Professional Documents
Culture Documents
Originalneutropolicy
Uploaded by
api-2550842530 ratings0% found this document useful (0 votes)
64 views9 pagesOriginal Title
originalneutropolicy
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
64 views9 pagesOriginalneutropolicy
Uploaded by
api-255084253Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 9
c301911 Page 1 of 9
University of Colorado Hospital Policy and Procedure
Neutropenia Management for Oncology and Hematopoietic Stem Cell
Transplant Patients
Related Policies and Procedures:
Standard Precautions
Hand Hygiene-Outside the Surgical Setting
Hospital Infection Control
Isolation/Transmission Based Precautions
Blood/Body Fluid Spills
Aseptic Technique in Invasive and Operative Procedures
Clean/Sterile Supply Storage in Clinical Areas
Infectious/Regulated Waste Management
Employee Work Restrictions for Infectious Diseases
Live Plant and Flower Restrictions
Diet Restrictions and Recommendations for the Hematology and Oncology
Immunocompromised Patient
Central Venous Lines
Animal Assisted Activities/Therapy Program
Approved by: Professional Practice, Policy and Procedure Committee
Effective: 10/07
Reviewed: 9/11
Description: This policy defines Neutropenia, as well as febrile neutropenia, and the
necessary assessment parameters, guidelines, interventions, and environmental modification that
must be implemented by University of Colorado Hospital health care providers in UCH clinical
settings when caring for neutropenic patients.
Accountability: All University of Colorado Hospital employees, physicians, volunteers,
students, temporary and contract employees are responsible for complying with the
precautions/measures described in this policy/procedure. Visitors and other non-hospital-
employee personnel will be informed of and asked to comply with the provisions of this policy
by the University of Colorado Hospital staff. Non-compliance will be dealt with on an
individual basis.
Definitions:
Neutrophils are the bodys first line of defense against microbial invasion. They constitute
approximately 40%-60% of the total white blood cell count that usually ranges from 4,000-
10,000/mm
3
.
Neutropenia is defined as an absolute neutrophil count (ANC) less than 500/mm
3
.
1. The relative risk for infection increases as the ANC decreases. The ANC is categorized into
grades, which reflect the risk for infection.
a. Grade 1: ANC 1500-2000/mm
3
= No Significant Risk
b. Grade 2: ANC 1000-1500/mm
3
=Slight Increase in Risk
Neutropenia Management for Oncology and Hematopoietic Stem Cell
Transplant Patients
c301911 Page 2 of 9
c. Grade 3: ANC 500-1000/mm
3
=Moderate Risk=Neutropenia
d. Grade 4: ANC less than 500/mm
3
=High Risk=Neutropenia
Signs and Symptoms of Infection
1. Localized symptoms of infection: pain at the site of infection that may or may not include
erythema or exudate.
2. Generalized symptoms of infection: chills, myalgias, arthralgias, cognitive or mental status
changes, anorexia, nausea/vomiting, fatigue, tachycardia, hypotension, tachypnea,
hypoxemia, and oliguria.
3. Site-Specific symptomatology: cough, dyspnea, abnormal breath sounds oral pain, back
pain, rectal discomfort with bowel elimination, pain at vascular access device site,
burning/urgency with urination.
Sources of Infection
1. The skin and mucous membranes are vulnerable sources of microbial invasion due to
IV/Central line access and mucositis. For patients undergoing HSCT (Hematopoietic Stem
Cell Transplant), additional risk factors include GVHD (Graft versus Host Disease), and
toxicities from conditioning regimens that cause prolonged neutropenia (10-30 days).
2. Primary sites of infection in the neutropenic patient are the digestive tract (mouth, pharynx,
esophagus, large and small bowel, rectum), as well as the sinuses, lungs, and skin.
3. Hand hygiene is considered the most important procedure to prevent the spread of infections.
Refer UCH Policy and Procedure: Hand Hygiene-Outside The Surgical Setting.
Table of Contents:
I. Assessment Parameters
II. Nursing Intervention for Treatment of Febrile Neutropenia
III. Neutropenic Precautions Sign, Appendix A
IV. ED Approach to Patient with Possible Neutropenic Fever, Appendix B
Policy/Procedure:
Policy
The frequency and severity of infection are inversely proportional to the Absolute Neutrophil
Count; the risks of severe infection and bloodstream infection are greatest when the neutrophil
count is less than 100/mm
3
. Most patients with solid tumors have neutropenia lasting 7-10 days
and are at much lower risk for infection. For patients undergoing HSCT, neutropenia can last
from 10-30 days which is consistent with the therapeutic goal of destroying malignant cells
within the bone marrow; therefore, the intent of treatment is grade 4 neutropenia. After the
neutrophil count recovers, humoral and cellular immune dysfunction may persist, maintaining
susceptibility to infection for months. Approximately 48% to 60% of neutropenic patients who
are febrile have an established or occult infection. Approximately 10-20% of patients with a
neutrophil count less than 100/mm
3
will develop a bloodstream infection. Ineffective
management of febrile neutropenia can result in delayed treatment potentially resulting in sepsis,
septic shock, and poorer patient outcomes. Proactive management of neutropenia is critical to
decreasing the depth and duration of neutropenia following HSCT, limiting exposure to
opportunistic and nosocomial pathogens, and ensuring prompt intervention should febrile
neutropenia or infection develop.
Neutropenia Management for Oncology and Hematopoietic Stem Cell
Transplant Patients
c301911 Page 3 of 9
Procedure
I. Assessment Parameters
A. Fever (oral temperature greater than or equal to 38.3 degrees Celsius) is usually the
first sign of a potentially life-threatening infection. Localized symptoms of infection
such as redness, swelling, pain, and exudate may not be present due to the inability
of the patients body to create an inflammatory response due to the absence or
decreased number of neutrophils.
1. Although uncommon, a patient with neutropenia and signs or symptoms of
infection (i.e. abdominal pain, severe mucositis, perirectal pain) without fever,
should be considered to have an active infection.
B. Assessment Guidelines
1. Determine expected duration and severity of neutropenia
a. Consider the patients current and past treatment regimens including one or
more of the following: chemotherapy, radiation therapy, immunotherapy,
immunosuppressive therapy, HSCT.
b. Consider the patients comorbitities, medications, history of prior documented
infections, recent antibiotic therapy, exposure to infections from household
members, pets, travel (including Tuberculosis exposure), HIV status, and
recent blood product administration.
2. Assess for common sites of infection in patients with fever and neutropenia: the
alimentary tract, groin, skin, lungs, sinus, ears, perivagina, perirectum, and
vascular access device sites
3. Monitor vital signs (T,P,R,BP) Q4h
4. Monitor Intake and Output Q8h (Q4h for active transplant patients)
5. Monitor laboratory data:
a. CBC with differential, including WBC count. If ANC less than 1000, institute
neutropenic precautions. Refer to Neutropenic Precautions sign (Appendix
A).
b. Comprehensive Metabolic Panel, LDH, Uric Acid, Creatinine, BUN, LFTs,
Total Serum Bilirubin.
c. Blood and other Culture Reports-notify Physician/Nurse Practitioner if
positive and institute appropriate transmission based precautions if necessary.
Refer to UCH Policy and Procedure: Isolation/Transmission Based
Precautions.
II. Nursing Intervention For Treatment of Febrile Neutropenia
A. Febrile Neutropenia
1. HSCT patients
a. Patients admitted for HSCT are treated with prophylactic antibiotics prior to
becoming neutropenic and throughout the expected neutropenic state during
hospitalization. Once patients receive their stem cells, they begin G-CSF
therapy to assist in WBC recovery. Refer to pre-printed orders for details.
Neutropenia Management for Oncology and Hematopoietic Stem Cell
Transplant Patients
c301911 Page 4 of 9
b. When a patient becomes febrile (oral temperature greater than or equal
to 38.3 degrees Celsius), refer to pre-printed orders, which indicate obtaining
a chest x-ray, urine culture and sensitivity, and two sets of blood cultures. At
least one of the two sets of cultures is to be obtained from the patients
vascular access device if present.
1. Collaborate with Physician/Nurse Practitioner regarding obtaining one of
the two sets of blood cultures peripherally.
c. According to the 2007 NCCN guidelines, if there is entry or exit site
inflammation around the vascular access device, a set of cultures is to be
obtained from each lumen and Vancomycin should be started or added to the
existing empiric therapy. If the vascular access device cultures are positive
for infection, collaborate with Physician/Nurse Practitioner regarding
obtaining further blood cultures from each lumen, removal of vascular access
device, and additional antibiotic therapy.
d. If patient symptomatology warrants, collaborate with Physician/Nurse
Practitioner regarding obtaining site specific cultures including rectal, stool,
skin, mouth, throat, sputum, and nasopharynx.
e. If patient continues to be febrile, blood cultures, urine culture and sensitivity,
and chest x-ray are to be done only once every 24 hours.
f. Refer to pre-printed orders for fever day antibiotic instructions. Once the
patient is febrile (oral temperature greater than or equal to 38.3 degrees
Celsius), antibiotics are to be given according to Fever Day 1 instructions.
Initiate antibiotic therapy within the hour of the fever but not before obtaining
blood cultures. For each subsequent fever not within consecutive 24 hour
periods, collaborate with Physican/Nurse Practitioner regarding antibiotics to
start/discontinue. If a patient continues to be febrile for consecutive 24 hour
periods, continue to follow the pre-printed orders indicating which antibiotics
to administer.
g. S/P Hematopoietic Stem Cell Transplant Patients returning to the hospital for
complications related to their transplant, including infection, are to be
directly admitted to the Hematopoietic Stem Cell Transplant unit when
possible. When a bed is not available, they are to wait at home until a bed is
ready or if their condition warrants, they are to go to the Emergency
Department and be placed in a private room if possible.
1. If patient is febrile, ED nurse is to collaborate with Nurse
Practitioner/Physician regarding ED Approach to Patient with Possible
Neutropenic Fever (Appendix B)
2. Solid Tumor Febrile Neutopenia patients not undergoing HSCT
a. Notify Physician to obtain order to draw two sets of blood cultures. One set
is to be drawn from the vascular access device if present, and one set is to be
drawn peripherally. Obtain an order for urine culture/sensitivity and chest x-
ray.
Neutropenia Management for Oncology and Hematopoietic Stem Cell
Transplant Patients
c301911 Page 5 of 9
b. According to the 2007 NCCN guidelines, if there is entry or exit site
inflammation around the vascular access device, a set of cultures is to be
obtained from each lumen and Vancomycin should be started or added to the
existing empiric therapy. If the vascular access device cultures are positive
for infection, collaborate with Physician regarding obtaining further blood
cultures from each lumen, removal of the vascular access device, and
additional antibiotic therapy
c. Obtain order to start antibiotics. Initiate antibiotic therapy within the hour of
the fever, but not before obtaining blood cultures. If patient symptomatology
warrants, collaborate with Physician regarding obtaining site specific cultures
including rectal, stool, skin, mouth, throat, sputum, and nasopharynx.
d. Collaborate with Physician regarding initiating G-CSF therapy.
e. Febrile Neutropenic solid tumor oncology patients in the Emergency
Department are to be triaged according to the ED Approach to Patient with
Possible Neutropenic Fever (Appendix B)
B. Environmental Modification
1. All neutropenic patients are placed in private rooms. Patients admitted for HSCT
are to be placed in positive pressure rooms with HEPA filtration.
2. Neutropenia precaution sign is to be placed beside the door to alert staff and
visitors of infection prevention protocol/measures. Refer to Neutropenic
Precautions sign (Appendix A).
C. Protective Measures for Neutropenic Patients
1. Handwashing is the single most important intervention to prevent infection.
a. All persons entering the room will soap and wash hands at time of entry and
time of exit with either alcohol based gel or with soap and water for 15
seconds.
2. Anyone with symptoms of illness is to avoid contact with neutropenic patients.
When contact is unavoidable, staff/visitors are to wear masks when entering the
patients room and adhere to proper hand hygiene.
3. Children under the age of 12 are not to enter the Hematopoietic Stem Cell
Transplant unit regardless of the presence of neutropenic patients.
4. Allogeneic Hematopoietic Stem Cell Transplant patients are to be fitted for a N-
95 mask upon admission. Once neutropenic, ANC less than 1000, these patients
are to be instructed to wear this mask whenever they leave their room.
5. HSCT patients who are under contact isolation due to their being infected with a
highly transmissible infectious organism, such as VRE and MRSA, are to remain
in their room at all times, unless required to leave their room for testing. In this
case, the patient is to wear appropriate PPE, including yellow gown, and gloves.
If the patient is neutropenic and/or under airborne/droplet precautions a mask is to
be worn (N-95 for allogeneic transplant patients at all times, standard mask for
autologous transplant patients, unless a N-95 is required for airborne/droplet
precautions).
6. Avoid rectal maneuvers (rectal temperatures, enemas, rectal medications, rectal
tubes, digital exams) and urinary catheterizations.
Neutropenia Management for Oncology and Hematopoietic Stem Cell
Transplant Patients
c301911 Page 6 of 9
7. Avoid breakdown of skin and mucous membranes by limiting venipunctures or
other invasive procedures. Cleanse and protect wounds that break the skin as
directed by Physician/Nurse Practitioner.
8. Place patient on neutropenic diet and ensure that patient receives bottled water.
Patients undergoing HSCT are not to receive food prepared outside of the hospital
due to the potential for infection. Refer to Neutropenic Precautions sign
(Appendix A)
9. Change urinals and hats when visibly soiled. Change nasal canulas, O2 masks
weekly and when visibly soiled.
10. Change peripheral IVs every 3 days and IV tubing every 2 days. Refer to UCH
Policy and procedure: Lines, Central Venous for instructions regarding dressing
changes.
11. Encourage consistent patient personal hygiene
a. Daily shower or bath, including shampooing head/hair
b. Change linens daily and more frequently if visibly soiled.
c. Routine oral care. Refer to UCH Hospital Guidelines regarding oral care.
12. Live plant and flowers are not allowed in the rooms of neutropenic patients whose
immune compromise is such that infection can be acquired from soil/plant
organisms. Refer to UCH Policy and Procedure: Live Plant and Fresh Flower
Restrictions.
13. Animals are restricted from the Oncology/HSCT unit due to the potential
infection risk for the immunocompromised patient population. Refer to UCH
Policy and Procedure: Animal Assisted Activities/Therapy Program.
References:
1. Centers for Disease Control and Prevention. (2003). Guidelines for Environmental Infection
Control in Healthcare Facilities, 2003 [Data file]. Available from Centers for Disease
Control and Prevention web site, www.cdc.gov. (LOE I)
2. Marrs, J. (2006). Care of Patients With Neutropenia. Clinical Journal of Oncology Nursing,
10(2), 164-166. (LOE IV)
3. NCCN. (2007). Fever and Neutropenia-v.1.2007. NCCN Clinical Practice Guidelines in
Oncology. (CD). Jenkintown, PA: NCCN. (LOE I)
4. Nirenberg, A., Bush, A.P., Davis, A., Friese, C.R., Gillespie, T.W., Rice, R.D. (2006).
Neutropenia: State of the Knowledge Part I/Part II. Clinical Journal of Oncology Nursing,
33(6), 1193-1201, 1202-1208. (LOE I)
5. Shelton, B.K. (2003). Evidence-Based Care for the Neutropenic Patient with Leukemia.
Seminars in Oncology Nursing, 19(2), 133-141. (LOE IV)
6. West, F., Mitchell, S. (2004). Evidence-Based Guidelines for the Management of
Neutropenia Following Outpatient Hematopoietic Stem Cell Transplantation. Clinical
Journal of Oncology Nursing, 8(6), 601-613. (LOE IV)
7. Zitella, L., Friese, C., Hauser, J., Holmes, B.G., Woolery, M.A., OLeary, C., Andrews, F.
(2006). Putting Evidence Into Practice: Preventions of Infection. Clinical Journal of
Oncology Nursing, 10(6), 739-750. (LOE I)
c301911
Neutropenia Management for Oncology and Hematopoietic Stem Cell
Transplant Patients
c301911 Page 7 of 9
Appendix A
NEUTROPENIC PRECAUTIONS
WASH HANDS BEFORE PATIENT CONTACT
Visitors with cold symptoms or contagious illness should not visit patient at this time.
Patient MUST wear a mask when leaving room.
NO FRESH FLOWERS OR PLANTS.
DIETARY RESTRICTIONS INCLUDE:
Fresh fruit and vegetables ONLY if thick skinned
o (oranges, melon, bananas), not overly ripe and thoroughly washed with soap and water.
NO soft cheeses, unpasteurized foods/fluids, dried fruits, pepper or loose tea.
NO undercooked or raw meat, fish or eggs.
Teas will be prepared directly by staff for patient by request.
Fresh ice will be provided by staff from clean ice trays.
Serve bottled water ONLY to be ordered and provided on trays.
PLEASE SEE THE NURSE IF YOU HAVE ANY QUESTIONS REGARDING THESE
PRECAUTIONS
Neutropenia Management for Oncology and Hematopoietic Stem Cell
Transplant Patients
c301911 Page 8 of 9
Appendix B
ED Approach to Patient with Possible Neutropenic Fever
ED GOAL:
! To administer antibiotics within 1 hour of ED presentation for patients with ANC (absolute
neutrophil count) less than 1000 mm
3
! To recognize which patients require in-patient management and which can be safely
managed as outpatients
(see Risk Stratification, p. 10)
! To facilitate outpatient AND inpatient work-up and continuity with patients oncology team.
TRIAGE PROCEDURE:
! ID patient at triage
Patient with oncology information card
Patient s/p chemotherapy/radiation treatment within 14 days
Patient s/p hematopoietic stem cell transplant
Oncology patient with fever or other vague c/o
! Provide and instruct neutropenic patient to wear a mask
! Obtain patients weight
! Determine allergies
! Document Neutropenic Patient in comments on tracking board
! Assign triage ESI Level 2 and bring patient to exam room immediately (consider Green Care
Team ID Red/Yellow full)
! Notify Resource Nurse, who will notify attending or senior resident of patients arrival.
! Place Neutropenic packet of algorithms on patients chart
ED PROCEDURE:
! When patient is placed in exam room, immediately draw CBC with manual differential and
two sets of blood cultures.
! Draw second blood culture from another site
! Notify physician as soon as ANC results have returned (lab will call results to primary RN).
! If ANC less than 1000, send all other labs as ordered on pre-printed order sheet. Other labs
may be clinically indicated even if ANC is greater than 1000.
! After receiving ANC results, the ED Attending or Senior Resident will contact the inpatient
BMT Nurse Practitioner if the patient is s/p hematopoietic stem cell transplant; otherwise the
Oncology Fellow is to be notified.
! Physician will stratify patient to either IP or OP treatment (according to clinical criteria listed
in packet) and will order appropriate antibiotics if ANC less than 1000.
! If outpatient treatment is appropriate: the physician will call the patients primary
Oncologist/Nurse and will coordinate discharge with PO antibiotics.
! Antibiotics must be administered immediately upon receiving the order from the Senior
Resident or ED Attending.
Neutropenia Management for Oncology and Hematopoietic Stem Cell
Transplant Patients
c301911 Page 9 of 9
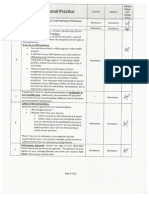
Risk Stratification in Febrile Neutropenia
Fever is defined as a single oral temperature greater than or equal to !38.3C (101F) or greater than or equal to
38.0C (100.4F) for greater than or equal to 1 hour. Neutropenia is defined as a neutrophil count less than 500
cells/mm
3
, or a count less than 1000 cells/mm
3
with a predicted decrease to less than 500 cells/mm
3
. (IDSA, 2002)
Group Description
Low
Risk (I)
Must
meet all
criteria
" No associated comorbid illnesses*
" Alert and oriented times 3 / No mental status changes
" Non transplant, solid tumor or hematologic malignancy with no previous fungal infection
" Serum creatinine less than 2mg/dl
" Liver function tests less than 3 times normal
" Receiving oncology care in the UCH system.
" Has resources and is able to fill oral antibiotic prescription within 12 hours (able to comply with and
consent to outpatient pathway)
" !Contact Hematology-Oncology Fellow to initiate outpatient order set and consent form.
High
Risk (II)
" Bone marrow transplant / hematologic malignancies or uncontrolled cancer
" Age greater than 60
" Altered mental status or confusion
" Unable to take PO medication (nausea / vomiting or mucositis); dehydration
" No telephone or transportation, no acute medical center within 1 hour from home
" Serum creatinine greater than 2.0 mg/dl or renal failure requiring intervention
" Liver function tests greater than 3 times normal
" SBP less than 90 mmHg, HR (resting) greater than 100 bpm, RR greater than 20/min, O2 sat less
than 90%(room air/baseline O2)
" Uncontrolled comorbid conditions*, significant burden of illness or poor performance status
" Expected prolonged neutropenia (less than 100/cells/mm
3
for greater than or equal to 7 days) or
bleeding requiring transfusion
" Obvious central line infection , pneumonia or other complex infection
" ! Initiate inpatient febrile neutropenia order set for inpatient admission and contact Hematology-
Oncology Fellow.
Critical
(III)
Meets high risk criteria and appears very ill (i.e. hypotension, shock)
! Initiate inpatient febrile neutropenia order set for inpatient critical car admission and contact Hematology-
Oncology Fellow.
*Comorbid conditions can include diabetes, COPD, CHF (cardiac problems or EKG changes.) The use of these guidelines is
subject to the clinical judgment of the practitioner and the patients clinical presentation.
OTR02030 (11/04)
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- As 1926.1 - 2012 Swimming Pool SafetyDocument49 pagesAs 1926.1 - 2012 Swimming Pool SafetyrteteNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- DMGT403 Accounting For Managers PDFDocument305 pagesDMGT403 Accounting For Managers PDFpooja100% (1)
- Fees Structure For Government Sponsored (KUCCPS) Students: University of Eastern Africa, BaratonDocument3 pagesFees Structure For Government Sponsored (KUCCPS) Students: University of Eastern Africa, BaratonGiddy LerionkaNo ratings yet
- Present Perfect.Document1 pagePresent Perfect.Leidy DiazNo ratings yet
- Vital StatisticsDocument35 pagesVital StatisticsRadha100% (1)
- Wall Street Expose: Monkey Business Reveals Investment Banking RealitiesDocument2 pagesWall Street Expose: Monkey Business Reveals Investment Banking Realitiestorquewip100% (1)
- Pathophysiology of Cardiogenic Pulmonary EdemaDocument8 pagesPathophysiology of Cardiogenic Pulmonary EdemaLili Fiorela CRNo ratings yet
- Microscopes Open Up An Entire World That You Can't See With The Naked EyeDocument4 pagesMicroscopes Open Up An Entire World That You Can't See With The Naked EyeLouie Jane EleccionNo ratings yet
- Advisor ChecklistDocument6 pagesAdvisor Checklistapi-255084253No ratings yet
- Final For GuidelinecomDocument10 pagesFinal For Guidelinecomapi-255084253No ratings yet
- Kyles Email Precepting AttendanceDocument2 pagesKyles Email Precepting Attendanceapi-255084253No ratings yet
- NeutrotoppppcDocument10 pagesNeutrotoppppcapi-255084253No ratings yet
- Pdca 2Document7 pagesPdca 2api-255084253No ratings yet
- Cna FlyerDocument1 pageCna Flyerapi-255084253No ratings yet
- Cna AcpcounciltemplateaprilDocument1 pageCna Acpcounciltemplateaprilapi-255084253No ratings yet
- Summary Email of April MeetingsDocument2 pagesSummary Email of April Meetingsapi-255084253No ratings yet
- Minutes From 2-14 MeetingDocument4 pagesMinutes From 2-14 Meetingapi-255084253No ratings yet
- Cnaacuitytool 3Document1 pageCnaacuitytool 3api-255084253No ratings yet
- Cna AcpcounciltemplatefebDocument1 pageCna Acpcounciltemplatefebapi-255084253No ratings yet
- Cna AcpcounciltemplatemarchDocument1 pageCna Acpcounciltemplatemarchapi-255084253No ratings yet
- Minutes From 3-14 MeetingDocument2 pagesMinutes From 3-14 Meetingapi-255084253No ratings yet
- Feedback Barb From Focus PdcaDocument2 pagesFeedback Barb From Focus Pdcaapi-255084253No ratings yet
- Mandatory April Meeting EmailDocument1 pageMandatory April Meeting Emailapi-255084253No ratings yet
- Falls Question CnaacpsDocument2 pagesFalls Question Cnaacpsapi-255084253No ratings yet
- Precept Form From KaylaDocument3 pagesPrecept Form From Kaylaapi-255084253No ratings yet
- Meeting Minutes From March EmailDocument1 pageMeeting Minutes From March Emailapi-255084253No ratings yet
- Email To Cnaacps About How To Access SPDocument1 pageEmail To Cnaacps About How To Access SPapi-255084253No ratings yet
- Sharepoint Vs Staff MeetingsDocument2 pagesSharepoint Vs Staff Meetingsapi-255084253No ratings yet
- Annsleys Response To FallsDocument2 pagesAnnsleys Response To Fallsapi-255084253No ratings yet
- Post Survey Respondent Unmatched Demographics UnmatchedDocument1 pagePost Survey Respondent Unmatched Demographics Unmatchedapi-255084253No ratings yet
- Kayla Eval On MeDocument1 pageKayla Eval On Meapi-255084253No ratings yet
- Email Confirmation From Anita All Cnas Are AddedDocument2 pagesEmail Confirmation From Anita All Cnas Are Addedapi-255084253No ratings yet
- 1st Sharepoint Posting CnaDocument2 pages1st Sharepoint Posting Cnaapi-255084253No ratings yet
- Post Survey Table MatchedDocument1 pagePost Survey Table Matchedapi-255084253No ratings yet
- Email To Anita About SPDocument1 pageEmail To Anita About SPapi-255084253No ratings yet
- Email About Sharepoint and TitlingDocument1 pageEmail About Sharepoint and Titlingapi-255084253No ratings yet
- 5314 Look Report Cna EmailDocument2 pages5314 Look Report Cna Emailapi-255084253No ratings yet
- Pantone and K100 Reverse White MedicineDocument16 pagesPantone and K100 Reverse White MedicinepaanarNo ratings yet
- Securifire 1000-ExtractedDocument2 pagesSecurifire 1000-ExtractedWilkeey EstrellanesNo ratings yet
- 8510C - 15, - 50, - 100 Piezoresistive Pressure Transducer: Features DescriptionDocument3 pages8510C - 15, - 50, - 100 Piezoresistive Pressure Transducer: Features Descriptionedward3600No ratings yet
- Pirates and Privateers of the Caribbean: A Guide to the GameDocument25 pagesPirates and Privateers of the Caribbean: A Guide to the GameLunargypsyNo ratings yet
- New Pacific Timber v. Señeris, 101 SCRA 686Document5 pagesNew Pacific Timber v. Señeris, 101 SCRA 686Ishmael AbrahamNo ratings yet
- Liebert PEX+: High Efficiency. Modular-Type Precision Air Conditioning UnitDocument19 pagesLiebert PEX+: High Efficiency. Modular-Type Precision Air Conditioning Unitjuan guerreroNo ratings yet
- Smartrac - Iolineug - r5Document66 pagesSmartrac - Iolineug - r5Darwin Elvis Giron HurtadoNo ratings yet
- BSHM 23 ReviewerDocument8 pagesBSHM 23 ReviewerTrixie Mae MuncadaNo ratings yet
- Declarative and Procedural Knowledge (Lêda's Final Paper) 2010 01Document13 pagesDeclarative and Procedural Knowledge (Lêda's Final Paper) 2010 01Jair Luiz S. FilhoNo ratings yet
- Going to the cinema listening practiceDocument2 pagesGoing to the cinema listening practiceMichael DÍligo Libre100% (1)
- MRI Week3 - Signal - Processing - TheoryDocument43 pagesMRI Week3 - Signal - Processing - TheoryaboladeNo ratings yet
- Ajwin Handbuch enDocument84 pagesAjwin Handbuch enEnzo AguilarNo ratings yet
- Drug Delivery Technologies and Future DirectionsDocument14 pagesDrug Delivery Technologies and Future Directionsraju1559405No ratings yet
- UEME 1143 - Dynamics: AssignmentDocument4 pagesUEME 1143 - Dynamics: Assignmentshikai towNo ratings yet
- Sles-55605 C071D4C1Document3 pagesSles-55605 C071D4C1rgyasuylmhwkhqckrzNo ratings yet
- GUEST MAIL HANDLINGDocument17 pagesGUEST MAIL HANDLINGJoelThambi0% (1)
- 3 5 3Document4 pages3 5 3Amr Mohamed RedaNo ratings yet
- JE Creation Using F0911MBFDocument10 pagesJE Creation Using F0911MBFShekar RoyalNo ratings yet
- Water 07 02314Document36 pagesWater 07 02314Satyajit ShindeNo ratings yet
- List of Psychotropic Drugs Under International ControlDocument32 pagesList of Psychotropic Drugs Under International ControlRadhakrishana DuddellaNo ratings yet
- Parts of A Computer With Their FunctionsDocument19 pagesParts of A Computer With Their FunctionsJaried SumbaNo ratings yet
- Data Structures LightHall ClassDocument43 pagesData Structures LightHall ClassIwuchukwu ChiomaNo ratings yet