Professional Documents
Culture Documents
Impaired Gas Exchange R/T Ventilation-Perfusion Imbalance Care Plan
Uploaded by
Cristina CenturionOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Impaired Gas Exchange R/T Ventilation-Perfusion Imbalance Care Plan
Uploaded by
Cristina CenturionCopyright:
Available Formats
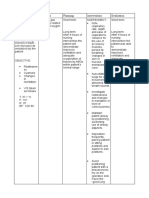
Assessment Data for Nursing Diagnosis Subjective: Mom says the child has been breathing with difficulty
and very fast. In addition he became very agitated and distressed when walking to the bathroom according with Moms statement. Objective:
Nursing Diagnosis Collaborative Problems
Expected Outcomes with Indicators Short Term: The client will demonstrate improved ventilation, adequate oxygenation and will be free of respiratory distress when walking by the end of the shift.
Nursing Intervention 1-Monitor respiratory rate, depth , and effort, including use of accessory muscles, nasal flaring and abnormal breathing patterns. 2- Auscultate breath sounds every 1-2 hrs or prn and be alert for crackles and wheezes that could indicate airway obstruction and increase the difficult breathing. 3- Monitor oxygen saturation continuously using pulse oximetry. Monitor ABGs labs values if available and chest X-rays 4- Position the client in semi-Fowlers position, with an upright posture at 45 degrees if possible.
Scientific Rationale Increased respiratory rate, use of accessory muscles, nasal flaring, abdominal breathing, and a look of panic in the clients eyes may be seen with hypoxia. (Ackley, 2006, p.558) In severe exacerbations, lungs sounds may be diminished or distant with air trapping. (Ackley, 2006, p.558)
1- Impaired gas exchange r/t ventilationperfusion imbalance AEB diminished PsO2 readings and SOB.
Evaluation/Effectiveness of Nursing Intervention The respiratory rate increased in relation with previous measurement to 25 respirations per minute. It is necessary to continue being monitored this vital sign. The expiratory wheezing detected earlier wasnt present when examined at the end of the shift. It needs to continue monitoring for a possible return. Saturation of O2 improved from 91% to 93% during shift, but it needs to reach more reassuring levels.
-PR: 112 at rest (Normal PR 70-110 at rest) - Increased heart rate when walking to bathroom: HR= 186 and distress - Increased RR: 25 ( Normal17-21) -S02: 91% (at 10 AM)-room air 93% (at 3 PM)- room air - Chest X-ray (11-042012): multiple small patches of atelectasis bilaterally. No consolidation. - Decreased breath sounds at the bases bilateral. - Expiratory wheezing in right upper/medium lobes - Substernal retraction. Long Term: The child and family will implement a daily treatment plan for asthma and reduce the number of asthma episodes, as long as possible (and doing so avoiding hospital admissions) by 1 month.
An oxygen saturation of less than 90% (normal: 95 to 100%) indicates significant oxygenation problems. (Ackley, 2006, p.558) Research done on clients on a ventilator demonstrated that being in a 45 degree upright position increased oxygenation and ventilation. Research on healthy subjects demonstrated that sitting upright resulted in higher tidal volumes and minute ventilation versus sitting in a slumped posture. (Ackley, 2006, p.558) Oxygen has been shown to correct hypoxemia , which can be caused by retained secretions). (Ackley, 2006, p.167) The goal of inpatient oxygen therapy for a client with asthma is to keep an oxygen greater than 95% to maintain cellular oxygenation. (Ackley, 2006,
The client while on bed was positioned in semi-Fowlers position, and he manifested being comfortable and breathing better in comparison to a lower position on the bed.
5- Administer and assess response to oxygen for respiratory distress. Provide humidified oxygen through an appropriate device ( nasal canula or Venturi mask per physician order).
The client needed to use oxygen once during shift because his SOB. When he walks outside of his room he carries his O2 thank. His SOB needs to continue being monitored and continue providing O2 as necessary.
p.558)
You might also like
- Impaired Gas ExchangeDocument2 pagesImpaired Gas ExchangeHanya Bint PotawanNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanAdreanah Martin RañisesNo ratings yet
- Nursing Care PlanDocument10 pagesNursing Care PlanElijah S GomezNo ratings yet
- Impaired Gas ExchangeDocument5 pagesImpaired Gas ExchangeKM67% (3)
- NCP - Impaired Gas ExchangeDocument4 pagesNCP - Impaired Gas ExchangeRene John Francisco100% (1)
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDocument2 pagesNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- Ineffective Breathing PatternDocument8 pagesIneffective Breathing PatternJansen Arquilita Rivera100% (2)
- Assessing Impaired Gas ExchangeDocument1 pageAssessing Impaired Gas ExchangeRryje Salleva100% (1)
- Assessment Diagnosis Planning Intervention Evaluation for Impaired Gas ExchangeDocument2 pagesAssessment Diagnosis Planning Intervention Evaluation for Impaired Gas ExchangeCharissa Magistrado De LeonNo ratings yet
- Impaired Gas Exchange-Sample NCPDocument1 pageImpaired Gas Exchange-Sample NCPKaycee BinanNo ratings yet
- Ineffective Breathing Pattern Related To Bronchospasm, Decreased Lung ExpansionDocument2 pagesIneffective Breathing Pattern Related To Bronchospasm, Decreased Lung ExpansionReylan Garcia43% (7)
- NCP - Impaired Gas ExchangeDocument2 pagesNCP - Impaired Gas Exchangejanelee2824No ratings yet
- Asthma Impaired Gas ExchangeDocument2 pagesAsthma Impaired Gas ExchangeNedeve Ozned100% (5)
- Ncp-Ineffective Airway ClearanceDocument3 pagesNcp-Ineffective Airway Clearancelouanne0550% (2)
- Acute Respiratory DistressDocument2 pagesAcute Respiratory Distressminaanne100% (3)
- NCP For Ineffective Breathing Pattern - RMC CasepressDocument2 pagesNCP For Ineffective Breathing Pattern - RMC Casepressmissyuri08No ratings yet
- NCP Impaired Gas ExchangeDocument2 pagesNCP Impaired Gas ExchangeCharissa Magistrado De LeonNo ratings yet
- Pneumonia-Ineffective Airway ClearanceDocument2 pagesPneumonia-Ineffective Airway ClearanceNursesLabs.com86% (7)
- Nursing Interventions for PneumoniaDocument2 pagesNursing Interventions for PneumoniaGabriel Tolentino70% (10)
- NCP Impaired Gas Exhange CHEST INJURYDocument4 pagesNCP Impaired Gas Exhange CHEST INJURYMa. Elaine Carla Tating100% (2)
- Asthma Risk For Activity IntoleranceDocument1 pageAsthma Risk For Activity IntoleranceWdy Tanakht Sparrow100% (4)
- NCP Ineffective Breathing Pattern TalaDocument1 pageNCP Ineffective Breathing Pattern TalaJhen Bitco Fidel70% (10)
- NCP Ineffective Airway ClearanceDocument4 pagesNCP Ineffective Airway ClearanceMary Joyce Limoico100% (1)
- Nursing Diagnosis and Interventions for Impaired Gas Exchange and Ineffective Airway ClearanceDocument4 pagesNursing Diagnosis and Interventions for Impaired Gas Exchange and Ineffective Airway ClearanceKen Simon100% (1)
- Student Nurses’ Community NURSING CARE PLAN – Renal FailureDocument2 pagesStudent Nurses’ Community NURSING CARE PLAN – Renal FailureAldrein GonzalesNo ratings yet
- POC Ineffective Breathing PatternDocument1 pagePOC Ineffective Breathing PatterncuicuitaNo ratings yet
- Respiratory Failure NCPDocument1 pageRespiratory Failure NCPkyaw100% (1)
- Improving Physical Mobility Through Nursing InterventionsDocument2 pagesImproving Physical Mobility Through Nursing InterventionsPrincess Averin Navarro50% (2)
- Ineffective Airway Clearance (Retained Secretions)Document1 pageIneffective Airway Clearance (Retained Secretions)Danna Tan50% (2)
- NCP - Ineffective Airway ClearanceDocument2 pagesNCP - Ineffective Airway Clearancelarapatricia1215No ratings yet
- NCP Ineffective Airway ClearanceDocument5 pagesNCP Ineffective Airway ClearanceArt Christian Ramos100% (1)
- Ineffective Airway Clearance Related To BronchospasmDocument2 pagesIneffective Airway Clearance Related To BronchospasmReylan Garcia100% (4)
- Impaired Gas Exchange NCPDocument1 pageImpaired Gas Exchange NCPCj AlconabaNo ratings yet
- Nursing Care Plan Impaired Gas ExchangeDocument1 pageNursing Care Plan Impaired Gas Exchangecuicuita100% (3)
- Nursing Diagnosis Nursing Intervention Rationale: Prioritized Nursing Problem For AtelectasisDocument2 pagesNursing Diagnosis Nursing Intervention Rationale: Prioritized Nursing Problem For AtelectasisFatima Zainab Matlih IdjiraniNo ratings yet
- NCP Impaired Gas ExchangeDocument1 pageNCP Impaired Gas ExchangeLaidy Aizahlyn Indoc Angod0% (3)
- Ineffective Breathing Pattern Pneumonia Nursing Care PlanDocument1 pageIneffective Breathing Pattern Pneumonia Nursing Care PlanJasonlee BaluyotNo ratings yet
- Assessing and Managing Respiratory DistressDocument3 pagesAssessing and Managing Respiratory DistressGen RodriguezNo ratings yet
- Nursing Care Plan for Activity IntoleranceDocument3 pagesNursing Care Plan for Activity Intolerancelouie roderos0% (1)
- Nursing Care Plan - Impaired Gas ExchangeDocument3 pagesNursing Care Plan - Impaired Gas ExchangeYum C86% (65)
- Nursing Care Plan 6 Impaired Gas ExchangeDocument9 pagesNursing Care Plan 6 Impaired Gas Exchangedbryant0101100% (12)
- 6 Pleural Effusion Nursing Care PlansDocument7 pages6 Pleural Effusion Nursing Care PlansShaina Fe RabaneraNo ratings yet
- NCP (Deficient Fluid VolumeDocument3 pagesNCP (Deficient Fluid VolumeNica RespondoNo ratings yet
- Assessing and Managing Ineffective Airway ClearanceDocument3 pagesAssessing and Managing Ineffective Airway ClearanceNelle Agni100% (1)
- NCPDocument6 pagesNCPKyla Carbonel100% (1)
- Nursing Care PlanDocument13 pagesNursing Care PlanCris Solis33% (3)
- NCP For CTTDocument1 pageNCP For CTTJen Rhae LimNo ratings yet
- NCP CR Impaired Spontaneous VentilationDocument8 pagesNCP CR Impaired Spontaneous VentilationJosett Romano75% (4)
- NCP For CTTDocument2 pagesNCP For CTTKay D. BeredoNo ratings yet
- Wk2 NCP Edited2012Document6 pagesWk2 NCP Edited2012Jessely Caling SalasNo ratings yet
- NCP SDocument8 pagesNCP SMarvie CadenaNo ratings yet
- TUGAS Bahasa InggrisDocument8 pagesTUGAS Bahasa InggrissantiNo ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway Clearanceapi-252726911No ratings yet
- Pneumonia Care PlanDocument3 pagesPneumonia Care PlanLeah MillerNo ratings yet
- NCP Ineffective Gas ExchangeDocument2 pagesNCP Ineffective Gas ExchangeRez ApegoNo ratings yet
- Oxygen Therapy in NeonatesDocument40 pagesOxygen Therapy in Neonatesindiamahesh100% (4)
- 2 NCPDocument2 pages2 NCPJohn CenasNo ratings yet
- OxygenationDocument19 pagesOxygenationdlneisha61100% (3)
- Canadian Fundamentals of Nursing 5th Edition Potter Solutions ManualDocument35 pagesCanadian Fundamentals of Nursing 5th Edition Potter Solutions Manualaliasfranklawxexb3x100% (14)
- NCP Ineffective Gas ExchangeDocument2 pagesNCP Ineffective Gas ExchangeRez ApegoNo ratings yet
- Brother Manual Kh950iDocument199 pagesBrother Manual Kh950iCristina CenturionNo ratings yet
- Nclex MedicationsDocument39 pagesNclex MedicationsCristina Centurion100% (2)
- Emergency DrugsDocument2 pagesEmergency DrugsCristina CenturionNo ratings yet
- Anxiety Class & Copy11-2Document33 pagesAnxiety Class & Copy11-2Cristina CenturionNo ratings yet
- Chair ExercisesDocument5 pagesChair ExercisesCristina CenturionNo ratings yet
- Cranial Nerves Assessment FormDocument3 pagesCranial Nerves Assessment FormCristina CenturionNo ratings yet
- Mood Disorders Class & Copy 11-1Document43 pagesMood Disorders Class & Copy 11-1Cristina CenturionNo ratings yet
- Nclex Made Incredible Easy - Cardio AnswersDocument16 pagesNclex Made Incredible Easy - Cardio AnswersCristina CenturionNo ratings yet
- Sociology: Chapter 1Document4 pagesSociology: Chapter 1Cristina CenturionNo ratings yet
- Thyroid StormDocument6 pagesThyroid StormCristina CenturionNo ratings yet
- Nclex TermsDocument48 pagesNclex TermsCristina Centurion100% (2)
- Ethical Dilemmas in Nursing - Code GrayDocument24 pagesEthical Dilemmas in Nursing - Code GrayCristina Centurion100% (1)
- Pharmacology OverviewDocument33 pagesPharmacology OverviewCristina CenturionNo ratings yet
- Neurological Stressors III Chronic Neurological Disorders: Joy Borrero, RN, MSN and NUR240 Nursing StudentsDocument38 pagesNeurological Stressors III Chronic Neurological Disorders: Joy Borrero, RN, MSN and NUR240 Nursing StudentsCristina CenturionNo ratings yet
- Sociology 1Document19 pagesSociology 1Cristina CenturionNo ratings yet
- Substance Abuse QuestionsDocument3 pagesSubstance Abuse QuestionsCristina CenturionNo ratings yet
- Cardiac DrugsDocument35 pagesCardiac DrugsCristina Centurion100% (3)
- Child Abuse and NeglectDocument1 pageChild Abuse and NeglectCristina CenturionNo ratings yet
- Asthma Article CareplanDocument2 pagesAsthma Article CareplanCristina CenturionNo ratings yet
- Sociology: Chapter 1Document4 pagesSociology: Chapter 1Cristina CenturionNo ratings yet
- Sociology: Chapter 1Document4 pagesSociology: Chapter 1Cristina CenturionNo ratings yet
- Substance Abuse NclexDocument4 pagesSubstance Abuse NclexCristina Centurion100% (3)
- NCPDocument2 pagesNCPKrizia TepootNo ratings yet
- Assessment of Respiratory FunctionDocument4 pagesAssessment of Respiratory FunctionCristine Dominique E. DonaireNo ratings yet
- Go Back To The Roots With Namhya ProjectDocument19 pagesGo Back To The Roots With Namhya ProjectAnkit Sinha100% (1)
- PneumothoraxDocument52 pagesPneumothoraxtrisna satrianaNo ratings yet
- Physical Examination CopdDocument3 pagesPhysical Examination CopdOM BAWNENo ratings yet
- Cronic Heart Failure - EscDocument55 pagesCronic Heart Failure - EscRisti Graharti100% (1)
- Symptoms Differential ChartsDocument52 pagesSymptoms Differential ChartsXiaxin Liu100% (2)
- Pregnancy Induced HypertensionDocument12 pagesPregnancy Induced Hypertensionnursereview100% (9)
- Efficacy of Pursed-Lips Breathing: A Breathing Pattern Retraining Strategy For Dyspnea ReductionDocument8 pagesEfficacy of Pursed-Lips Breathing: A Breathing Pattern Retraining Strategy For Dyspnea ReductionGaoudam NatarajanNo ratings yet
- Seminar On Bronchial Asthma NewDocument42 pagesSeminar On Bronchial Asthma NewShabna SameerNo ratings yet
- History Taking Checklist.Document4 pagesHistory Taking Checklist.لو ترىNo ratings yet
- Final Case Presentation Unstable AnginaDocument28 pagesFinal Case Presentation Unstable AnginaZendy Nicole Cano SaavedraNo ratings yet
- CDC - Ventilator-Associated Pneumonia (VAP) EventDocument13 pagesCDC - Ventilator-Associated Pneumonia (VAP) EventAl MuzakkiNo ratings yet
- Pulmonary Rehabilitation (S)Document79 pagesPulmonary Rehabilitation (S)liz100% (3)
- COPD Guide: Causes, Symptoms and TreatmentDocument30 pagesCOPD Guide: Causes, Symptoms and TreatmentMoses Jr KazevuNo ratings yet
- Jurnal Gawat DaruratDocument7 pagesJurnal Gawat DaruratFirzhan FharezNo ratings yet
- Pediatric Mock Resuscitation ScenariosDocument6 pagesPediatric Mock Resuscitation ScenariosdinkytinkNo ratings yet
- Master Dentistry2Document275 pagesMaster Dentistry2Isak Shatika0% (1)
- Asthma in Children CMEDocument37 pagesAsthma in Children CMEGideon K. MutaiNo ratings yet
- Efficacy and Tolerability of A Fluid Extract Combination of Thyme Herb and Ivy Leaves and Matched Placebo in Adults Suffering From Acute Bronchitis With Productive Cough PDFDocument9 pagesEfficacy and Tolerability of A Fluid Extract Combination of Thyme Herb and Ivy Leaves and Matched Placebo in Adults Suffering From Acute Bronchitis With Productive Cough PDFvitor_chenNo ratings yet
- Msds of LiOHDocument6 pagesMsds of LiOHmunawar786No ratings yet
- Side Effects of VancomycinDocument20 pagesSide Effects of VancomycinSiti Hajar Mohd ZaidiNo ratings yet
- Complications in Treatment of LYMEDocument131 pagesComplications in Treatment of LYMECharles Mitchell100% (1)
- MCI FMGE Question Paper 2007Document0 pagesMCI FMGE Question Paper 2007Sharat ChandraNo ratings yet
- Handbook of Systemic Treatments For Cancer - 8th EditionDocument186 pagesHandbook of Systemic Treatments For Cancer - 8th EditionLaurențiu Acostioaei67% (3)
- General Medicine and Surgery For Dental Practitioners - Part 1. History Taking and Examination of The Clothed PatientDocument4 pagesGeneral Medicine and Surgery For Dental Practitioners - Part 1. History Taking and Examination of The Clothed Patientanees jamalNo ratings yet
- Respiratory Disorders: Parainfluenza, RSV, RhinovirusDocument5 pagesRespiratory Disorders: Parainfluenza, RSV, RhinovirusSoojung Nam100% (1)
- Respiratory Comp: Nursing DiagnosisDocument1 pageRespiratory Comp: Nursing DiagnosisMaria Francheska OsiNo ratings yet
- Oxygen InsuffiencyDocument21 pagesOxygen InsuffiencyAntony Raj Culandai Swamy100% (1)
- Management of Dyspnea in Advanced Cancer - ASCO GuidelineDocument25 pagesManagement of Dyspnea in Advanced Cancer - ASCO GuidelineThaísa NogueiraNo ratings yet