Professional Documents
Culture Documents
Robbins Pathology Chapter 24 - Endocrine
Uploaded by
scorpiosphinx79Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Robbins Pathology Chapter 24 - Endocrine
Uploaded by
scorpiosphinx79Copyright:
Available Formats
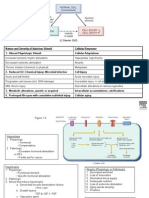
Pathology Chapter 24 Endocrine Thyroid P 1116 Diffuse goiter Endemic iodine deficiency o Goitrogen consumption Sporadic o Female, goitrogens,
gens, hereditary enzymatic defects affecting thyroid hormone synthesis (AR), idiopathic Clinical course: mass effects, normal T3 and T4, high-normal to mildly elevated TSH
Multinodular goiter Sporadic and endemic Caused by recurrent episodes of hyperplasia and involution of long-standing single nodule goiters Arise because of variation in follicular cell response to trophic hormones Clinical course: mass effects, euthyroid or subclinical hyperthyroidism (decreased TSH), uneven iodine uptake o Plummer syndrome: toxic multinodular goiter may develop in long-standing goiter (producing hyperthyroidism) without infiltrative ophthalmopathy and dermopathy
Neoplasms benign:malignant::10:1; Malignancy is more likely in: solitary nodules, younger patients, males, history of radiation, cold nodules; DX by fine-needle aspiration Adenomas o Discrete, solitary masses derived from follicular epithelium, most are non-functional, do not give rise to carcinoma o Somatic mutations of TSH receptor signalling pathway found in toxic adenomas o Hallmark is intact, well-formed capsule (vs multinodular goiters vs follicular carcinomas); Hrthle cells o Clinical course: unilateral painless mass (can cause mass effects), non-functioning adenomas are cold, toxic adenomas are hot; surgically removed, have excellent prognosis and do not recur or metastasize Carcinomas o Papillary: 85%; derived from follicular epithelium; activation of MAPK pathway by RET or NTRK1 rearrangements or activating BRAF mutations; RET/PTC rearrangements more common in tumors with radiation history; BRAF mutations associated with metastatic disease and extra-thyroid extension; increased risk with radiation exposure; solitary or multifocal, psammoma bodies (calcifications) seen, papillary foci point to dx, ground-glass Orphan Annie eye nuclei; first manifestation may be enlarged lymph node, thyroid nodule moves with swallowing, mass effects suggests advanced disease; cold nodules; excellent prognosis (better in pts <40YOA and without extrathyroid extension) o Follicular: 5-15%; derived from follicular epithelium; 1/3-1/2 have mutations in PI-3K/AKT signalling pathway (constant activation); associated with iodine deficiency; single nodules, Hrthle cells present occasionally, do not spread to lymph nodes but may extend into surrounding soft tissue, metastasize to liver, lungs, bone; cold nodules, prognosis depends on stage and extension; tx is thyroidectomy and radioactive iodine (to ID mets), thyroid hormone after surgery o Anaplastic (undifferentiated): <5%; derived from follicular epithelium; arise de novo or by dedifferentiation of a well-differentiated papillary or follicular carcinoma; aggressive (mortality almost 100%); variable morphology (giant cells, spindle cells, mixed spindle and giant); present as rapidly-enlarging neck mass (probably already spread to lungs by time of presentation), symptoms: dysphagia, hoarseness, cough; no effective tx, death w/in 1 yr o Medullary: 5%; familial cancer occurs in MEN2 associated with germline RET mutations (constant activation); neuroendocrine neoplasms derived from parafollicular (C) cells, secrete calcitonin, serotonin, ACTH or VIP; sporadic present as solitary nodules, familial are commonly bilateral and multicentric; sx: mass effects in sporadic sometimes paraneoplastic sx; CEA marker; familial tumor sx: thyroid sx or endocrine tumors of other organs; MEN2B cancers are most aggressive
Congenital anomalies Thyroglossal duct or cyst: midline anterior to trachea, from remnants of tubular development of thyroid, mucinous or clear secretions, high in neck lined by stratified squamous epithelium, low in neck lined by thyroidal acinar epithelium, lymphocytic infiltrate present close to epithelium, infection may result in abscess or cancer
Parathyroid Glands Chief cells with secretory granules containing PTH, oxyphil cells containing mitochondria and glycogen; stromal fat in gland increases with age; activity controlled by free calcium (ionized) in blood (decreased levels stimulate PTH release) PTH: increases renal tubular reabsorption of calcium, increases conversion of vitamin D to active dihydroxy form in kidneys, increases urinary phosphate excretion, augments GI calcium absorption o Elevated levels of PTH cause hypercalcemia; malignancy is most common cause of hypercalcemia (due to increased bone reabsorption both in osteolytic metastases and tumors that have not metastasized to bone that secrete active PTHrP) PTHrP inhibits osteoprotegerin secretion by osteoblastic cells, altering RANKL/osteoprotegerin ratio in favor of osteoclastogenesis
Hyperparathyroidism Primary: autonomous, spontaneous overproduction of PTH due to lesions; associated with skeletal eroisions and kidney stones; can be asymptomatic (pts labs need to be checked periodically) or present with painful bones, renal stones, abdominal groans, and psychic moans, can also have cardiac arryhthmias and neuromuscular abnormalities o Adenoma: 85-95%, affects adult women; most cases are sporadic, familal adenomas are associated with MEN1, MEN2, and familal hypocalciuric hypercalcemia (AD, enhanced parathyroid function due to decreased sensitivity to extracellular calcium due to inactivating mutations in parathyroid calcium-sensing receptor gene (CASR)); most sporadic tumors are monoclonal; sporadic tumor defects: Cyclin D1 gene inversions, MEN1 mutations; adenomas are usually solitary and arise near thyroid glands or in ectopic site (mediastinum); bizarre and pleiomorphic nuclei seen o Primary hyperplasia: 5-10%; usually all 4 glands; usually chief cell hyperplasia o Parathyroid carcinoma: <1%; circumscribed lesions similar to adenomas or invasive; cells appear normal, diagnosis based on local invasion and metastases Secondary: seen in chronic renal insufficiency and with inadequate dietary calcium, steatorrhea, vitamin D deficiency; CRF -> decreased phosphate excretion -> hyperphosphatemia -> depression of serum calcium levels -> stimulation of PTH; CRF -> loss of renal substance -> decreased -1-hydroxylase -> decreased vitamin D activation -> decreases intestinal absorption of calcium; vitamin D has suppressive effects on parathyroid growth and PTH secretion; parathyroid glands are hyperplastic (more chief cells, less fat cells); renal osteodystrophy (bone lesions); metastatic calcification of heart, lungs, stomach, blood vessels (calcifylaxis); tx with vitamin D and phosphate binders Tertiary: parathyroid activity becomes autonomous and excessive with resultant hypercalcemia; tx is parathyroidectomy
Hypoparathyroidism Causes: o Usually due to inadvertent damage to parathyroids during thyroid surgery o Autoimmune hypoparathyroidism: associated with chronic mucocutaneous candidiasis and primary adrenal insufficiency (autoimmune polyendocrine syndrome type 1 (APS1)) caused by mutations in AIRE gene o Autosomal dominant hypoparathyroidism: caused by gain-of-function mutation of calcium-sensing receptor (CASR) gene which cause suppression of PTH -> hypocalcemia and hypercalciuria o Familal isolated hypoparathyroidism: AD mutation in PTH precursor peptide gene which impairs processing of mature hormone; AR loss of function mutation in glial cells missing-2 (GCM-2) transcription factor gene, essential for parathyroid gland development o Congenital absence of parathyroid glands: 22q11 deletion syndrome (DiGeorge) Clinical manifestations: o Tetany (neuromuscular irritability), paresthesias, carpopedal spasm, laryngospasm, generalized seizures; Chvostek sign, Trousseau sign; Mental status changes; Intracranial manifestations; ocular calcifications; cardiovascular manifestations (prolonged QT interval); dental abnormalities (hypoplasia, etc)
Pseudohyperparathyroidism: end organ resistance to actions of PTH; PTH is normal or elevated, hypocalcemia, hyperphosphatemia Albrights hereditary osteodystrophy: AD kidney unresponsiveness to PTH One form with multi-organ hormone resistance due to genetic defects in G protein second messenger signalling pathway; THS and FSH/LH resistance
You might also like
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Systemic Lupus Erythematosus: Basic, Applied and Clinical AspectsFrom EverandSystemic Lupus Erythematosus: Basic, Applied and Clinical AspectsGeorge C. TsokosNo ratings yet
- Patho4-6 - Liver (Dr. Dy)Document13 pagesPatho4-6 - Liver (Dr. Dy)miguel cuevas100% (1)
- Patho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Document12 pagesPatho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Grant GarcesNo ratings yet
- Pathology Cell InjuryDocument57 pagesPathology Cell InjuryMajd MustafaNo ratings yet
- Robbin's SummariesDocument98 pagesRobbin's SummariesnopedontsuemepleaseNo ratings yet
- Endocrine PathologyDocument13 pagesEndocrine Pathologysarguss14100% (1)
- GI PathologyDocument22 pagesGI Pathologyzeroun24100% (5)
- GASTROINSTINAL TRACT Robbins 8th EditionDocument4 pagesGASTROINSTINAL TRACT Robbins 8th EditionLim EricNo ratings yet
- Renal Pathology Lectures - PPT SeriesDocument267 pagesRenal Pathology Lectures - PPT SeriesMarc Imhotep Cray, M.D.100% (12)
- Endocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologyDocument3 pagesEndocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologySamuelNo ratings yet
- Endocrine System - Part 1 (Robbins)Document28 pagesEndocrine System - Part 1 (Robbins)sarguss14100% (2)
- Inflammation and Repair OverviewDocument10 pagesInflammation and Repair OverviewMiguel Cuevas DolotNo ratings yet
- Endocrine Pathology p17-32Document16 pagesEndocrine Pathology p17-32zeroun24No ratings yet
- General Pathology Bimonthly Exam Compilation Updated 2Document197 pagesGeneral Pathology Bimonthly Exam Compilation Updated 2Cherry Rahima100% (1)
- Cell Injury & AdaptationDocument22 pagesCell Injury & AdaptationUmam LoyalNo ratings yet
- Pathology of Liver, Biliary, and PancreasDocument52 pagesPathology of Liver, Biliary, and PancreasHassan.shehri100% (11)
- Robbins Ch. 20 The Kidney Review QuestionsDocument10 pagesRobbins Ch. 20 The Kidney Review QuestionsPA2014100% (4)
- Robbins Ch. 26 Bones Joints and Soft-Tissue Tumors Review QuestionsDocument7 pagesRobbins Ch. 26 Bones Joints and Soft-Tissue Tumors Review QuestionsPA2014100% (1)
- Top 100 Pathology Secrets List W/ NotesDocument6 pagesTop 100 Pathology Secrets List W/ NotesPA2014100% (4)
- Chapter 11 Blood Vessels 8th Ed NotesDocument7 pagesChapter 11 Blood Vessels 8th Ed NotesKyle Christopher SiaNo ratings yet
- Cellular Injury, Adaptation and Cell DeathDocument8 pagesCellular Injury, Adaptation and Cell DeathJessica Febrina Wuisan100% (1)
- Hemodynamic Disorders, Thromboembolic Disease, and ShockDocument87 pagesHemodynamic Disorders, Thromboembolic Disease, and Shockgifty100% (1)
- Genetic and Pediatric Diseases Chapter SummaryDocument16 pagesGenetic and Pediatric Diseases Chapter SummaryJustine HungNo ratings yet
- Chapter 5 (Questions 2008-2009 Compiled)Document28 pagesChapter 5 (Questions 2008-2009 Compiled)vetpathforumNo ratings yet
- Chapter 10 - Diseases of Infancy and ChildhoodDocument17 pagesChapter 10 - Diseases of Infancy and ChildhoodAgnieszka WisniewskaNo ratings yet
- Endocrine PathologyDocument31 pagesEndocrine PathologyAnonymous 49jFPGI5KN100% (1)
- Cardiac Physiology & Pathology TopicsDocument3 pagesCardiac Physiology & Pathology TopicsByeongsu Park100% (1)
- Patho - Inflammation SummaryDocument28 pagesPatho - Inflammation SummaryTep Gonzales71% (7)
- Robbins and Cotran's Pathologic Basis of Disease Chapter 1Document14 pagesRobbins and Cotran's Pathologic Basis of Disease Chapter 1Mon Dominguez100% (2)
- Acute Inflammation - Robbins Basic Pathology - Inflammation & RepairDocument24 pagesAcute Inflammation - Robbins Basic Pathology - Inflammation & RepairLuis Adrian De Jesús100% (9)
- Robbins Questions Chp1-10Document28 pagesRobbins Questions Chp1-10verbatimmt100% (1)
- Ch.1 Baby Robbins OutlineDocument11 pagesCh.1 Baby Robbins OutlinePA2014100% (3)
- Robbins Basic Pathology 9th Edition QBankDocument4 pagesRobbins Basic Pathology 9th Edition QBankVarshini Tamil SelvanNo ratings yet
- SURGPATH - 2.1 The Gastrointestinal Tract (Robbins) - TableDocument8 pagesSURGPATH - 2.1 The Gastrointestinal Tract (Robbins) - TableAngela Caguitla100% (1)
- P.G. Curriculum M.D. Pathology Index: 1. GoalDocument18 pagesP.G. Curriculum M.D. Pathology Index: 1. GoalAvwan DududNo ratings yet
- Liver - RobbinsDocument25 pagesLiver - Robbinssarguss14100% (2)
- WBC Pathology: Lecturer: Associate Professor T. A. GrekovaDocument49 pagesWBC Pathology: Lecturer: Associate Professor T. A. GrekovaFaheem MusthafaNo ratings yet
- DB13 - Pathophysiology of AtherosclerosisDocument2 pagesDB13 - Pathophysiology of Atherosclerosisi_vhie03No ratings yet
- Renal Vascular Disease GuideDocument46 pagesRenal Vascular Disease GuideCoy NuñezNo ratings yet
- Pancreatic Hormones and Antidiabetic AgentsDocument3 pagesPancreatic Hormones and Antidiabetic AgentsChristian DeeNo ratings yet
- CardiacArrhythmiasPathophysiology PDFDocument1 pageCardiacArrhythmiasPathophysiology PDFNeelam Raj ThakurNo ratings yet
- Hyperthyroidism: DR Rajeshwar ReddyDocument59 pagesHyperthyroidism: DR Rajeshwar ReddyRajeshwarreddy RamaswamyNo ratings yet
- Introduction to Pathology: Study of Disease at the Cellular LevelDocument44 pagesIntroduction to Pathology: Study of Disease at the Cellular Level53-Deepankar SutradharNo ratings yet
- Chapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFDocument9 pagesChapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFChethranNo ratings yet
- Thyroid Gland DisordersDocument64 pagesThyroid Gland DisordersFaisal RavifNo ratings yet
- Pathology GlomerulonephritisDocument4 pagesPathology GlomerulonephritisGerardLum100% (2)
- Anca VasculitisDocument12 pagesAnca Vasculitisatul_desai_3100% (2)
- Robbins Pathology Chapter 13 - White Blood CellsDocument7 pagesRobbins Pathology Chapter 13 - White Blood Cellsscorpiosphinx7980% (5)
- EBM - 5. Adrenal DisordersDocument101 pagesEBM - 5. Adrenal DisordersBRI KUNo ratings yet
- Robbins Pathology Chapter 14 - RBCsDocument7 pagesRobbins Pathology Chapter 14 - RBCsscorpiosphinx79100% (10)
- Gastrointestinal PathologyDocument14 pagesGastrointestinal PathologyRahul ShuklaNo ratings yet
- Cell Injury and Cell DeathDocument35 pagesCell Injury and Cell DeathMarc Imhotep Cray, M.D.No ratings yet
- Robbin's Chapter 20 Kidney PathologyDocument4 pagesRobbin's Chapter 20 Kidney Pathologynbaumgartner0100% (1)
- Git PathologyDocument113 pagesGit PathologyanggitaNo ratings yet
- Causes, Types and Morphology of Cell Injury and DeathDocument18 pagesCauses, Types and Morphology of Cell Injury and DeathYoja GarzonNo ratings yet
- Liver PathologyDocument21 pagesLiver Pathologyzeroun24100% (6)
- Skin Summary ChartDocument7 pagesSkin Summary ChartMarco HernandezNo ratings yet
- Conn Syndrome, (Hyper-Aldosteronism) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandConn Syndrome, (Hyper-Aldosteronism) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- DIT Study GuideDocument10 pagesDIT Study Guideaagarwalmd0% (1)
- Robbins Pathology Chapter 13 - White Blood CellsDocument7 pagesRobbins Pathology Chapter 13 - White Blood Cellsscorpiosphinx7980% (5)
- Robbins Pathology Chapter 17 Liver and Biliary TractDocument2 pagesRobbins Pathology Chapter 17 Liver and Biliary Tractscorpiosphinx79No ratings yet
- Robbins Pathology Chapter 14 - RBCsDocument7 pagesRobbins Pathology Chapter 14 - RBCsscorpiosphinx79100% (10)
- READING PRACTICE TEST 3Document9 pagesREADING PRACTICE TEST 3Cao Son Dang Vu0% (1)
- Application of Fascial Manipulation Technique in Chronic Shoulder PainDocument9 pagesApplication of Fascial Manipulation Technique in Chronic Shoulder PainIsabelGuijarroMartinez100% (1)
- I. Objectives A. Content Standards: Monday Tuesday Wednesday Thursday FridayDocument8 pagesI. Objectives A. Content Standards: Monday Tuesday Wednesday Thursday FridayMaribel NayadNo ratings yet
- Yoga Class 12Document13 pagesYoga Class 12Vandan KNo ratings yet
- Exploring Creation With Advanced Biology 2 Edition - Errata: Textbook - 1 and 2 PrintingsDocument2 pagesExploring Creation With Advanced Biology 2 Edition - Errata: Textbook - 1 and 2 PrintingsJacquie ScholeNo ratings yet
- Hormone Practice Test: StudentDocument17 pagesHormone Practice Test: StudentKayne SuratosNo ratings yet
- Components of Blood - Red Blood Cells, White Blood Cells, and PlateletsDocument20 pagesComponents of Blood - Red Blood Cells, White Blood Cells, and PlateletsVishal SharmaNo ratings yet
- CNS Development and OrganizationDocument6 pagesCNS Development and OrganizationKhamron BridgewaterNo ratings yet
- How Do We Take Care of Our Endocrine SystemDocument7 pagesHow Do We Take Care of Our Endocrine SystemAndrei CunananNo ratings yet
- Hemato OnologyDocument60 pagesHemato OnologyGousayAlkhazmariNo ratings yet
- Surface Anatomy: de La Salle-Lipa College of LawDocument79 pagesSurface Anatomy: de La Salle-Lipa College of LawFatzie MendozaNo ratings yet
- Alveolar BoneDocument24 pagesAlveolar BoneHanna SouthwellNo ratings yet
- Anatomicallandmarksofdenturebearingareaof 130812025925 Phpapp02Document48 pagesAnatomicallandmarksofdenturebearingareaof 130812025925 Phpapp02AnimeAngelNo ratings yet
- Hema - Cytochemistry With TablesDocument4 pagesHema - Cytochemistry With TablesAce TardoNo ratings yet
- Hemostasis and Platelet FunctionDocument17 pagesHemostasis and Platelet FunctionUzama Binu AliNo ratings yet
- Digestive System Part 2 Large Intestine Water and Mineral AbsorptionDocument16 pagesDigestive System Part 2 Large Intestine Water and Mineral AbsorptionFhayee Sulaik HaronNo ratings yet
- Reproductive Health Guide Matches Key PartsDocument2 pagesReproductive Health Guide Matches Key Partsalan patinoNo ratings yet
- Blok 10 03.11.2017Document174 pagesBlok 10 03.11.2017VaniaNo ratings yet
- Hydatidosis: A Mystery Box at Various SitesDocument7 pagesHydatidosis: A Mystery Box at Various SitesIJAR JOURNALNo ratings yet
- Chapter 7 CELL STRUCTURE AND FUNCTION PDFDocument16 pagesChapter 7 CELL STRUCTURE AND FUNCTION PDFAngelene PelayoNo ratings yet
- Bradycardia & TachycardiaDocument14 pagesBradycardia & TachycardiaHendri SaputraNo ratings yet
- PAS Stain Procedure and Fixatives in HistochemistryDocument18 pagesPAS Stain Procedure and Fixatives in HistochemistryParveen AkhtarNo ratings yet
- Uddin Et Al., 2022Document4 pagesUddin Et Al., 2022James BondNo ratings yet
- Materi Digestive SystemDocument13 pagesMateri Digestive Systembetta putriNo ratings yet
- Mythic18 Alarms ExplanationDocument4 pagesMythic18 Alarms ExplanationNelsonNo ratings yet
- PhysiologyDocument5 pagesPhysiologyCpopNo ratings yet
- Understanding Hypothyroidism: Causes, Symptoms and TreatmentDocument14 pagesUnderstanding Hypothyroidism: Causes, Symptoms and TreatmentMari IllustriousNo ratings yet
- Primary Abdominal Ectopic Pregnancy: A Case ReportDocument4 pagesPrimary Abdominal Ectopic Pregnancy: A Case ReportYared TJNo ratings yet
- Science Quest 8 AC 3E c04 PDFDocument94 pagesScience Quest 8 AC 3E c04 PDFmaxx100% (1)
- Chapter No. 3 4 Gerontological NursingDocument110 pagesChapter No. 3 4 Gerontological NursingHerman ZoletaNo ratings yet