Professional Documents
Culture Documents
n320 Peds NCP wk4
Uploaded by
api-301826049Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
n320 Peds NCP wk4
Uploaded by
api-301826049Copyright:
Available Formats
Kapiolani Community College
Associate Degree Nursing Program
Nurs320 Nursing Care Plan
Student Name Bradley Keown
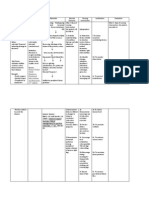
Nursing Diagnosis: Risk for activity intolerance.
Date of Care: 12/03/15
Date Submitted: 12/07/15
Related to: Anemia induced by chemotherapy.
As manifested by: Post chemotherapy CBC w/ HgB: 7.8 and Hct: 22.4%; periods of rest after minor exertion.
Scientific Rationale: AML causes there to be less room for RBCs to be produced. After being treated with chemotherapy, total production of blood cells are
severely lowered as well as decreasing appetite which leads to decreased nutrient intake to make cells. Due to the lack of circulating red blood cells in her
system, there is an increased risk of oxygen and nutrients not being properly transported, leading to a decrease in function and stability.
Reference: http://www.cancer.gov/about-cancer/treatment/side-effects/fatigue/fatigue-pdq
Outcomes (measurable)
Short Term
No reports of any fatigue and/or
weakness.
Interventions
1. Assess for the signs and symptoms
of activity intolerance (reports of
fatigue/weakness, exertional
dyspnea, chest pain, diaphoresis or
dizziness).
2. Assess patients level of mobility.
3. Assess vital signs.
4. Perform actions to promote rest
and/or conserve energy (minimize
environment activity and noise,
cluster care, keep personal articles
within reach, reduce fear and
anxiety, promote rest).
5. Perform actions to reduce cardiac
workload and maintain adequate
cardiac reserve (place client in
semi- to high Fowlers, instruct
client to avoid Valsalva response,
promote deep breathing,
discourage caffeine).
6. Assess/Promote adequate
nutritional intake.
7. Instruct client to report decreased
activity or s/s of activity intolerance.
Rationale
1. These signs and symptoms can be
indications of a worsening in
condition.
2. Obtaining a baseline for patients
capability is essential for noting
alterations.
3. Abnormal heartrate, respiratory rate
or blood pressure can indicate
change in condition.
4. Increased rest and conservation of
energy can help prevent
development of fatigue.
5. Increased cardiac workload can
further lead to fatigue and
weakness.
6. Adequate nutrition is required to
create energy and for proper
function of all body parts.
7. Changes in activity tolerance can
indicate a worsening in condition.
Evaluation
1. Patient reported no
fatigue/weakness. No overt s/s
other than pt laying down after
ambulation to and from play room
(sat in playroom to make doll
dresses).
2. Pt is reported by previous nurses to
be very energetic with no limitations
in mobility.
3. Patients vital signs remained within
normal limits. 1220 HR: 92, RR: 20,
BP: 100/62.
4. Clustered care around 0815 and
1220, kept lights low and kept
patients frequently used items near
bedside. Patient displayed ability to
provide self-care and ambulation
w/o issue.
5. Kept patient in semi- Fowlers or
upright, informed patient not to
strain herself and promoted fluids
that were non-caffeinated
(Grandmother verbalized
understanding).
6. Patient was informed, but was a
pecky eater. 25% of breakfast was
eaten and 50% of lunch after
obtaining ranch. Informed nurse,
she reported that low percentages is
normal for pt and that she makes up
for it by snacking throughout the
day.
7. Informed patient and patients care
provider (grandmother) to monitor
for s/s of activity intolerance. Both
reported understanding
Long Term
Pt will continue to be able to
perform activities of daily living
without exertional dyspnea, chest
pain, diaphoresis, dizziness,
and/or change in vital signs.
Reference: http://www1.us.elsevierhealth.com/SIMON/Ulrich/Constructor/diagnoses.cfm?did=35 (8th ed.). Philadelphia, PA: Elsevier.
You might also like
- Nursing Care Plan Ineffective Peripheral Tissue PerfusionDocument3 pagesNursing Care Plan Ineffective Peripheral Tissue PerfusionRosalie Delfin90% (10)
- 5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care PlansDocument3 pages5 Altered Nutrition Less Than Body Requirements Chronic Renal Failure Nursing Care Plansjustin_sane40% (5)
- Cva NCPDocument1 pageCva NCPxiang jinNo ratings yet
- Siegelman Online Advantage 1.1 PDFDocument39 pagesSiegelman Online Advantage 1.1 PDFDana Ysabelle Ibarra100% (1)
- DM NCPDocument7 pagesDM NCPMichael Anthony Cardenas Macaballug67% (3)
- PACES 21 - Communication Skills and EthicsDocument10 pagesPACES 21 - Communication Skills and EthicsDrShamshad Khan100% (1)
- NCP Ineffective Tissue Perfusion and Self Care DeficitDocument5 pagesNCP Ineffective Tissue Perfusion and Self Care DeficitFrances Anne Pasiliao100% (3)
- Student Case Study Example Template Free Download PDFDocument14 pagesStudent Case Study Example Template Free Download PDFNana YaaNo ratings yet
- NCPs For Diabetes MellitusDocument6 pagesNCPs For Diabetes MellitusEjie Boy Isaga100% (1)
- CHF Concept MapDocument4 pagesCHF Concept MapLisaSanders99No ratings yet
- Activity Intolerance NCPDocument7 pagesActivity Intolerance NCPMariquita BuenafeNo ratings yet
- Drug StudyDocument7 pagesDrug StudyKim GalamgamNo ratings yet
- Advanced Clinical Therapies in Cardiovascular Chinese MedicineFrom EverandAdvanced Clinical Therapies in Cardiovascular Chinese MedicineNo ratings yet
- World Class Technology.: Results That Make A DifferenceDocument2 pagesWorld Class Technology.: Results That Make A DifferenceAndre ZeaNo ratings yet
- Activity 3.1.2 Rapid Pathogen IdentificationDocument8 pagesActivity 3.1.2 Rapid Pathogen Identificationsahsdjkh7No ratings yet
- NCP For Imbalanced NutritionDocument6 pagesNCP For Imbalanced NutritionMelvin MartinezNo ratings yet
- Bev NCP TodayDocument13 pagesBev NCP TodayBeverlyNo ratings yet
- CVA NCPDocument6 pagesCVA NCPErika Arboleras0% (1)
- NCP CHFDocument10 pagesNCP CHFMykel Jake VasquezNo ratings yet
- Diagnosa Baru EinDocument2 pagesDiagnosa Baru EinthethayNo ratings yet
- Heath Day 4 Care Plan 3Document12 pagesHeath Day 4 Care Plan 3api-639508852No ratings yet
- 1Document7 pages1YolieEspejo100% (2)
- HEMATOLOGICAL CONDITIONS Answers Theory 2Document14 pagesHEMATOLOGICAL CONDITIONS Answers Theory 2CJ RelleveNo ratings yet
- NCPDocument3 pagesNCPKrizelle Abadesco Libo-on50% (2)
- NCPDocument22 pagesNCPMaricris S. Sampang100% (1)
- NCP (Fatigue)Document1 pageNCP (Fatigue)student_019100% (1)
- Ru For CVD BleesDocument30 pagesRu For CVD BleesKaye LeNo ratings yet
- Student Case Study Example TemplateDocument14 pagesStudent Case Study Example Templateapi-376910880No ratings yet
- Select All That Apply SATADocument67 pagesSelect All That Apply SATAHermie Joy Maglaqui100% (1)
- Tif30Document49 pagesTif30HCX dghhqNo ratings yet
- Decreased Cardiac OutputDocument4 pagesDecreased Cardiac OutputAdnan Khan100% (1)
- Acute Respiratory Distress SyndromeDocument4 pagesAcute Respiratory Distress SyndromeBianca WelchNo ratings yet
- Cervical Cancer ChemotherapyDocument6 pagesCervical Cancer ChemotherapyTheeya Quigao0% (1)
- Nursing Care Plan: Blood ChemDocument5 pagesNursing Care Plan: Blood ChemMary Gold EleveraNo ratings yet
- NCPDocument10 pagesNCPannamargie07No ratings yet
- DIABETES Nursing ManagementDocument11 pagesDIABETES Nursing ManagementKaloy KamaoNo ratings yet
- Pat2 Med Surg 2Document19 pagesPat2 Med Surg 2api-339132978No ratings yet
- DischargeDocument49 pagesDischargejonel_amarilleNo ratings yet
- Mary Cris Canon CHF For or Case Study.Document12 pagesMary Cris Canon CHF For or Case Study.Mary Cris CanonNo ratings yet
- Nursing Care PlanDocument22 pagesNursing Care Planaln00550% (2)
- NCP DMDocument21 pagesNCP DMKate ManalastasNo ratings yet
- Anemia CareplanDocument14 pagesAnemia Careplanbenardnyakundi99No ratings yet
- Case Presentation of AnemiaDocument71 pagesCase Presentation of AnemiaJessica Esther Canlas100% (2)
- Medical Surgical Nursing Care 4th Edition Burke Test BankDocument19 pagesMedical Surgical Nursing Care 4th Edition Burke Test Banksophiechaurfqnz100% (32)
- Dr. Vinod K. Ravaliya, MPT Cardiothoracic Physiotherapy Shree Krishna Hospital KMPIP, KaramsadDocument54 pagesDr. Vinod K. Ravaliya, MPT Cardiothoracic Physiotherapy Shree Krishna Hospital KMPIP, KaramsadShubha DiwakarNo ratings yet
- Care Plan 1 240Document16 pagesCare Plan 1 240api-314575117No ratings yet
- Cardiac-Vascular Nursing Exam Sample Questions: Increased Central Venous PressureDocument5 pagesCardiac-Vascular Nursing Exam Sample Questions: Increased Central Venous PressureMelodia Turqueza GandezaNo ratings yet
- Cardiac-Vascular Nursing Exam Sample Questions: Increased Central Venous PressureDocument5 pagesCardiac-Vascular Nursing Exam Sample Questions: Increased Central Venous PressureMelodia Turqueza GandezaNo ratings yet
- Clinical Pearls CardiologyDocument6 pagesClinical Pearls CardiologyMaritza24No ratings yet
- I Am Sharing 'Case Study NCM 118' With YouDocument6 pagesI Am Sharing 'Case Study NCM 118' With YouQusai BassamNo ratings yet
- NCMB316 Rle 2-10-7addison's DiseaseDocument4 pagesNCMB316 Rle 2-10-7addison's DiseaseMaica LectanaNo ratings yet
- PRIORITIZATION-NCP Acute Myelogenous LeukemiaDocument2 pagesPRIORITIZATION-NCP Acute Myelogenous LeukemiaAllan Macacapagal50% (2)
- Nutrition in The Critically Ill PatientDocument13 pagesNutrition in The Critically Ill PatientnainazahraNo ratings yet
- Chapter 15Document27 pagesChapter 15Jessica nonyeNo ratings yet
- NCPGDMDocument8 pagesNCPGDMChristopher LontocNo ratings yet
- Group e Polycythemia Verapinakafinal 2Document75 pagesGroup e Polycythemia Verapinakafinal 2deserieroseonateNo ratings yet
- Edukasi Pasien JantungDocument17 pagesEdukasi Pasien JantungAqshaTiaraViazeldaNo ratings yet
- (Osborn) Chapter 42: Learning Outcomes (Number and Title)Document28 pages(Osborn) Chapter 42: Learning Outcomes (Number and Title)KittiesNo ratings yet
- Siegelman Online Advantage 1.2Document40 pagesSiegelman Online Advantage 1.2Samantha AgustinNo ratings yet
- HyperkalemiaDocument17 pagesHyperkalemiaKrishna VidhuriNo ratings yet
- Addressing Myths About Exercise in Hemodialysis PatientsDocument6 pagesAddressing Myths About Exercise in Hemodialysis PatientsjoseNo ratings yet
- Case Pres 2ndrotDocument11 pagesCase Pres 2ndrotJoseph Emmanuel CandaNo ratings yet
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionFrom EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionNo ratings yet
- n320 Keownb CulturalDocument4 pagesn320 Keownb Culturalapi-301826049No ratings yet
- n320 Peds NCP wk3Document2 pagesn320 Peds NCP wk3api-301826049No ratings yet
- SynopsisDocument3 pagesSynopsisapi-301826049No ratings yet
- 360 Keownb LeadershipstyleDocument2 pages360 Keownb Leadershipstyleapi-301826049No ratings yet
- Med-Surg Keownb Journal wk2Document2 pagesMed-Surg Keownb Journal wk2api-301826049No ratings yet
- Med-Surg Keownb Journal wk1Document2 pagesMed-Surg Keownb Journal wk1api-301826049No ratings yet
- Reference Letter For BradDocument1 pageReference Letter For Bradapi-301826049No ratings yet
- Keownb 362 PDPDocument1 pageKeownb 362 PDPapi-301826049No ratings yet
- Dandruff and HomoeopathyDocument4 pagesDandruff and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- Group Case Study - Pulmonary TBDocument8 pagesGroup Case Study - Pulmonary TBCj NiñalNo ratings yet
- Sensus Harian TGL 05 Maret 2022........Document104 pagesSensus Harian TGL 05 Maret 2022........Ruhut Putra SinuratNo ratings yet
- School of Law, Galgotias University: Moot PropostionDocument3 pagesSchool of Law, Galgotias University: Moot PropostionwalterNo ratings yet
- Blood PressureDocument11 pagesBlood PressureHilma NadzifaNo ratings yet
- Drug Study-Ceftriaxone ClindamycinDocument2 pagesDrug Study-Ceftriaxone ClindamycinDavid VillanuevaNo ratings yet
- Tomografia UrotacDocument12 pagesTomografia Urotacnoeg_909929No ratings yet
- Great Atlas of Dermatology IndexedDocument73 pagesGreat Atlas of Dermatology Indexedjohn pauloNo ratings yet
- Perioperative Nursing 50 ItemsDocument4 pagesPerioperative Nursing 50 Itemssan maeNo ratings yet
- ?KPSC Assistant Dental Surgeon Exam 2021Document39 pages?KPSC Assistant Dental Surgeon Exam 2021Tejas KulkarniNo ratings yet
- Document 85Document51 pagesDocument 85Shameena AnwarNo ratings yet
- Https Learn - Cellsignal.com Hubfs Pdfs 21-Bpa-35731-Therapeutics-brochure-digitalDocument12 pagesHttps Learn - Cellsignal.com Hubfs Pdfs 21-Bpa-35731-Therapeutics-brochure-digitalashuwillusinfraNo ratings yet
- Kristjansson 2009Document14 pagesKristjansson 2009AdosotoNo ratings yet
- Fecal Calprotectin in IBDDocument34 pagesFecal Calprotectin in IBDNathania Nadia Budiman100% (1)
- Comparison of Hemorrhoid Sclerotherapy Using Glucose 50% vs. Phenol in Olive OilDocument4 pagesComparison of Hemorrhoid Sclerotherapy Using Glucose 50% vs. Phenol in Olive OilGabrielEnricoPangarianNo ratings yet
- The Study of Drug Resistance in Bacteria Using Antibiotics: June 2019Document6 pagesThe Study of Drug Resistance in Bacteria Using Antibiotics: June 20197'A'06Aditya BeheraNo ratings yet
- Berry White - Delta 8 THC Vape CartridgeDocument5 pagesBerry White - Delta 8 THC Vape CartridgeGodl JonathanNo ratings yet
- Obstetric ExaminationDocument4 pagesObstetric ExaminationSusan GeorgeNo ratings yet
- CV For FellowshipDocument3 pagesCV For Fellowshipapi-568710214No ratings yet
- Effect of Nonsurgical Periodontal Therapy. I. Moderately Advanced Periodontitis. Badersten A, Nilvéus R, Egelberg J. J Clin Periodontol. 1981 Feb8 (1) 57 72 PDFDocument17 pagesEffect of Nonsurgical Periodontal Therapy. I. Moderately Advanced Periodontitis. Badersten A, Nilvéus R, Egelberg J. J Clin Periodontol. 1981 Feb8 (1) 57 72 PDFMashal AmirNo ratings yet
- Pharmacy Journals 100Document7 pagesPharmacy Journals 100alexpharmNo ratings yet
- Pediatrics MCQs - DR Ranjan Singh - Part 2Document10 pagesPediatrics MCQs - DR Ranjan Singh - Part 2k sagarNo ratings yet
- NUR-116 Exam Sample-1Document4 pagesNUR-116 Exam Sample-1peternady202No ratings yet
- DT311 TPS Bahasa Inggris - Ani - CBT - Paket 1Document4 pagesDT311 TPS Bahasa Inggris - Ani - CBT - Paket 1Eki BBNo ratings yet
- Inistitutional Assessementknowledge Test For Comprhenssive NursingDocument19 pagesInistitutional Assessementknowledge Test For Comprhenssive NursingkassahunNo ratings yet
- Multiple MyelomaDocument2 pagesMultiple MyelomaKolin JandocNo ratings yet
- Microbiology - Exercise 3e AntibiogramDocument5 pagesMicrobiology - Exercise 3e Antibiogramapi-253346521No ratings yet