Professional Documents
Culture Documents
Emergency Management of Patients With Drug Overdose
Uploaded by
theglobalnursingOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Emergency Management of Patients With Drug Overdose
Uploaded by
theglobalnursingCopyright:
Available Formats
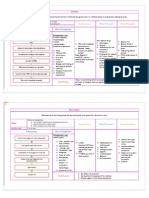
EMERGENCY MANAGEMENT OF PATIENTS WITH DRUG OVERDOSE
Drug
Stimulants Cocaine Intranasally (snorting): inhaled into nostrils through straws By smoking (freebasing): cocaine hydrochloride dissolved in ether to yield a pure cocaine alkaloid base (called crack, rocks); smoking in a small pipe delivers large quantities of cocaine to lungs Intravenously Polysubstance (cocaine and heroin)
Clinical Manifestations
Cocaine is a central nervous system (CNS) stimulant that can increase heart rate and blood pressure and cause hyperpyrexia, seizures, increased energy, agitation, aggression, and ventricular dysrhythmias. It produces intense euphoria, then anxiety, sadness,insomnia, and sexual indifference;cocaine hallucinations with delusions; psychosis with extreme paranoia and ideas of persecution; and hypervigilance. Chronic psychotic symptoms may persist. Overall psychotic symptoms are short-lived compared to methamphetamines
Therapeutic Management
1. Maintain airway and provide respiratory support 2. Control seizures. 3. Monitor cardiovascular effects; have lidocaine and debrillator available. 4. Treat for hyperthermia. 5. If cocaine was ingested, evacuate stomach contents and use activated charcoal to treat. Whole bowel irrigation may be necessary to treat body packers (mules). 6. Refer for psychiatric evaluation and treatment in an inpatient unit that eliminates access to the drug. Include drug rehabilitation counseling.
Opioids Heroin Opium or paregoric Morphine, codeine, semisynthetic derivatives: oxycodone (OxyContin), methadone, meperidine (Demerol), propoxyphene (Darvon), tramadol (Ultram), fentanyl (Sublimaze)
Acute intoxication (overdose) Pinpoint pupils (may be dilated with severe hypoxia); decreased blood pressure Marked respiratory depression/ arrest Pulmonary edema Stupor Scoma Seizures Fresh needle marks along course of any supercial vein; skin abscesses
1. Support respiratory and cardiovascular functions. 2. Establish an intravenous (IV) line; obtain blood for chemical and toxicologic analysis. Patient may be given bolus of glucose To eliminate possibility of hypoglycemia. 3. Give narcotic antagonist (naloxone hydrochloride IV, IM [Narcan]) as prescribed to reverse severe respiratory depression and coma. 4. Continue to monitor level of responsiveness and respirations, pulse, and blood pressure.Duration of action of naloxone hydrochloride is shorter than that of heroin;repeated dosages may be necessary. 5.Send urine for analysis; opioids can be detected in urine. 6. Obtain an electrocardiogram. 7. Do not leave patient unattended;he or she may lapse back into coma rapidly. Clinical status may change from minute to minute. Hemodialysis may be indicated for severe drug intoxication. Activated charcoal may be considered if opioids were taken orally and if the patient is alert.
8. Monitor for pulmonary edema, which is frequently seen in patients who abuse/overdose on narcotics. 9. Refer patient for psychiatric and drug rehabilitation evaluation before discharge.
Barbiturates Pentobarbital (Nembutal), secobarbital (Seconal), amobarbital (Amytal), gamma-hydroxybutyrate (GHB, liquid Ecstasy)
Acute intoxication (may mimic alcohol intoxication): Respiratory depression Flushed face Decreased pulse rate; decreased blood pressure Increasing nystagmus Depressed deep tendon reexes Decreasing mental alertness Difculty in speaking Poor motor coordination Coma, death GHB: Sexual disinhibition Amnesia, myoclonus, agitation Overdoses when mixed with alcohol
Inhalants Amyl nitrate Freon Propane Trichloroethylene Gasoline Perchloroethylene Toluene (metallic paint spray)
Effects mimic those of alcohol, with dizziness and imbalance Euphoria, headache, altered level of consciousness to coma Renal, hepatic, and cardiac toxicity Aplastic anemia Fetal growth retardation Respiratory depression Vasodilation Nosebleeding Circumoral red spots
1. Maintain airway and provide respiratory support. 2. Endotracheal intubation or tracheostomy is considered if there is any doubt about the adequacy of airway exchange. a. Check airway frequently. b. Perform suctioning as necessary. 3. Support cardiovascular and respiratory functions; most deaths result from respiratory depression or shock. 4. Start infusion through large-gauge needle or IV catheter to support blood pressure;coma and dehydration result in hypotension and respond to infusion of intravenous uids with elevation of blood pressure. Sodium bicarbonate may be prescribed to alkalinize urine; it promotes excretion of barbiturates. 5. Evacuate stomach contents or lavage as soon as possible to prevent absorption; repeated doses of activated charcoal may be administered. 6. Assist with hemodialysis for severely overdosed patient. 7. Maintain neurologic and vital sign ow sheet. 8. Patient awakening from overdose may demonstrate combative behavior. 9. Refer for psychiatric and drug rehabilitation consultation to evaluate suicide potential and drug abuse. 1. Provide airway support, ventilation, and oxygen. 2. Treat cardiac dysrhythmias and hypotension. 3. Provide advanced cardiac life support (ACLS) as needed. 4. Monitor for profound hypotension when amyl nitrate is combined with MDMA and sildenal.
Amphetamine-Type Drugs (pep pills, uppers, speed, crystal meth) Amphetamine (Benzedrine) Dextroamphetamine (Dexedrine) Methamphetamine (Desoxyn, speed) 3,4Methylenedioxymethamphetamine (MDMA) (Ecstasy, Adam)* 3,4Methylenedioxymethamphetamine (MDEA) (Eve) 3,4-Methylenedioxyamphetamine (MDA)methylphenidate (Ritalin) ice, rocks, crystal meth
Nausea, vomiting, anorexia, palpitations, tachycardia, increased blood pressure, tachypnea, anxiety, nervousness, diaphoresis, mydriasis Repetitive or stereotyped behavior Irritability, insomnia, agitation Visual misperceptions, auditory hallucinations Fearfulness, anxiety, depression, hostility, paranoia Hyperactivity, rapid speech, euphoria, hyperalertness Decreased inhibition Seizures, coma, hyperthermia, cardiovascular collapse, rhabdomyolysis MDMA is both a hallucinogenic and stimulant
1. Provide airway support, ventilation, cardiac monitoring; insert IV line. 2. Use gastrointestinal (GI) evacuation in cases of oral overdose; activated charcoal, gastric lavage. 3. Keep in calm, cool, quiet environment; elevated temperature potentiates amphetamine toxicity. Maintain normothermia cooling the patient as necessary. 4. Use small doses of diazepam (Valium) (IV) or haloperidol (Haldol) as prescribed for CNS and muscular hyperactivity. 5.Administer appropriate pharmacologic therapy as prescribed for severe hypertension and ventricular dysrhythmias. 6.Treat seizures with benzodiazepines (eg, diazepam) as prescribed. 7. Treat sympathetic stimulation with beta-blocker agents as prescribed. 8. Try to communicate with patient if delusions or hallucinations are present. 9. Place in a protective environment (preferably psychiatric security room with video monitoring) to observe for suicide attempt. 10. Refer for psychiatric and drug rehabilitation evaluation. 1. Evaluate and maintain patients airway, breathing, and circulation. 2. Determine by urine or serum drug screen whether the patient has ingested hallucinogenic drug or has a toxic psychosis. 3.Try to communicate with and reassure the patient. a. Talking down involves understanding the process through which the patient is proceeding and helping him overcome his fears while establishing contact with reality. b. Remind the patient that fear is common with this problem. c. Reassure the patient that he is not losing his mind but is experiencing the effect of drugs and that this will wear off.
Hallucinogens or Psychedelic-Type Drugs Lysergic acid diethylamide (LSD) Phencyclidine HCl (PCP, angel dust) Mescaline, psilocybin Cannabinoids (marijuana) Ketamine (special K)
Nystagmus Mild hypertension Marked confusion bordering on panic Incoherence, hyperactivity Withdrawn Combative behavior; delirium, mania, selfinjury (lasts 6 to 12 hours) Hallucinations, body image distortion Hypertension, hyperthermia, renal failure Flashback: recurrence of LSD-like state without having taken the drug; may occur weeks or months after drug was taken Ketamine: out-of-body experience; increased aggressiveness
d. Instruct the patient to keep the eyes open; this reduces the intensity of reaction. e. Reduce sensory stimuli: minimize noise, lights, movement, tactile stimulation. 4. Sedate the patient as prescribed if hyperactivity cannot be controlled; diazepam (Valium) or a barbiturate may be prescribed. 5. Search for evidence of trauma; hallucinogen users have a tendency to act out their hallucinations. 6.Manage seizures with benzodiazepines (eg, diazepam) as necessary. 7. Observe patient closely; patients behavior may become hazardous. Have safety ofcers stationed near the patients room. 8. Monitor for hypertensive crisis if patient has prolonged psychosis due to drug ingestion. 9. Place patient in a protected environment under proper medical supervision to prevent self-inicted bodily harm. Management for Phencyclidine Abusers 1. Place patient in a calm, supportive environment to minimize stimuli; protect From self-injury. 2. Avoid talking down. 3. Do not leave patient unobserved. Treat symptoms as they occur. a. Drug effects are unpredictable and prolonged. b. Symptoms are likely to exacerbate; patient becomes out of control. 4. Refer all patients in this category for psychiatric and drug evaluation/ rehabilitation. Drugs Producing Sedation, Intoxication, or Psychological and Physical Dependence (nonbarbiturate sedatives) Diazepam (Valium) Chlordiazepoxide (Librium) Oxazepam (Serax) Lorazepam (Ativan) Midazolam (Versed) Flunitrazepam (Rohypnol, rooes, date rape drug)* Seizures, coma, circulatory collapse, death Acute intoxication: Respiratory depression Decreasing mental alertness Confusion Slurred speech, decreased blood pressure Ataxia Pulmonary edema Coma, death Flunitrazepam: 1. Endotracheal tube is inserted as a precaution; use assisted ventilation to stabilize and correct respiratory depression. Observe for sudden apnea and laryngeal spasm. 2. Assess for hypotension a. Insert indwelling urinary catheter for comatose patient; decreased urinary volume is an index of reduced renal
Disinhibition with antegrade amnesia Weakness and unsteadiness with impaired judgment Powerlessness
ow associated with reduced intravascular volume or vascular collapse. b. Start volume expansion with saline or dextrose as prescribed. 3. Evacuate stomach contents; emesis; lavage; activated charcoal; cathartic. 4. Start ECG monitoring. Observe for dysrhythmias. 5.Administer umazenil (Romazicon), a benzodiazepine antagonist (reversal agent). 6. Refer patient for psychiatric evaluation (potential suicide intent). 1. Treat respiratory depression. 2. Induce gastric emptying by lavage. 3. Give activated charcoal to adsorb aspirin; a cathartic may be administered With charcoal to help ensure intestinal cleansing. 4. Support patient with IV infusions as prescribed to establish hydration and correct electrolyte imbalances, including Administration of sodium bicarbonate. 5. Enhance elimination of salicylates as directed by forced diuresis, alkalinization of urine, peritoneal dialysis, or hemodialysis, according to severity of intoxication. 6. Monitor serum salicylate level for efcacy of treatment. 7. Administer specic prescribed pharmacologic agent for bleeding and other problems. 8. Concretions formed in the gut may result in prolonged exposure as they are digested. 9. Refer patient for psychiatric evaluation (potential suicide intent). 1. Maintain airway. 2. Obtain acetaminophen level. Levels _140 mg/kg are toxic. 3. Laboratory studiesliver function tests, prothrombin time/partial thromboplastin time, complete blood count, blood urea nitrogen, creatinine. 4. Administer syrup of ipecac and follow emesis with activated charcoal. 5. Prepare for possible hemodialysis, which clears acetaminophen but does not halt liver damage.
Salicylate Poisoning Aspirin (present in compound analgesic tablets) Toxic levels (150200 mg/kg body weight) Chronic toxicity (occurs in elderly due to decreased renal function) Long-term intoxication (_100 mg/kg/day for more than 2 days)
Restlessness, tinnitus, deafness, blurring of vision Hyperpnea, hyperpyrexia, sweating Epigastric pain, vomiting, dehydration Respiratory alkalosis and metabolic acidosis Disorientation, coma, cardiovascular collapse Coagulopathy
Acetaminophen (present in prescription and nonprescription analgesics, antipyretics, and cold remedies)
Lethargy to encephalopathy and death GI upset, diaphoresis Right upper quadrant pain Abnormal liver function tests, prolonged prothrombin time, increased bilirubin, disseminated intravascular coagulation Hepatomegaly leading to liver failure Metabolic acidosis Hypoglycemia
6. Administer N-acetylcysteine (NAC, Mucomyst) as soon as possible. NAC replenishes essential liver enzymes and requires a total of 18 doses every 4 hours. Charcoal absorbs NAC; do not administer together. Repeat NAC dose if patient vomits. 7. Refer patient for psychiatric evaluation (potential suicide intent). Tricyclic Antidepressants (TCAs) Amitriptyline (Elavil) Doxepin (Sinequan) Nortriptyline (Aventyl) Imipramine (Tofranil) Dysrhythmia: ventricular brillation/ tachycardia, tachycardia Hypotension Pulmonary edema, hypoxemia, acidosis Confusion, agitation, coma Visual hallucinations Clonus, tremors, hyperactive reexes, nystagmus, myoclonic jerking Seizures Blurred vision, ushing, hyperthermia 1. Provide airway support, ventilation, cardiac monitoring; insert IV line with normal saline solution. 2. If within 12 hours after overdose, insert a nasogastric tube and instill activated charcoal with sorbitol every 4 hours. 3. Administer a sodium bicarbonate drip to decrease dysrhythmias; the alkaline environment increases the protein binding of the metabolite. 4. Administer vasopressors. 5. Use only Class IB antiarrhythmics (eg, lidocaine), as some other types of antiarrhythmics have the same effect as TCA. 6. Manage seizure activity with benzodiazepines (eg, diazepam) as necessary. 7. Refer patient for psychiatric evaluation for potential suicide intent and evaluation of medication regimen for effectiveness.
Selective Serotonin Reuptake Inhibitors Decreased level of consciousness, confusion 1. Administer activated charcoal with (SSRIs) and Other Antidepressants Respiratory depression possibly whole-bowel irrigation if a Trazodone (Desyrel) Increased heart rate sustained-release medication was taken. Fluoxetine (Prozac) Serotonin syndrome: 2. Use seizure precautions and administer Paroxetine (Paxil) Agitation, seizures benzodiazepines (eg, diazepam) as Sertraline (Zoloft) Hyperthermia, diaphoresis ordered. Venlafaxine (Effexor) Hypertension 3. Serotonin syndrome may occur if the Escitalopram (Lexapro) SSRI was taken in conjunction with Bupropion (Wellbutrin) dextromethorphan or meperidine. Source: Brunner & Suddarths textbook of medical-surgical nursing. 12th ed. /Suzanne C. Smeltzer ... [et al.].pp.2178-2183
You might also like
- SJCTs Pilot Examination Information & InstructionsDocument6 pagesSJCTs Pilot Examination Information & InstructionsSkep100% (1)
- Common Signs and Symptoms of Diseases (Pathognomonic Sign)Document3 pagesCommon Signs and Symptoms of Diseases (Pathognomonic Sign)theglobalnursing91% (11)
- Lifestyle DiseasesDocument44 pagesLifestyle Diseaseskyro draxNo ratings yet
- Drugs Affecting Calcium BalanceDocument63 pagesDrugs Affecting Calcium BalanceRd Chandane100% (1)
- Exam 3 Review Med SurgDocument18 pagesExam 3 Review Med SurgCarol ReidNo ratings yet
- HIV Practice TestDocument2 pagesHIV Practice TestJoslyn GrossNo ratings yet
- OD-PRO-HSE-032 Safety To Work at Height - Rev.01Document31 pagesOD-PRO-HSE-032 Safety To Work at Height - Rev.01aymenmoataz100% (1)
- LVMH - Code of ConductDocument13 pagesLVMH - Code of ConductElena DianaNo ratings yet
- Drug Overdose and ManagementDocument9 pagesDrug Overdose and ManagementKoRnflakes100% (1)
- Night Sweats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandNight Sweats, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Myocarditis, (Inflamed Heart Muscles) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandMyocarditis, (Inflamed Heart Muscles) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Sirs, Shock, Sepsis, ModsDocument8 pagesSirs, Shock, Sepsis, ModsthubtendrolmaNo ratings yet
- Everything You Need to Know About DiabetesDocument39 pagesEverything You Need to Know About DiabetesSubramaniam RamanNo ratings yet
- Understanding Low Blood PressureDocument6 pagesUnderstanding Low Blood PressureRajeev Nechiyil100% (1)
- Adult Health III Final Study GuideDocument12 pagesAdult Health III Final Study GuideRyanne JNo ratings yet
- ShockDocument21 pagesShockMin-Joo Esther ParkNo ratings yet
- Administration of Injections PresentationsDocument30 pagesAdministration of Injections PresentationsgopusankarNo ratings yet
- Diagnosis & Treament: ShockDocument52 pagesDiagnosis & Treament: ShockasepNo ratings yet
- Infective Diseases of Heart: Wella KarolinaDocument47 pagesInfective Diseases of Heart: Wella KarolinahayosiapaNo ratings yet
- Fluid Electrolytes and Acid Base BalanceDocument108 pagesFluid Electrolytes and Acid Base BalancesayednourNo ratings yet
- Bee Stings: The British Beekeepers AssociationDocument3 pagesBee Stings: The British Beekeepers AssociationantonioforteseNo ratings yet
- Thyroid CrisisDocument11 pagesThyroid CrisisKoka KolaNo ratings yet
- Hypertensive DrugsDocument2 pagesHypertensive DrugsNedaAbdullahNo ratings yet
- Seminar On Shock: IntroductionDocument22 pagesSeminar On Shock: Introductionmahendra singhNo ratings yet
- Acute Pancreatitis: J Koh & D ChengDocument7 pagesAcute Pancreatitis: J Koh & D ChengGloriaaaNo ratings yet
- Safe SuctioningDocument31 pagesSafe SuctioningKatrina Ponce100% (2)
- Addisonian Crisis: Manish K Medical Officer IgmhDocument47 pagesAddisonian Crisis: Manish K Medical Officer IgmhNaaz Delhiwale100% (1)
- Pericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerDocument2 pagesPericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerlhenNo ratings yet
- Shock, Sirs & ModsDocument37 pagesShock, Sirs & ModsambitioustamannaNo ratings yet
- Anaphylaxis Shock: Bagian Anestesi FK UNISSULA SemarangDocument15 pagesAnaphylaxis Shock: Bagian Anestesi FK UNISSULA SemarangTeguh PambudiNo ratings yet
- Addison and Cushing DMDocument22 pagesAddison and Cushing DManon_391984943No ratings yet
- Multiple SclerosisDocument6 pagesMultiple SclerosisRonnel Alvin Antonio AdrianoNo ratings yet
- Medical-Surgical Nursing Review: 315 Key ConceptsDocument15 pagesMedical-Surgical Nursing Review: 315 Key ConceptsJap Avila BernasNo ratings yet
- Municable DiseasesDocument18 pagesMunicable DiseasesEdamarie ChuaNo ratings yet
- CKD Symptoms and TreatmentsDocument3 pagesCKD Symptoms and TreatmentsrhizzyNo ratings yet
- WHO Management of PoisoningDocument159 pagesWHO Management of PoisoningMarian Joyce Princess YuqueNo ratings yet
- A. Cardiac Failure: Biologic CrisisDocument11 pagesA. Cardiac Failure: Biologic CrisisJillian CaumbanNo ratings yet
- Acute Myocardial InfarctionDocument22 pagesAcute Myocardial InfarctionkpsuanNo ratings yet
- ShockDocument21 pagesShockNyakie MotlalaneNo ratings yet
- Evaluation and Management of Suspected Sepsis and Septic Shock in AdultsDocument62 pagesEvaluation and Management of Suspected Sepsis and Septic Shock in AdultsGiussepe Chirinos CalderonNo ratings yet
- Asthma and COPD NCLEXDocument17 pagesAsthma and COPD NCLEXPotchiee PfizerNo ratings yet
- Cad PPTDocument81 pagesCad PPTvaishnaviNo ratings yet
- Pleural Fluid AnalysisDocument15 pagesPleural Fluid AnalysisNatalie Sarah MoonNo ratings yet
- Nursing Managment of Chest Tubes: by Alice Leung RN, BSN, PCCNDocument55 pagesNursing Managment of Chest Tubes: by Alice Leung RN, BSN, PCCNFrancis Xavier S. Mendez0% (1)
- Myocardium - The heart muscle that surrounds the ventricles and atriaDocument19 pagesMyocardium - The heart muscle that surrounds the ventricles and atriaFilane AntonetteNo ratings yet
- Anatomy, Diagnostics and Nursing Care of Pancreatitis and Gallbladder DisordersDocument21 pagesAnatomy, Diagnostics and Nursing Care of Pancreatitis and Gallbladder DisordersKatrinaJimenezNo ratings yet
- Eye ExaminationDocument23 pagesEye Examinationcynthia167No ratings yet
- Dissiminated Intravascular Coagulation PathoDocument2 pagesDissiminated Intravascular Coagulation Pathoapi-341263362No ratings yet
- DR Anuj Raj BijukchheDocument95 pagesDR Anuj Raj BijukchheMUHAMMAD JAWAD HASSANNo ratings yet
- InhalDocument33 pagesInhallupeNo ratings yet
- EYE DISORDERS: GLAUCOMA AND CATARACTSDocument127 pagesEYE DISORDERS: GLAUCOMA AND CATARACTSjoan olanteNo ratings yet
- Drug Used in Skin and Mucus MembraneDocument35 pagesDrug Used in Skin and Mucus MembraneMamta Yadav100% (1)
- Neuro, GI, GU, MSK midterm and final reviewDocument3 pagesNeuro, GI, GU, MSK midterm and final reviewjenn1722No ratings yet
- Concept Map Et Al 11-04-15Document7 pagesConcept Map Et Al 11-04-15api-353656227No ratings yet
- Main drug therapy for ulcerative colitis is sulfa for one yearDocument4 pagesMain drug therapy for ulcerative colitis is sulfa for one yearcathyNo ratings yet
- Hypertension and Cardiovascular DiseaseDocument99 pagesHypertension and Cardiovascular DiseaseMiguel CuevasNo ratings yet
- Case Study: Congestive Heart FailureDocument7 pagesCase Study: Congestive Heart FailureXI-E / 21 / MARY TRIANANo ratings yet
- Empyema 171013100219Document23 pagesEmpyema 171013100219Mahmoud Abdel MoneimNo ratings yet
- Cardiovascular EmergenciesDocument20 pagesCardiovascular EmergenciesJohn FisherNo ratings yet
- Basic Principles in Disaster Nursing and ShockDocument12 pagesBasic Principles in Disaster Nursing and ShockitsmyhavenNo ratings yet
- Chapter 25heart Failure and Inflammatory DysfunctionDocument10 pagesChapter 25heart Failure and Inflammatory DysfunctionNurse UtopiaNo ratings yet
- Congestive Heart FailureDocument74 pagesCongestive Heart FailureNiharikaNo ratings yet
- Chap.30 Med SurgDocument4 pagesChap.30 Med SurgSheldon SloanNo ratings yet
- Portal hypertension diagnosis and managementDocument23 pagesPortal hypertension diagnosis and managementSumathi Gopinath100% (1)
- Disorders of Cranial NervesDocument3 pagesDisorders of Cranial Nervestheglobalnursing100% (2)
- NLE 12-2012 ResultsDocument359 pagesNLE 12-2012 ResultsPRC Baguio0% (2)
- Perioperative NursingDocument12 pagesPerioperative Nursingtheglobalnursing100% (12)
- Major Fluid and Electrolyte ImbalancesDocument5 pagesMajor Fluid and Electrolyte ImbalancestheglobalnursingNo ratings yet
- Expanded Program On ImmunizationDocument1 pageExpanded Program On ImmunizationtheglobalnursingNo ratings yet
- Common Eye Problems in ChildrenDocument6 pagesCommon Eye Problems in ChildrentheglobalnursingNo ratings yet
- Summary Differences Between Dementia and DeliriumDocument4 pagesSummary Differences Between Dementia and Deliriumtheglobalnursing100% (1)
- Congenital Heart DiseasesDocument6 pagesCongenital Heart Diseasestheglobalnursing100% (2)
- Disorders of The Lips, Mouth and GumsDocument5 pagesDisorders of The Lips, Mouth and GumstheglobalnursingNo ratings yet
- Gastrointestinal SystemDocument8 pagesGastrointestinal Systemtheglobalnursing100% (1)
- Respiratory SystemDocument9 pagesRespiratory Systemtheglobalnursing89% (9)
- Cardiovascular SystemDocument10 pagesCardiovascular Systemtheglobalnursing75% (4)
- Fundamentals of NursingDocument44 pagesFundamentals of Nursingtheglobalnursing100% (2)
- Neurologic NursingDocument14 pagesNeurologic Nursingtheglobalnursing100% (6)
- Pyschiatric NursingDocument40 pagesPyschiatric Nursingtheglobalnursing100% (1)
- Maternal and Child NursingDocument63 pagesMaternal and Child Nursingtheglobalnursing100% (1)
- Musculoskeletal System Nursing ReviewerDocument11 pagesMusculoskeletal System Nursing Reviewerposh003850% (2)
- Endocrine SystemDocument8 pagesEndocrine Systemtheglobalnursing80% (5)
- Community Health NursingDocument9 pagesCommunity Health NursingtheglobalnursingNo ratings yet
- Speech Disorders - ChildrenDocument2 pagesSpeech Disorders - ChildrenAmanda Kenshi NurfitriNo ratings yet
- Mozart, Beethoven, Yesudas Effect Class 2Document12 pagesMozart, Beethoven, Yesudas Effect Class 2Dr Suvarna NalapatNo ratings yet
- ImplantsDocument11 pagesImplantsraheelNo ratings yet
- Administering Blood Transfusion GuideDocument1 pageAdministering Blood Transfusion GuideKyla ManarangNo ratings yet
- Ethical Decision Making in ResearchDocument2 pagesEthical Decision Making in ResearchChandraKurniawanNo ratings yet
- Interim Public Health Operational Guidelines For Amoebiasis: (Entamoeba Histolytica)Document34 pagesInterim Public Health Operational Guidelines For Amoebiasis: (Entamoeba Histolytica)QworldNo ratings yet
- Umesh Pharma 1507821908 - 365Document22 pagesUmesh Pharma 1507821908 - 365Training and PlacementNo ratings yet
- PALLIATIVE CARE SYMPTOM MANAGEMENTDocument153 pagesPALLIATIVE CARE SYMPTOM MANAGEMENTrlinao100% (3)
- Douglas Crucey, A043 446 797 (BIA June 12, 2017)Document20 pagesDouglas Crucey, A043 446 797 (BIA June 12, 2017)Immigrant & Refugee Appellate Center, LLCNo ratings yet
- Performa Stereo Quick User GuideDocument2 pagesPerforma Stereo Quick User GuideJUAN CARLOSNo ratings yet
- Igem ListDocument9 pagesIgem ListMilad YadollahiNo ratings yet
- FrostbiteDocument17 pagesFrostbiteIsabel Barredo Del Mundo100% (2)
- AA PamphletDocument52 pagesAA PamphletCarmen UleiaNo ratings yet
- Grade 7 (TLE) Week 1Document12 pagesGrade 7 (TLE) Week 1RoswlleNo ratings yet
- Catheterization ChecklistDocument3 pagesCatheterization ChecklistAlthea Aubrey AgbayaniNo ratings yet
- New Applications August 2022Document70 pagesNew Applications August 2022rahul kakapuriNo ratings yet
- Remember: Blood CirculationDocument4 pagesRemember: Blood CirculationvicpardoNo ratings yet
- Mary Law PEO Model PDFDocument15 pagesMary Law PEO Model PDFalepati29No ratings yet
- Cancer Lesson Plan For High SchoolDocument7 pagesCancer Lesson Plan For High SchoolUm IbrahimNo ratings yet
- All India Aakash Test Series (AIATS) 12th Class Test Schedule for NEET/AIIMS 2019Document2 pagesAll India Aakash Test Series (AIATS) 12th Class Test Schedule for NEET/AIIMS 2019Chirasree Laha100% (1)
- Label, Procedure, AdvertisementDocument6 pagesLabel, Procedure, AdvertisementActrissia Aprilla SandhyNo ratings yet
- Verification of Conformity Safety Consideration For Radio Equipment DirectiveDocument1 pageVerification of Conformity Safety Consideration For Radio Equipment DirectiveThắng CòiNo ratings yet
- Mole Airlines, Emp. Form. ExcerciseDocument2 pagesMole Airlines, Emp. Form. ExcerciseKamariah IsmailNo ratings yet
- K CC1 102 Hse MSDS 005 - R0 EaDocument8 pagesK CC1 102 Hse MSDS 005 - R0 EaWalter Gerardo BelluzNo ratings yet
- Single/ Exam Zone Centre DetailsDocument5 pagesSingle/ Exam Zone Centre DetailsHarsh AroraNo ratings yet
- Manuale Advantage 350Document50 pagesManuale Advantage 350PaulmankeNo ratings yet
- D A Up To 2 YearDocument7 pagesD A Up To 2 YearNischitha G CNo ratings yet