN121/ Group 83
Far Eastern University
Institute of Nursing
Nursing Care Plan
Nursing Diagnosis/ Analysis Goal & Objectives Nursing Intervention Rationale Evaluation
Cues
Impaired Skin Skin is the Responses to
Integrity primary defense Short Term: Independent: interventions/
r/ t pressure ulcer of the body; it After 6-8 hrs of Assess between folds of Pressure ulcers teaching plans
secondary to protects the nursing skin, remove anti under medical and actions
prolonged immobility body against interventions of embolic stockings or devices are performed.
and unrelieved infections and nursing devices & use a mirror commonly Attainment/pro
pressure diseases interventions, the to see the heels. Also overlooked. gress toward
brought about client will: assess under oxygen desired
Subjective : by the invasion tubing especially on the outcome(s)
The relative of microbes in Have ears & the cheek, Modifications
mentioned the body. A reduced risk of beneath splints and of plan of care.
“nagsusugat yung normal skin is further under medical devices.
may pwetan nya. moist and impairment of Note objective data of Reassessment of
Siguro dahil intact; dryness skin integrity pressure ulcer (stage, ulcer is completed
matagal na siyang of the skin is Patient’s length, width, depth, each time dressing
nakahiga.” more prone to caregivers will wound bed are changed or
friction that may demonstrate appearance, drainage & sooner if ulcer
Objective: result to understanding & condition of periulcer shows
Presence of grade impairment of skill in care of tissue) manifestations of
1 pressure ulcer the skin wound deterioration.
on the lumbar integrity as Analyses of the
area. compared with trends in healing
Disruption of skin a moist skin. Long Term: are important step
surface Pressure on soft After 3-4 days of in assessment.
(epidermis) tissues between nursing
bony interventions, the
prominences client will: Increase the frequency To disperse
↓ of turning (turning q2). pressure over
Compresses Experience Position the client to time or
capillaries & healing of stay off the ulcer. If decreasing the
occludes blood ulcer/regain there is no turning tissue load
flow skin integrity surface without a
↓ (reduce size of pressure ulcer, use a
Pressure not ulcer) pressure redistribution
relieved Reduce risk for bed & continue
↓ infection turning the client
Microthrombi Elevate heels off the Heel covers do not
formation bed by using pillows or relieve pressure,
↓ heel elevation botts. but they can
+ occlusion in reduce friction.
capillaries & Maintain head of bed
blood flow @ the lowest To prevent further
↓ elevation, if client occurrence of
Formation of must have the head pressure ulcer.
blister elevated to prevent
↓ aspiration, reposition
Rupture of to 30 degree lateral
blister position. Use seat
↓ cushions & assess
+ open wound sacral ulcers daily.
Follow body substance To reduce risk of
isolation precautions; infection
use clean gloves &
clean dressing for
wound care.
Practicing proper hand
washing before & after
wound care.
Dependent/Collaborative:
Ensure adequate To prevent
dietary intake. Review malnutrition &
dietician’s delayed healing
recommendations.
Prevent the ulcer To prevent
from being exposed to contamination/spr
urine & feces. Use ead of infection
indwelling catheters,
bowel containment
systems, & topical creams
or dressings.
Supplement the To promote
diet with vitamins & wound healing on
minerals. Vitamins C and clients who do not
zinc are commonly have adequate
prescribed. calories.
Provide oral Pressure ulcers
supplementations, tube- cannot heal in
feedings or clients with severe
hyperalimentation to malnutrition.
achieve positive nitrogen
balance.
Remove devitalized To promote faster
tissue from the wound healing & reduce
bed, except in the infection
avascular tissue or on the
heels. Began by cleansing
the ulcer bed with normal
saline, then use
appropriate technique for
debridement. Once the
ulcer is free of devitalized
tissue, apply dressing the
keep the wound bed
moist & the surrounding
skin dry. Do not use
occlusive dressings on
ulcer.
You might also like
- NCP Impaired SkinDocument2 pagesNCP Impaired Skinarjay2306_obcq100% (1)
- Nursing Care Plan For Pressure UlcerDocument4 pagesNursing Care Plan For Pressure UlcerJobelle Acena67% (3)
- NCP-Impaired Skin IntegrityDocument2 pagesNCP-Impaired Skin IntegrityMikee Ann Valdez96% (26)
- NCP Impaired Skin IntegrityDocument2 pagesNCP Impaired Skin IntegrityEm Gancenia100% (2)
- NCP 2 Impaired Skin IntegrityDocument3 pagesNCP 2 Impaired Skin IntegrityAela Maive MontenegroNo ratings yet
- NCP Impaired Skin IntegrityDocument3 pagesNCP Impaired Skin IntegrityFlauros Ryu Jabien83% (6)
- NCP Impaired Skin IntegrityDocument2 pagesNCP Impaired Skin IntegrityEden Marie Francisco100% (2)
- Impaired Skin Integrity NCPDocument4 pagesImpaired Skin Integrity NCPClint DelacruzNo ratings yet
- NCP-Impaired Skin IntegrityDocument2 pagesNCP-Impaired Skin IntegrityRI NA100% (1)
- NCP: Patient With A Pressure UlcerDocument2 pagesNCP: Patient With A Pressure UlcerICa Marlina100% (1)
- Nursing Care Plan of Pressure UlcersDocument1 pageNursing Care Plan of Pressure UlcersCyrus De Asis46% (13)
- Nursing Care Plan (Impaired Skin Integrity)Document4 pagesNursing Care Plan (Impaired Skin Integrity)arlee marquez91% (161)
- Nursing Care Plan: Cues and Data Nursing Diagnosis Analysis Goal and Objectives Interventions Rationale EvaluationDocument3 pagesNursing Care Plan: Cues and Data Nursing Diagnosis Analysis Goal and Objectives Interventions Rationale EvaluationPaul Cubacub100% (1)
- Impaired Skin IntegrityDocument1 pageImpaired Skin Integritykatvillanueva88% (8)
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegrityJerryson Justo100% (2)
- Betty Impaired Skin IntegrityDocument2 pagesBetty Impaired Skin IntegrityBenjie DimayacyacNo ratings yet
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegrityBesael Baccol100% (1)
- NCP Delayed Wound RecoveryDocument5 pagesNCP Delayed Wound RecoveryDarkCeades100% (2)
- NURSING CARE PLAN On Impaired Skin IntegrityDocument2 pagesNURSING CARE PLAN On Impaired Skin Integrityapi-371817493% (30)
- Nanda 11 Edi. P. 620-621Document3 pagesNanda 11 Edi. P. 620-621Besael Baccol0% (1)
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegrityBesael BaccolNo ratings yet
- Nursing Care Plan Impaired Skin IntegrityDocument1 pageNursing Care Plan Impaired Skin Integrityderic89% (9)
- NCP Impaired Skintissue IntegrityDocument5 pagesNCP Impaired Skintissue IntegrityArt Christian RamosNo ratings yet
- Nursing Care Plan Impaired Skin IntegrityDocument2 pagesNursing Care Plan Impaired Skin Integritycuicuita100% (3)
- Impaired Skin Integrity Related To Surgical Removal of SkinDocument3 pagesImpaired Skin Integrity Related To Surgical Removal of Skinnnaesor_10910% (2)
- Nursing Care PlanDocument3 pagesNursing Care PlanInah Arcellana100% (2)
- NCP: Acute GastroenteritisDocument3 pagesNCP: Acute GastroenteritishauteanicoleNo ratings yet
- NCP Risk For Impaired Skin IntegrityDocument3 pagesNCP Risk For Impaired Skin IntegrityAnne de Vera100% (11)
- Nursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesNursing Care Plan Assessment Nursing Diagnosis Inference Planning Intervention Rationale Evaluation SubjectiveGaurav Gaikwad100% (3)
- NCP Impaired Skin IntegrityDocument2 pagesNCP Impaired Skin IntegrityLiza Marie Cayetano Adarne93% (14)
- Acute Pain NCPDocument1 pageAcute Pain NCPRyan PanNo ratings yet
- Nursing Care Plan Risk For Impaired Skin IntegrityDocument3 pagesNursing Care Plan Risk For Impaired Skin IntegrityCrystal Joy Misa100% (1)
- POSTOP - Impaired Skin Integrity (Latest)Document3 pagesPOSTOP - Impaired Skin Integrity (Latest)michelle_celeste100% (2)
- NCP Epidural HemDocument32 pagesNCP Epidural HemKatrina PonceNo ratings yet
- XIII. NCP Risk For FallsDocument1 pageXIII. NCP Risk For FallsMartin T Manuel100% (2)
- NCP - Impaired Tissue IntegrityDocument3 pagesNCP - Impaired Tissue IntegrityRene John FranciscoNo ratings yet
- NCP - Risk For Impaired Skin Integrity R/T Dry Skin and Behaviors That May Lead To Skin Integrity Impairment AEB Scratching of ScabsDocument1 pageNCP - Risk For Impaired Skin Integrity R/T Dry Skin and Behaviors That May Lead To Skin Integrity Impairment AEB Scratching of ScabsCarl Elexer Cuyugan Ano100% (4)
- NCP - Impaired Skin IntegrityDocument1 pageNCP - Impaired Skin Integrityjanelee28240% (2)
- NCP Impaired Physical MobilityDocument2 pagesNCP Impaired Physical MobilityKristine Young0% (1)
- NCP3 Skin IntegrityDocument3 pagesNCP3 Skin IntegritySheng Arquiza67% (3)
- Impaired Skin IntegrityDocument4 pagesImpaired Skin IntegrityVianah Eve EscobidoNo ratings yet
- (NCPS) Impaired Physical Mobility 2Document2 pages(NCPS) Impaired Physical Mobility 2roren100% (1)
- NCP-Risk For FallsDocument2 pagesNCP-Risk For FallsGregg Palabrica100% (4)
- Cebu Institute of Technology - University College of NursingDocument2 pagesCebu Institute of Technology - University College of NursingSergi Lee OrateNo ratings yet
- NCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)Document2 pagesNCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)yanny0350% (2)
- Nursing Care Plan Final Draft Bullingerballow Julie MDocument8 pagesNursing Care Plan Final Draft Bullingerballow Julie Mapi-545881335No ratings yet
- Nursing Diagnosis Background Study Inference Goals and Objectives Interventions Rationale EvaluationDocument5 pagesNursing Diagnosis Background Study Inference Goals and Objectives Interventions Rationale EvaluationAubrey SungaNo ratings yet
- Diabetes Mellitus: Assessment Diagnosis Planning Intervention Rationale EvaluationDocument12 pagesDiabetes Mellitus: Assessment Diagnosis Planning Intervention Rationale EvaluationDerick RanaNo ratings yet
- 3 Pressure Ulcer (Bedsores) Nursing Care Plans - NurseslabsDocument12 pages3 Pressure Ulcer (Bedsores) Nursing Care Plans - NurseslabsJOSHUA DICHOSONo ratings yet
- Nursing Care Plan For Cesarean SectionDocument5 pagesNursing Care Plan For Cesarean SectionJon Gab Paquit85% (33)
- Impaired Skin DMDocument3 pagesImpaired Skin DMimnotdatsunny100% (1)
- Short Term: Independent:: 7 CM, Stage IV Pressure Ulcer in The SacrumDocument2 pagesShort Term: Independent:: 7 CM, Stage IV Pressure Ulcer in The Sacrumaaron tabernaNo ratings yet
- NCP Imapired Skin IntegrityDocument5 pagesNCP Imapired Skin IntegrityAno BaItoNo ratings yet
- NCP Impaired Skin IntergrityDocument2 pagesNCP Impaired Skin IntergrityDianna RoseNo ratings yet
- Nursing Care Plan Cues Nursing Diagnosis Analysis Goal Intervention Rationale Evaluatio NDocument3 pagesNursing Care Plan Cues Nursing Diagnosis Analysis Goal Intervention Rationale Evaluatio NAishleen OrmandoNo ratings yet
- Nursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term GoalsDocument3 pagesNursing Care Plan (NCP) : Date and Time Nursing Diagnosis Short - Term and Long - Term GoalsdanicaNo ratings yet
- Apalisok NCPDocument3 pagesApalisok NCPApalisok GerardNo ratings yet
- College of Nursing and Allied Medical Sciences: WesleyanDocument3 pagesCollege of Nursing and Allied Medical Sciences: WesleyanCharie OcampoNo ratings yet
- 1 ST NCPDocument3 pages1 ST NCPHazel BandayNo ratings yet
- NCP Bed SoresDocument3 pagesNCP Bed SoresShe CalliNo ratings yet
- Pa Tho Physiology of TuberculosisDocument3 pagesPa Tho Physiology of TuberculosisFlauros Ryu JabienNo ratings yet
- Pathophysiology of TuberculosisDocument3 pagesPathophysiology of TuberculosisFirenze Fil96% (56)
- Organise Meetings (Answers)Document16 pagesOrganise Meetings (Answers)Flauros Ryu Jabien100% (1)
- NCP Acute PainDocument3 pagesNCP Acute PainIsrael Soria EsperoNo ratings yet
- Nursing Care Plan (Readiness of Enhanced Therapeutic Management)Document2 pagesNursing Care Plan (Readiness of Enhanced Therapeutic Management)Flauros Ryu Jabien77% (26)
- Problem PrioritizationDocument1 pageProblem PrioritizationFlauros Ryu JabienNo ratings yet
- NCP Impaired Skin IntegrityDocument3 pagesNCP Impaired Skin IntegrityFlauros Ryu Jabien83% (6)
- Drug TramadolDocument2 pagesDrug TramadolFlauros Ryu Jabien100% (2)
- Drug Study (Aspirin, in Enalapril Maleate, Tramadol, AmlodipineDocument10 pagesDrug Study (Aspirin, in Enalapril Maleate, Tramadol, AmlodipineFlauros Ryu Jabien100% (1)
- NCP PainDocument4 pagesNCP PainFlauros Ryu JabienNo ratings yet
- Drug Study PantoprazoleDocument2 pagesDrug Study PantoprazoleFlauros Ryu Jabien100% (3)
- NCP ReadinessDocument2 pagesNCP ReadinessFlauros Ryu Jabien100% (3)
- Nursing Care Plan (Readiness of Enhanced Therapeutic Management)Document2 pagesNursing Care Plan (Readiness of Enhanced Therapeutic Management)Flauros Ryu Jabien100% (2)
- Drug Study (Aspirin, in Enalapril Maleate)Document13 pagesDrug Study (Aspirin, in Enalapril Maleate)Flauros Ryu Jabien50% (2)
- Drug Study (Ospital NG Sampaloc)Document4 pagesDrug Study (Ospital NG Sampaloc)Flauros Ryu JabienNo ratings yet
- Nurses Bill of RightsDocument1 pageNurses Bill of RightsFlauros Ryu Jabien100% (1)
- NCP Pediatric (Diarrhea and Impaired Mucous Membrane)Document8 pagesNCP Pediatric (Diarrhea and Impaired Mucous Membrane)Flauros Ryu Jabien60% (5)
- OsteoarthritisDocument60 pagesOsteoarthritisFlauros Ryu JabienNo ratings yet
- TramadolDocument7 pagesTramadolFlauros Ryu JabienNo ratings yet
- NCP (Hyperthermia)Document3 pagesNCP (Hyperthermia)Flauros Ryu Jabien100% (1)
- NCP (Case Pres)Document1 pageNCP (Case Pres)Flauros Ryu JabienNo ratings yet
- Pathophysiology HemothoraxDocument1 pagePathophysiology HemothoraxFlauros Ryu Jabien50% (4)
- Problem PrioritizationDocument2 pagesProblem PrioritizationFlauros Ryu Jabien100% (3)
- CCHU9005 Food and Values L3 - Eating Meat: Joe Y. F. Lau Department of Philosophy 2021Document29 pagesCCHU9005 Food and Values L3 - Eating Meat: Joe Y. F. Lau Department of Philosophy 2021Pakhin LaiNo ratings yet
- Idaho Cacfp Menu Toolkit FinalDocument144 pagesIdaho Cacfp Menu Toolkit FinalFernanda TorresNo ratings yet
- Chapter 14. The Digestive SystemDocument27 pagesChapter 14. The Digestive SystemScianna Christel LastimosaNo ratings yet
- Journal Pre-Proof: Metabolism OpenDocument59 pagesJournal Pre-Proof: Metabolism OpenJhon AsencioNo ratings yet
- CarbohydratesDocument14 pagesCarbohydratesPauline AnneNo ratings yet
- Passages FactualDocument14 pagesPassages FactualAnusha MNo ratings yet
- Fiwe Extractor de Fibra PDFDocument1 pageFiwe Extractor de Fibra PDFTrajano CepedaNo ratings yet
- Obesity Project 2021Document16 pagesObesity Project 2021JIESSNU A/L ANBARASU MoeNo ratings yet
- Manufacturing Sports Nutrition and Supplements - FinalDocument21 pagesManufacturing Sports Nutrition and Supplements - Finalrajneesh kumarNo ratings yet
- TLE GRADE 9 Handout 1 (SECOND QUARTER)Document4 pagesTLE GRADE 9 Handout 1 (SECOND QUARTER)cherry ann cruceroNo ratings yet
- Benefits of BreastfeedingDocument2 pagesBenefits of BreastfeedingESPINOSA JHANNANo ratings yet
- Famacion - CHN Survey ToolDocument14 pagesFamacion - CHN Survey ToolKyra Bianca R. Famacion100% (1)
- Weight Management Herbalife Nutrition - Australia & New ZealandDocument1 pageWeight Management Herbalife Nutrition - Australia & New ZealandNepali ThitoNo ratings yet
- Vem12 - GoatsDocument104 pagesVem12 - Goatsjayr ludoviceNo ratings yet
- DapusDocument11 pagesDapusOrindia SuarminNo ratings yet
- NST Supported by Original Data (Age)Document18 pagesNST Supported by Original Data (Age)Rika LedyNo ratings yet
- Journal Pre-Proof: Clinical Epidemiology and Global HealthDocument22 pagesJournal Pre-Proof: Clinical Epidemiology and Global HealthClaudia BuheliNo ratings yet
- Exploration: 5.1.5 Explore: Fighting Free RadicalsDocument5 pagesExploration: 5.1.5 Explore: Fighting Free RadicalsSid Mathur100% (1)
- Food AdulterationDocument39 pagesFood AdulterationAlizaNo ratings yet
- Test Bank For Nutrition and You 2nd Edition by BlakeDocument16 pagesTest Bank For Nutrition and You 2nd Edition by Blakeoraliehue5z05pyNo ratings yet
- Nutrition in Animals Class 7 WsDocument2 pagesNutrition in Animals Class 7 WsShweta RathiNo ratings yet
- Lista Precios FlowDocument1 pageLista Precios FlowGabrielNo ratings yet
- Discharge Plan - Dinson, Red Angela O. BSN 1-BDocument2 pagesDischarge Plan - Dinson, Red Angela O. BSN 1-BRed Angela DinsonNo ratings yet
- Comprehension SPM 20210304Document2 pagesComprehension SPM 20210304Rachel LeeNo ratings yet
- Tomato PowderDocument38 pagesTomato PowderMa Cristina Del MoroNo ratings yet
- (Sep 22) FNSD Manual - 1st DraftDocument232 pages(Sep 22) FNSD Manual - 1st DraftAbraham EshetuNo ratings yet
- Cargill 2020 Annual Report PDFDocument7 pagesCargill 2020 Annual Report PDFEva Natalia SiraitNo ratings yet
- 5 Ways To Turn Any Treat Into A Delicious Healthy RecipeDocument22 pages5 Ways To Turn Any Treat Into A Delicious Healthy Recipealex_grgNo ratings yet
- 50 Hi NucleusDocument2 pages50 Hi NucleusJohnNo ratings yet
- Secrets From The Restaurant - 25 Delicious Recipesrets Behind Your Favorite Meals! - Nancy SilvermanDocument55 pagesSecrets From The Restaurant - 25 Delicious Recipesrets Behind Your Favorite Meals! - Nancy Silvermanscribd2No ratings yet