Professional Documents
Culture Documents
Neclex Questions Test 3
Uploaded by
Brittany WorrallCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neclex Questions Test 3
Uploaded by
Brittany WorrallCopyright:
Available Formats
NEUROMUSCULAR DISORDERS 7. A patient with Guillain-Barr syndrome asks the nurse what has caused the disease.
In responding to the patient, the nurse explains that Guillain-Barr syndrome a. results from an acute infection and inflammation of the peripheral nerves. b. is due to an immune reaction that attacks the covering of the peripheral nerves. c. is caused by destruction of the peripheral nerves after exposure to a viral infection. d. results from degeneration of the peripheral nerve caused by viral attacks. Correct Answer: B 8. A 24-year-old patient is hospitalized with the onset of Guillain-Barr syndrome. During this phase of the patient's illness, the most essential assessment for the nurse to carry out is a. monitoring the cardiac rhythm continuously. b. determining the level of consciousness q2hr. c. evaluating sensation and strength of the extremities. d. performing constant evaluation of respiratory function. Correct Answer: D 10. A patient who has numbness and weakness of both feet is hospitalized with Guillain-Barr syndrome. The nurse will anticipate that collaborative interventions at this time will include a. intubation and mechanical ventilation. b. insertion of a nasogastric (NG) feeding tube. c. administration of methylprednisolone (Solu-Medrol). d. IV infusion of immunoglobulin (Sandoglobulin). Correct Answer: D 25. Which of these nursing actions for a patient with Guillain-Barr syndrome is most appropriate for the nurse to delegate to an experienced nursing assistant? a. Nasogastric tube feeding q4hr b. Artificial tear administration q2hr c. Assessment for bladder distension q2hr d. Passive range of motion to extremities q8hr Correct Answer: D 9. When caring for a patient who has Guillain-Barr syndrome, which assessment data obtained by the nurse will require the most immediate action? a. The patient complains of severe tingling pain in the feet. b. The patient has continuous drooling of saliva. c. The patient's blood pressure (BP) is 106/50 mm Hg. d. The patient's quadriceps and triceps reflexes are absent. Correct Answer: B 13. When teaching the patient with newly diagnosed multiple sclerosis (MS) about the disease, the nurse explains that a. MS is a congenitally acquired illness that causes progressive neurologic deterioration. b. impulses travel too fast over nerves that have lost their myelin coat and cause overstimulation of muscle fibers. c. autoimmune processes cause gradual destruction of the myelin sheath of nerves in the brain and spinal cord. d. antibodies are produced against acetylcholine receptors at the synapse and result in blocked muscle contraction. Correct Answer: C 14. When obtaining a health history and physical assessment for a patient with possible multiple sclerosis (MS), the nurse should a. confirm patient information with family members. b. ask about a recent history of temperature spikes. c. question the patient about any leg weakness or spasm. d. determine whether hypersexuality has caused problems.
Correct Answer: C 15. A 28-year-old woman has had multiple sclerosis (MS) for 3 years and wants to have children before her disease worsens. When she asks about the risks associated with pregnancy, the nurse explains that a. MS is associated with a slightly increased risk for congenital defects. b. symptoms of MS are likely to become worse during her pregnancy. c. women with MS frequently have premature labor. d. MS symptoms may be worse after the pregnancy. Correct Answer: D 16. A patient with multiple sclerosis (MS) is to begin treatment with glatiramer acetate (Copaxone). In planning the patient teaching necessary with the use of the drug, the nurse recognizes that the patient will need to be taught a. how to draw up and administer injections of the medication. b. use of contraceptive methods other than oral contraceptives for birth control. c. to plan laboratory monitoring of CBC, chemistries, and liver function every 3 months. d. that the drug will control symptoms but has no effect on the progression of the disease. Correct Answer: A 17. When planning care for a patient with MS who has a nursing diagnosis of risk for activity intolerance related to extremity weakness secondary to stress, the most appropriate patient goal is a. "The patient will express minimal stress level." b. "Strength in arms and legs will be maintained." c. "The patient will complete ADLs without fatigue." d. "Intake of high-nutrition foods will be adequate." Correct Answer: C 18. A patient with multiple sclerosis (MS) has a nursing diagnosis of urinary retention related to sensorimotor deficits. An appropriate nursing intervention for this problem is to a. decrease fluid intake in the evening. b. teach the patient how to use the Cred method. c. suggest the use of incontinence briefs for nighttime use only. d. assist the patient to the commode every 2 hours during the day. Correct Answer: B 19. The nurse identifies the nursing diagnosis of impaired physical mobility related to bradykinesia for a patient with Parkinson's disease. To assist the patient to ambulate safely, the nurse should a. allow the patient to ambulate only with assistance. b. instruct the patient to rock from side to side to initiate leg movement. c. have the patient take small steps in a straight line directly in front of the feet. d. teach the patient to keep the feet in contact with the floor and slide them forward. Correct Answer: B 20. A patient who has been taking bromocriptine (Parlodel) and benztropine (Cogentin) for Parkinson's disease is experiencing a worsening of symptoms. The nurse will anticipate that patient may benefit from a. complete drug withdrawal for a few weeks. b. use of levodopa (L-dopa)-carbidopa (Sinemet). c. withdrawal of anticholinergic therapy. d. increasing the dose of bromocriptine. Correct Answer: B 21. A patient with Parkinson's disease has decreased tongue mobility and an inability to move the facial muscles. The nurse recognizes that these impairments commonly contribute to the nursing diagnosis of a. disuse syndrome related to loss of muscle control. b. self-care deficit related to bradykinesia and rigidity. c. impaired verbal communication related to difficulty articulating. d. impaired oral mucous membranes related to inability to swallow.
Correct Answer: C 22. A patient has a new prescription for levodopa (L-dopa) to control symptoms of Parkinson's disease. Which assessment data obtained by the nurse may indicate a need for a decrease in the dose? a. The patient has a chronic dry cough. b. The patient has 4 loose stools in a day. c. The patient develops a deep vein thrombosis. d. The patient's blood pressure is 90/46 mm Hg. Correct Answer: D 23. A patient with myasthenia gravis (MG) is admitted to the hospital with severe weakness and acute respiratory insufficiency. The health care provider performs a Tensilon test to distinguish between myasthenic crisis and cholinergic crisis. During the test, it will be most important to monitor the patient's a. pupillary size. b. muscle strength. c. respiratory function. d. level of consciousness (LOC). Correct Answer: C 24. When teaching a patient with myasthenia gravis (MG) about management of the disease, the nurse advises the patient to a. anticipate the need for weekly plasmapheresis treatments. b. protect the extremities from injury due to poor sensory perception. c. do frequent weight-bearing exercise to prevent muscle atrophy. d. perform necessary physically demanding activities in the morning. Correct Answer: D 25. A hospitalized patient with myasthenia gravis (MG) has a nursing diagnosis of imbalanced nutrition: less than body requirements related to impaired swallowing. To promote nutrition, the nurse suggests that before meals the patient should avoid a. watching television. b. talking on the phone. c. typing on the computer. d. ambulating in the halls. Correct Answer: B 27. A patient with amyotrophic lateral sclerosis (ALS) is hospitalized with pneumonia. Which nursing action will be included in the plan of care? a. Observing for agitation and paranoia b. Assisting the patient with active range of motion (ROM) c. Using simple words and phrases to explain procedures d. Administer muscle relaxants as needed for muscle spasms Correct Answer: B 31. A patient is seen in the health clinic with symptoms of a stooped posture, shuffling gait, and pill rolling-type tremor. The nurse will anticipate teaching the patient about a. preparation for an MRI. b. purpose of EEG testing. c. antiparkinsonian drugs. d. oral corticosteroids. Correct Answer: C SPINAL CORD INJURY/TBI 5. A patient has a lesion that affects lower motor neurons. During assessment of the patient's lower extremities, the nurse expects to find
a. spasticity. b. flaccidity. c. hyperactive reflexes. d. loss of sensation. Answer: B 2. When interviewing an acutely confused patient with a head injury, which of these questions will provide the most useful information? a. "Have you ever been hospitalized for a neurologic problem?" b. "Do you have any pain at the present time?" c. "What have you had to eat in the last 24 hours?" d. "Can you describe you usual pattern for coping with injury?" Answer: B 9. When admitting a patient with acute confusion to the hospital, the nurse will interview the patient about health problems and health history primarily to a. determine the patient's motivation for self-care. b. include the patient in health care decisions. c. use the information given by the patient to guide care. d. assess the patient's baseline cognitive abilities. Answer: D 13. The following orders are received for a patient who is unconscious after a head injury caused by an automobile accident. Which one should the nurse question? a. Perform neurologic checks every 15 minutes. b. Prepare the patient for lumbar puncture. c. Obtain x-rays of the skull and spine. d. Do computed tomography (CT) scan with and without contrast. Answer: B 8. When obtaining a health history from a patient with a neurologic problem, which question by the nurse will elicit the most useful response from the patient? a. "Do you ever have any nausea or dizziness?" b. "Does the pain radiate from your back into your legs?" c. "Do you have any sensations of pins and needles in your feet?" d. "Can you describe the sensations you are having in your chest?" Answer: D 4. In a patient who has a corticospinal tract lesion, the nurse should assess for a. extremity movement and strength. b. cranial nerve function. c. peripheral sensitivity to pain. d. level of consciousness (LOC). Answer: A 2. When admitting a patient who has a history of paraplegia as a result of a spinal cord injury, the nurse will plan to a. check the patient for urinary incontinence every 2 hours to maintain skin integrity. b. assist the patient to the toilet on a scheduled basis to help ensure bladder emptying. c. use intermittent catheterization on a regular schedule to avoid the risk of infection. d. ask the patient about the usual urinary pattern and measures used for bladder control. Answer: D 12. Neurologic testing of the patient by the nurse indicates impaired functioning of the left glossopharyngeal nerve (CN IX) and the vagus nerve (CN X). Based on these findings, the nurse plans to a. insert an oral airway. b. withhold oral fluid or foods.
c. provide highly seasoned foods. d. apply artificial tears every hour. Answer: B 11. To assess the functioning of the optic nerve (CN II), the nurse should a. apply a cotton wisp strand to the cornea. b. have the patient read a magazine. c. shine a bright light into the patient's pupil. d. check for equal opening of the eyelids. Answer: B 13. The following orders are received for a patient who is unconscious after a head injury caused by an automobile accident. Which one should the nurse question? a. Perform neurologic checks every 15 minutes. b. Prepare the patient for lumbar puncture. c. Obtain x-rays of the skull and spine. d. Do computed tomography (CT) scan with and without contrast. Answer: B 14. The charge nurse is observing a new staff nurse who is assessing a patient with a possible spinal cord lesion for sensation. Which action indicates a need for further teaching about neurologic assessment? a. The new nurse tests for light touch before testing for pain. b. The new nurse has the patient close the eyes during testing. c. The new nurse tells the patient, "You may feel a pinprick now." d. The new nurse uses an irregular pattern to test for intact touch. Answer: C 16. When reviewing the results of a patient's cerebrospinal fluid analysis, the nurse will notify the health care provider about a. pH of 7.35. b. white blood cell count (WBC) of 4/ml (0.004/L). c. protein 30 mg/dl (0.30 g/L). d. glucose 30 mg/dl (1.7 mmol/L). Answer: D 13. A patient with a neck fracture at the C5 level is admitted to the intensive care unit (ICU) following initial treatment in the emergency room. During initial assessment of the patient, the nurse recognizes the presence of spinal shock on finding a. hypotension, bradycardia, and warm extremities. b. involuntary, spastic movements of the arms and legs. c. the presence of hyperactive reflex activity below the level of the injury. d. flaccid paralysis and lack of sensation below the level of the injury. Correct Answer: D 14. When caring for a patient who had a C8 spinal cord injury 10 days ago and has a weak cough effort, bibasilar crackles, and decreased breath sounds, the initial intervention by the nurse should be to a. administer oxygen at 7 to 9 L/min with a face mask. b. place the hands on the epigastric area and push upward when the patient coughs. c. encourage the patient to use an incentive spirometer every 2 hours during the day. d. suction the patient's oral and pharyngeal airway. Correct Answer: B 15. As a result of a gunshot wound, a patient has an incomplete right spinal cord lesion at the level of T7, resulting in Brown-Squard syndrome. Which nursing action should be included in the plan of care? a. Assessment of the patient for left leg pain
b. Assessment of the patient for left arm weakness c. Positioning the patient's right leg when turning the patient d. Teaching the patient to look at the left leg to verify its position Correct Answer: C 16. A patient with a T1 spinal cord injury is admitted to the intensive care unit (ICU). The nurse will teach the patient and family that a. use of the shoulders will be preserved. b. full function of the patient's arms will be retained. c. total loss of respiratory function may occur temporarily. d. elevations in heart rate are common with this type of injury. Correct Answer: B 17. The health care provider orders administration of IV methylprednisolone (Solu-Medrol) for the first 24 hours to a patient who experienced a spinal cord injury at the T10 level 3 hours ago. When evaluating the effectiveness of the medication the nurse will assess a. blood pressure and heart rate. b. respiratory effort and O2 saturation. c. motor and sensory function of the legs. d. bowel sounds and abdominal distension. Correct Answer: C 18. A patient with a paraplegia resulting from a T10 spinal cord injury has a neurogenic reflex bladder. When the nurse develops a plan of care for this problem, which nursing action will be most appropriate? a. Teaching the patient how to self-catheterize b. Assisting the patient to the toilet q2-3hr c. Use of the Cred method to empty the bladder d. Catheterization for residual urine after voiding Correct Answer: A 19. A patient with a history of a T2 spinal cord tells the nurse, "I feel awful today. My head is throbbing, and I feel sick to my stomach." Which action should the nurse take first? a. Notify the patient's health care provider. b. Check the blood pressure (BP). c. Give the ordered antiemetic. d. Assess for a fecal impaction. Correct Answer: B Rationale: The BP should be assessed immediately in a patient with an injury at the T6 level or higher who complains of a headache to determine whether autonomic dysreflexia is causing the symptoms, including hypertension. Notification of the patient's health care provider is appropriate after the BP is obtained. Administration of an antiemetic is indicated after autonomic dysreflexia is ruled out as the cause of the nausea. The nurse may assess for a fecal impaction, but this should be done after checking the BP and lidocaine jelly should be used to prevent further increases in the BP. 20. The nurse discusses long-range goals with a patient with a C6 spinal cord injury. An appropriate patient outcome is a. transfers independently to a wheelchair. b. drives a car with powered hand controls. c. turns and repositions self independently when in bed. d. pushes a manual wheelchair on flat, smooth surfaces. Correct Answer: D 21. A patient who sustained a T1 spinal cord injury a week ago refuses to discuss the injury and becomes verbally abusive to the nurses and other staff. The patient demands to be transferred to another hospital, where "they know what they are doing." The best response by the nurse to the patient's behavior is to a. ask for the patient's input into the plan for care.
b. clarify that abusive behavior will not be tolerated. c. reassure the patient that the anger will pass and rehabilitation will then progress. d. ignore the patient's anger and continue to perform needed assessments and care. Correct Answer: A 22. A 26-year-old patient with a C8 spinal cord injury tells the nurse, "My wife and I have always had a very active sex life, and I am worried that she may leave me if I cannot function sexually." The most appropriate response by the nurse to the patient's comment is to a. advise the patient to talk to his wife to determine how she feels about his sexual function. b. tell the patient that sildenafil (Viagra) helps to decrease erectile dysfunction in patients with spinal cord injury. c. inform the patient that most patients with upper motor neuron injuries have reflex erections. d. suggest that the patient and his wife work with a nurse specially trained in sexual counseling. Correct Answer: D 23. A 25-year-old patient has returned home following extensive rehabilitation for a C8 spinal cord injury. The home care nurse visits and notices that the patient's spouse and parents are performing many of the activities of daily living (ADLs) that the patient had been managing during rehabilitation. The most appropriate action by the nurse at this time is to a. tell the family members that the patient can perform ADLs independently. b. remind the patient about the importance of independence in daily activities. c. recognize that it is important for the patient's family to be involved in the patient's care and support their activities. d. develop a plan to increase the patient's independence in consultation with the with the patient, spouse, and parents. Correct Answer: D 27. When caring for a patient who was admitted 24 hours previously with a C5 spinal cord injury, which nursing action has the highest priority? a. Continuous cardiac monitoring for bradycardia b. Administration of methylprednisolone (Solu-Medrol) infusion c. Assessment of respiratory rate and depth d. Application of pneumatic compression devices to both legs Correct Answer: C SEIZURES 7. A patient has a tonic-clonic seizure while the nurse is in the patient's room. During the seizure, it is important for the nurse to a. insert an oral airway during the seizure to maintain a patent airway. b. restrain the patient's arms and legs to prevent injury during the seizure. c. avoid touching the patient to prevent further nervous system stimulation. d. time and observe and record the details of the seizure and postictal state. Correct Answer: D Rationale: Because diagnosis and treatment of seizures frequently are based on the description of the seizure, recording the length and details of the seizure is important. Insertion of an oral airway and restraining the patient during the seizure are contraindicated. The nurse may need to move the patient to decrease the risk of injury during the seizure. 8. The nurse witnesses a patient with a seizure disorder as the patient suddenly jerks the arms and legs, falls to the floor, and regains consciousness immediately. It will be most important for the nurse to a. document the timing and description of the seizure. b. notify the patient's health care provider about the seizure. c. give the scheduled dose of divalproex (Depakote). d. assess the patient for a possible head injury. Correct Answer: D
9. After experiencing a generalized tonic-clonic seizure in the classroom, an elementary school teacher is evaluated and diagnosed with idiopathic epilepsy. The patient cries and tells the nurse, "I can not teach anymore. It will be too difficult for the students if this happens again at work." The most appropriate nursing diagnosis for the patient is a. anxiety related to loss of control during seizures. b. hopelessness related to diagnosis of chronic illness. c. disturbed body image related to new diagnosis of a seizure disorder. d. ineffective role performance related to misinformation about epilepsy. Correct Answer: D 10. The health care provider prescribes phenytoin (Dilantin) for control of complex partial seizures. After the nurse has taught the patient about phenytoin, which patient statement indicates understanding of the medication? a. "I should use soft swabs rather than a toothbrush to clean my mouth." b. "After I have a seizure, I should call an ambulance to take me to the hospital." c. "I may need to have my blood taken frequently to check the level of the Dilantin." d. "I will take the medication at the beginning of the seizure when I experience an aura." Correct Answer: C 11. When a patient experiences a generalized tonic-clonic seizure in the emergency department after a head injury, all of the following orders are received. Which one will the nurse implement first? a. Send to radiology for computed tomography (CT) scan. b. Administer midazolam (Versed). c. Check capillary blood glucose. d. Monitor level of consciousness (LOC). Correct Answer: B 12. A patient found in a tonic-clonic seizure reports afterward that the seizure was preceded by numbness and tingling of the arm. The nurse knows that this finding indicates a(n) _____ seizure. a. absence b. simple partial c. complex partial d. generalized myoclonic Correct Answer: C
STROKE The nurse obtains all of the following information about a 65-year-old patient in the clinic. When developing a plan to decrease stroke risk, which risk factor is most important for the nurse to address? a. The patient smokes a pack of cigarettes daily. b. The patient's blood pressure (BP) is chronically between 150/80 to 170/90 mm Hg. c. The patient works at a desk and relaxes by watching television. d. The patient is 25 pounds above the ideal weight. Correct Answer: B Rationale: Hypertension is the most important modifiable risk factor. Smoking, physical inactivity, and obesity all contribute to stroke risk but not so much as hypertension. A patient with right-sided weakness that started 1 hour ago is admitted to the emergency department and all these diagnostic tests are ordered. Which order should the nurse act on first? a. Noncontrast computed tomography (CT) scan b. Chest radiograph
c. Complete blood count (CBC) d. Electrocardiogram (ECG) Correct Answer: A Rationale: Rapid screening with a noncontrast CT scan is needed before administration of tissue plasminogen activator (tPA), which must be given within 3 hours of the onset of clinical manifestations of the stroke. The sooner the tPA is given, the smaller the area of brain injury. The other diagnostic tests give information about possible causes of the stroke and do not need to be completed as urgently as the CT scan. The nurse expects that management of the patient who experiences a brief episode of tinnitus, diplopia, and dysarthria with no residual effects will include a. heparin via continuous intravenous infusion. b. prophylactic clipping of cerebral aneurysms. c. therapy with tissue plasminogen activator (tPA). d. oral administration of ticlopidine (Ticlid). Correct Answer: D Rationale: The patient's symptoms are consistent with transient ischemic attack (TIA), and drugs that inhibit platelet aggregation are prescribed after a TIA to prevent stroke. Continuous heparin infusion is not routinely used after TIA or with acute ischemic stroke. The patient's symptoms are not consistent with a cerebral aneurysm. tPA is used only for acute ischemic stroke, but not for TIA. Aspirin is ordered for a patient who is admitted with a possible stroke. Which information obtained during the admission assessment indicates that the nurse should consult with the health care provider before giving the aspirin? a. The patient has atrial fibrillation. b. The patient has dysphasia. c. The patient states, "I suddenly developed a terrible headache." d. The patient has a history of brief episodes of right hemiplegia. Correct Answer: C Rationale: A sudden-onset headache is typical of a subarachnoid hemorrhage, and aspirin is contraindicated. Atrial fibrillation, dysphasia, and transient ischemic attack (TIA) are not contraindications to aspirin use, so the nurse can administer the aspirin. A patient with a stroke experiences right-sided arm and leg paralysis and facial drooping on the right side. When obtaining admission assessment data about the patient's clinical manifestations, it is most important the nurse assess the patient's a. ability to follow commands. b. visual fields. c. right-sided reflexes. d. emotional state. Correct Answer: A Rationale: Because the patient with a left-sided brain stroke may also have difficulty with comprehension and use of language, so it is important to obtain baseline data about the ability to follow commands. This will impact on patient safety and nursing care. The visual fields are not typically affected by a left-sided stroke. Information about reflexes
and emotional state will be collected but is not as high a priority as information about language abilities. 6. The nurse on the medical unit receives a verbal report from the emergency department nurse that a patient has an occlusion of the left posterior cerebral artery. When admitting the patient to the medical floor, the nurse will anticipate that the patient may have a. visual deficits. b. dysphasia. c. confusion. d. poor judgment. Correct Answer: A Rationale: Visual disturbances are expected with posterior cerebral artery occlusion. Aphasia occurs with middle cerebral artery involvement. Cognitive deficits and changes in judgment are more typical of anterior cerebral artery occlusion. The health care provider prescribes clopidogrel (Plavix) for a patient with cerebral atherosclerosis. When teaching about the new medication, the nurse will tell the patient a. that Plavix will reduce cerebral artery plaque formation. b. to monitor and record the blood pressure daily. c. to call the health care provider if stools are tarry. d. that Plavix will dissolve clots in the cerebral arteries. Correct Answer: C Rationale: Plavix inhibits platelet function and increases the risk for gastrointestinal bleeding, so patients should be advised to notify the health care provider about any signs of bleeding. The medication does not lower blood pressure, decrease plaque formation, or dissolve clots. The health care provider recommends a carotid endarterectomy for a patient with carotid atherosclerosis and a history of transient ischemic attacks (TIA). The patient asks the nurse to describe the procedure. Which response by the nurse is appropriate? a. "The diseased portion of the artery in the brain is removed and replaced with a synthetic graft." b. "The carotid endarterectomy involves surgical removal of plaque from an artery in the neck." c. "A catheter with a deflated balloon is positioned at the narrow area, and the balloon is inflated to flatten the plaque." d. "A wire is threaded through an artery in the leg to the clots in the carotid artery and the clots are removed." Correct Answer: B Rationale: In a carotid endarterectomy, the carotid artery is incised and the plaque is removed. The response beginning, "The diseased portion of the artery in the brain is removed" describes an arterial graft procedure. The answer beginning, "A catheter with a deflated balloon is positioned at the narrow area" describes an angioplasty. The final response (beginning, "A wire is threaded through the artery") describes the Merci procedure. On initial assessment of a patient hospitalized following a stroke, the nurse finds the patient's blood pressure to be 180/90 mm Hg. Which of the following orders by the health care provider should the nurse question? a. Infuse normal saline at 75 ml/hr. b. Keep head of bed elevated at least 30 degrees.
c. Administer tissue plasminogen activator (tPA) per protocol. d. Titrate labetolol (Normodyne) drip to keep BP less than 140/90 mm Hg. Correct Answer: D Rationale: Since elevated BP may be a protective response to maintain cerebral perfusion, antihypertensive therapy is recommended only if MAP is >130 mm Hg or systolic pressure is >220 mm Hg. Fluid intake should be 1500 to 2000 ml daily to maintain cerebral blood flow. The head of the bed should be elevated to at least 30 degrees unless the patient has symptoms of poor tissue perfusion. tPA may be administered if the patient meets the other criteria for tPA use. A patient with a history of several transient ischemic attacks (TIAs) arrives in the emergency room with hemiparesis and dysarthria that started 2 hours previously. The nurse anticipates the need to prepare the patient for a. intravenous heparin administration. b. transluminal angioplasty. c. surgical endarterectomy. d. tissue plasminogen activator (tPA) infusion. Correct Answer: D Rationale: The patient's history and clinical manifestations suggest an acute ischemic stroke and a patient who is seen within 3 hours of stroke onset is likely to receive tPA (after screening with a CT scan). Heparin administration in the emergency phase is not indicated. Emergent carotid transluminal angioplasty or endarterectomy are not indicated for the patient who is having an acute ischemic stroke. The nurse identifies the nursing diagnosis of impaired verbal communication for a patient with expressive aphasia. An appropriate nursing intervention to help the patient communicate is to a. ask simple questions that the patient can answer with "yes" or "no." b. develop a list of words that the patient can read and practice reciting. c. have the patient practice facial and tongue exercises to improve motor control necessary for speech. d. prevent embarrassing the patient by changing the subject if the patient does not respond in a timely manner. Correct Answer: A Rationale: Communication will be facilitated and less frustrating to the patient when questions that require a "yes" or "no" response are used. When the language areas of the brain are injured, the patient might not be able to read or recite words, which will frustrate the patient without improving communication. Expressive aphasia is caused by damage to the language areas of the brain, not by the areas that control the motor aspects of speech. The nurse should allow time for the patient to respond. A patient with a stroke has progressive development of neurologic deficits with increasing weakness and decreased level of consciousness (LOC). The priority nursing diagnosis for the patient is a. risk for impaired skin integrity related to immobility. b. disturbed sensory perception related to brain injury. c. risk for aspiration related to inability to protect airway. d. impaired physical mobility related to weakness. Correct Answer: C Rationale: Protection of the airway is the priority of nursing care for a patient having an acute stroke. The other
diagnoses are also appropriate, but interventions to prevent aspiration are the priority at this time. A patient has a stroke affecting the right hemisphere of the brain. Based on knowledge of the effects of right brain damage, the nurse establishes a nursing diagnosis of a. impaired physical mobility related to right hemiplegia. b. impaired verbal communication related to speech-language deficits. c. risk for injury related to denial of deficits and impulsiveness. d. ineffective coping related to depression and distress about disability. Correct Answer: C Rationale: Right-sided brain damage typically causes denial of any deficits and poor impulse control, leading to risk for injury when the patient attempts activities such as transferring from a bed to a chair. Right-sided brain damage causes left hemiplegia. Left-sided brain damage typically causes language deficits. Left-sided brain damage is associated with depression and distress about the disability. 14. A patient with homonymous hemianopsia resulting from a stroke has a nursing diagnosis of disturbed sensory perception related to hemianopsia. To help the patient learn to compensate for the deficit during the rehabilitation period, the nurse should a. apply an eye patch to the affected eye. b. approach the patient on the unaffected side. c. place objects necessary for activities of daily living on the patient's affected side. d. have the patient use the eye muscles to move the eyes through the entire visual field. Correct Answer: C Rationale: During the rehabilitation period, placing objects on the affected side will encourage the patient to use the scanning technique to visualize the affected side. Because homonymous hemianopsia affects half the visual field in each eye, use of an eye patch is not appropriate. Approaching the patient on the affected side is appropriate during the acute period but does not help the patient learn skills needed to compensate for the visual defect. The problem is with the visual field, not with the eye muscles, so practice moving the eyes through the visual field will not be effective. A patient who has had a subarachnoid hemorrhage is being cared for in the intensive care unit. Which information about the patient is most important to communicate to the health care provider? a. The patient complains of an ongoing severe headache. b. The patient's blood pressure is 90/50 mm Hg. c. The cerebrospinal fluid (CFS) report shows red blood cells (RBCs). d. The patient complains about having a stiff neck. Correct Answer: B Rationale: To prevent cerebral vasospasm and maintain cerebral perfusion, blood pressure needs to be maintained at a high level after a subarachnoid hemorrhage. A low or drop in BP indicates a need to administer fluids and/or vasopressors to increase the BP An ongoing headache, RBCs in the CSF, and a stiff neck are all typical clinical manifestations of a subarachnoid hemorrhage and do not need to be rapidly communicated to the health care provider. The nurse identifies the nursing diagnosis of imbalanced nutrition: less than body requirements related to inability to feed self for a patient with right-sided hemiplegia. An appropriate nursing intervention is to
a. assist the patient to eat with the left hand. b. provide oral care before and after meals. c. teach the patient the "chin-tuck" technique. d. provide a wide variety of food choices. Correct Answer: A Rationale: Because the nursing diagnosis indicates that the patient's imbalanced nutrition is related to the right-sided hemiplegia, the appropriate interventions will focus on teaching the patient to use the left hand for self-feeding. The other interventions are appropriate for patients with other etiologies for the imbalanced nutrition. 17. The nurse is assisting the patient who is recovering from an acute stroke and has right-side hemiplegia to transfer from the bed to the wheelchair. Which action by the nurse is appropriate? a. Positioning the wheelchair next to the bed on the patient's right side b. Placing the wheelchair parallel to the bed on the patient's left side c. Setting the wheelchair directly in front of the patient, who is sitting on the side of the bed d. Moving the wheelchair a few steps from the bed and having the patient walk to the chair Correct Answer: B Rationale: Placing the wheelchair on the patient's left side will allow the patient to use the left hand to grasp the left arm of the chair to transfer. If the chair is placed on the patient's right side or in front of the patient, it will be awkward to use the strong arm, and the patient will be at increased risk for a fall. Because the patient has hemiplegia, it is not appropriate to place the chair where the patient will need to walk to it. A 32-year-old patient has a stroke resulting from a ruptured aneurysm and subarachnoid hemorrhage. Which intervention will be included in the care plan? a. Encouraging patient to cough and deep breath every 4 hours b. Inserting an oropharyngeal airway to prevent airway obstruction c. Assisting to dangle on edge of bed and assess for dizziness d. Applying intermittent pneumatic compression stockings Correct Answer: D Rationale: The patient with a subarachnoid hemorrhage usually has minimal activity to prevent cerebral vasospasm or further bleeding and is at risk for deep vein thrombosis (DVT). Activities (such as coughing and sitting up) that might increase intracranial pressure (ICP) or decrease cerebral blood flow are avoided. Because there is no indication that the patient is unconscious, an oropharyngeal airway is inappropriate. A patient who has had a stroke has a new order to attempt oral feedings. The nurse should assess the gag reflex and then a. offer the patient a sip of juice. b. order a varied pureed diet. c. assess the patient's appetite. d. assist the patient into a chair.
Correct Answer: D Rationale: The patient should be as upright as possible before attempting feeding to make swallowing easier and decrease aspiration risk. To assess swallowing ability, the nurse should initially offer water or ice to the patient. Pureed diets are not recommended because the texture is too smooth. The patient may have a poor appetite, but the oral feeding should be attempted regardless. A patient has right-sided weakness and aphasia as a result of a stroke but is attempting to use the left hand for feeding and other activities. The patient's wife insists on feeding and dressing him, telling the nurse, "I just don't like to see him struggle." A nursing diagnosis that is most appropriate in this situation is a. situational low self-esteem related to increasing dependence on others. b. interrupted family processes related to effects of illness of a family member. c. disabled family coping related to inadequate understanding by patient's spouse. d. ineffective therapeutic regimen management related to hemiplegia and aphasia. Correct Answer: C Rationale: The information supports the diagnosis of disabled family coping because the wife does not understand the rehabilitation program. There are no data supporting low self-esteem, and the patient is attempting independence. The data do not support an interruption in family processes because this may be a typical pattern for the couple. The patient's attempts to use the left hand indicate that he is managing the therapeutic regimen appropriately. Several weeks after a stroke, a patient has urinary incontinence resulting from an impaired awareness of bladder fullness. A bladder retraining program for the patient should include a. limiting fluid intake to 1000 ml daily to reduce urine volume. b. assisting the patient onto the bedside commode every 2 hours. c. performing intermittent catheterization after each voiding to check for residual urine. d. using an external "condom" catheter to protect the skin and prevent embarrassment. Correct Answer: B Rationale: Developing a regular voiding schedule will prevent incontinence and may increase patient awareness of a full bladder. A 1000-ml fluid intake is too restricted and will lead to dehydration. Intermittent catheterization and use of a condom catheter are appropriate in the acute phase of stroke but should not be considered solutions for long-term management because of the risks for urinary tract infection (UTI) and skin breakdown. A 72-year-old is being discharged home following a stroke. The patient is able to walk with assistance but needs help with hygiene, dressing, and eating. Which statement by the patient's wife indicates that discharge planning goals have been met? a. "I can provide the care my husband needs if I use the support and resources available in the community." b. "Because my husband will have continuous improvement in his condition, I won't need outside assistance in his care for very long." c. "I can handle all of my husband's needs thanks to the instructions you've given me." d. "I have arranged for a home health aide to provide all the care my husband will need." Correct Answer: A Rationale: The statement that community resources will be used indicates a realistic outcome. The patient is unlikely to continue to improve to the point of needing no assistance. The wife is likely to be overwhelmed by the patient's needs if she attempts to manage without assistance. There is no indication that the patient will need a home health
aide to meet all of his care needs. A patient who has a history of a transient ischemic attack (TIA) has an order for aspirin 160 mg daily. When the nurse is administering the medications, the patient says, "I don't need the aspirin today. I don't have any aches or pains." Which action should the nurse take? a. Document that the aspirin was refused by the patient. b. Call the health care provider to clarify the medication order. c. Explain that the aspirin is ordered to decrease stroke risk. d. Tell the patient that the aspirin is used to prevent aches. Correct Answer: C Rationale: Aspirin is ordered to prevent stroke in patients who have experienced TIAs. Documentation of the patient's refusal to take the medication is an inadequate response by the nurse. There is no need to clarify the order with the health care provider. The aspirin is not ordered to prevent aches and pains. A patient is admitted to the hospital with dysphasia and right-sided weakness that resolves in a few hours. The nurse will anticipate teaching the patient about a. alteplase (tPA). b. aspirin (Ecotrin). c. warfarin (Coumadin). d. nimodipine (Nimotop). Correct Answer: B Rationale: Following a TIA, patients typically are started on medications such as aspirin to inhibit platelet function and decrease stroke risk. tPA is used for acute ischemic stroke. Coumadin is usually used for patients with atrial fibrillation. Nimodipine is used to prevent cerebral vasospasm after a subarachnoid hemorrhage. The nurse is caring for a patient with carotid artery narrowing who has just returned after having left carotid artery angioplasty and stenting. Which assessment information is of most concern to the nurse? a. The pulse rate is 104 beats/min. b. There are fine crackles at the lung bases. c. The patient has difficulty talking. d. The blood pressure is 142/88 mm Hg. Correct Answer: C Rationale: Small emboli can occur during carotid artery angioplasty and stenting, and the aphasia indicates a possible stroke during the procedure. Slightly elevated pulse rate and blood pressure are not unusual as a result of anxiety associated with the procedure. Fine crackles at the lung bases may indicate atelectasis caused by immobility during the procedure; the nurse should have the patient take some deep breaths. A patient with left-sided hemiparesis arrives by ambulance to the emergency department. Which action should the nurse take first? a. Obtain the Glasgow Coma Scale score. b. Check the respiratory rate. c.
Monitor the blood pressure. d. Send the patient for a CT scan. Correct Answer: B Rationale: The initial nursing action should be to assess the airway and take any needed actions to assure a patent airway. The other activities should take place quickly after the ABCs (airway, breathing, circulation) are completed. A patient with sudden-onset right-sided weakness has a CT scan and is diagnosed with an intracerebral hemorrhage. Which information about the patient is most important to communicate to the health care provider? a. The patient has atrial fibrillation and takes warfarin (Coumadin). b. The patient takes a diuretic because of a history of hypertension. c. The patient's blood pressure is 144/90 mm Hg. d. The patient's speech is difficult to under Correct Answer: A Rationale: The use of warfarin will have contributed to the intracerebral bleeding and remains a risk factor for further bleeding. Administration of vitamin K is needed to reverse the effects of the warfarin, especially if the patient is to have surgery to correct the bleeding. The history of hypertension is a risk factor for the patient but has no immediate effect on the patient's care. The BP of 144/90 indicates the need for ongoing monitoring but not for any immediate change in therapy. Slurred speech is consistent with a left-sided stroke, and no change in therapy is indicated. A patient with a left-sided brain stroke suddenly bursts into tears when family members visit. The nurse should a. explain to the family that depression is normal following a stroke. b. have the family members leave the patient alone for a few minutes. c. teach the family that emotional outbursts are common after strokes. d. use a calm voice to ask the patient to stop the crying behavior. Correct Answer: C Rationale: Patients who have left-sided brain stroke are prone to emotional outbursts, which are not necessarily related to the emotional state of the patient. Depression after a stroke is common, but the suddenness of the patient's outburst suggests that depression is not the major cause of the behavior. The family should stay with the patient. The crying is not within the patient's control and asking the patient to stop will lead to embarrassment.
You might also like
- Medical Surgical Nursing Nclex Questions Neuro2Document12 pagesMedical Surgical Nursing Nclex Questions Neuro2dee_day_8No ratings yet
- Neur0 NLE Practice ExamDocument10 pagesNeur0 NLE Practice ExamRI NANo ratings yet
- NCLEX Test CVA, Neuro 24Document19 pagesNCLEX Test CVA, Neuro 24Ann Michelle TarrobagoNo ratings yet
- Psyche AnswersDocument16 pagesPsyche AnswersFreeNursingNotesNo ratings yet
- Chapter 37 - Management of Patients With Gastric and Duodenal DisordersDocument9 pagesChapter 37 - Management of Patients With Gastric and Duodenal DisordersMindy Severino100% (1)
- Psycho Social Cultural Integrity RationalesDocument10 pagesPsycho Social Cultural Integrity Rationalesrhymes2u100% (3)
- Cancer Exam 3Document14 pagesCancer Exam 3Stella Jane Megano100% (1)
- NCLEXDocument13 pagesNCLEXJheanAlphonsineT.MeansNo ratings yet
- Quiz 13 Medical Surgical NursingDocument18 pagesQuiz 13 Medical Surgical NursingHannahleth Gorzon100% (1)
- Special - NCLEX - Exam - Jakarta - Students - PDF Filename UTF-8''Special NCLEX Exam - Jakarta StudentsDocument23 pagesSpecial - NCLEX - Exam - Jakarta - Students - PDF Filename UTF-8''Special NCLEX Exam - Jakarta Studentsrizqi100% (1)
- MS ExamDocument7 pagesMS Examjosephine100% (2)
- Maternity Nursing C) The Action of The Doderlein's BacillusDocument11 pagesMaternity Nursing C) The Action of The Doderlein's BacillusLeilah Khan100% (1)
- 10 Diabetes NCLEX QuestionsDocument7 pages10 Diabetes NCLEX QuestionsMar Ordanza100% (6)
- Hematologic Disorders NCLEXDocument15 pagesHematologic Disorders NCLEXPotchiee PfizerNo ratings yet
- Cancer and Oncology Nursing NCLEX Practice Quiz-1Document30 pagesCancer and Oncology Nursing NCLEX Practice Quiz-1Susie Salmon100% (2)
- Med Surg PNLE Exam QuestionsDocument9 pagesMed Surg PNLE Exam Questionsdanielle ordoñezNo ratings yet
- Testmanship - Medical Surgical Nursing Test Taking Strategy-Based June 2009 Nursing Licensure ExaminationDocument16 pagesTestmanship - Medical Surgical Nursing Test Taking Strategy-Based June 2009 Nursing Licensure ExaminationJennine Reyes100% (1)
- CHN and CD Test Questions With RationalesDocument6 pagesCHN and CD Test Questions With RationalesTomzki Cornelio100% (1)
- Maternal & Child Health Nursing Exam 7: NLE Pre-Boards (100 Items)Document35 pagesMaternal & Child Health Nursing Exam 7: NLE Pre-Boards (100 Items)cha mcbNo ratings yet
- Medical Surgical Nursing Questions and Answers With Rationale - Nurses ClassDocument5 pagesMedical Surgical Nursing Questions and Answers With Rationale - Nurses ClassKarren Fernandez100% (2)
- NCLEX Practice Questions - Digestive System 3Document11 pagesNCLEX Practice Questions - Digestive System 3Geevee Naganag VentulaNo ratings yet
- 100 Item MEDICAL SURGICAL Nursing ExaminationDocument18 pages100 Item MEDICAL SURGICAL Nursing ExaminationAijem Ryan100% (1)
- Endocrine NCLEX PN Pract & ANS Questions IIDocument13 pagesEndocrine NCLEX PN Pract & ANS Questions IIYA HONo ratings yet
- Medical Surgical Nursing: Answer: (C) "With A Pillow, Apply Pressure Against The Incision."Document5 pagesMedical Surgical Nursing: Answer: (C) "With A Pillow, Apply Pressure Against The Incision."Jhevilin RMNo ratings yet
- Med Surg Questions Oct 25 Angela DeVarsoDocument38 pagesMed Surg Questions Oct 25 Angela DeVarsonochip10100% (1)
- Fatima Exam QuestionsDocument15 pagesFatima Exam QuestionsPisay Shehannah Grail MedinaNo ratings yet
- Endocrine DisordersDocument28 pagesEndocrine DisordersRhitzle Ann50% (2)
- NP1 Nursing Board Exam June 2008 Answer KeyDocument15 pagesNP1 Nursing Board Exam June 2008 Answer KeyBettina SanchezNo ratings yet
- Nursing Practice 2-5Document47 pagesNursing Practice 2-5Emir Mukhtar Malcampo KamidNo ratings yet
- Nur 151: P1 Examination Part 1: EmailDocument13 pagesNur 151: P1 Examination Part 1: EmailJilkiah Mae Alfoja Campomanes100% (2)
- Set 1Document40 pagesSet 1Dick Morgan FerrerNo ratings yet
- Disaster P1examDocument9 pagesDisaster P1examJushua Opsima RuizNo ratings yet
- Hematologic MS Nclex QuestionsDocument36 pagesHematologic MS Nclex QuestionsSophia Rose Delos Santos100% (2)
- OR Exam July 2019Document4 pagesOR Exam July 2019Maria Sheila Belza100% (4)
- Sas 16Document4 pagesSas 16Sistine Rose Labajo100% (1)
- WatermelonDocument27 pagesWatermelonSunny Mae T PuigNo ratings yet
- Review Practice QuestionsDocument12 pagesReview Practice QuestionsJhannNo ratings yet
- OB DRILLS With RATIO EDITED BLDocument228 pagesOB DRILLS With RATIO EDITED BLJuswa ViasonNo ratings yet
- Commitment. Excellence. Quality. Page 1Document7 pagesCommitment. Excellence. Quality. Page 1Jake CopradeNo ratings yet
- Neuro Senses Onco OrthoDocument11 pagesNeuro Senses Onco OrthoNom NomNo ratings yet
- Psychiatric Nursing - 50 ItemsDocument5 pagesPsychiatric Nursing - 50 Itemsapi-3718174100% (1)
- Nursing Practice Test - EndocrineDocument20 pagesNursing Practice Test - Endocrinemay17sanchez100% (7)
- To Answer - SituationDocument8 pagesTo Answer - SituationMarc Justine Pabia BoralNo ratings yet
- Sas 12Document5 pagesSas 12Sistine Rose LabajoNo ratings yet
- Ha Hahahahahahahahaha HahahahahahahahahaDocument6 pagesHa Hahahahahahahahaha HahahahahahahahahaCassandra LeeNo ratings yet
- Chapter 38 - Management of Patients With Intestinal and Rectal DisordersDocument7 pagesChapter 38 - Management of Patients With Intestinal and Rectal DisordersMichael BoadoNo ratings yet
- Nursing Research POST TEST PNLE 2023 AKDocument14 pagesNursing Research POST TEST PNLE 2023 AKFANER CIENAH MARIENo ratings yet
- Cancer QuizDocument7 pagesCancer QuizJoshua Flores Fernan100% (1)
- Module 49Document2 pagesModule 49Duchess Juliane Jose MirambelNo ratings yet
- NCLEX Practice ExamDocument10 pagesNCLEX Practice ExamJune DumdumayaNo ratings yet
- Community Health Nursing Questions ADocument11 pagesCommunity Health Nursing Questions AFleur Jenne100% (1)
- NCLEX Exam: Respiratory System Disorders (60 Questions) : CorrectDocument41 pagesNCLEX Exam: Respiratory System Disorders (60 Questions) : CorrectErica Veluz LuyunNo ratings yet
- Digestive System Disorder NCLEX Practice QuizDocument7 pagesDigestive System Disorder NCLEX Practice Quizjules100% (1)
- 640-663 ImciDocument25 pages640-663 ImciYaj Cruzada100% (1)
- GI Answer Key Part 1Document5 pagesGI Answer Key Part 1monmon100% (1)
- Neuro QuestionsDocument19 pagesNeuro Questionssarasmith1988100% (6)
- Brooke Cybel TanateDocument5 pagesBrooke Cybel TanateEbenezer Manguerra Diala Gube Jr.No ratings yet
- Hemorragia SubaracnoideaDocument18 pagesHemorragia SubaracnoideaResidencia NeurologíaNo ratings yet
- ACNS Surgical Manual PDFDocument248 pagesACNS Surgical Manual PDFKevin EdroNo ratings yet
- Triple H Therapy in SAHDocument10 pagesTriple H Therapy in SAHMontasir AhmedNo ratings yet
- StrokeDocument74 pagesStrokeDonnaBells Hermo Labaniego100% (2)
- Chapter 257: Head Trauma: Introduction and EpidemiologyDocument35 pagesChapter 257: Head Trauma: Introduction and EpidemiologyIustitia Septuaginta SambenNo ratings yet
- Stroke RehabilitationDocument18 pagesStroke RehabilitationJayricDepalobos100% (4)
- Pathophysiology ErDocument3 pagesPathophysiology ErAlexa A. AldayNo ratings yet
- Cerebrovascular Disease MCQDocument25 pagesCerebrovascular Disease MCQDr. Kishore Kumar Ubrangala85% (13)
- Cerebrospinal Fluid (CSF) AnalysisDocument8 pagesCerebrospinal Fluid (CSF) AnalysisVidhya.MNo ratings yet
- Neuro DisordersDocument159 pagesNeuro DisordersQuolette Constante100% (1)
- Neuro BriefDocument11 pagesNeuro Briefbeyayal338No ratings yet
- Hemorrhagic Stroke CBLDocument106 pagesHemorrhagic Stroke CBLJessica NadiaNo ratings yet
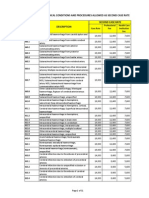
- PhilHealth Circular No. 0035, s.2013 Annex 3 List of Medical Conditions and Procedures Allowed As Second Case RateDocument31 pagesPhilHealth Circular No. 0035, s.2013 Annex 3 List of Medical Conditions and Procedures Allowed As Second Case RateChrysanthus Herrera0% (1)
- CardinalDocument64 pagesCardinalMarc Conrad MolinaNo ratings yet
- Predictor Scale of Delayed Cerebral Ischemic in Aneurysmal Subarachnoid Hemorrhage Case Series: What A Radiologist Should KnowDocument5 pagesPredictor Scale of Delayed Cerebral Ischemic in Aneurysmal Subarachnoid Hemorrhage Case Series: What A Radiologist Should KnowPopy TheresiaNo ratings yet
- Cerebrovascular Accident Introduction Brain Damage Medical SurgicalDocument12 pagesCerebrovascular Accident Introduction Brain Damage Medical SurgicalReymund Timog TalarocNo ratings yet
- Stroke 1Document43 pagesStroke 1n&t3000No ratings yet
- Cerebrovascular AccidentDocument10 pagesCerebrovascular Accidentcarls burg a. resurreccionNo ratings yet
- Etiology and Classification of StrokeDocument10 pagesEtiology and Classification of Strokeaeiou33No ratings yet
- Stroke by Dr. Amit RoyDocument32 pagesStroke by Dr. Amit RoyDr Sutanwi DasNo ratings yet
- Gunn - Pearls and Pitfalls in Emergency Radiology - Variants and Other Difficult DiagnosesDocument387 pagesGunn - Pearls and Pitfalls in Emergency Radiology - Variants and Other Difficult Diagnosesvalentina costrubscaia0% (1)
- Cerebral AneurysmDocument36 pagesCerebral AneurysmHarby Ongbay Abellanosa100% (1)
- The Golden Hour: Acute Ischemic StrokeDocument9 pagesThe Golden Hour: Acute Ischemic StrokeKanliajie Kresna KastiantoNo ratings yet
- NEURODIAGNOSISDocument17 pagesNEURODIAGNOSISRohit kumar Saravana kumarNo ratings yet
- Cross Sectional Imaging Made Easy® PDFDocument207 pagesCross Sectional Imaging Made Easy® PDFsalah subbah100% (2)
- CNS (102 Questions) : Form More Slowly and Insidiously ThanDocument38 pagesCNS (102 Questions) : Form More Slowly and Insidiously Thanclark146No ratings yet
- MnemonicsDocument31 pagesMnemonicspickach100% (3)
- Hemorrhagic StrokeDocument31 pagesHemorrhagic StrokeKaren Mae Dacoco MamuyacNo ratings yet
- Manual of Common Bedside Surgical Procedures-CHAPTER 6 Neurosurgical ProceduresDocument30 pagesManual of Common Bedside Surgical Procedures-CHAPTER 6 Neurosurgical ProceduresCosti TanaseNo ratings yet
- 39 MCQ's in NeurosurgeryDocument26 pages39 MCQ's in NeurosurgeryAhmed Hamid Ibrahim100% (4)